Predictors of a Change and Correlation in Activities of Daily Living after Hip Fracture in Elderly Patients in a Community Hospital in Poland: A Six-Month Prospective Cohort Study
Abstract
:1. Introduction
2. Objectives
3. Materials and Methods
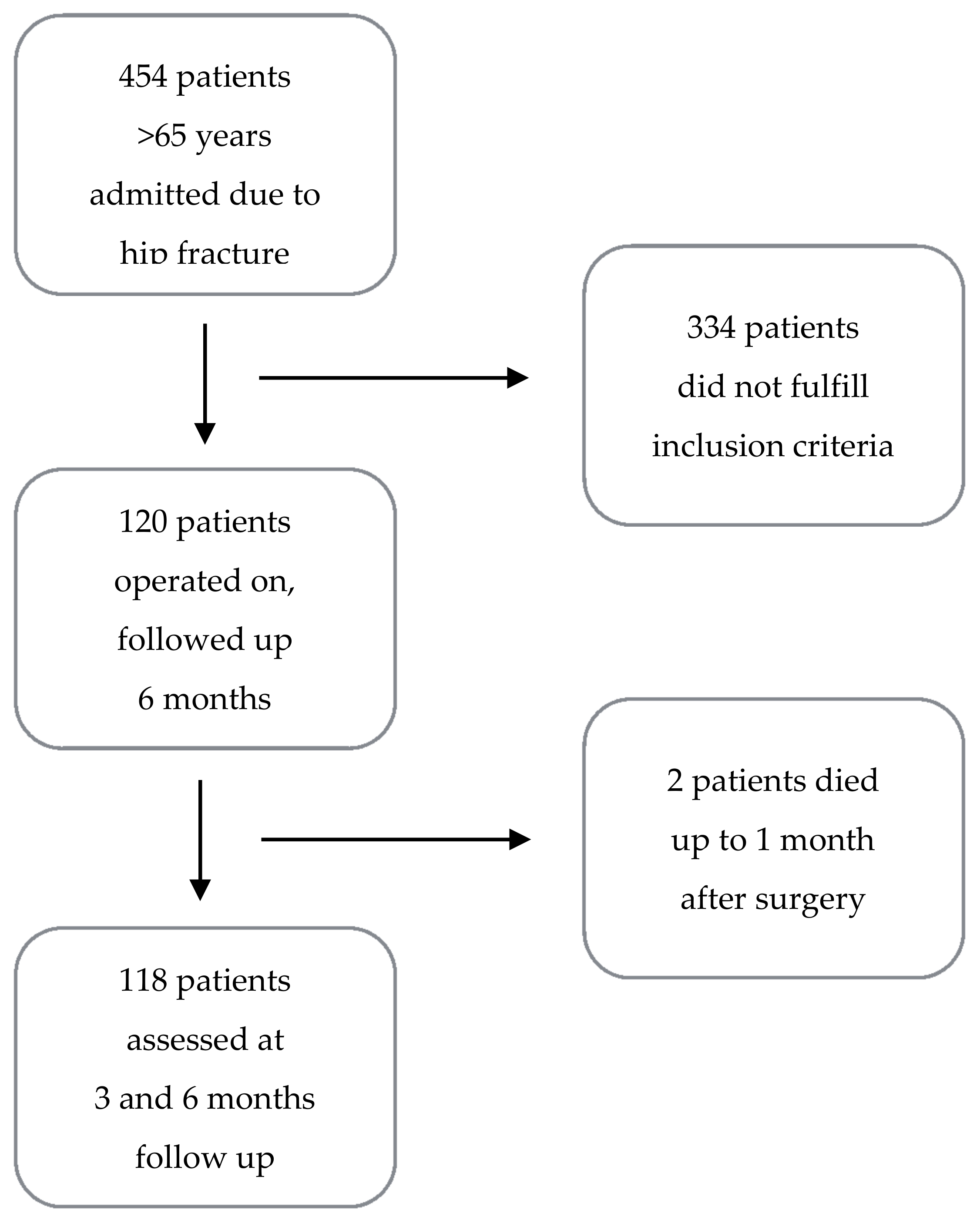
3.1. Design, Setting, Population, and Sampling
3.2. Data Collection
3.3. Statistical Analysis
4. Results
4.1. Baseline Characteristics and Surgical Features of Patients
4.2. Change in Functional Status
4.3. Prognostic Factors for Functional Status at Follow-Up
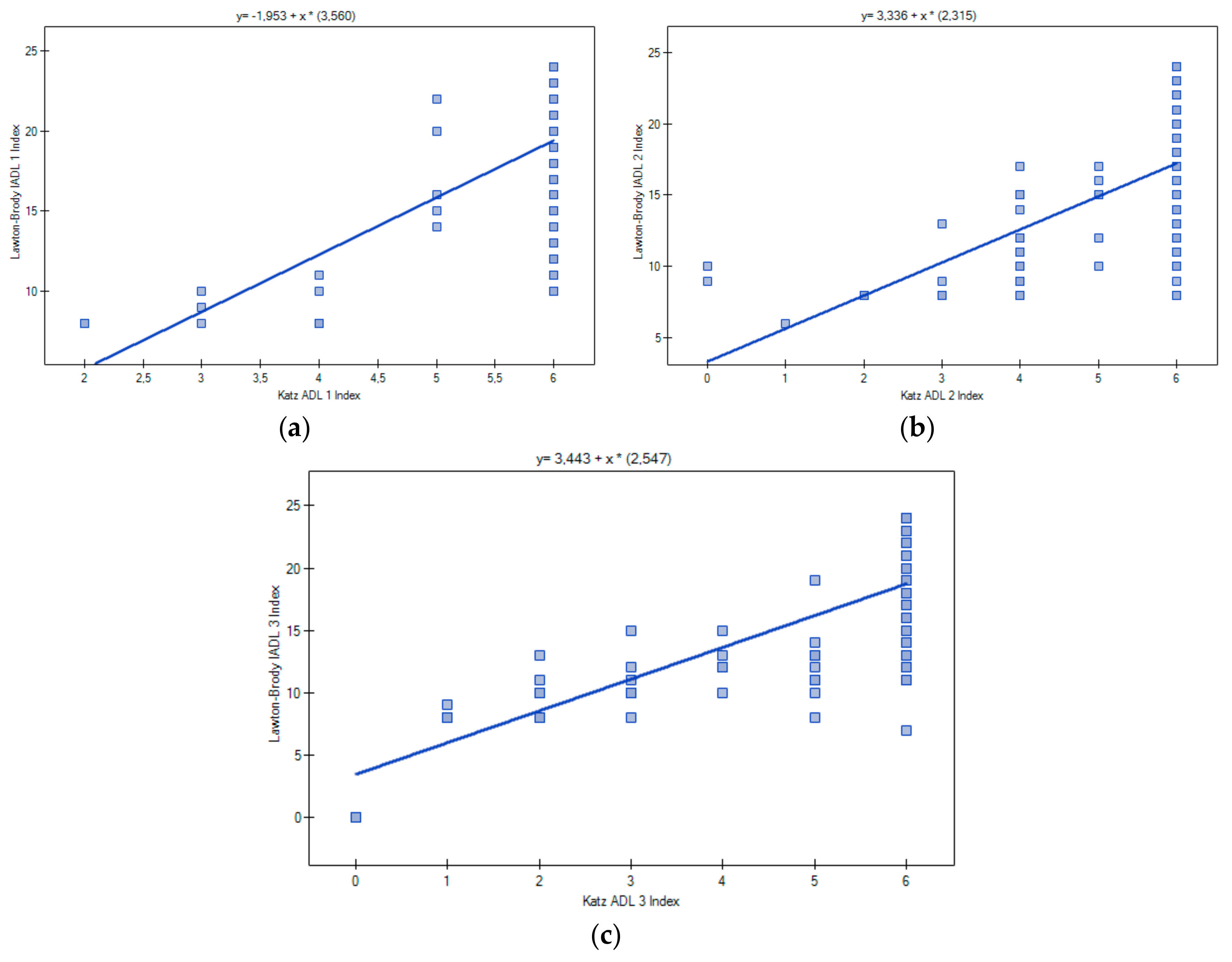
4.4. Correlation between ADL and IADL
5. Discussion
5.1. Results Overview
5.2. Change in Functional Status
5.3. Correlation between ADL and IADL
5.4. Predictors for Functional Outcomes: ADL and IADL
6. Limitations
7. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Roth, T.; Kammerlander, C.; Gosch, M.; Luger, T.J.; Blauth, M. Outcome in geriatric fracture patients and how it can be improved. Osteoporos. Int. 2010, 21 (Suppl. 4), S615–S619. [Google Scholar] [CrossRef] [PubMed]
- Cummings, S.R.; Melton, L.J. Epidemiology and outcomes of osteoporotic fractures. Lancet 2002, 3359, 1761–1767. [Google Scholar] [CrossRef]
- Vergara, I.; Vrotsou, K.; Orive, M.; Gonzalez, N.; Garcia, S.; Quintana, J.M. Factors related to functional prognosis in elderly patients after accidental hip fractures: A prospective cohort study. BMC Geriatr. 2014, 14, 124. [Google Scholar] [CrossRef] [PubMed]
- Czerwiński, E.; Boczoń, K.; Kumorek, A. Epidemiology of osteoporotic fractures. Postp. Nauk Med. 2012, 3, 206–212. [Google Scholar]
- Kanis, J.A.; Odén, A.; McCloskey, E.W.; Johansson, H.; Wahl, D.A.; Cooper, C.; IOF Working Group on Epidemiology and Quality of Life. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos. Int. 2012, 23, 2239–2256. [Google Scholar] [PubMed]
- Spector, W.D.; Fleishman, J.A. Combining activities of daily living with instrumental activities of daily living to measure functional disability. J. Gerontol. 1998, 53, 46–57. [Google Scholar] [CrossRef]
- Dyer, S.M.; Crotty, M.; Fairhall, N.; Magaziner, J.; Beaupre, L.A.; Cameron, I.D.; Sherrington, C.; Fragility Fracture Network (FFN) Rehabilitation Research Special Interest Group. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016, 16, 158. [Google Scholar]
- Norton, R.; Butler, M.; Robinson, E.; Lee-Joe, T.; Campbell, A.J. Declines in physical functioning attributable to hip fracture among older people: A follow-up study of case-control participants. Disabil. Rehabil. 2000, 22, 345–351. [Google Scholar] [PubMed]
- Papadimitriou, N.; Tsilidis, K.K.; Orfanos, P.; Benetou, V.; Ntzani, E.E.; Soerjomataram, I.; Künn-Nelen, A.; Pettersson-Kymmer, U.; Eriksson, S.; Brenner, H.; et al. Burden of hip fracture using disability-adjusted life-years: A pooled analysis of prospective cohorts in the CHANCES consortium. Lancet 2017, 2, e239–e246. [Google Scholar] [CrossRef]
- Shah, M.R.; Aharonoff, G.B.; Wolinsky, P.; Zuckerman, J.D.; Koval, K.J. Outcome after hip fracture in individuals ninety years of age and older. J. Orthop. Trauma 2001, 15, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Alegre-López, J.; Cordero-Guevara, J.; Alonso-Valdivielso, J.L.; Fernandez-Melon, J. Factors associated with mortality and functional disability after hip fracture: An inception cohort study. Osteoporos. Int. 2005, 16, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.T. Factors affecting functional prognosis of patients with hip fracture. Eur. J. Phys. Rehabil. Med. 2011, 47, 257–264. [Google Scholar] [PubMed]
- Córcoles-Jiménez, M.P.; Villada-Munera, A.; Del Egido-Fernández, M.Á.; Candel-Parra, E.; Moreno-Moreno, M.; Jiménez-Sánchez, M.D.; Piña-Martínez, A. Recovery of activities of daily living among older people one year after hip fracture. Clin. Nurs. Res. 2015, 24, 604–623. [Google Scholar] [CrossRef] [PubMed]
- Mariconda, M.; Costa, G.G.; Cerbasi, S.; Recano, P.; Orabona, G.; Gambacorta, M.; Misasi, M. Factors Predicting Mobility and the Change in Activities of Daily Living after Hip Fracture: A 1-Year Prospective Cohort Study. J. Orthop. Trauma 2016, 30, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, M.G.; Ginex, V.; Mariani, E.; Zati, A.; Cotti, A.; Pignotti, E.; Clerici, F. Cognitive impairment is a negative short-term and long-term prognostic factor in elderly patients with hip fracture. Eur. J. Phys. Rehabil. Med. 2015, 51, 815–823. [Google Scholar] [PubMed]
- Pfeifer, E. Short Portable Mental Status Questionnaire (SPMSQ). J. Am. Geriatr. Soc. 1975, 23, 433–441. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- El Miedany, Y. Comorbidity in Rheumatic Diseases; Springer: Cham, Switzerland, 2017. [Google Scholar]
- Katz, S.; Ford, A.; Moskowitz, W.R.; Jackson, A.B.; Jaffe, M.W. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontology 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Daabiss, M. American Society of Anaesthesiologists physical status classification. Indian J. Anaesth. 2011, 55, 111–115. [Google Scholar] [CrossRef] [PubMed]
- R Development Core Team. A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, 2015. Available online: http://www.R-project.org (accessed on 10 August 2017).
- Venables, W.N.; Ripley, B.D. Modern Applied Statistics with S, 4th ed.; Springer: New York, NY, USA, 2002; Available online: http://www.stats.ox.ac.uk/pub/MASS4 (accessed on 8 September 2017).
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression, 2nd ed.; John Wiley & Sons Inc.: New York, NY, USA; Chichester, UK; Weinheim, Germany; Brisbane, Australia; Singapore; Toronto, ON, Canada, 2000. [Google Scholar]
- Lin, P.C.; Chang, S.Y. Functional recovery among elderly people one year after hip fracture surgery. J. Nurs. Res. 2004, 12, 72–82. [Google Scholar] [CrossRef] [PubMed]
- Koval, K.J.; Skovron, M.L.; Polatsch, D.; Aharonoff, G.B.; Zuckerman, J.D. Dependency after hip fracture in geriatric patients: A study of predictive factors. J. Orthop. Trauma 1996, 10, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Beaupre, L.A.; Jones, C.A.; Johnston, D.W.; Wilson, D.M.; Majumdar, S.R. Recovery of function following a hip fracture in geriatric ambulatory persons living in nursing homes: Prospective cohort study. J. Am. Geriatr. Soc. 2012, 60, 1268–1273. [Google Scholar] [CrossRef] [PubMed]
- González-Zabaleta, J.; Pita-Fernandez, S.; Seoane-Pillado, T.; López-Calviño, B.; Gonzalez-Zabaleta, J.L. Dependence for basic and instrumental activities of daily living after hip fractures. Arch. Gerontol. Geriatr. 2015, 60, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Roehrig, B.; Hoeffken, K.; Pientka, L.; Wedding, U. How many and which items of activities of daily living (ADL) and instrumental activities of daily living (IADL) are necessary for screening. Crit. Rev. Oncol. Hematol. 2007, 62, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Kachooei, A.R.; Ebrahimzadeh, M.H.; HallajMoghadam, M.; Fattahi, A.S.; Razi, S.; Salehi, M.; Azema, H. Disabilities and activities of daily living among veterans with old hip disarticulation and transpelvic amputation. Arch. Trauma Res. 2014, 3, e16003. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Bennet, J.M.; Shaw, B.A.; Quiñones, A.R.; Ye, W.; Xu, X.; Ofstedal, M.B. Gender differences in functional status in middle and older age: Are there any age variations? J. Gerontol. Soc. Sci. 2008, 63B, S282–S292. [Google Scholar] [CrossRef]
- Sylliaas, H.; Thingstad, P.; Wyller, T.B.; Helbostad, J.; Sletvold, O.; Bergland, A. Prognostic factors for self-rated function and perceived health in patient living at home three months after a hip fracture. Disabil. Rehabil. 2012, 34, 1225–1231. [Google Scholar] [CrossRef] [PubMed]
- Dudkiewicz, I.; Burg, A.; Salai, M.; Hershkovitz, A.I. Gender differences among patients with proximal femur fractures during rehabilitation. Gend. Med. 2011, 8, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Samuelsson, B.; Hedström, M.I.; Ponzer, S.; Söderqvist, A.; Samnegård, E.; Thorngren, K.G.; Cederholm, T.; Sääf, M.; Dalen, N. Gender differences and cognitive aspects on functional outcome after hip fracture—A 2 years’ follow-up of 2134 patients. Age Ageing 2009, 38, 686–692. [Google Scholar] [CrossRef] [PubMed]
- Salthouse, T.A. When does age-related cognitive decline begin? Neurobiol. Aging 2009, 30, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Wills, P.; Viitanen, M.; Fastbom, J.; Winblad, B. Cognitive Impairment, Drug Use, and the Risk of Hip Fracture in Persons over 75 Years Old: A Community-based Prospective Study. Am. J. Epidemiol. 1998, 148, 887–892. [Google Scholar] [CrossRef] [PubMed]
- Dubljanin-Raspopović, E.; Marković-Denić, L.; Marinković, J.; Nedeljković, U.; Bumbaširević, M. Does early functional outcome predict 1-year mortality in elderly patients with hip fracture? Clin. Orthop. Relat. Res. 2013, 471, 2703–2710. [Google Scholar] [CrossRef] [PubMed]
- Padykuła, M.; Kózka, M. Cognitive impairment in geriatric patients hospitalized in the conservative ward. Probl. Pielęg. 2015, 23, 300–305. [Google Scholar]
- Gruber-Baldini, A.; Zimmerman, S.; Morrison, R.S.; Grattan, L.M.; Hebel, J.R.; Dolan, M.M.; Hawkes, W.; Magaziner, J. Cognitive Impairment in Hip Fracture Patients: Timing of Detection and Longitudinal Follow-Up. J. Am. Geriatr. Soc. 2003, 51, 1227–1236. [Google Scholar] [CrossRef] [PubMed]
- Chaves Gde, F.; Oliveira, A.M.; Chaves, J.A.; Forlenza, O.V.; Aprahamian, I.; Nunes, P.V. Assessment of impairment in activities of daily living in mild cognitive impairment using an individualized scale. Arq. Neuropsiquiatr. 2016, 74, 549–554. [Google Scholar] [CrossRef] [PubMed]
- Derejczyk, J.; Bień, B.; Kokoszka-Paszkot, J.; Szczygieł, J. Gerontology and geriatrics in Poland against Europe—Is it necessary to invest in? Gerontol. Pol. 2008, 16, 149–159. [Google Scholar]
- Heikkinen, T.; Jalovaara, P. Four or twelve months’ follow-up in the evaluation of functional outcome after hip fracture surgery? Scand. J. Surg. 2005, 94, 59–66. [Google Scholar] [CrossRef] [PubMed]
| Variable | Total | SPMSQ 8–10 | SPMSQ 6–7 | SPMSQ 3–5 | p |
|---|---|---|---|---|---|
| N = 120 | N = 59 | N = 29 | N = 32 | ||
| Age (years) | |||||
| Mean | 80.1 | 79.6 | 83.3 | 82 | 0.002 * |
| Gender | |||||
| Female | 98 (81.7) | 47 (79.7) | 24 (82.8) | 27 (84.3) | 0.84 * |
| Male | 22 (18.3) | 12 (20.3) | 5 (17.2) | 5 (15.7) | |
| Residence | |||||
| Urban | 74 (61.7) | 37 (62.7) | 20 (69.0) | 16 (50.0) | 0.29 * |
| Rural | 46 (38.3) | 22 (37.2) | 9 (31.0) | 16 (50.0) | |
| CCI Index | |||||
| 1–3 | 60 (50.0) | 41 (69.5) | 13 (44.8) | 6 (18.8) | <0.001 ** |
| 4–7 | 60 (50.0) | 18 (30.5) | 16 (55.2) | 26 (81.2) | Tau −0.43 |
| ADL index | |||||
| 5–6 | 110 (91.7) | 58 (98.3) | 29 (100.0) | 23 (71.9) | <0.001 ** |
| 3–4 | 8 (6.7) | 1 (1.7) | 0 (0.0) | 7 (21.9) | Tau 0.35 |
| 0–2 | 2 (1.6) | 0 (0.0) | 0 (0.0) | 2 (6.2) | |
| IADL score | |||||
| 19–24 | 65 (54.2) | 54 (91.5) | 10 (34.5) | 1 (3.1) | <0.001 ** |
| 13–18 | 36 (30.0) | 4 (6.8) | 19 (65.5) | 13 (40.6) | Tau 0.77 |
| 9–12 | 13 (10.8) | 1 (1.7) | 0 (0.0) | 12 (37.5) | |
| ≤8 | 6 (5.0) | 0 (0.0) | 0 (0.0) | 6 (18.8) | |
| Type of fracture | |||||
| Intertrochanteric | 75 (62.5) | 38 (64.4) | 18 (62.1) | 20 (62.5) | 0.97 * |
| Femoral neck | 44 (37.5) | 21(35.6) | 11 (37.9) | 12 (37.5) | |
| Time to surgery | |||||
| ≤48 h | 72 (51.7) | 21 (35.6) | 15 (51.7) | 12 (37.5) | 0.32 * |
| >48 h | 48 (48.3) | 38 (64.4) | 14 (48.3) | 20 (62.5) | |
| Type of anesthesia | |||||
| Local | 107 (89.2) | 55 (93.2) | 26 (89.7) | 26 (81.3) | 0.20 * |
| General | 13 (10.8) | 4 (6.8) | 3 (10.3) | 6 (18.7) | |
| ASA class | |||||
| 1–2 | 47 (39.1) | 31 (52.5) | 10 (34.5) | 6 (18.7) | 0.001 ** |
| 3–4 | 73 (60.9) | 28 (47.5) | 19 (65.5) | 26 (81.3) | Tau 0.27 |
| Type of procedure | |||||
| Osteosynthesis | 79 (65.8) | 42 (71.2) | 18 (62.1) | 19 (59.4) | 0.46 * |
| Arthroplasty | 41 (34.2) | 17 (28.8) | 11 (37.9) | 13 (40.6) | |
| Blood transfusion | |||||
| Yes | 31 (25.8) | 10 (16.9) | 9 (31.0) | 12 (37.5) | 0.07 * |
| No | 89 (74.2) | 49 (80.1) | 20 (69.0) | 20 (62.5) | |
| Mean length of surgery (min) | |||||
| 59.4 | 58.2 | 62.9 | 61.6 | 0.49 ** | |
| Mean length of hospital stay (days) | |||||
| 14.1 | 15.2 | 13.2 | 12.8 | 0.54 ** | |
| Mean time from surgery to mobilization (days) | |||||
| 2 | 2.1 | 2.6 | 2.4 | 0.54 ** | |
| Variable | ADL | IADL | ||||||
|---|---|---|---|---|---|---|---|---|
| 3 Months | 6 Months | 3 Months | 6 Months | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender | ||||||||
| Male | 1 | 1 | 1 | 1 | ||||
| Female | 5.79 | 1.35–24.88 * | 2.11 | 0.55–8.04 | 1.96 | 0.36–10.62 | 1.03 | 0.35–3.06 |
| Age | ||||||||
| ≥80 years | 1 | 1 | 1 | 1 | ||||
| <80 years | 2.23 | 0.68–7.05 | 1.23 | 0.40–1.24 | 1.11 | 0.31–3.97 | 4.11 | 1.47–11.48 ** |
| SPMSQ index: | ||||||||
| Cognitive impairment | 1 | 1 | 1 | 1 | ||||
| Intact intellectual functioning | 11.67 | 3.13–23.54 *** | 7.2 | 2.19–22.84 *** | 7.19 | 1.09–27.40 * | 1.2 | 0.48–3.13 |
| Pre-fracture ADL index | 1.13 | 0.63–2.02 | 1.23 | 1.02–3.17 * | ||||
| Pre-fracture IADL score | - | - | - | - | 4 | 1.62–9.73 ** | 1.17 | 1.03–1.40 * |
| R2 | 0.376 | 0.374 | 0.189 | 0.165 | ||||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ganczak, M.; Chrobrowski, K.; Korzeń, M. Predictors of a Change and Correlation in Activities of Daily Living after Hip Fracture in Elderly Patients in a Community Hospital in Poland: A Six-Month Prospective Cohort Study. Int. J. Environ. Res. Public Health 2018, 15, 95. https://doi.org/10.3390/ijerph15010095
Ganczak M, Chrobrowski K, Korzeń M. Predictors of a Change and Correlation in Activities of Daily Living after Hip Fracture in Elderly Patients in a Community Hospital in Poland: A Six-Month Prospective Cohort Study. International Journal of Environmental Research and Public Health. 2018; 15(1):95. https://doi.org/10.3390/ijerph15010095
Chicago/Turabian StyleGanczak, Maria, Krzysztof Chrobrowski, and Marcin Korzeń. 2018. "Predictors of a Change and Correlation in Activities of Daily Living after Hip Fracture in Elderly Patients in a Community Hospital in Poland: A Six-Month Prospective Cohort Study" International Journal of Environmental Research and Public Health 15, no. 1: 95. https://doi.org/10.3390/ijerph15010095





