Incidence Rates of and Mortality after Hip Fracture among German Nursing Home Residents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Study Population
2.2. Hip Fractures
2.3. Selection of Controls
2.4. Statistical Analyses
3. Results
3.1. Baseline Characteristics
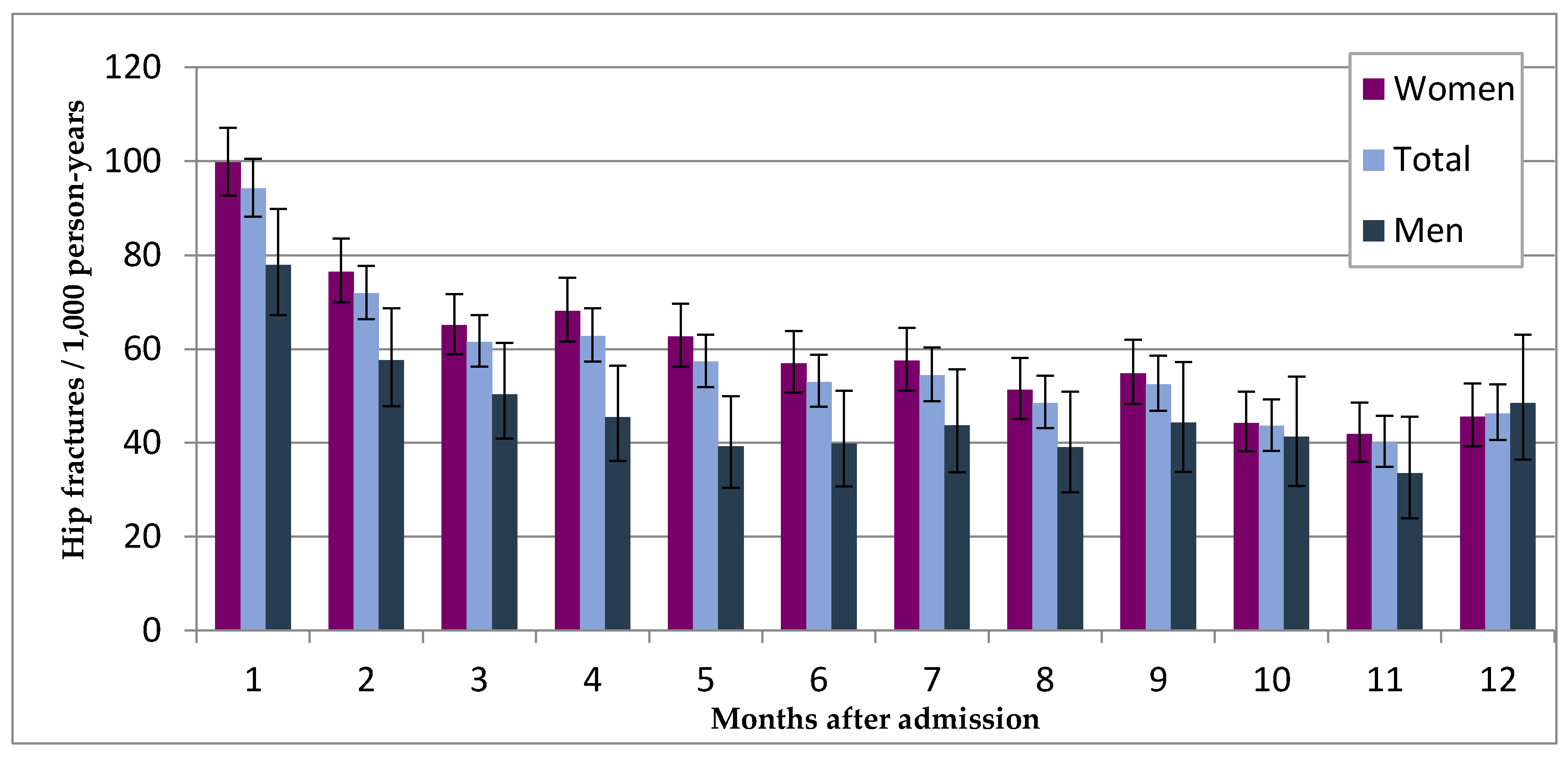
3.2. Incidence of Hip Fracture
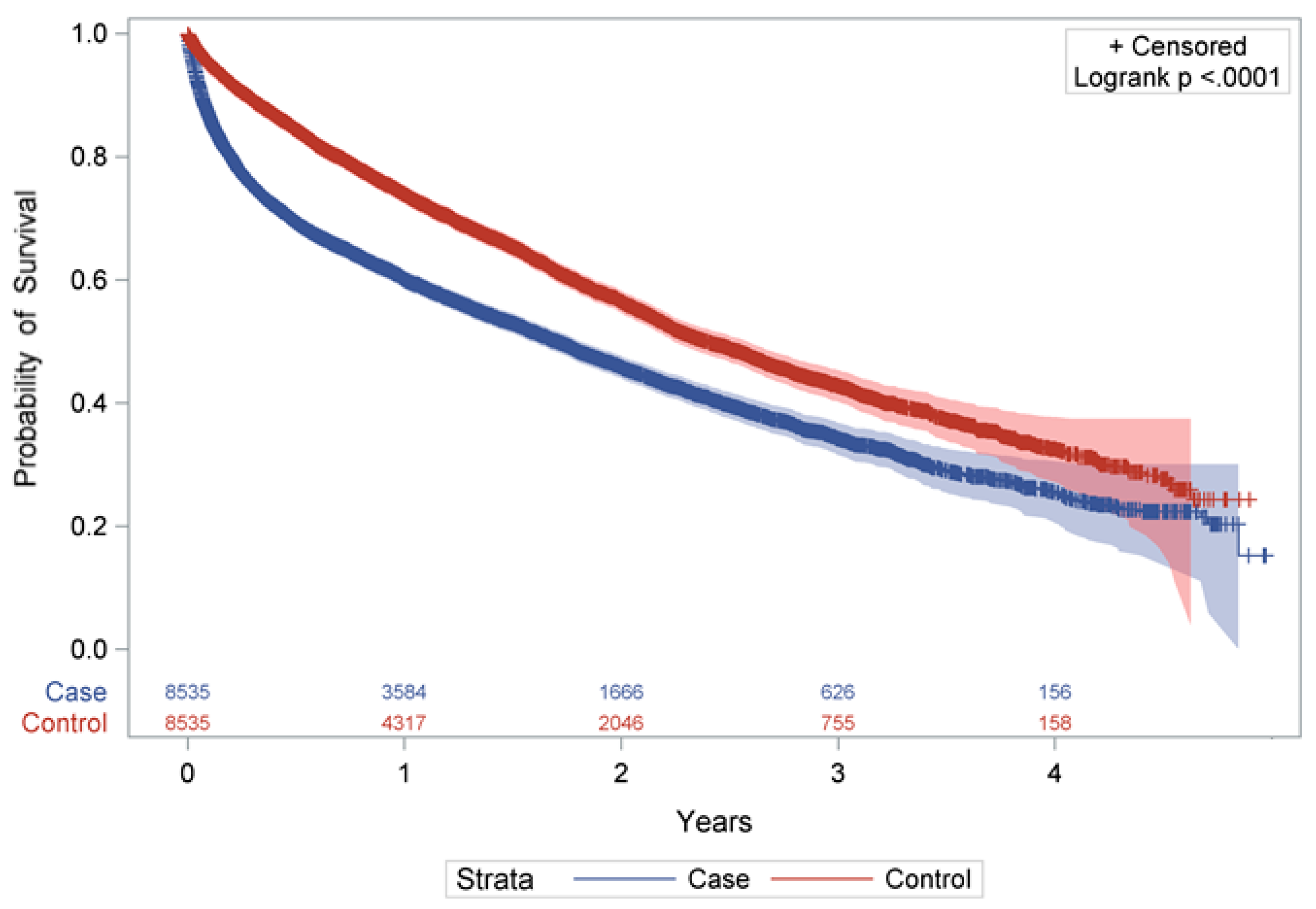
3.3. Mortality after Hip Fracture Compared to Controls
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Women | Men | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N† | PY | IR ☐ (95% CI) | N† | PY | IR ☐ (95% CI) | N† | PY | IR ☐ (95% CI) | ||
| Months after admission | ||||||||||
| 1 | 732 | 7345 | 99.7 (92.6–107.1) | 190 | 2439 | 77.9 (67.2–89.8) | 922 | 9784 | 94.2 (88.2–100.5) | |
| 2 | 509 | 6652 | 76.5 (70.0–83.5) | 123 | 2137 | 57.6 (47.8–68.7) | 632 | 8789 | 71.9 (66.4–77.7) | |
| 3 | 403 | 6194 | 65.1 (58.9–71.7) | 98 | 1947 | 50.3 (40.9–61.3) | 501 | 8140 | 61.5 (56.3–67.2) | |
| 4 | 398 | 5842 | 68.1 (61.6–75.2) | 82 | 1803 | 45.5 (36.2–56.5) | 480 | 7645 | 62.8 (57.3–68.7) | |
| 5 | 348 | 5546 | 62.7 (56.3–69.7) | 66 | 1681 | 39.3 (30.4–50.0) | 414 | 7227 | 57.3 (51.9–63.1) | |
| 6 | 301 | 5286 | 56.9 (50.7–63.8) | 63 | 1578 | 39.9 (30.7–51.1) | 364 | 6864 | 53.0 (47.7–58.8) | |
| 7 | 291 | 5059 | 57.5 (51.1–64.5) | 65 | 1488 | 43.7 (33.7–55.7) | 356 | 6546 | 54.4 (48.9–60.3) | |
| 8 | 248 | 4837 | 51.3 (45.1–58.1) | 55 | 1406 | 39.1 (29.5–50.9) | 303 | 6244 | 48.5 (43.2–54.3) | |
| 9 | 254 | 4632 | 54.8 (48.3–62.0) | 59 | 1331 | 44.3 (33.8–57.2) | 313 | 5963 | 52.5 (46.8–58.6) | |
| 10 | 196 | 4433 | 44.2 (38.2–50.9) | 52 | 1260 | 41.3 (30.8–54.1) | 248 | 5693 | 43.6 (38.3–49.3) | |
| 11 | 178 | 4245 | 41.9 (36.0–48.6) | 40 | 1195 | 33.5 (23.9–45.6) | 218 | 5440 | 40.1 (34.9–45.8) | |
| 12 | 185 | 4054 | 45.6 (39.3–52.7) | 55 | 1134 | 48.5 (36.5–63.1) | 240 | 5189 | 46.3 (40.6–52.5) | |
References
- Bevölkerung Deutschlands Bis 2060-13. Koordinierte Bevölkerungsvorausberechnung. Available online: https://www.destatis.de/DE/Publikationen/Thematisch/Bevoelkerung/VorausberechnungBevoelkerung/BevoelkerungDeutschland2060Presse5124204159004.pdf?__blob=publicationFile (accessed on 6 December 2017).
- Gesundheit älterer Menschen. Available online: https://www.bzga.de/themenschwerpunkte/gesundheitaelterermenschen/ (accessed on 6 December 2017).
- WHO. Burden of major musculoscletal conditions. Bull. World Health Organ. 2003, 81, 646–656. [Google Scholar]
- Sugarman, J.R.; Connell, F.A.; Hansen, A.; Helgerson, S.D.; Jessup, M.C.; Lee, H. Hip fracture incidence in nursing home residents and community-dwelling older people, Washington State, 1993–1995. J. Am. Geriatr. Soc. 2002, 50, 1638–1643. [Google Scholar] [CrossRef] [PubMed]
- Ooms, M.E.; Vlasman, P.; Lips, P.; Nauta, J.; Bouter, L.M.; Valkenburg, H.A. The incidence of hip fractures in independent and institutionalized elderly people. Osteoporos. Int. 1994, 4, 6–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Finsterwald, M.; Sidelnikov, E.; Orav, E.J.; Dawson-Hughes, B.; Theiler, R.; Egli, A.; Platz, A.; Simmen, H.P.; Meier, C.; Grob, D.; et al. Gender-specific hip fracture risk in community-dwelling and institutionalized seniors age 65 years and older. Osteoporos. Int. 2014, 25, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Rapp, K.; Becker, C.; Cameron, I.D.; Klenk, J.; Kleiner, A.; Bleibler, F.; Konig, H.H.; Buchele, G. Femoral fracture rates in people with and without disability. Age Ageing 2012, 41, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Rapp, K.; Becker, C.; Lamb, S.E.; Icks, A.; Klenk, J. Hip fractures in institutionalized elderly people: Incidence rates and excess mortality. J. Bone Miner. Res. 2008, 23, 1825–1831. [Google Scholar] [CrossRef] [PubMed]
- Berry, S.D.; Lee, Y.; Zullo, A.R.; Kiel, D.P.; Dosa, D.; Mor, V. Incidence of hip fracture in U.S. nursing homes. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 1230–1234. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, F.; Glaeske, G. Incidence of hip fracture in Germany–person-related analysis of health insurance population. Gesundheitswesen 2006, 68, 161–164. [Google Scholar] [CrossRef] [PubMed]
- Mann, E.; Meyer, G.; Haastert, B.; Icks, A. Comparison of hip fracture incidence and trends between Germany and Austria 1995–2004: An epidemiological study. BMC Public Health 2010, 10, 46. [Google Scholar] [CrossRef] [PubMed]
- Icks, A.; Arend, W.; Becker, C.; Rapp, K.; Jungbluth, P.; Haastert, B. Incidence of hip fractures in Germany, 1995–2010. Arch. Osteoporos. 2013, 8, 140. [Google Scholar] [CrossRef] [PubMed]
- Icks, A.; Haastert, B.; Wildner, M.; Becker, C.; Meyer, G. Hip fracture incidence in Germany: Analysis of the National Hospital Discharge Registry 2004. Dtsch. Med. Wochenschr. 2008, 133, 125–128. [Google Scholar] [CrossRef] [PubMed]
- Walter, L.C.; Lui, L.Y.; Eng, C.; Covinsky, K.E. Risk of hip fracture in disabled community-living older adults. J. Am. Geriatr. Soc. 2003, 51, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Rapp, K.; Lamb, S.E.; Klenk, J.; Kleiner, A.; Heinrich, S.; Konig, H.H.; Nikolaus, T.; Becker, C. Fractures after nursing home admission: Incidence and potential consequences. Osteoporos. Int. 2009, 20, 1775–1783. [Google Scholar] [CrossRef] [PubMed]
- Berry, S.D.; Samelson, E.J.; Bordes, M.; Broe, K.; Kiel, D.P. Survival of aged nursing home residents with hip fracture. J. Gerontol. A Biol. Sci. Med. Sci. 2009, 64, 771–777. [Google Scholar] [CrossRef] [PubMed]
- Neuman, M.D.; Silber, J.H.; Magaziner, J.S.; Passarella, M.A.; Mehta, S.; Werner, R.M. Survival and functional outcomes after hip fracture among nursing home residents. JAMA Intern. Med. 2014, 174, 1273–1280. [Google Scholar] [CrossRef] [PubMed]
- Center, J.R.; Nguyen, T.V.; Schneider, D.; Sambrook, P.N.; Eisman, J.A. Mortality after all major types of osteoporotic fracture in men and women: An observational study. Lancet 1999, 353, 878–882. [Google Scholar] [CrossRef]
- Daten zum Gesundheitswesen: Versicherte 2017. Available online: https://www.vdek.com/presse/daten/b_versicherte.html (accessed on 10 November 2017).
- Daly, L. Simple SAS macros for the calculation of exact binomial and Poisson confidence limits. Comput. Biol. Med. 1992, 22, 351–361. [Google Scholar] [CrossRef]
- Daly, L.E. Confidence limits made easy: Interval estimation using a substitution method. Am. J. Epidemiol. 1998, 147, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Kleinbaum, D.G.; Klein, M. Survival Analyses: A Self-Learning Text, 2nd ed.; Springer: New York, NY, USA, 2005. [Google Scholar]
- Norton, R.; Campbell, A.J.; Reid, I.R.; Butler, M.; Currie, R.; Robinson, E.; Gray, H. Residential status and risk of hip fracture. Age Ageing 1999, 28, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Brennan nee Saunders, J.; Johansen, A.; Butler, J.; Stone, M.; Richmond, P.; Jones, S.; Lyons, R.A. Place of residence and risk of fracture in older people: A population-based study of over 65-year-olds in Cardiff. Osteoporos. Int. 2003, 14, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Rudman, I.W.; Rudman, D. High rate of fractures for men in nursing homes. Am. J. Phys. Med. Rehabil. 1989, 68, 2–5. [Google Scholar] [CrossRef] [PubMed]
- Chandler, J.M.; Zimmerman, S.I.; Girman, C.J.; Martin, A.R.; Hawkes, W.; Hebel, J.R.; Sloane, P.D.; Holder, L.; Magaziner, J. Low bone mineral density and risk of fracture in white female nursing home residents. JAMA 2000, 284, 972–977. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.S.; Sambrook, P.N.; Simpson, J.M.; Cameron, I.D.; Cumming, R.G.; Seibel, M.J.; Lord, S.R.; March, L.M. Risk factors for hip fracture among institutionalised older people. Age Ageing 2009, 38, 429–434. [Google Scholar] [CrossRef] [PubMed]
- Brauer, C.A.; Coca-Perraillon, M.; Cutler, D.M.; Rosen, A.B. Incidence and mortality of hip fractures in the United States. JAMA 2009, 302, 1573–1579. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Oyama, M.; Takahashi, S.; Yoshizawa, Y.; Kobayashi, R.; Oshiki, R.; Saito, T.; Tsuchiya, Y. Fracture incidence in nursing homes in Japan. Osteoporos. Int. 2010, 21, 797–803. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, F.; Boeschen, D.; Dorks, M.; Herget-Rosenthal, S.; Petersen, J.; Schmiemann, G. Renal insufficiency and medication in nursing home residents. A cross-sectional study (IMREN). Dtsch. Arztebl. Int. 2016, 113, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, F.; Kaduszkiewicz, H.; Glaeske, G.; van den Bussche, H.; Koller, D. Prevalence of dementia in nursing home and community-dwelling older adults in Germany. Aging Clin. Exp. Res. 2014, 26, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Harris, I.A.; Yong, S.; McEvoy, L.; Thorn, L. A prospective study of the effect of nursing home residency on mortality following hip fracture. ANZ J. Surg. 2010, 80, 447–450. [Google Scholar] [CrossRef] [PubMed]
- Leibson, C.L.; Tosteson, A.N.; Gabriel, S.E.; Ransom, J.E.; Melton, L.J. Mortality, disability, and nursing home use for persons with and without hip fracture: A population-based study. J. Am. Geriatr. Soc. 2002, 50, 1644–1650. [Google Scholar] [CrossRef] [PubMed]
- Roche, J.J.; Wenn, R.T.; Sahota, O.; Moran, C.G. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: Prospective observational cohort study. BMJ 2005, 331, 1374. [Google Scholar] [CrossRef] [PubMed]
- Forsen, L.; Sogaard, A.J.; Meyer, H.E.; Edna, T.; Kopjar, B. Survival after hip fracture: Short- and long-term excess mortality according to age and gender. Osteoporos. Int. 1999, 10, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Empana, J.P.; Dargent-Molina, J.; Breart, G. Effect of hip fracture on mortality in elderly women: The EPIDOS prospective study. J. Am. Geriatr. Soc. 2004, 52, 685–690. [Google Scholar] [CrossRef] [PubMed]
- Wehren, L.E.; Hawkes, W.G.; Orwig, D.L.; Hebel, J.R.; Zimmerman, S.I.; Magaziner, J. Gender differences in mortality after hip fracture: The role of infection. J. Bone Miner. Res. 2003, 18, 2231–2237. [Google Scholar] [CrossRef] [PubMed]
- Farahmand, B.Y.; Michaelsson, K.; Ahlbom, A.; Ljunghall, S.; Baron, J.A.; Swedish Hip Fracture Study, G. Survival after hip fracture. Osteoporos. Int. 2005, 16, 1583–1590. [Google Scholar] [CrossRef] [PubMed]
- Handoll, H.H.; Farrar, M.J.; McBirnie, J.; Tytherleigh-Strong, G.; Milne, A.A.; Gillespie, W.J. Heparin, low molecular weight heparin and physical methods for preventing deep vein thrombosis and pulmonary embolism following surgery for hip fractures. Cochrane Database Syst. Rev. 2002, CD000305. [Google Scholar] [CrossRef] [PubMed]
- Lonnroos, E.; Kautiainen, H.; Karppi, P.; Hartikainen, S.; Kiviranta, I.; Sulkava, R. Incidence of second hip fractures. A population-based study. Osteoporos. Int. 2007, 18, 1279–1285. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, F.; Icks, A. Structural differences between health insurance funds and their impact on health services research: Results from the Bertelsmann health-care monitor. Gesundheitswesen 2012, 74, 291–297. [Google Scholar] [CrossRef] [PubMed]
| Men | Women | IRR Women/Men (95% CI) | |||||
|---|---|---|---|---|---|---|---|
| N † | PY | IR ☐ (95% CI) | N † | PY | IR ☐ (95% CI) | ||
| Age (years) | |||||||
| 65–69 | 54 | 2440 | 22.1 (16.6–28.9) | 128 | 4074 | 31.4 (26.2–37.4) | 1.42 (1.04–1.96) |
| 70–74 | 116 | 4627 | 25.1 (20.7–30.1) | 332 | 10,158 | 32.7 (29.3–36.4) | 1.30 (1.06–1.62) |
| 75–79 | 188 | 6222 | 30.2 (26.0–34.9) | 698 | 16,949 | 41.2 (38.2–44.4) | 1.36 (1.16–1.60) |
| 80–84 | 364 | 8568 | 42.5 (38.2–47.1) | 1448 | 28,733 | 50.4 (47.8–53.1) | 1.19 (1.06–1.33) |
| 85–89 | 470 | 8887 | 52.9 (48.2–57.9) | 2497 | 42,418 | 58.9 (56.6–61.2) | 1.11 (1.01–1.23) |
| 90–94 | 282 | 4493 | 62.8 (55.7–70.5) | 1555 | 24,518 | 63.4 (60.3–66.7) | 1.01 (0.89–1.15) |
| ≥95 | 64 | 962 | 66.6 (51.3–85.0) | 341 | 5540 | 61.5 (55.2–68.4) | 0.92 (0.71–1.21) |
| Level of care | |||||||
| 0/I | 948 | 21,060 | 45.0 (42.2–48.0) | 4937 | 89,880 | 54.9 (53.4–56.5) | 1.22 (1.14–1.31) |
| II | 538 | 12,852 | 41.9 (38.4–45.6) | 1909 | 37,214 | 51.3 (49.0–53.7) | 1.22 (1.11–1.35) |
| III | 52 | 2286 | 22.7 (17.0–29.8) | 153 | 5296 | 28.9 (24.5–33.8) | 1.27 (0.93–1.75) |
| Total | 1538 | 36,198 | 42.5 (40.4–44.7) | 6999 | 132,390 | 52.9 (51.6–54.1) | 1.24 (1.18–1.32) |
| Women | Men | Total | ||||
|---|---|---|---|---|---|---|
| Cases | Controls | Cases | Controls | Cases | Controls | |
| Mortality in % (95% CI) | ||||||
| 0.5 year | 27.6 | 14.3 | 44.3 | 21.3 | 30.6 | 15.6 |
| (26.6–28.7) | (13.5–15.2) | (41.7–46.8) | (19.9–23.6) | (29.6–31.7) | (14.8–16.4) | |
| 1 year | 36.7 | 24.1 | 54.3 | 35.4 | 39.9 | 26.1 |
| (35.5–38.0) | (23.0–25.2) | (51.7–57.0) | (32.9–38.1) | (38.8–41.1) | (25.1–27.1) | |
| 2 years | 51.2 | 40.6 | 67.4 | 57.1 | 54.1 | 43.5 |
| (49.8–52.6) | (39.2–42.0) | (64.6–70.2) | (54.0–60.3) | (52.8–55.4) | (42.2–44.8) | |
| 3 years | 63.1 | 54.4 | 78.1 | 70.8 | 65.8 | 57.2 |
| (61.5–64.8) | (52.6–56.1) | (74.9–81.2) | (67.2–74.4) | (64.3–67.3) | (55.6–58.8) | |
| 4 years | 71.7 | 65.1 | 88.2 | 78.3 | 74.6 | 67.4 |
| (69.6–73.9) | (62.7–67.7) | (83.7–91.9) | (73.8–82.6) | (72.7–76.5) | (65.3–69.6) | |
| Women (HR (95% CI)) | Men (HR (95% CI)) | Combined (HR (95% CI)) | |
|---|---|---|---|
| Cases vs. Controls | |||
| x 1–2 months | 2.65 (2.37–2.99) | 3.34 (2.78–4.01) | 2.82 (2.57–3.11) |
| x 3–4 months | 1.92 (1.65–2.23) | 2.07 (1.58–2.72) | 1.96 (1.72–2.23) |
| x 5–6 months | 1.48 (1.24–1.76) | 1.35 (0.96–1.92) | 1.46 (1.25–1.70) |
| x 7–12 months | 1.11 (0.98–1.26) | 1.05 (0.83–1.33) | 1.10 (0.98–1.22) |
| x >12 months | 1.05 (0.96–1.14) | 0.94 (0.78–1.13) | 1.03 (0.95–1.11) |
| Sex (men vs. women) | - | - | 1.72 (1.62–1.81) |
| Age | |||
| 65–74 years | 1 | 1 | 1 |
| 75–84 years | 1.34 (1.17–1.53) | 1.50 (1.24–1.82) | 1.40 (1.25–1.56) |
| 85–94 years | 1.89 (1.66–2.15) | 2.06 (1.71–2.47) | 1.95 (1.76–2.17) |
| ≥95 years | 2.70 (2.30–3.16) | 3.08 (2.36–4.04) | 2.82 (2.47–3.23) |
| Level of care | |||
| 0/I | 1 | 1 | 1 |
| II | 1.23 (1.17–1.30) | 1.22 (1.11–1.35) | 1.12 (1.17–1.29) |
| III | 1.74 (1.50–2.03) | 1.31 (1.02–1.69) | 1.60 (1.40–1.82) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jacobs, H.; Zeeb, H.; Hoffmann, F. Incidence Rates of and Mortality after Hip Fracture among German Nursing Home Residents. Int. J. Environ. Res. Public Health 2018, 15, 289. https://doi.org/10.3390/ijerph15020289
Jacobs H, Zeeb H, Hoffmann F. Incidence Rates of and Mortality after Hip Fracture among German Nursing Home Residents. International Journal of Environmental Research and Public Health. 2018; 15(2):289. https://doi.org/10.3390/ijerph15020289
Chicago/Turabian StyleJacobs, Hannes, Hajo Zeeb, and Falk Hoffmann. 2018. "Incidence Rates of and Mortality after Hip Fracture among German Nursing Home Residents" International Journal of Environmental Research and Public Health 15, no. 2: 289. https://doi.org/10.3390/ijerph15020289






