Empathy Variation in General Practice: A Survey among General Practitioners in Denmark
Abstract
:1. Introduction
2. Methods
2.1. Survey
2.2. Sample Selection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Morse, J.M.; Anderson, G.; Bottorff, J.L.; Yonge, O.; O’Brien, B.; Solberg, S.M.; McIlveen, K.H. Exploring empathy: A conceptual fit for nursing practice? Image J. Nurs. Scholarsh. 1992, 24, 273–280. [Google Scholar] [CrossRef]
- Caspi, A.; Silva, P.A. Temperamental Qualities at Age Three Predict Personality Traits in Young Adulthood: Longitudinal Evidence from a Birth Cohort. Child Dev. 1995, 66, 486–498. [Google Scholar] [CrossRef] [PubMed]
- McDonald, N.M.; Messinger, D.S. The development of empathy: How, when, and why. In Free Will, Emotions, and Moral Actions: Philosophy and Neuroscience in Dialogue; Acerbi, A., Lombo, J.A., Sanguinetti, J.J., Eds.; IF-Press: Rome, Italy, 2011. [Google Scholar]
- Roberts, B.W.; DelVecchio, W.F. The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychol. Bull. 2000, 126, 3–25. [Google Scholar] [CrossRef] [PubMed]
- Derksen, F.; Bensing, J.; Kuiper, S.; van Meerendonk, M.; Lagro-Janssen, A. Empathy: What does it mean for GPs? A qualitative study. Fam. Pract. 2015, 32, 94–100. [Google Scholar] [CrossRef] [PubMed]
- Derksen, F.; Olde Hartman, T.C.; van Dijk, A.; Plouvier, A.; Bensing, J.; Lagro-Janssen, A. Consequences of the presence and absence of empathy during consultations in primary care: A focus group study with patients. Patient Educ. Couns. 2017, 100, 987–993. [Google Scholar] [CrossRef] [PubMed]
- Derksen, F.; Bensing, J.; Lagro-Janssen, A. Effectiveness of empathy in general practice: A systematic review. Br. J. Gen. Pract. 2013, 63, e76–e84. [Google Scholar] [CrossRef] [PubMed]
- Mercer, S.W.; Higgins, M.; Bikker, A.M.; Fitzpatrick, B.; McConnachie, A.; Lloyd, S.M.; Little, P.; Watt, G.C. General Practitioners’ Empathy and Health Outcomes: A Prospective Observational Study of Consultations in Areas of High and Low Deprivation. Ann. Fam. Med. 2016, 14, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Thirioux, B.; Birault, F.; Jaafari, N. Empathy Is a Protective Factor of Burnout in Physicians: New Neuro-Phenomenological Hypotheses Regarding Empathy and Sympathy in Care Relationship. Front. Psychol. 2016, 7, 763. [Google Scholar] [CrossRef] [PubMed]
- Howick, J.; Steinkopf, L.; Ulyte, A.; Roberts, N.; Meissner, K. How empathic is your healthcare practitioner? A systematic review and meta-analysis of patient surveys. BMC Med. Educ. 2017, 17, 136. [Google Scholar] [CrossRef] [PubMed]
- Derksen, F.; Olde Hartman, T.; Bensing, J.; Lagro-Janssen, A. Empathy in general practice-the gap between wishes and reality: Comparing the views of patients and physicians. Fam. Pract. 2017. [Google Scholar] [CrossRef] [PubMed]
- Gleichgerrcht, E.; Decety, J. Empathy in Clinical Practice: How Individual Dispositions, Gender, and Experience Moderate Empathic Concern, Burnout, and Emotional Distress in Physicians. PLoS ONE 2013, 8, e61526. [Google Scholar] [CrossRef] [PubMed]
- Heje, H.N.; Olesen, F.; Vedsted, P. Patients’ assessment of general practitioners. Association with type of practice. Ugeskr. Laeger 2010, 172, 1119–1126. [Google Scholar] [PubMed]
- Konrath, S.H.; O’Brien, E.H.; Hsing, C. Changes in Dispositional Empathy in American College Students over Time: A Meta-Analysis. Pers. Soc. Psychol. Rev. 2011, 15, 180–198. [Google Scholar] [CrossRef] [PubMed]
- Twenge, J.M.; Campbell, S.M. Generational differences in psychological traits and their impact on the workplace. J. Manag. Psychol. 2008, 23, 862–877. [Google Scholar] [CrossRef]
- Hojat, M.; Vergare, M.J.; Maxwell, K.; Brainard, G.; Herrine, S.K.; Isenberg, G.A.; Veloski, J.; Gonnella, J.S. The devil is in the third year: A longitudinal study of erosion of empathy in medical school. Acad. Med. 2009, 84, 1182–1191. [Google Scholar] [CrossRef] [PubMed]
- Kelm, Z.; Womer, J.; Walter, J.K.; Feudtner, C. Interventions to cultivate physician empathy: A systematic review. BMC Med. Educ. 2014, 14, 219. [Google Scholar] [CrossRef] [PubMed]
- Hojat, M.; Axelrod, D.; Spandorfer, J.; Mangione, S. Enhancing and sustaining empathy in medical students. Med. Teach. 2013, 35, 996–1001. [Google Scholar] [CrossRef] [PubMed]
- Mercer, S.W.; Reynolds, W.J. Empathy and quality of care. Br. J. Gen. Prac. 2002, 52, S9–S12. [Google Scholar]
- Hojat, M.; Gonnella, J.S.; Nasca, T.J.; Mangione, S.; Vergare, M.; Magee, M. Physician empathy: Definition, components, measurement, and relationship to gender and specialty. Am. J. Psychiatry 2002, 159, 1563–1569. [Google Scholar] [CrossRef] [PubMed]
- Neumann, M.; Scheffer, C.; Tauschel, D.; Lutz, G.; Wirtz, M.; Edelhäuser, F. Physician empathy: Definition, outcome-relevance and its measurement in patient care and medical education. GMS Z. Fur Med. Ausbild. 2012, 29, Doc11. [Google Scholar]
- Kataoka, H.U.; Koide, N.; Hojat, M.; Gonnella, J.S. Measurement and correlates of empathy among female Japanese physicians. BMC Med. Educ. 2012, 12, 48. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.H.; Li, H.H.; Wu, C.M.; Wang, P.C. The influence of personality traits on nurses’ job satisfaction in Taiwan. Int. Nurs. Rev. 2010, 57, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Foulkrod, K.H.; Field, C.; Brown, C.V. Trauma surgeon personality and job satisfaction: Results from a national survey. Am. Surg. 2010, 76, 422–427. [Google Scholar] [PubMed]
- Hojat, M.; Mangione, S.; Nasca, T.J.; Cohen, M.J.M.; Gonnella, J.S.; Erdmann, J.B.; Veloski, J.J.; Magee, M. The Jefferson scale of physician empathy: Development and Preliminary psychometric data. Educ. Psychol. Meas. 2001, 61, 349–365. [Google Scholar] [CrossRef]
- Hojat, M.; Gonnella, J.S.; Mangione, S.; Nasca, T.J.; Veloski, J.J.; Erdmann, J.B.; Callahan, C.A.; Magee, M. Empathy in medical students as related to academic performance, clinical competence and gender. Med. Educ. 2002, 36, 522–527. [Google Scholar] [CrossRef] [PubMed]
- Hojat, M.; Zuckerman, M.; Magee, M.; Mangione, S.; Nasca, T.; Vergare, M.; Gonnella, J.S. Empathy in medical students as related to specialty interest, personality, and perceptions of mother and father. Pers. Individ. Differ. 2005, 39, 1205–1215. [Google Scholar] [CrossRef]
- Andersen, C.M. The Association between Attachment and Delay in the Diagnosis of Cancer in Primary Care; Aarhus University: Aarhus, Denmark, 2015. [Google Scholar]
- Di Lillo, M.; Cicchetti, A.; Lo Scalzo, A.; Taroni, F.; Hojat, M. The Jefferson Scale of Physician Empathy: Preliminary psychometrics and group comparisons in Italian physicians. Acad. Med. 2009, 84, 1198–1202. [Google Scholar] [CrossRef] [PubMed]
- Suh, D.H.; Hong, J.S.; Lee, D.H.; Gonnella, J.S.; Hojat, M. The Jefferson Scale of Physician Empathy: A preliminary psychometric study and group comparisons in Korean physicians. Med. Teach. 2012, 34, e464–e468. [Google Scholar] [CrossRef] [PubMed]
- Chaitoff, A.; Sun, B.; Windover, A.; Bokar, D.; Featherall, J.; Rothberg, M.B.; Misra-Hebert, A.D. Associations Between Physician Empathy, Physician Characteristics, and Standardized Measures of Patient Experience. Acad. Med. 2017, 92, 1464–1471. [Google Scholar] [CrossRef] [PubMed]
- Sun, B.; Luo, Z.; Zhang, W.; Li, W.; Li, X. Age-related differences in affective and cognitive empathy: Self-report and performance-based evidence. Neuropsychol. Dev. Cogn. Sect. B Aging Neuropsychol. Cogn. 2017, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Shariat, S.V.; Eshtad, E.; Ansari, S. Empathy and its correlates in Iranian physicians: A preliminary psychometric study of the Jefferson Scale of Physician Empathy. Med. Teach. 2010, 32, e417–e421. [Google Scholar] [CrossRef] [PubMed]
- Noyes, R.; Kukoyi, O.A.; Longley, S.L.; Langbehn, D.R.; Stuart, S.P. Effects of continuity of care and patient dispositional factors on the physician-patient relationship. Ann. Clin. Psychiatry 2011, 23, 180–185. [Google Scholar] [PubMed]
- Gray, D.P.; Evans, P.; Sweeney, K.; Lings, P.; Seamark, D.; Seamark, C.; Dixon, M.; Bradley, N. Towards a theory of continuity of care. J. R. Soc. Med. 2003, 96, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Yuguero, O.; Ramon Marsal, J.; Esquerda, M.; Vivanco, L.; Soler-Gonzalez, J. Association between low empathy and high burnout among primary care physicians and nurses in Lleida, Spain. Eur. J. Gen. Pract. 2017, 23, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Lelorain, S.; Sultan, S.; Zenasni, F.; Catu-Pinault, A.; Jaury, P.; Boujut, E.; Rigal, L. Empathic concern and professional characteristics associated with clinical empathy in French general practitioners. Eur. J. Gen. Pract. 2013, 19, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Soncini, F.; Silvestrini, G.; Poscia, A.; Ciorba, V.; Conti, A.; Murru, C.; Rinaldi, A.; Zoccali, A.; Azzolini, E.; Bandini, C.B.L.; et al. Public Health Physicians and Empathy. Are we really empathic? The Jefferson Scale applied to Italian resident doctors in Public Health Francesco Soncini. Eur. J. Public Health 2013, 23 (Suppl. 1), ckt124.068. [Google Scholar] [CrossRef]
- Gerdes, K.E.; Segal, E. Importance of empathy for social work practice: Integrating new science. Soc. Work 2011, 56, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Fortney, L.; Luchterhand, C.; Zakletskaia, L.; Zgierska, A.; Rakel, D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: A pilot study. Ann. Fam. Med. 2013, 11, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.; Norbeck, T.; Price, G.; Libby, R.; Jones, P. 2016 Survey of America’s Physicians: Practice Patterns & Perspectives; The Physicians Foundation: Dallas, TX, USA, 2016. [Google Scholar]
- Shanafelt, T.D. Enhancing meaning in work: A prescription for preventing physician burnout and promoting patient-centered care. JAMA 2009, 302, 1338–1340. [Google Scholar] [CrossRef] [PubMed]
- Ahrweiler, F.; Neumann, M.; Goldblatt, H.; Hahn, E.G.; Scheffer, C. Determinants of physician empathy during medical education: Hypothetical conclusions from an exploratory qualitative survey of practicing physicians. BMC Med. Educ. 2014, 14, 122. [Google Scholar] [CrossRef] [PubMed]
- Cummings, S.M.; Savitz, L.A.; Konrad, T.R. Reported response rates to mailed physician questionnaires. Health Serv. Res. 2001, 35, 1347–1355. [Google Scholar] [PubMed]
- Lin, H.-C.; Xirasagar, S.; Laditka, J.N. Patient perceptions of service quality in group versus solo practice clinics. Int. J. Qual. Health Care 2004, 16, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Søgaard, V. Operationalisering af Landdistriktsbegrebet. Available online: http://static.sdu.dk/mediafiles/E/B/F/%7BEBF22F13-17ED-41D9-AF4D-100BB39A9DCE%7DCLFReport9landdistriktsbegrebet.pdf (accessed on 1 March 2018).
- Rabe-Hesketh, S.; Skrondal, A. Multilevel and Longitudinal Modeling Using Stata, 3rd ed.; Taylor & Francis: Abingdon, UK, 2012. [Google Scholar]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Krasner, M.S.; Epstein, R.M.; Beckman, H.; Suchman, A.L.; Chapman, B.; Mooney, C.J.; Quill, T.E. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 2009, 302, 1284–1293. [Google Scholar] [CrossRef] [PubMed]
- Ster, M.P.; Selic, P. Intended Career Choice in Family Medicine in Slovenia: An Issue of Gender, Family Background or Empathic Attitudes in Final Year Medical Students? Mater. Socio-Med. 2017, 29, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Wündrich, M.; Schwartz, C.; Feige, B.; Lemper, D.; Nissen, C.; Voderholzer, U. Empathy training in medical students—A randomized controlled trial. Med. Teach. 2017, 39, 1096–1098. [Google Scholar] [CrossRef] [PubMed]
- Asuero, A.M.; Queralto, J.M.; Pujol-Ribera, E.; Berenguera, A.; Rodriguez-Blanco, T.; Epstein, R.M. Effectiveness of a mindfulness education program in primary health care professionals: A pragmatic controlled trial. J. Contin. Educ. Health Prof. 2014, 34, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Teding van Berkhout, E.; Malouff, J.M. The efficacy of empathy training: A meta-analysis of randomized controlled trials. J. Couns. Psychol. 2016, 63, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Richter, D.; Kunzmann, U. Age differences in three facets of empathy: Performance-based evidence. Psychol. Aging 2011, 26, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.D.; Hasan, O.; Dyrbye, L.N.; Sinsky, C.; Satele, D.; Sloan, J.; West, C.P. Changes in Burnout and Satisfaction with Work-Life Balance in Physicians and the General US Working Population Between 2011 and 2014. Mayo Clin. Proc. 2015, 90, 1600–1613. [Google Scholar] [CrossRef] [PubMed]
- Wieck, C.; Kunzmann, U. Age differences in empathy: Multidirectional and context-dependent. Psychol. Aging 2015, 30, 407–419. [Google Scholar] [CrossRef] [PubMed]
- Grosseman, S.; Novack, D.H.; Duke, P.; Mennin, S.; Rosenzweig, S.; Davis, T.J.; Hojat, M. Residents’ and standardized patients’ perspectives on empathy: Issues of agreement. Patient Educ. Couns. 2014, 96, 22–28. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, E.; Konrath, S.H.; Gruhn, D.; Hagen, A.L. Empathic concern and perspective taking: Linear and quadratic effects of age across the adult life span. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2013, 68, 168–175. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.E.; Voyer, D. Sex differences in the ability to recognise non-verbal displays of emotion: A meta-analysis. Cognit. Emot. 2014, 28, 1164–1195. [Google Scholar] [CrossRef] [PubMed]
- Christov-Moore, L.; Simpson, E.A.; Coudé, G.; Grigaityte, K.; Iacoboni, M.; Ferrari, P.F. Empathy: Gender effects in brain and behavior. Neurosci. Biobehav. Rev. 2014, 46 Pt 4, 604–627. [Google Scholar] [CrossRef] [PubMed]
- Wood, W.; Eagly, A.H. A cross-cultural analysis of the behavior of women and men: Implications for the origins of sex differences. Psychol. Bull. 2002, 128, 699–727. [Google Scholar] [CrossRef] [PubMed]
- Zeldow, P.B.; Daugherty, S.R. The stability and attitudinal correlates of warmth and caring in medical students. Med. Educ. 1987, 21, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Bethlehem, R.A.I.; Allison, C.; van Andel, E.M.; Coles, A.I.; Neil, K.; Baron-Cohen, S. Does empathy predict altruism in the wild? Soc. Neurosci. 2017, 12, 743–750. [Google Scholar] [CrossRef] [PubMed]
- Persson, B.N.; Kajonius, P.J. Empathy and universal values explicated by the empathy-altruism hypothesis. J. Soc. Psychol. 2016, 156, 610–619. [Google Scholar] [CrossRef] [PubMed]
- Kjeldmand, D.; Holmstrom, I.; Rosenqvist, U. Balint training makes GPs thrive better in their job. Patient Educ. Couns. 2004, 55, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, K.M.; Andersen, J.S.; Søndergaard, J. General Practice and Primary Health Care in Denmark. J. Am. Board Fam. Med. 2012, 25 (Suppl. 1), S34–S38. [Google Scholar] [CrossRef] [PubMed]
- Glaser, K.M.; Markham, F.W.; Adler, H.M.; McManus, P.R.; Hojat, M. Relationships between scores on the Jefferson Scale of physician empathy, patient perceptions of physician empathy, and humanistic approaches to patient care: A validity study. Med. Sci. Monit. 2007, 13, Cr291–Cr294. [Google Scholar] [PubMed]
- Chen, D.C.R.; Pahilan, M.E.; Orlander, J.D. Comparing a Self-Administered Measure of Empathy with Observed Behavior among Medical Students. J. Gen. Intern. Med. 2010, 25, 200–202. [Google Scholar] [CrossRef] [PubMed]
- Baez, S.; Flichtentrei, D.; Prats, M.; Mastandueno, R.; García, A.M.; Cetkovich, M.; Ibáñez, A. Men, women … who cares? A population-based study on sex differences and gender roles in empathy and moral cognition. PLoS ONE 2017, 12, e0179336. [Google Scholar] [CrossRef] [PubMed]
- Hojat, M.; Spandorfer, J.; Louis, D.Z.; Gonnella, J.S. Empathic and Sympathetic Orientations toward Patient Care: Conceptualization, Measurement, and Psychometrics. Acad. Med. 2011, 86, 989–995. [Google Scholar] [CrossRef] [PubMed]
- Youssef, F.F.; Nunes, P.; Sa, B.; Williams, S. An exploration of changes in cognitive and emotional empathy among medical students in the Caribbean. Int. J. Med. Educ. 2014, 5, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, R. Empirical research on empathy in medicine—A critical review. Patient Educ. Couns. 2009, 76, 307–322. [Google Scholar] [CrossRef] [PubMed]
- Wolf, O.T.; Schulte, J.M.; Drimalla, H.; Hamacher-Dang, T.C.; Knoch, D.; Dziobek, I. Enhanced emotional empathy after psychosocial stress in young healthy men. Stress 2015, 18, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Manczak, E.M.; DeLongis, A.; Chen, E. Does Empathy Have a Cost? Diverging Psychological and Physiological Effects within Families. Health Psychol. 2016, 35, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Brady, C.; Bambury, R.M.; O’Reilly, S. Empathy and the wounded healer: A mixed-method study of patients and doctors views on empathy. Ir. Med. J. 2015, 108, 125–126. [Google Scholar] [PubMed]
- Fiona, E.F.; Karen, J.R.; Michael, F.H.; Gordon, J.T.; Jane, S.; Jenny, S.; Brian, R. Experiencing “The Other Side”: A Study of Empathy and Empowerment in General Practitioners Who Have Been Patients. Qual. Health Res. 2009, 19, 1580–1588. [Google Scholar]
| Stratum | % of GPs in Population | # of GPs per Strata |
|---|---|---|
| Non-partnership practice and rural municipality | 5.91% | 70 |
| Non-partnership practice and heterogeneous municipality | 7.83% | 93 |
| Non-partnership practice and urban municipality | 15.21% | 182 |
| Partnership practice and rural municipality | 15.65% | 187 |
| Partnership practice and heterogeneous municipality | 32.91% | 394 |
| Partnership practice and urban municipality | 22.49% | 269 |
| Total | 100% | 1195 |
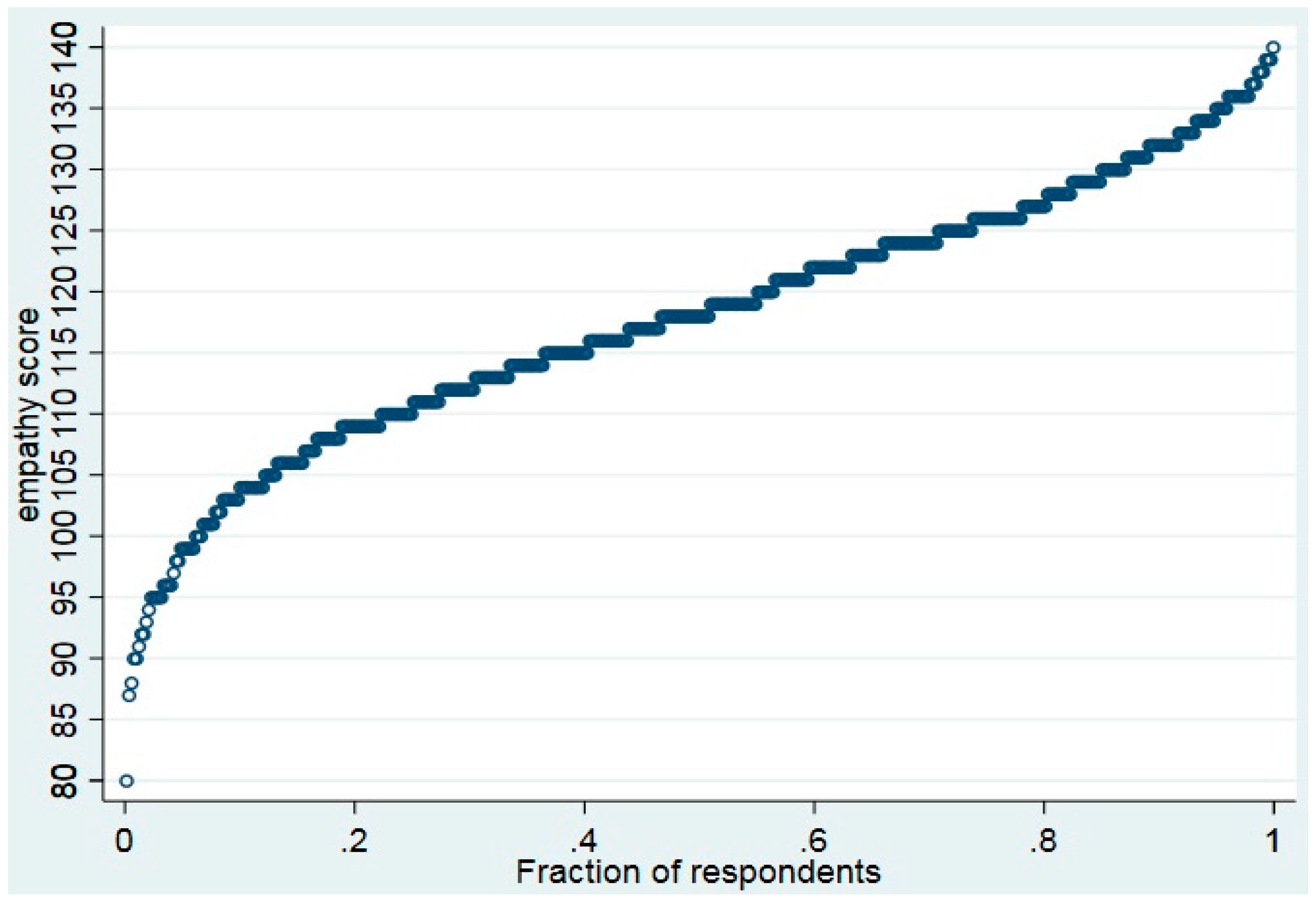
| Characteristic | Mean (SD)/Percentage | CV | p5 | Median | p95 |
|---|---|---|---|---|---|
| Empathy Score | 117.85 (10.09) | 0.09 | 99 | 118 | 135 |
| Demographic Characteristics | |||||
| Physician Age | 54.91 (7.86) | 0.14 | 42 | 55 | 66 |
| Gender | |||||
| Male | 53.4% | ||||
| Female | 46.6% | ||||
| Professional Characteristics | |||||
| Practice Location | |||||
| Urban practice | 49.3% | ||||
| Rural practice | 17.2% | ||||
| Mixed practice | 33.4% | ||||
| Practice Type | |||||
| Partnership practice | 72% | ||||
| Non-partnership | 28% | ||||
| Employment Outside of Clinic | |||||
| Yes | 54.5% | ||||
| No | 45.5% | ||||
| Years since GP specialization | 19.08 (8.27) | 0.43 | 7 | 19 | 32 |
| Years in present practice | 17.19 (16.74) | 0.97 | 4 | 15 | 31 |
| Characteristic | Mean (SD)/Percentage | CV | p5 | Median | p95 |
|---|---|---|---|---|---|
| Job Satisfaction | |||||
| Somewhat or very satisfied | 79.7% | ||||
| Neutral | 10.3% | ||||
| Somewhat or very unsatisfied | 9.9% | ||||
| Contribution of Medical Practice Factors to Job Satisfaction ± | |||||
| Physician-patient relationship | 6.17 (0.81) | 0.13 | 5 | 6 | 7 |
| Intellectual stimulation | 5.65 (1.06) | 0.19 | 4 | 6 | 7 |
| Interaction with colleagues | 5.41 (1.40) | 0.26 | 3 | 6 | 7 |
| Economic profit | 4.92 (1.24) | 0.25 | 2 | 5 | 7 |
| Prestige | 3.71 (1.5) | 0.41 | 1 | 4 | 6 |
| Characteristic | Odds Ratio (95% CI) | p-Value | Reference Group |
|---|---|---|---|
| Demographic Characteristics | |||
| Gender | |||
| Male | 0.91 (0.59, 1.41) | NS | Female |
| Age | |||
| 45–54 | 0.44 (0.21, 0.95) | 0.036 | 35–44 |
| 55–64 | 0.65 (0.26, 1.64) | NS | 35–44 |
| 65+ | 0.74 (0.23, 2.35) | NS | 35–44 |
| Professional Characteristics | |||
| Practice location | |||
| Urban | 1.01 (0.65, 1.57) | NS | Heterogeneous |
| Rural | 0.93 (0.52, 1.68) | NS | Heterogeneous |
| Practice type | |||
| Non-partnership | 1.51 (0.93, 2.46) | NS | Partnership |
| Employment Outside Clinic | |||
| No | 0.59 (0.38, 0.91) | 0.016 | Yes |
| Years since GP specialization | |||
| 14–22 | 1.19 (0.60, 2.38) | NS | 0–13 |
| 23+ | 1.15 (0.47, 2.84) | NS | 0–13 |
| Years in present practice | |||
| 11–19 | 0.92 (0.49, 1.740 | NS | 0–10 |
| 20+ | 0.68 (0.31, 1.48) | NS | 0–10 |
| Job Satisfaction Characteristics | |||
| Job Satisfaction | |||
| Somewhat or Very Satisfied | 0.95 (0.57, 1.69) | NS | Neutral satisfaction or less |
| Contribution of Medical Practice Factors to Job Satisfaction | |||
| Physician-patient relationship | |||
| High (6–7) | 4.30 (2.14, 8.64) | <0.0001 | Low and Medium (1–5) |
| Prestige | |||
| High (6–7) | 0.91 (0.48, 1.74) | NS | Low and Medium (1–5) |
| Intellectual stimulation | |||
| High (6–7) | 1.53 (0.99, 2.37) | 0.053 | Low and Medium (1–5) |
| Interaction with colleagues | |||
| High (6–7) | 1.90 (1.20, 3.01) | 0.006 | Low and Medium (1–5) |
| Economic profit | |||
| High (6–7) | 1.09 (0.72, 1.67) | NS | Low and Medium (1–5) |
| Number of respondents (N) | 464 | ||
| Number of groups | 406 | ||
| Wald Chi2 | 42.03 | 0.0002 | |
| Variance inflation factor (mean) | 2.24 | ||
| Intraclass correlation coefficient | <0.0001 | 0.497 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Charles, J.A.; Ahnfeldt-Mollerup, P.; Søndergaard, J.; Kristensen, T. Empathy Variation in General Practice: A Survey among General Practitioners in Denmark. Int. J. Environ. Res. Public Health 2018, 15, 433. https://doi.org/10.3390/ijerph15030433
Charles JA, Ahnfeldt-Mollerup P, Søndergaard J, Kristensen T. Empathy Variation in General Practice: A Survey among General Practitioners in Denmark. International Journal of Environmental Research and Public Health. 2018; 15(3):433. https://doi.org/10.3390/ijerph15030433
Chicago/Turabian StyleCharles, Justin A., Peder Ahnfeldt-Mollerup, Jens Søndergaard, and Troels Kristensen. 2018. "Empathy Variation in General Practice: A Survey among General Practitioners in Denmark" International Journal of Environmental Research and Public Health 15, no. 3: 433. https://doi.org/10.3390/ijerph15030433






