Hygiene and Health: Who Do Mothers in Vanuatu Communicate with about Health?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. The Setting
2.3. Participant Selection and Questionnaire
- Demographic characteristics of mothers: occupation, education, religion, marital status
- Social network items:a. General advice inside the community: Q15 Have you talked to anyone in “Rural 1” village/”Urban 1” to get advice or discuss problems in the past six months?b. Health advice inside the community: Q23 Have you talked to anyone in “Rural 1” village/”Urban 1” to get health advice in the past six months?c. Health information and advice outside the community: Q34 What other ways have you heard about personal health, other than from people “Rural 1” village/”Urban 1”?; Q35 Of the people who live or work outside “Rural 1/”Urban 1”, whom have you talked with about personal health in the past six months?
2.4. Network Analysis
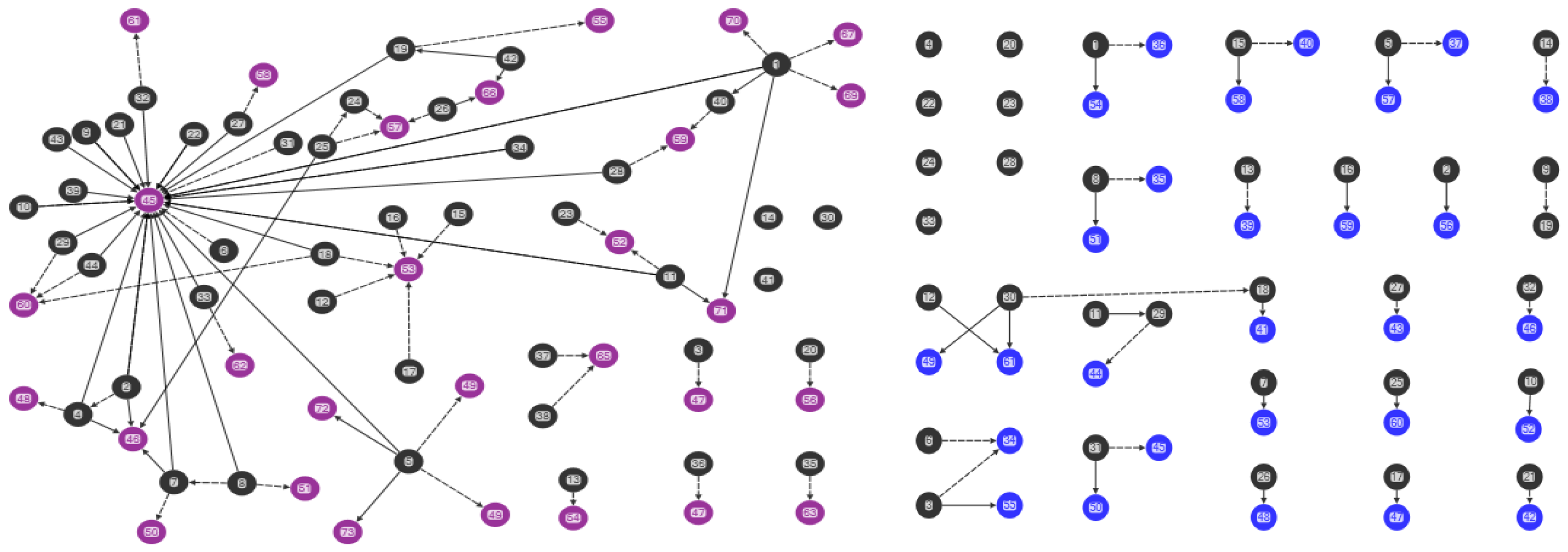
- “Combined mothers’ health advice-seeking network” (Q15, Q23): both general and health advice-seeking (Figure 1)
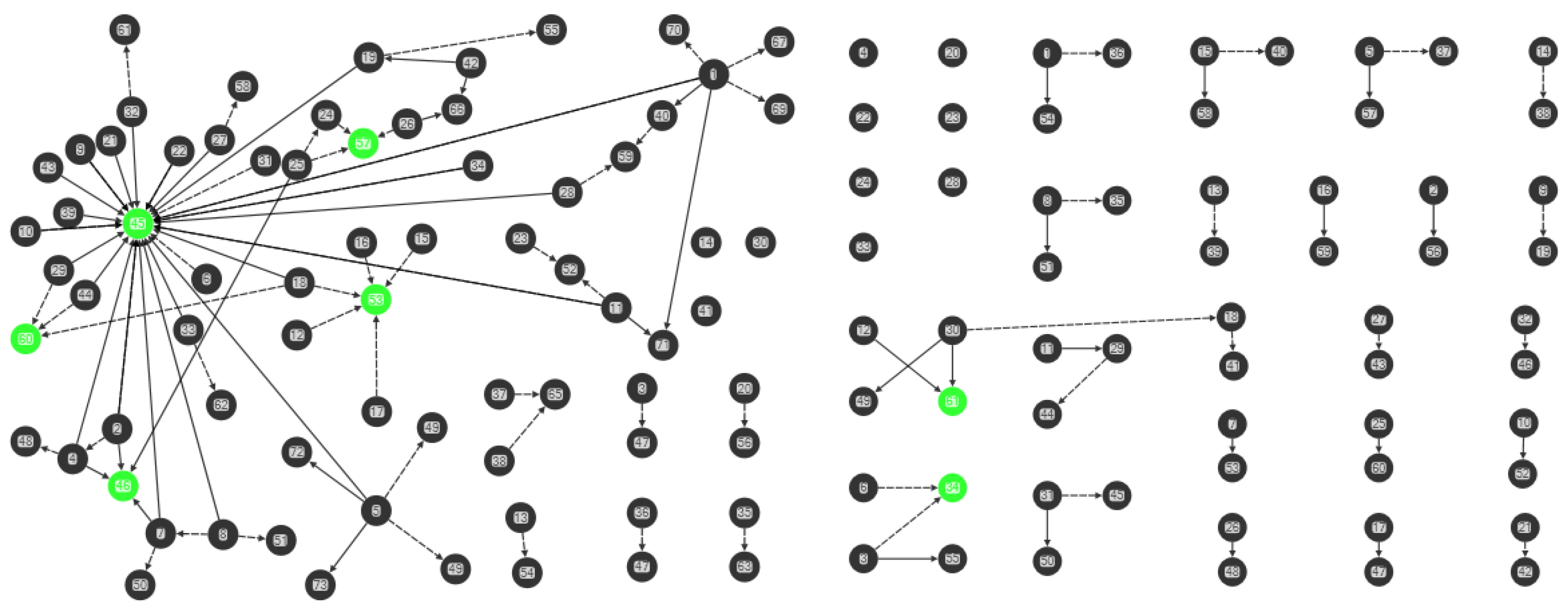
- “Centrality in the combined mothers’ health advice-seeking network” (Q15, Q23): individuals with high in-degree measures (Figure 2)
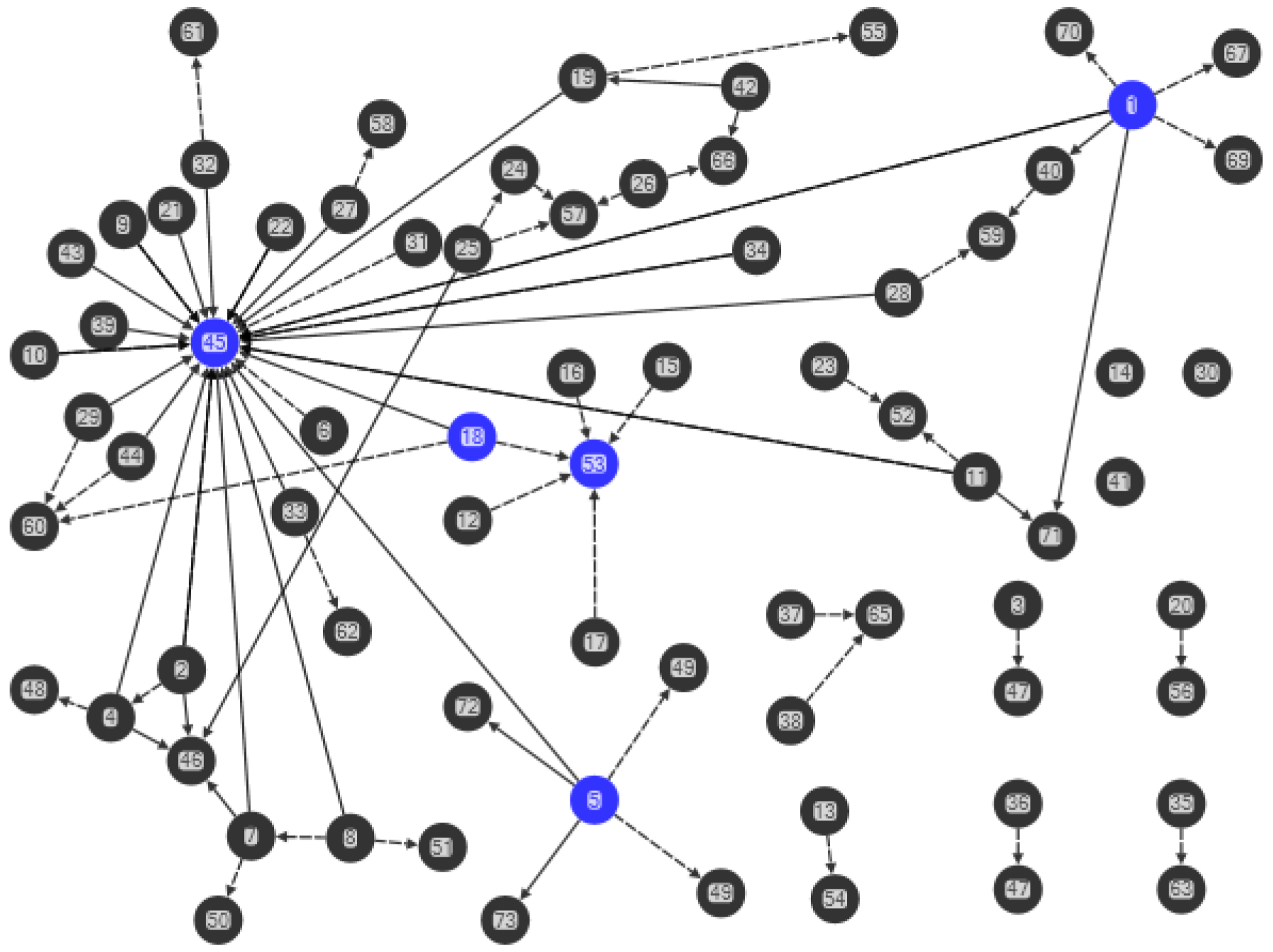
- “Brokerage in the combined mothers’ health advice-seeking network” (Q15, Q23): individuals with high betweenness measures (Figure 3)
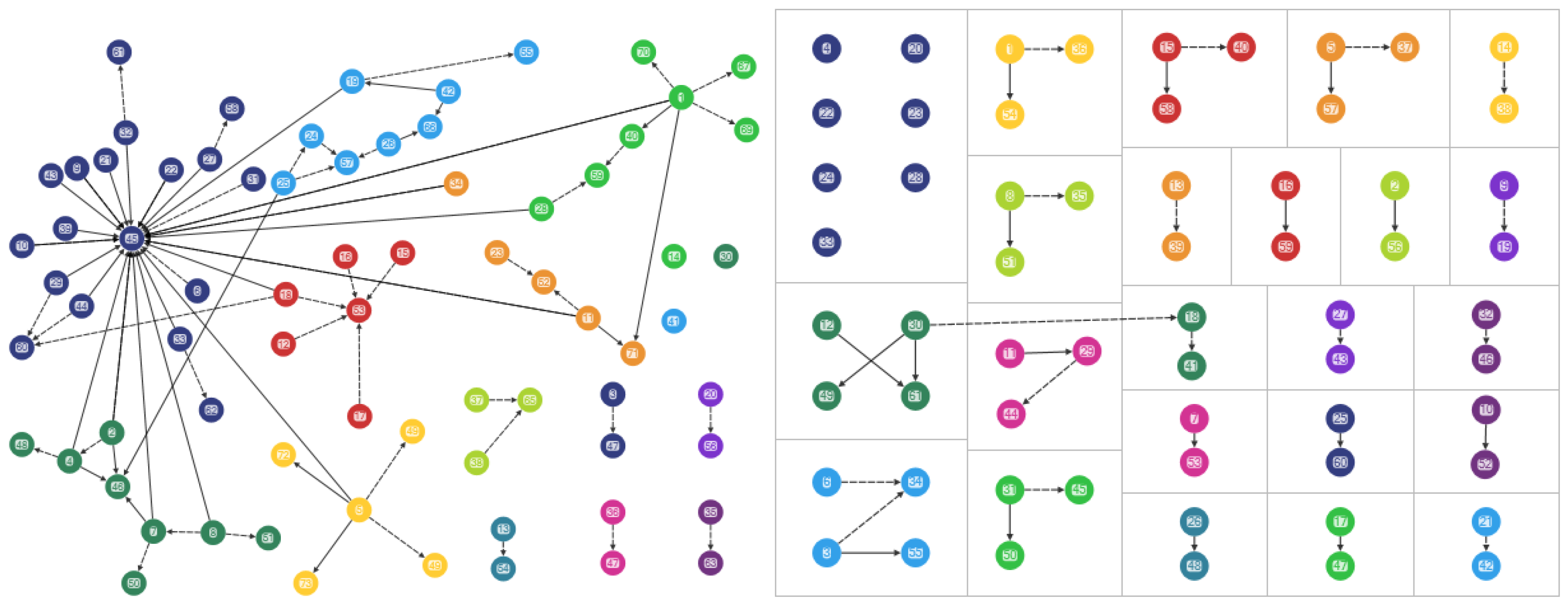
- “Clusters in the combined mothers’ health advice-seeking network” (Q15, Q23): pockets of interconnected individuals (Figure 4)
3. Results
3.1. Demographic Characteristics of the Study Sample
3.2. Sociograms
3.3. Combined Advice-Seeking (Q15, Q23)
3.4. Central Individuals
3.5. Clusters
3.6. Tie strength, Brokers and Isolates
4. Discussion
4.1. Relationships
4.2. Density of Relationships
4.3. Central Individuals
4.4. Clusters, Brokers and Ties
4.5. Practical Implications and Recommendations for Health Communication and Behavior Change
4.5.1. Opinion Leadership
4.5.2. Change Agents
4.6. Social Capital and New Knowledge
4.7. Limitations
5. Conclusions
Acknowledgments
Author Contributions
Conflict of Interest
References
- UNICEF. UNICEF Data: Monitoring the Situation of Children and Women. Child Health, January 2018. Available online: https://data.unicef.org/topic/child-health/diarrhoeal-disease/# (accessed on 7 February 2018).
- Vanuatu Ministry of Health, Vanuatu National Statistics Office and Secretariat of the Pacific Community (SPC). Vanuatu Demographic and Health Survey 2013. Final Report; 2014. Available online: https://vnso.gov.vu/images/Special_Report/Vanuatu_Demographic_and_Health_Survey_Report/2013_VDHS_FINAL_Report.pdf (accessed on 7 February 2018).
- Ministry of Health, Government of Republic of Vanuatu. Vanuatu Multiple Indicator Cluster Survey 2007; Final Report; United Nations Children Fund (UNICEF): Vanuatu, Vanuatu, 2009.
- Ejemot, R.I.; Ehiri, J.E.; Meremikwu, M.M.; Critchley, J.A. Hand washing for preventing diarrhoea. Cochrane Database Syst. Rev. 2008, CD004265. [Google Scholar] [CrossRef]
- World Health Organisation. Diarrhoeal Disease. Fact Sheet No.330. 2013. (Updated 2017 May). Available online: http://www.who.int/mediacentre/factsheets/fs330/en/ (accessed on 7 February 2018).
- Wagner, E.G.; Lanoix, J.N. Excreta Disposal for Rural Areas and Small Communities; World Health Organization: Geneva, Switzerland, 1958. [Google Scholar]
- Larson, E. State-of-the-science-2004: Time for a ‘no excuses/no tolerance’ (NET) strategy. Am. J. Infect. Control 2005, 33, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Vindigni, S.M.; Riley, P.L.; Jhung, M. Systematic review: Handwashing behavior in low-to middle-income countries: Outcome measures and behavior maintenance. Trop. Med. Int. Health 2011, 16, 466–477. [Google Scholar] [CrossRef] [PubMed]
- Curtis, V.; Cairncross, S.; Yonli, R. Review: Domestic hygiene and diarrhea—Pinpointing the problem. Trop. Med. Int. Health 2000, 5, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Huis, A.; van Achterberg, T.; de Bruin, M.; Grol, R.; Schoonhoven, L.; Hulscher, M. A systematic review of hand hygiene improvement strategies: A behavioral approach. Implement. Sci. 2012, 7, 92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Judah, G.; Aunger, R.; Schmidt, W.-P.; Michie, S.; Granger, S.; Curtis, V. Experimental pretesting of hand-washing interventions in a natural setting. Am. J. Public Health 2009, 99, S405–S412. [Google Scholar] [CrossRef] [PubMed]
- Whitby, M.; Pessoa-Silva, C.L.; McLaws, M.L.; Allegranzi, B.; Sax, H.; Larson, E.; Seto, W.H.; Donaldson, L.; Pittet, D. Behavioural considerations for hand hygiene practices: The basic building blocks. J. Hosp. Infect. 2007, 65, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Biran, A.; Schmidt, W.P.; Wright, R.; Jones, T.; Seshadri, M.; Isaac, P.; Nathan, N.A.; Hall, P.; McKenna, J.; Granger, S.; et al. The effect of a soap promotion and hygiene education campaign on handwashing behavior in rural India: A cluster randomised trial. Trop. Med. Int. Health 2009, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Curtis, V.A.; Danquah, L.O.; Aunger, R.V. Planned, motivated and habitual hygiene behavior: An eleven country review. Health Educ. Res. 2009, 24, 655–673. [Google Scholar] [CrossRef] [PubMed]
- Almedom, A.M. Recent developments in hygiene behavior research: An emphasis on methods and meaning. Trop. Med. Int. Health 1996, 1, 177–182. [Google Scholar]
- Aunger, R.; Schmidt, W.-P.; Ranpura, A.; Coombes, Y.; Mainad, P.M.; Matiko, C.N.; Curtis, V. Three kinds of psychological determinants for hand-washing behavior in Kenya. Soc. Sci. Med. 2010, 70, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Marjadi, B.; McLaws, M.L. Rural Indonesian health care workers’ constructs of infection prevention and control knowledge. Am. J. Infect. Control 2010, 38, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Aboud, F.E.; Singla, D.R. Challenges to changing health behaviors in developing countries: A critical overview. Soc. Sci. Med. 2012, 75, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Grol, R.; Grimshaw, J. From best evidence to best practice: Effective implementation of change in patients' care. Lancet 2003, 362, 1225–1230. [Google Scholar] [CrossRef]
- Curtis, V.; Aunger, R. Motivational mismatch: Evolved motives as the source of-and solution to-global public health problems. In Applied Evolutionary Psychology; Roberts, C., Ed.; Oxford University Press: Oxford, UK, 2011; pp. 259–275. [Google Scholar]
- Rogers, E.M. Diffusion of Innovations, 5th ed.; Free Press: New York, NY, USA, 2003. [Google Scholar]
- Stoebenau, K.; Valente, T.W. Using network analysis to understand community-based programs: A case study from highland Madagascar. Int. Fam. Plan. Perspect. 2003, 29, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Valente, T.W.; Watkins, S.C.; Jato, M.N.; van der Straten, A.; Tsitsol, L.P. Social network associations with contraceptive use among Cameroonian women in voluntary associations. Soc. Sci. Med. 1997, 45, 677–687. [Google Scholar] [CrossRef]
- Borgatti, S.P. Identifying sets of key players in a social network. Comput. Math. Organ. Theory 2006, 12, 21–34. [Google Scholar] [CrossRef]
- Flodgren, G.; Parmelli, E.; Doumitm, G.; Gattellari, M.; O'Brien, M.A.; Grimshaw, J.; Eccles, M.P. Local opinion leaders: Effects on professional practice and heath care outcomes. Cochrane Database Syst. Rev. 2007. [Google Scholar] [CrossRef]
- Rogers, E.M.; Cartano, D.G. Methods of measuring opinion leadership. Public Opin. Q. 1962, 26, 435–441. [Google Scholar] [CrossRef]
- Smith, K.P.; Christakis, N.A. Social networks and health. Annu. Rev. Sociol. 2008, 34, 405–429. [Google Scholar] [CrossRef]
- Luby, S.P.; Halder, A.K.; Huda, T.; Unicomb, L.; Johnston, R.B. The effect of handwashing at recommended times with water alone and with soap on child diarrhea in rural Bangladesh: An observational study. PLoS Med. 2011, 8, e1001052. [Google Scholar] [CrossRef] [PubMed]
- Valente, T.W. Network interventions. Science 2012, 337, 49–53. [Google Scholar] [CrossRef] [PubMed]
- Vanuatu National Statistics Office and Secretariat of the Pacific Community. 2009 National Population and Housing Census. Analytical Report Volume 2; 2009. Available online: https://vnso.gov.vu/images/PublicDocuments/Census/2009/2009%20Census%20Analytical%20Report%20-%20Vol2.pdf (accessed on 7 February 2018).
- Keesing, R. Kastom in Melanesia: An overview. Mankind 1982, 13, 297–301. [Google Scholar] [CrossRef]
- Chung, M.; Hill, D. Urban Informal Settlements in Vanuatu: Challenge for Equitable Development. Report Prepared for Pacific Islands Forum Secretariat and United Nations Economic and Social Commission for Asia and the Pacific, Pacific Operation Centre; 2002. Available online: http://mjcs.gov.vu/images/research_database/Vanuatu_Squatter_Settlement_Study_2002.pdf (accessed on 7 February 2018).
- Rogers, E.M.; Kincaid, D.L. Communication Networks: Toward a New Paradigm for Research; Free Press: New York, NY, USA, 1981. [Google Scholar]
- Greenland, K.; Iradati, E.; Ati, A.; Maskoen, Y.Y.; Aunger, R. The context and practice of handwashing among new mothers in Serang, Indonesia: A formative research study. BMC Public Health 2013, 13, 830. [Google Scholar] [CrossRef] [PubMed]
- Whitby, M.; McLaws, M.-L.; Ross, M.W. Why healthcare workers don’t wash their hands: A behavioral explanation. Infect. Control Hosp. Epidemiol. 2006, 27, 484–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valente, T.W. Social Networks and Health: Models, Methods, and Applications; Oxford University Press: New York, NY, USA, 2010; 296p. [Google Scholar]
- Smith, M.; Milic-Frayling, N.; Shneiderman, B.; Mendes Rodrigues, E.; Leskovec, J.; Dunne, C. NodeXL: A Free and Open Network Overview, Discovery and Exploration Add-in for Excel 2007/2010. Social Media Research Foundation. 2010. Available online: https://nodexl.codeplex.com/releases/view/117659 (accessed on 7 February 2018).
- Creswick, N.; Westbrook, J.I. Social network analysis of medication advice-seeking interactions among staff in an Australian hospital. Int. J. Med. Inform. 2010, 79, e116–e125. [Google Scholar] [CrossRef] [PubMed]
- Yousefi-Nooraie, R.; Dobbins, M.; Brouwers, M.; Wakefield, P. Information seeking for making evidence-informed decisions: A social network analysis on the staff of a public health department in Canada. BMC Health Serv. Res. 2012, 12, 118. [Google Scholar] [CrossRef] [PubMed]
- Scott, J. Network Analysis, 2nd ed.; A Handbook; Sage: Thousand Oaks, CA, USA, 1991; pp. 1–208. [Google Scholar]
- Farbey, B.A. Structural models: An introduction to theory of directed graphs. J. Oper. Res. Soc. 1966, 17, 202–203. [Google Scholar] [CrossRef]
- Nieminen, V. On centrallity in a graph. Scand. J. Psychol. 1974, 15, 322–336. [Google Scholar] [CrossRef]
- Freeman, L.C. Centrality in social networks: Conceptual clarification. Soc. Netw. 1979, 1, 215–239. [Google Scholar] [CrossRef]
- Long, J.C.; Cunningham, F.C.; Braithwaite, J. Bridges, brokers and boundary spanners in collaborative networks: A systematic review. BMC Health Serv. Res. 2013, 13, 158. [Google Scholar] [CrossRef] [PubMed]
- Long, J. Network Structure and the Role of Key Players in Healthcare Networks. Ph.D. Thesis, The University of New South Wales, Sydney, Australia, 2013. [Google Scholar]
- Watts, D.W.; Strogatz, S.H. Collective dynamics of ‘small-world’ networks. Nature 1998, 393, 440–442. [Google Scholar] [CrossRef] [PubMed]
- Granovetter, M. The strength of weak ties. Am. J. Sociol. 1977, 78, 1360–1380. [Google Scholar] [CrossRef]
- Granovetter, M. The strength of weak ties: A network theory revisited. Sociol. Theory 1983, 1, 201–233. [Google Scholar] [CrossRef]
- Borgatti, S.P.; Mehra, A.; Brass, D.J.; Labianca, G. Network analysis in the social sciences. Science 2009, 323, 892–895. [Google Scholar] [CrossRef] [PubMed]
- Palmore, J.A.; Furlong, M.J.; Buchmeier, F.X.; Park, I.H.; Souder, L.M. Family planning opinion leadership in Korea, 1971. Stud. Fam. Plan. 1976, 7, 349–356. [Google Scholar] [CrossRef]
- Widmer, A. Diversity as valued and troubled: Social identities and demographic categories in understandings of rapid urban growth in Vanuatu. Anthropol. Med. 2013, 20, 142–159. [Google Scholar] [CrossRef] [PubMed]
- File, K.; McLaws, M.-L. Ni-Vanuatu health-seeking practices for general health and childhood diarrheal illness: Results from a qualitative methods study. BMC Res. Notes 2015, 8, 189. [Google Scholar] [CrossRef] [PubMed]
- Weller, S.C.; Baer, R.D.; de Alba Garcia, J.G.; Glazer, M.; Trotter, R.; Pachter, L.; Klein, R.E. Regional variation in Latino descriptions of susto. Cult. Med. Psychiatry 2002, 26, 449–472. [Google Scholar] [PubMed]
- Long, J.C.; Cunningham, F.C.; Carswell, P.; Braithwaite, J. Who are the key players in a new translational research network? BMC Health Serv. Res. 2013, 13, 338. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, K.; Valente, T.; Pentz, M.A. Network structural influences on the adoption of evidenced-based prevention in communities. J. Commun. Psychol. 2009, 37, 830–845. [Google Scholar] [CrossRef] [PubMed]
- Levy-Storms, L.; Wallace, S.P. Use of mammography screening among older Samoan women in Los Angeles county: A diffusion network approach. Soc. Sci. Med. 2003, 57, 987–1000. [Google Scholar] [CrossRef]
- Maden, C.; McKendrick, S.; Grace, R. Alternative medicine use at Vila Central Hospital Vanuatu: A survey of the use of ‘custom medicine’ in patients and staff. Trop Dr. 2003, 33, 22–24. [Google Scholar] [CrossRef] [PubMed]
- Viney, K.; Johnson, P.; Tagaro, M.; Fanai, S.; Linh, N.N.; Kelly, P.; Herley, D.; Sleigh, A. Traditional healers and the potential for collaboration with the national tuberculosis programme in Vanuatu: Results from a mixed methods study. BMC Public Health 2014, 14, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Szreter, S.; Woolcock, M. Health by association? Social capital, social theory, and the political economy of public health. Int. J. Epidemiol. 2004, 33, 650–667. [Google Scholar] [CrossRef] [PubMed]
- Kawachi, I. Commentary: Social capital and health: Making the connections one step at a time. Int. J. Epidemiol. 2006, 35, 989–993. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Traditional Medicine Strategy: 2014–2023. 2013, Vol. 1, Alternative and Integrative Medicine. pp. 1–78. Available online: http://apps.who.int/iris/bitstream/10665/92455/1/9789241506090_eng.pdf (accessed on 7 February 2018).
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
File, K.; Valente, T.; McLaws, M.-L. Hygiene and Health: Who Do Mothers in Vanuatu Communicate with about Health? Int. J. Environ. Res. Public Health 2018, 15, 443. https://doi.org/10.3390/ijerph15030443
File K, Valente T, McLaws M-L. Hygiene and Health: Who Do Mothers in Vanuatu Communicate with about Health? International Journal of Environmental Research and Public Health. 2018; 15(3):443. https://doi.org/10.3390/ijerph15030443
Chicago/Turabian StyleFile, Karen, Thomas Valente, and Mary-Louise McLaws. 2018. "Hygiene and Health: Who Do Mothers in Vanuatu Communicate with about Health?" International Journal of Environmental Research and Public Health 15, no. 3: 443. https://doi.org/10.3390/ijerph15030443



