The Association between Air Pollution and Outpatient and Inpatient Visits in Shenzhen, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Collection for the Hospital Outpatient and Inpatient Visit
- The ratio of zero records was greater or equal to mean of that for all hospitals
- The ratio of outliers (records fall outside mean ±2 standard deviation) was greater or equal to mean ratio of outliers +2 standard deviations
- The coefficient of variation was greater or equal to mean ±2 standard deviations
2.2. Data Collection for Air Pollution and Weather Condition
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Chen, R.; Wang, X.; Meng, X.; Hua, J.; Zhou, Z.; Chen, B.; Kan, H. Communicating air pollution-related health risks to the public: An application of the Air Quality Health Index in Shanghai, China. Environ. Int. 2013, 51, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, M.S.; Burnett, R.T.; Stieb, D.M.; Brophy, J.M.; Daskalopoulou, S.S.; Valois, M.F.; Brook, J.R. Associations between ambient air pollution and daily mortality among elderly persons in Montreal, Quebec. Sci. Total Environ. 2013, 463, 931–942. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Chu, C.; Tan, J.; Cao, J.; Song, W.; Xu, X.; Jiang, C.; Ma, W.; Yang, C.; Chen, B.; et al. Ambient air pollution and hospital admission in Shanghai, China. J. Hazard. Mater. 2010, 181, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Strickland, M.J.; Darrow, L.A.; Klein, M.; Flanders, W.D.; Sarnat, J.A.; Waller, L.A.; Sarnat, S.E.; Mulholland, J.A.; Tolbert, P.E. Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am. J. Respir. Crit. Care Med. 2010, 182, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J.; Slater, D.; Larson, T.V.; Pierson, W.E.; Koenig, J.Q. Particulate air pollution and hospital emergency room visits for asthma in Seattle. Am. Rev. Respir. Dis. 1993, 147, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, E.; Villeneuve, P.J.; Cakmak, S. Air pollution and emergency department visits for asthma in Windsor, Canada. Can. J. Public Health 2012, 103, 4–8. [Google Scholar] [PubMed]
- Schwartz, J.; Morris, R. Air pollution and hospital admissions for cardiovascular disease in Detroit, Michigan. Am. J. Epidemiol. 1995, 142, 23–35. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Tong, S.; Zhang, Y.; Barnett, A.G.; Jia, Y.; Pan, X. The relationship between particulate air pollution and emergency hospital visits for hypertension in Beijing, China. Sci. Total Environ. 2010, 408, 4446–4450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xia, X.; Zhang, A.; Liang, S.; Qi, Q.; Jiang, L.; Ye, Y. The association between air pollution and population health risk for respiratory infection: A case study of Shenzhen, China. Int. J. Environ. Res. Public Health 2017, 14, 950. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Jia, Y.; Pan, X.; Liu, L.; Wichmann, H.E. The association between fine particulate air pollution and hospital emergency room visits for cardiovascular diseases in Beijing, China. Sci. Total Environ. 2009, 407, 4826–4830. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Barnett, A.G.; Zhang, Y.; Tong, S.; Yu, W.; Pan, X. The short-term effect of air pollution on cardiovascular mortality in Tianjin, China: Comparison of time series and case-crossover analyses. Sci. Total Environ. 2010, 409, 300–306. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, J.; Li, W.; Tan, J.; Song, W.; Xu, X.; Jiang, C.; Chen, G.; Chen, R.; Ma, W.; Chen, B.; et al. Association of ambient air pollution with hospital outpatient and emergency room visits in Shanghai, China. Sci. Total Environ. 2009, 407, 5531–5536. [Google Scholar] [CrossRef] [PubMed]
- Lisabeth, L.D.; Escobar, J.D.; Dvonch, J.T.; Sanchez, B.N.; Majersik, J.J.; Brown, D.L.; Smith, M.A.; Morgenstern, L.B. Ambient air pollution and risk for ischemic stroke and transient ischemic attack. Ann. Neurol. 2008, 64, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Oudin, A.; Stromberg, U.; Jakobsson, K.; Stroh, E.; Bjork, J. Estimation of short-term effects of air pollution on stroke hospital admissions in southern Sweden. Neuroepidemiology 2010, 34, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Hagler, G.S.W.; Bergin, M.H.; Salmon, L.G.; Yu, J.Z.; Wan, E.C.H.; Zheng, M.; Zeng, L.M.; Kiang, C.S.; Zhang, Y.H.; Lau, A.K.H. Source areas and chemical composition of fine particulate matter in the Pearl River Delta region of China. Atmos. Environ. 2006, 40, 3802–3815. [Google Scholar] [CrossRef]
- Jahnet, H.J.; Schneider, A.; Breitner, S.; Eißner, R.; Wendisch, M.; Krämer, A. Particulate matter pollution in the megacities of the Pearl River Delta, China—A systematic literature review and health risk assessment. Int. J. Hyg. Environ. Health 2011, 214, 281–295. [Google Scholar] [CrossRef] [PubMed]
- Richter, A.; Burrows, J.P.; Nuess, H.; Granier, C.; Niemeier, U. Increase in tropospheric nitrogen dioxide over China observed from space. Nature 2005, 437, 129–132. [Google Scholar] [CrossRef] [PubMed]
- Tao, Y.B.; Huang, W.; Huang, X.L.; Zhong, L.J.; Lu, S.E.; Li, Y.; Dai, L.Z.; Zhang, Y.H.; Zhu, T. Estimated acute effects of ambient ozone and nitrogen dioxide on mortality in the Pearl River Delta of southern China. Environ. Health Perspect. 2012, 120, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Peel, J.L.; Tolbert, P.E.; Klein, M.; Metzger, K.B.; Flanders, W.D.; Todd, K.; Mulholland, J.A.; Ryan, P.B.; Frumkin, H. Ambient air pollution and respiratory emergency department visits. Epidemiology 2005, 16, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, A.; Stroh, E.; Nihlen, U.; Montnemery, P.; Axmon, A.; Jakobsson, K. Traffic exposure associated with allergic asthma and allergic rhinitis in adults. A cross-sectional study in southern Sweden. Int. J. Health Geogr. 2009, 8, 25. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Wang, W.; Lv, J.; Krafft, T.; Xu, J. Time-series studies on air pollution and daily outpatient visits for allergic rhinitis in Beijing, China. Sci. Total Environ. 2011, 409, 2486–2492. [Google Scholar] [CrossRef] [PubMed]
- Wood, S.N.; Augustin, N.H. GAMs with integrated model selection using penalized regression splines and applications to environmental modelling. Ecol. Model. 2002, 157, 157–177. [Google Scholar] [CrossRef] [Green Version]
- Chan, T.C.; Chen, M.L.; Lin, I.F.; Lee, C.H.; Chiang, P.H.; Wang, D.W.; Chuang, J.H. Spatiotemporal analysis of air pollution and asthma patient visits in Taipei, Taiwan. Int. J. Health Geogr. 2009, 8, 26. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.M.; Thach, T.Q.; Chau, P.Y.; Chan, E.K.; Chung, R.Y.; Ou, C.Q.; Yang, L.; Peiris, J.S.; Thomas, G.N.; Lam, T.H.; et al. Interaction between air pollution and respiratory viruses: Time-series study of daily mortality and hospital admissions in Hong Kong. Res. Rep. Health Eff. Inst. 2010, 154, 283–362. [Google Scholar]
- Li, R.; Jiang, N.; Liu, Q.; Huang, J.; Guo, X.; Liu, F.; Gao, Z. Impact of air pollutants on outpatient visits for acute respiratory outcomes. Int. J. Environ. Res. Public Health 2017, 14, 47. [Google Scholar] [CrossRef] [PubMed]
- Pan, H.H.; Chen, C.T.; Sun, H.L.; Ku, M.S.; Liao, P.F.; Lu, K.H.; Sheu, J.N.; Huang, J.Y.; Pai, J.Y.; Lue, K.H. Comparison of the effects of air pollution on outpatient and inpatient visits for asthma: A population-based study in Taiwan. PLoS ONE 2014, 9, e96190. [Google Scholar] [CrossRef] [PubMed]
- Bell, M.L.; Peng, R.D.; Dominici, F.; Samet, J.M. Emergency hospital admissions for cardiovascular diseases and ambient levels of carbon monoxide: Results for 126 United States urban counties, 1999–2005. Circulation 2009, 120, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Fusco, D.; Forastiere, F.; Michelozzi, P.; Spadea, T.; Ostro, B.; Arca, M.; Perucci, C.A. Air pollution and hospital admissions for respiratory conditions in Rome, Italy. Eur. Respir. J. 2001, 17, 1143–1150. [Google Scholar] [CrossRef] [PubMed]
- Villeneuve, P.J.; Chen, L.; Rowe, B.H.; Coates, F. Outdoor air pollution and emergency department visits for asthma among children and adults: A case-crossover study in northern Alberta, Canada. Environ. Health 2007, 6, 40. [Google Scholar] [CrossRef] [PubMed]
- Hajat, S.; Haines, A.; Goubet, S.A.; Atkinson, R.W.; Anderson, H.R. Association of air pollution with daily GP consultations for asthma and other lower respiratory conditions in London. Thorax 1999, 54, 597–605. [Google Scholar] [CrossRef] [PubMed]
- Santos, U.P.; Terra-Filho, M.; Lin, C.A.; Pereira, L.A.; Vieira, T.C.; Saldiva, P.H.; Braga, A.L. Cardiac arrhythmia emergency room visits and environmental air pollution in Sao Paulo, Brazil. J. Epidemiol. Community Health 2008, 62, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Takenoue, Y.; Kaneko, T.; Miyamae, T.; Mori, M.; Yokota, S. Influence of outdoor NO2 exposure on asthma in childhood: Meta-analysis. Pediatr. Int. 2012, 54, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Winquist, A.; Klein, M.; Tolbert, P.; Flanders, W.D.; Hess, J.; Sarnat, S.E. Comparison of emergency department and hospital admissions data for air pollution time-series studies. Environ. Health 2012, 11, 70. [Google Scholar] [CrossRef] [PubMed]
- Schildcrout, J.S.; Sheppard, L.; Lumley, T.; Slaughter, J.C.; Koenig, J.Q.; Shapiro, G.G. Ambient air pollution and asthma exacerbations in children: An eight-city analysis. Am. J. Epidemiol. 2006, 164, 505–517. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.K.; Chang, S.C.; Lin, C.; Chen, Y.C.; Wang, Y.C. Comparing ozone metrics on associations with outpatient visits for respiratory diseases in Taipei Metropolitan area. Environ. Pollut. 2013, 177, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.S.; Chan, C.C. Effects of air pollution on daily clinic visits for lower respiratory tract illness. Am. J. Epidemiol. 2002, 155, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Slaughter, J.C.; Kim, E.; Sheppard, L.; Sullivan, J.H.; Larson, T.V.; Claiborn, C. Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. J. Expo. Anal. Environ. Epidemiol. 2005, 15, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Ma, G.P.; Zou, B.L.; Xu, Z.C.; Lv, J.C. Association of respiratory diseases outpatient visits and air pollution in a district, Guangzhou: A time-series study. J. Environ. Health 2012, 29, 526–528. [Google Scholar]
| Variable | Mean | Standard Deviation (SD) | Min | Max |
|---|---|---|---|---|
| Hospital admission | ||||
| Outpatient visits | 100,495.42 | 9752.35 | 70,167.00 | 122,731.00 |
| Inpatient visits | 2540.69 | 336.90 | 1756.00 | 3348.00 |
| Air pollutants (µg/m3) | ||||
| SO2 | 8.33 | 2.45 | 4.12 | 21.32 |
| CO | 850.45 | 168.41 | 551.62 | 1408.88 |
| NO2 | 33.36 | 11.50 | 13.67 | 101.58 |
| O3 | 55.53 | 23.56 | 16.00 | 162.53 |
| PM10 | 49.11 | 24.40 | 13.54 | 160.48 |
| PM2.5 | 29.87 | 17.09 | 7.00 | 100.71 |
| Weather conditions | ||||
| Relative Humidity (%) | 71.93 | 11.05 | 28.00 | 93.00 |
| Pressure (hPa) | 1005.97 | 6.45 | 990.60 | 1019.30 |
| Temperature (°C) | 23.96 | 5.24 | 11.90 | 33.00 |
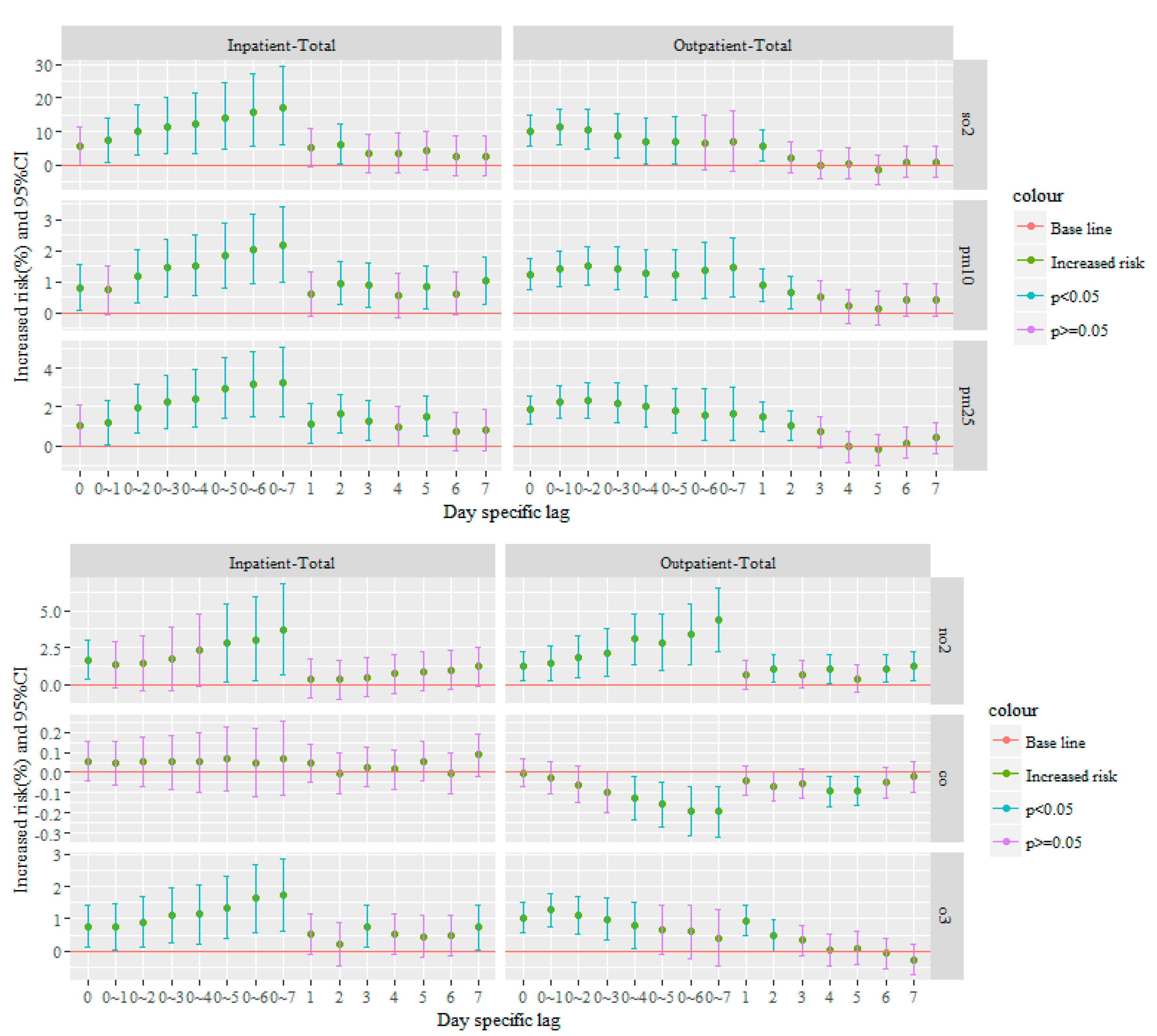
| Lag (Days) | % Changes (95% CI)—Outpatient Visits for All Hospitals | |||||
|---|---|---|---|---|---|---|
| SO2 | CO | NO2 | O3 | PM10 | PM2.5 | |
| 0 | 10.21 (5.75~14.86) | 0 (−0.07~0.07) | 1.21 (0.24~2.19) | 1.03 (0.57~1.50) | 1.24 (0.73~1.75) | 1.85 (1.11~2.59) |
| 1 | 5.87 (1.4~10.54) | −0.04 (−0.11~0.04) | 0.65 (−0.32~1.63) | 0.93 (0.46~1.4) | 0.90 (0.38~1.42) | 1.50 (0.74~2.26) |
| 2 | 2.31 (−2.06~6.88) | −0.07 (−0.14~0.01) | 1.09 (0.14~2.05) | 0.48 (0.01~0.95) | 0.65 (0.14~1.17) | 1.01 (0.26~1.77) |
| 3 | −0.08 (−4.19~0.21) | −0.05 (−0.13~0.02) | 0.68 (−0.27~1.63) | 0.34 (−0.13~0.81) | 0.51 (−0.01~1.03) | 0.69 (−0.08~1.46) |
| 4 | 0.59 (−3.88~5.26) | −0.09 (−0.17~0.02) | 1.06 (0.07~2.06) | 0.04 (−0.45~0.54) | 0.20 (−0.33~0.75) | −0.06 (−0.86~0.74) |
| 5 | −1.55 (−5.79~2.88) | −0.09 (−0.16~0.02) | 0.4 (−0.55~1.35) | 0.09 (−0.41~0.60) | 0.15 (−0.39~0.69) | −0.22 (−1.02~0.58) |
| 6 | 0.98 (−3.38~5.54) | −0.05 (−0.12~0.02) | 1.09 (0.12~2.07) | −0.07 (−0.53~0.40) | 0.4 (−0.12~0.94) | 0.12 (−0.67~0.92) |
| 7 | 0.90 (−3.46~5.47) | −0.02 (−0.09~0.05) | 1.23 (0.28~2.2) | −0.26 (−0.72~0.20) | 0.41 (−0.11~0.93) | 0.4 (−0.39~1.18) |
| 0~1 | 11.48 (6.32~16.89) | −0.02 (−0.1~0.06) | 1.39 (0.23~2.58) | 1.28 (0.76~1.80) | 1.41 (0.84~1.97) | 2.23 (1.41~3.06) |
| 0~2 | 10.62 (4.87~16.69) | −0.06 (−0.15~0.03) | 1.86 (0.46~3.26) | 1.11 (0.53~1.71) | 1.52 (0.90~2.13) | 2.36 (1.45~3.28) |
| 0~3 | 8.61 (2.34~15.26) | −0.1 (−0.2~0) | 2.13 (0.54~3.73) | 0.99 (0.34~1.65) | 1.43 (0.74~2.12) | 2.19 (1.16~3.23) |
| 0~4 | 7.04 (0.30~14.23) | −0.12 (−0.23~0.02) | 3.05 (1.32~4.81) | 0.77 (0.07~1.49) | 1.28 (0.52~2.04) | 2.04 (0.97~3.12) |
| 0~5 | 7.18 (0.46~14.34) | −0.16 (−0.27~0.04) | 2.84 (0.95~4.77) | 0.65 (−0.12~1.42) | 1.23 (0.41~2.05) | 1.81 (0.66~2.97) |
| 0~6 | 6.56 (−1.35~15.11) | −0.19 (−0.31~0.07) | 3.4 (1.37~5.47) | 0.61 (−0.22~1.44) | 1.38 (0.49~2.28) | 1.6 (0.29~2.93) |
| 0~7 | 6.85 (−1.68~16.12) | −0.19 (−0.32~0.07) | 4.38 (2.25~6.56) | 0.41 (−0.46~1.28) | 1.45 (0.50~2.41) | 1.64 (0.24~3.05) |
| % Changes (95% CI)—Inpatient Visits for All Hospitals | ||||||
| 0 | 5.61 (−0.05~11.59) | 0.05 (−0.04~0.15) | 1.66 (0.36~2.98) | 0.77 (0.10~1.43) | 0.80 (0.06~1.54) | 1.06 (−0.02~2.14) |
| 1 | 5.19 (−0.45~11.15) | 0.05 (−0.05~0.14) | 0.4 (−0.88~1.70) | 0.52 (−0.1~1.14) | 0.61 (−0.08~1.31) | 1.13 (0.12~2.15) |
| 2 | 6.11 (0.35~12.20) | 0 (−0.10~0.10) | 0.33 (−1.01~1.68) | 0.2 (−0.48~0.89) | 0.96 (0.26~1.66) | 1.64 (0.62~2.67) |
| 3 | 3.37 (−2.33~9.41) | 0.03 (−0.07~0.13) | 0.47 (−0.83~1.79) | 0.77 (0.13~1.41) | 0.89 (0.18~1.59) | 1.26 (0.23~2.30) |
| 4 | 3.44 (−2.26~9.46) | 0.01 (−0.08~0.11) | 0.72 (−0.58~2.04) | 0.53 (−0.11~1.17) | 0.57 (−0.14~1.27) | 0.95 (−0.07~1.99) |
| 5 | 4.26 (−1.43~10.28) | 0.06 (−0.04~0.1) | 0.87 (−0.42~2.19) | 0.45 (−0.18~1.09) | 0.83 (0.14~1.52) | 1.51 (0.51~2.53) |
| 6 | 2.61 (−3.01~8.56) | 0 (−0.11~0.10) | 0.96 (−0.34~2.28) | 0.49 (−0.15~1.13) | 0.63 (−0.07~1.33) | 0.72 (−0.3~1.75) |
| 7 | 2.59 (−3.09~8.61) | 0.09 (−0.02~0.19) | 1.2 (−0.13~2.55) | 0.73 (0.04~1.43) | 1.02 (0.27~1.78) | 0.79 (−0.27~1.86) |
| 0~1 | 7.29 (0.82~14.18) | 0.05 (−0.06~0.16) | 1.31 (−0.26~2.90) | 0.74 (0.05~1.45) | 0.75 (−0.04~1.53) | 1.19 (0.04~2.34) |
| 0~2 | 10.22 (3.01~17.92) | 0.06 (−0.07~0.18) | 1.44 (−0.41~3.34) | 0.90 (0.14~1.67) | 1.19 (0.34~2.05) | 1.93 (0.68~3.19) |
| 0~3 | 11.48 (3.55~20.01) | 0.05 (−0.08~0.19) | 1.72 (−0.43~3.93) | 1.10 (0.26~1.93) | 1.46 (0.54~2.38) | 2.26 (0.90~3.63) |
| 0~4 | 12.3 (3.62~21.7) | 0.05 (−0.1~0.2) | 2.30 (−0.10~4.76) | 1.14 (0.23~2.05) | 1.54 (0.54~2.54) | 2.42 (0.95~3.91) |
| 0~5 | 14.24 (4.83~24.49) | 0.07 (−0.09~0.23) | 2.77 (0.17~5.43) | 1.34 (0.37~2.32) | 1.83 (0.78~2.90) | 2.97 (1.41~4.55) |
| 0~6 | 15.99 (5.79~27.17) | 0.05 (−0.12~0.22) | 3.04 (0.24~5.92) | 1.63 (0.59~2.67) | 2.05 (0.93~3.19) | 3.18 (1.53~4.86) |
| 0~7 | 17.13 (6.13~29.26) | 0.07 (−0.11~0.25) | 3.66 (0.63~6.77) | 1.70 (0.59~2.84) | 2.20 (1.01~3.41) | 3.27 (1.51~5.07) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Y.; Chen, S.; Xu, J.; Liu, X.; Wu, Y.; Zhou, L.; Cheng, J.; Ma, H.; Zheng, J.; Lin, D.; et al. The Association between Air Pollution and Outpatient and Inpatient Visits in Shenzhen, China. Int. J. Environ. Res. Public Health 2018, 15, 178. https://doi.org/10.3390/ijerph15020178
Liu Y, Chen S, Xu J, Liu X, Wu Y, Zhou L, Cheng J, Ma H, Zheng J, Lin D, et al. The Association between Air Pollution and Outpatient and Inpatient Visits in Shenzhen, China. International Journal of Environmental Research and Public Health. 2018; 15(2):178. https://doi.org/10.3390/ijerph15020178
Chicago/Turabian StyleLiu, Yachuan, Shanen Chen, Jian Xu, Xiaojian Liu, Yongsheng Wu, Lin Zhou, Jinquan Cheng, Hanwu Ma, Jing Zheng, Denan Lin, and et al. 2018. "The Association between Air Pollution and Outpatient and Inpatient Visits in Shenzhen, China" International Journal of Environmental Research and Public Health 15, no. 2: 178. https://doi.org/10.3390/ijerph15020178




