A Cross-Sectional Study of Viral Hepatitis Perception among Residents from Southeast and North Regions of Brazil
Abstract
:1. Introduction
2. Methods
2.1. Study Population
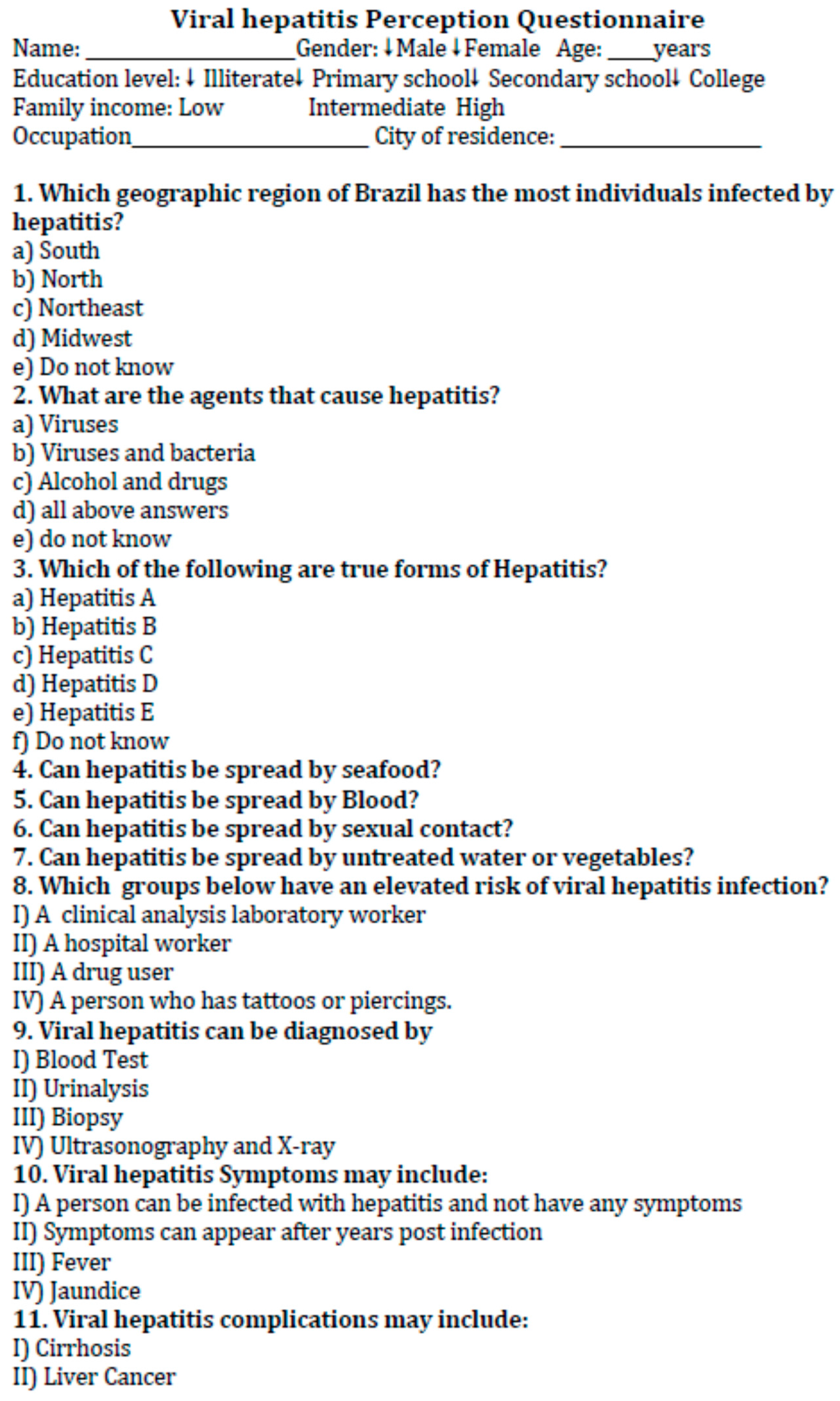
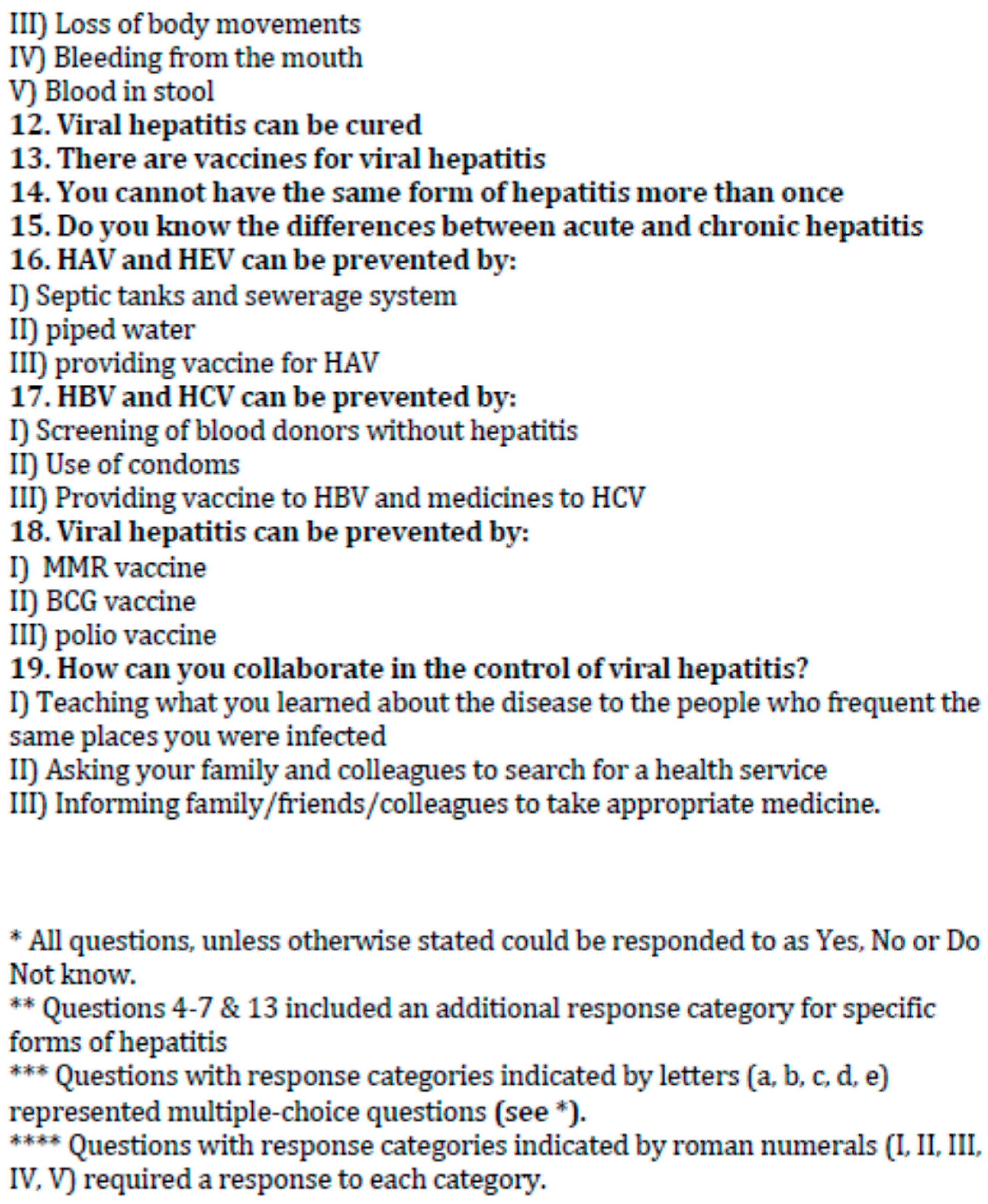
2.2. Questionnaire
3. Results
3.1. Demographic Characteristics
3.2. Viral Hepatitis Perception in Manaus City
3.3. Viral Hepatitis Perception in Rio de Janeiro City
3.4. Perception about Viral Hepatitis According to Demographic Characteristics
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Focaccia, R. Tratado de Hepatites Virais e Doenças Associadas, 3rd ed.; Atheneu: São Paulo, Brazil, 2013; p. 1320. [Google Scholar]
- Ogholikhan, S.; Schwarz, K.B. Hepatitis vaccines. Vaccines 2016, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Health Topics: Hepatitis. 2017. Available online: http://www.who.int/topics/hepatitis/en/ (accessed on 4 October 2017).
- Ministry of Health. Boletim Epidemiológico—Hepatites Virais. 2017. Available online: http://www.aids.gov.br/pt-br/pub/2017/boletim-epidemiologico-de-hepatites-virais-2017 (accessed on 29 August 2017).
- Pereira, L.M.; Martelli, C.M.; Merchán-Haman, E.; Montarroyos, U.R.; Braga, M.C.; de Lima, M.L.; Cardoso, M.R.; Turchi, M.D.; Costa, M.A.; de Alencar, L.C.; et al. Population-based multicentric survey of hepatitis B infection and risk factor differences among three regions in Brazil. Am. J. Trop. Med. Hyg. 2009, 81, 240–247. [Google Scholar] [PubMed]
- Pereira, L.M.; Martelli, C.M.; Moreira, R.C.; Merchan-Hamman, E.; Stein, A.T.; Cardoso, M.R.; Figueiredo, G.M.; Montarroyos, U.R.; Braga, C.; Turchi, M.D.; et al. Prevalence and risk factors of Hepatitis C virus infection in Brazil, 2005 through 2009: A cross-sectional study. BMC Infect. Dis. 2013, 13, 60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Echevarría, J.M.; González, J.E.; Lewis-Ximenez, L.L.; Dos Santos, D.R.; Munné, M.S.; Pinto, M.A.; Pujol, F.H.; Rodríguez-Lay, L.A. Hepatitis E virus infection in Latin America: A review. J. Med. Virol. 2013, 85, 1037–1045. [Google Scholar] [CrossRef] [PubMed]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. 2015. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld (accessed on 31 August 2017).
- Yang, W.T.; Wu, L.W.; Tseng, T.C.; Chen, C.L.; Yang, H.C.; Su, T.H.; Wang, C.C.; Kuo, S.F.; Liu, C.H.; Chen, P.J.; et al. Hepatitis B Surface Antigen Loss and Hepatocellular Carcinoma Development in Patients with Dual Hepatitis B and C Infection. Medicine 2016, 95, e2995. [Google Scholar] [CrossRef] [PubMed]
- Villar, L.M.; Cruz, H.M.; Barbosa, J.R.; Bezerra, C.S.; Portilho, M.M.; Scalioni, L.P. Update on hepatitis B and C virus diagnosis. World J. Virol. 2015, 4, 323–342. [Google Scholar] [CrossRef] [PubMed]
- Ataei, B.; Shirani, K.; Alavian, S.M.; Ataie, M. Evaluation of knowledge and practice of hairdressers in women’s beauty salons in Isfahan about hepatitis B, hepatitis C, and AIDS in 2010 and 2011. Hepat. Mon. 2013, 13, e6215. [Google Scholar] [CrossRef] [PubMed]
- Wu, E.; Chen, X.; Guan, Z.; Cao, C.; Rao, H.; Feng, B. A comparative study of patients’ knowledge about hepatitis C in the United States and in urban and rural China. Hepatol. Int. 2015, 9, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Mesfin, Y.M.; Kibret, K.T. Assessment of Knowledge and Practice towards Hepatitis B among Medical and Health Science Students in Haramaya University, Ethiopia. PLoS ONE 2013, 8, e79642. [Google Scholar] [CrossRef] [PubMed]
- Noman, U.H.; Hassali, M.A.; Shafie, A.A.; Saleem, F.; Farooqui, M.; Aljadhey, A. A cross sectional assessment of knowledge, attitude and practice towards Hepatitis B among healthy population of Quetta, Pakistan. BMC Public Health 2012, 12, 692. [Google Scholar] [CrossRef]
- Strong, C.; Hur, K.; Kim, F.; Pan, J.; Tran, S.; Juon, R.S. Sociodemographic characteristics, knowledge and prevalence of viral hepatitis infection among Vietnamese Americans at community screenings. J. Immigr. Minor. Health 2015, 17, 298–301. [Google Scholar] [CrossRef] [PubMed]
- Instituto Brasileiro de Geografia e Estatística. Nota Técnica Estimativas da População dos Municípios Brasileiros Com Data de Referência em 1° de Julho de 2014. Available online: http://www.ibge.gov.br/home/presidencia/noticias/pdf/analise_estimativas_2014.pdf (accessed on 8 May 2017).
- Saleh, D.A.; Amr, S.; Jillson, I.A.; Wang, J.H.; Khairy, W.A.; Loffredo, C.A. Knowledge and perceptions of hepatitis C infection and pesticides use in two rural villages in Egypt. BMC Public Health 2014, 14, 501. [Google Scholar] [CrossRef] [PubMed]
- Patra, S.; Kumar, A.; Trivedi, S.S.; Puri, M.; Sarin, S.K. Maternal and fetal outcomes in pregnant women with acute hepatitis E virus infection. Ann. Intern. Med. 2007, 147, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Amodio, E.; Di Benedetto, M.A.; Gennaro, L.; Maida, C.M.; Romano, N. Knowledge, attitudes and risk of HIV, HBV and HCV infections in hairdressers of Palermo city (South Italy). Eur. J. Public Health 2010, 20, 433–437. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, M.A.; Rizvi, F.; Ashraf, M.Z.; Niazi, M. Knowledge and practices of barbers regarding hepatitis B and hepatitis C in BahraKahu, Islamabad–Pakistan. Rawal Med. J. 2010, 35, 37–40. [Google Scholar]
- Jokhio, A.H.; Bhatti, T.A.; Memon, M.S. Knowledge, attitudes and practices of barbers about hepatitis B and C transmission in Hyderabad, Pakistan. East. Mediterr. Health J. 2010, 16, 1079–1084. [Google Scholar] [PubMed]
- Cui, W.; Sun, Y.; Xu, A.; Gao, R.; Gong, L.; Zhang, L.; Jiang, M. Hepatitis E seroprevalence and related risk factors among seafood processing workers: A cross-sectional survey in Shandong Province, China. Int. J. Infect. Dis. 2016, 49, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Polo, D.; Varela, M.F.; Romalde, J.L. Detection and quantification of hepatitis A virus and norovirus in Spanish authorized shellfish harvesting areas. Int. J. Food Microbiol. 2015, 193, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Komatsu, H.; Inui, A.; Sogo, T.; Tateno, A.; Shimokawa, R.; Fujisawa, T. Tears from children with chronic hepatitis B virus (HBV) infection Are infectious vehicles of HBV transmission: Experimental transmission of HBV by tears, using mice with chimeric human livers. J. Infect. Dis. 2012, 206, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Geng, Y.; Zhao, C.; Huang, W.; Harrison, T.J.; Zhang, H.; Geng, K.; Wang, Y. Detection and assessment of infectivity of hepatitis E virus in urine. J. Hepatol. 2016, 64, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Tourinho, R.S.; Amado, L.A.; Villar, L.M.; Sampaio, D.V.; Moraes, A.C.; Rodrigues do Ó, K.M. Importance of the cutoff ratio for detecting antibodies against hepatitis A virus in oral fluids by enzyme immunoassay. J. Virol. Methods 2011, 173, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Ye, Z.; Xu, L.; Zhang, B.; Liang, H.; Feng, Z.; Liu, S.; Shi, W. Diagnostic value of urine HBV DNA for hepatitis B virus-associated glomerulonephritis. Nan Fang Yi Ke Da Xue Bao 2014, 34, 1705–1706. [Google Scholar]
| Items | Total (287) |
|---|---|
| n (%) | |
| Local | |
| Rio de Janeiro | 153 (53.3) |
| Manaus | 134 (46.7) |
| Gender | |
| Female | 173 (60.3) |
| Male | 114 (39.7) |
| Age groups (years) | |
| 18–21 | 34 (11.8) |
| 21–30 | 115 (40.1) |
| 31–40 | 66 (23.0) |
| 41–50 | 41 (14.3) |
| >50 | 29 (10.1) |
| Not declared | 2 (0.7) |
| Education | |
| Illiterate | 26 (9.1) |
| Primary school | 42 (14.6) |
| Secondary school | 162 (56.4) |
| College | 56 (19.5) |
| Not declared | 1 (0.4) |
| Family income | |
| Low | 157 (54.7) |
| Intermediate | 57 (19.9) |
| High | 42 (14.6) |
| Not declared | 31 (10.8) |
| Statement | Number (%) | |||||
|---|---|---|---|---|---|---|
| Manaus (n = 134) | Rio de Janeiro (n = 153) | |||||
| Correct | Incorrect | Do Not Know | Correct | Incorrect | Do Not Know | |
| General information | ||||||
| There is hepatitis A | 94 (70.1) | 11 (8.2) | 29 (21.6) | 120 (78.4) | 33 (21.6) | 0 (0) |
| There is hepatitis B | 94 (70.1) | 11 (8.2) | 29 (21.6) | 132 (86.3) | 21 (13.7) | 0 (0.0) |
| There is hepatitis C | 94 (70.1) | 11 (8.2) | 29 (21.6) | 114 (74.5) | 39 (25.5) | 0 (0.0) |
| There is hepatitis D | 56 (41.8) | 49 (36.6) | 29 (21.6) | 41 (26.8) | 112 (73.2) | 0 (0.0) |
| There is hepatitis E | 48 (35.8) | 57 (42.6) | 29 (21.6) | 50 (32.7) | 103 (67.3) | 0 (0.0) |
| Viral hepatitis can be cured | 44 (32.8) | 34 (25.4) | 56 (41.8) | 93 (60.8) | 28 (18.3) | 32 (20.9) |
| There are vaccines for viral hepatitis | 67 (50.0) | 18 (13.4) | 49 (36.6) | 111 (72.5) | 6 (3.9) | 36 (23.5) |
| There are vaccines for HAV and HBV | 16 (11.9) | 4 (3.0) | 114 (85.1) | 25 (16.4) | 12 (7.8) | 116 (75.8) |
| You cannot have the same hepatitis more than once | 50 (37.3) | 22 (16.4) | 62 (46.3) | 62 (40.5) | 39 (25.5) | 52 (34.0) |
| There are differences between acute and chronic hepatitis | 22 (16.4) | 112 (83.6) | 0 (0.0) | 47 (30.7) | 104 (68.0) | 2 (1.3) |
| You can help to control hepatitis by teaching what you have learned to other individuals who frequent the same place where you were infected | 129 (96.3) | 2 (1.5) | 3 (2.2) | 120 (78.4) | 15 (9.8) | 18 (11.8) |
| You can help to control hepatitis by informing family and colleagues to search for a health service | 125 (93.3) | 5 (3.7) | 4 (3.0) | 127 (83.0) | 8 (5.2) | 18 (11.8) |
| You can help to control hepatitis by informing family and colleagues to buy and take appropriate medicine to inactivate the virus | 66 (49.3) | 46 (34.3) | 22 (16.4) | 84 (54.9) | 51 (33.3) | 18 (11.8) |
| Diagnosis | ||||||
| Hepatitis can be diagnosed by blood test | 123 (91.8) | 5 (3.7) | 6 (4.5) | 146 (95.4) | 6 (3.9) | 1 (0.7) |
| Hepatitis cannot be diagnosed by Urinalysis | 59 (44.0) | 59 (44.0) | 16 (11.9) | 110 (71.9) | 41 (26.8) | 2 (1.3) |
| Hepatitis can be diagnosed by Biopsy | 24 (17.9) | 94 (70.1) | 16 (11.9) | 100 (65.4) | 50 (32.7) | 3 (2.0) |
| Hepatitis cannot be diagnosed by X-ray | 20 (14.9) | 91 (67.9) | 23 (17.2) | 140 (91.5) | 12 (7.8) | 1 (0.7) |
| Symptoms | ||||||
| Absence of symptoms | 64 (47.8) | 54 (40.3) | 16 (11.9) | 86 (56.2) | 21 (13.7) | 46 (30.1) |
| Symptoms can appear years after infection | 62 (46.3) | 55 (41.0) | 17 (12.7) | 62 (40.5) | 69 (45.1) | 22 (14.4) |
| Fever can be a symptom | 102 (76.1) | 17 (12.7) | 15 (11.2) | 101 (66.0) | 30 (19.6) | 22 (14.4) |
| Jaundice can be a symptom | 122 (91.0) | 2 (1.5) | 10 (7.5) | 117 (76.5) | 15 (9.8) | 21 (13.7) |
| Questions | Number (%) | |||||
|---|---|---|---|---|---|---|
| Manaus (n = 134) | Rio de Janeiro (n = 153) | |||||
| Correct | Incorrect | Do Not Know | Correct | Incorrect | Do Not Know | |
| Hepatitis can be spread by | ||||||
| Seafood | 35 (26.1) | 96 (71.6) | 3 (2.2) | 61 (39.9) | 74 (48.4) | 18 (11.8) |
| HAV and HEV can be transmitted by seafood | 7 (5.2) | 4 (3.0) | 123 (91.8) | 3 (2.0) | 3 (2.0) | 147 (96.0) |
| Blood | 107 (79.9) | 27 (20.1) | 0 (0.0) | 135 (88.2) | 14 (9.2) | 4 (2.6) |
| HBV, HCV, and HDV can be transmitted by blood | 18 (13.4) | 13 (9.7) | 103 (76.9) | 24 (15.7) | 7 (4.6) | 122 (79.7) |
| Sexual contact | 94 (70.1) | 39 (29.1) | 1 (0.7) | 116 (75.8) | 30 (19.6) | 7 (4.6) |
| HBV, HCV, and HDV can be transmitted by sexual contact | 19 (14.2) | 10 (7.5) | 105 (78.3) | 23 (15.0) | 4 (2.6) | 126 (82.4) |
| Water or vegetables without treatment | 84 (62.7) | 50 (37.3) | 0 (0.0) | 128 (83.7) | 17 (11.1) | 7 (4.6) |
| HAV and HEV can be transmitted by water or vegetables without treatment | 12 (8.9) | 6 (4.5) | 116 (86.6) | 17 (11.1) | 10 (6.5) | 126 (82.4) |
| People at risk of acquiring hepatitis | ||||||
| Drug users | 63 (47.0) | 71 (53.0) | 0 (0.0) | 130 (85.0) | 18 (11.8) | 5 (3.3) |
| People with tattoos or piercings | 67 (50.0) | 67 (50.0) | 0 (0.0) | 120 (78.4) | 28 (18.3) | 5 (3.3) |
| Hospital Employees | 117 (87.3) | 17 (12.7) | 0 (0.0) | 117 (76.5) | 31 (20.3) | 5 (3.3) |
| Clinical laboratory workers | 118 (88.1) | 16 (11.9) | 0 (0.0) | 110 (71.9) | 38 (24.8) | 5 (3.3) |
| Complications | ||||||
| Hepatitis can lead to cirrhosis | 115 (85.8) | 3 (2.2) | 16 (11.9) | 104 (68.0) | 19 (12.4) | 30 (19.6) |
| Hepatitis can lead to liver cancer | 107 (79.9) | 15 (11.2) | 12 (9.0) | 89 (58.2) | 33 (21.6) | 31 (20.3) |
| Hepatitis cannot lead to loss of body movements | 68 (50.7) | 23 (17.2) | 43 (32.1) | 83 (54.2) | 38 (24.8) | 32 (20.9) |
| Hepatitis cannot lead to bleeding from mouth | 33 (24.6) | 66 (49.3) | 35 (26.1) | 78 (51.0) | 45 (29.4) | 30 (19.6) |
| Hepatitis cannot lead to blood in stool | 25 (18.7) | 65 (48.5) | 44 (32.8) | 62 (40.5) | 61 (39.9) | 30 (19.6) |
| Prevention | ||||||
| HAV and HEV can be prevented by septic tanks and sewerage systems | 116 (86.6) | 6 (4.5) | 12 (9.0) | 100 (65.4) | 25 (16.3) | 28 (18.3) |
| HAV and HEV can be prevented by piped water | 114 (85.1) | 9 (6.7) | 11 (8.2) | 106 (69.3) | 19 (12.4) | 28 (18.3) |
| HAV and HEV can be prevented by providing vaccine for HAV | 108 (80.6) | 15 (11.2) | 11 (8.2) | 97 (63.4) | 28 (18.3) | 28 (18.3) |
| HBV and HCV can be prevented by selecting blood donors not infected by hepatitis | 111 (82.8) | 7 (5.2) | 16 (11.9) | 108 (70.6) | 20 (13.1) | 25 (16.3) |
| HBV and HCV can be prevented by use of condoms | 105 (78.4) | 10 (7.5) | 19 (14.2) | 113 (73.9) | 16 (10.5) | 24 (15.7) |
| HBV and HCV can be prevented by providing vaccine and drugs | 104 (77.6) | 9 (6.7) | 21 (15.7) | 118 (77.1) | 10 (6.5) | 25 (16.3) |
| Vaccine to measles, mumps, and rubella (MMR) cannot prevent hepatitis | 39 (29.1) | 58 (43.3) | 37 (27.6) | 59 (38.6) | 71 (46.4) | 23 (15.0) |
| Vaccine to BCG cannot prevent hepatitis | 67 (50.0) | 24 (17.9) | 43 (32.1) | 110 (71.9) | 18 (11.8) | 25 (16.3) |
| Vaccine to POLIO cannot prevent hepatitis | 79 (59.0) | 17 (12.7) | 38 (28.4) | 115 (75.2) | 15 (9.8) | 23 (15.0) |
| Item | Mean Score (SD) | Knowledge Levels * n (%) | p-Value | |||
|---|---|---|---|---|---|---|
| Very Weak | Weak | Intermediate | Desirable | |||
| Gender | ||||||
| Male | 25.1 (7.7) | 31 (43.05) | 33 (38.4) | 27 (39.1) | 23 (38.3) | 0.617 |
| Female | 25.4 (6.9) | 41 (56.95) | 53 (61.6) | 42(60.9) | 37 (61.7) | |
| Age group (years) | ||||||
| ≤20 | 23.7 (8.0) | 13 (18.1) | 7 (8.1) | 8 (11.6) | 6 (10.0) | 0.673 |
| 21–30 | 25.0 (7.5) | 24 (33.3) | 46 (53.5) | 23 (33.3) | 24 (40.0) | |
| 31–40 | 27.2 (6.4) | 12 (16.6) | 16 (18.6) | 17 (24.6) | 21 (35.0) | |
| 41–50 | 25.0 (7.1) | 13 (18.1) | 8 (9.3) | 12 (17.4) | 8 (13.3) | |
| ≥51 | 24.0 (6.0) | 10 (13.9) | 9 (10.5) | 9 (13.1) | 1 (1.7) | |
| Education | ||||||
| Illiterate | 23.3 (7.0) | 8 (11.1) | 10 (11.8) | 8 (11.6) | 0 (0.0) | <0.001 |
| Primary School | 22.9 (7.2) | 13 (18.1) | 15 (17.6) | 11 (15.9) | 3 (5.0) | |
| Secondary School | 24.8 (7.2) | 45 (62.5) | 50 (58.8) | 36 (52.2) | 31 (51.7) | |
| Graduated | 29.1 (6.0) | 6 (8.3) | 10 (11.8) | 14 (20.3) | 26 (43.3) | |
| Family Income | 0.001 | |||||
| Low | 24.5 (7.2) | 42 (71.2) | 52 (85.3) | 40 (62.6) | 23 (40.4) | |
| Intermediate | 26.1 (7.1) | 13 (22.0) | 1 (1.6) | 12 (18.7) | 16 (28.0) | |
| High | 29.2 (5.9) | 4 (6.8) | 8 (13.1) | 12 (18.7) | 18 (31.6) | |
| City | 0.001 | |||||
| Rio de Janeiro | 26.3 (7.3) | 31 (43.1) | 39 (45.3) | 41 (59.4) | 42 (70.0) | |
| Manaus | 24.1 (7.0) | 41 (56.9) | 47 (54.7) | 28 (40.6) | 18 (30.0) | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cruz, H.M.; De Paula, V.S.; Villar, L.M. A Cross-Sectional Study of Viral Hepatitis Perception among Residents from Southeast and North Regions of Brazil. Int. J. Environ. Res. Public Health 2018, 15, 189. https://doi.org/10.3390/ijerph15020189
Cruz HM, De Paula VS, Villar LM. A Cross-Sectional Study of Viral Hepatitis Perception among Residents from Southeast and North Regions of Brazil. International Journal of Environmental Research and Public Health. 2018; 15(2):189. https://doi.org/10.3390/ijerph15020189
Chicago/Turabian StyleCruz, Helena Medina, Vanessa Salete De Paula, and Livia Melo Villar. 2018. "A Cross-Sectional Study of Viral Hepatitis Perception among Residents from Southeast and North Regions of Brazil" International Journal of Environmental Research and Public Health 15, no. 2: 189. https://doi.org/10.3390/ijerph15020189




