Depression, Suicidal Behaviour, and Mental Disorders in Older Aboriginal Australians
Abstract
:1. Introduction
1.1. Mental Health of Older Aboriginal Australians
1.2. Formative Experiences and Late-Life Depression
1.3. Aims of Current Study
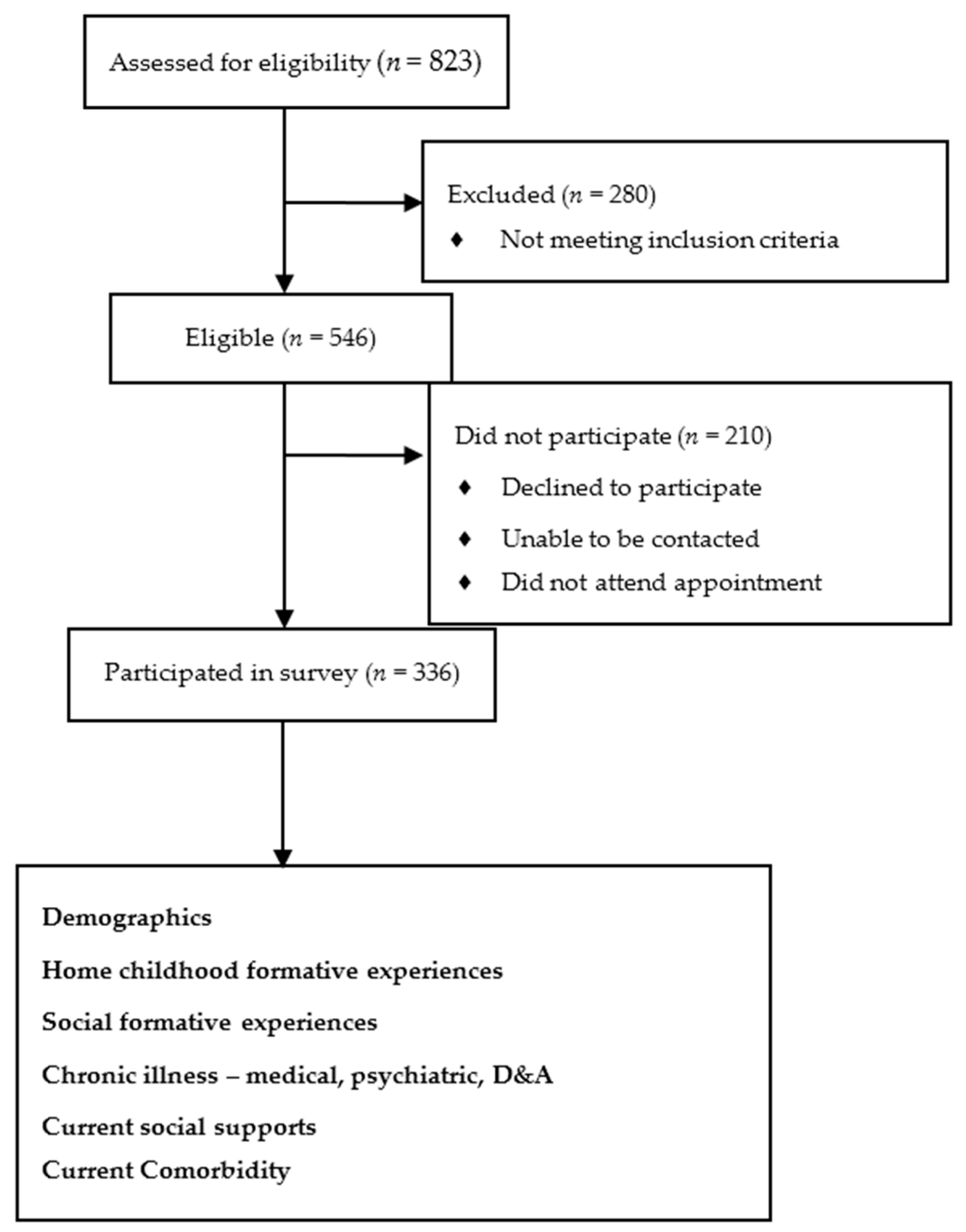
2. Materials and Methods
2.1. Outcome Measures
2.2. Demographic Data
2.3. Childhood Formative Experiences at Home
2.4. Social Formative Experiences
2.5. Chronic Illness Experiences
2.6. Psychosocial Factors
2.7. Data Analysis
2.8. Univariate Analysis
2.9. Multivariate Analysis
3. Results
3.1. Demographics
3.2. Prevalence Rates
Lifetime and Point Prevalence of Mental Disorders
3.3. Univariate Associations with Current Depression
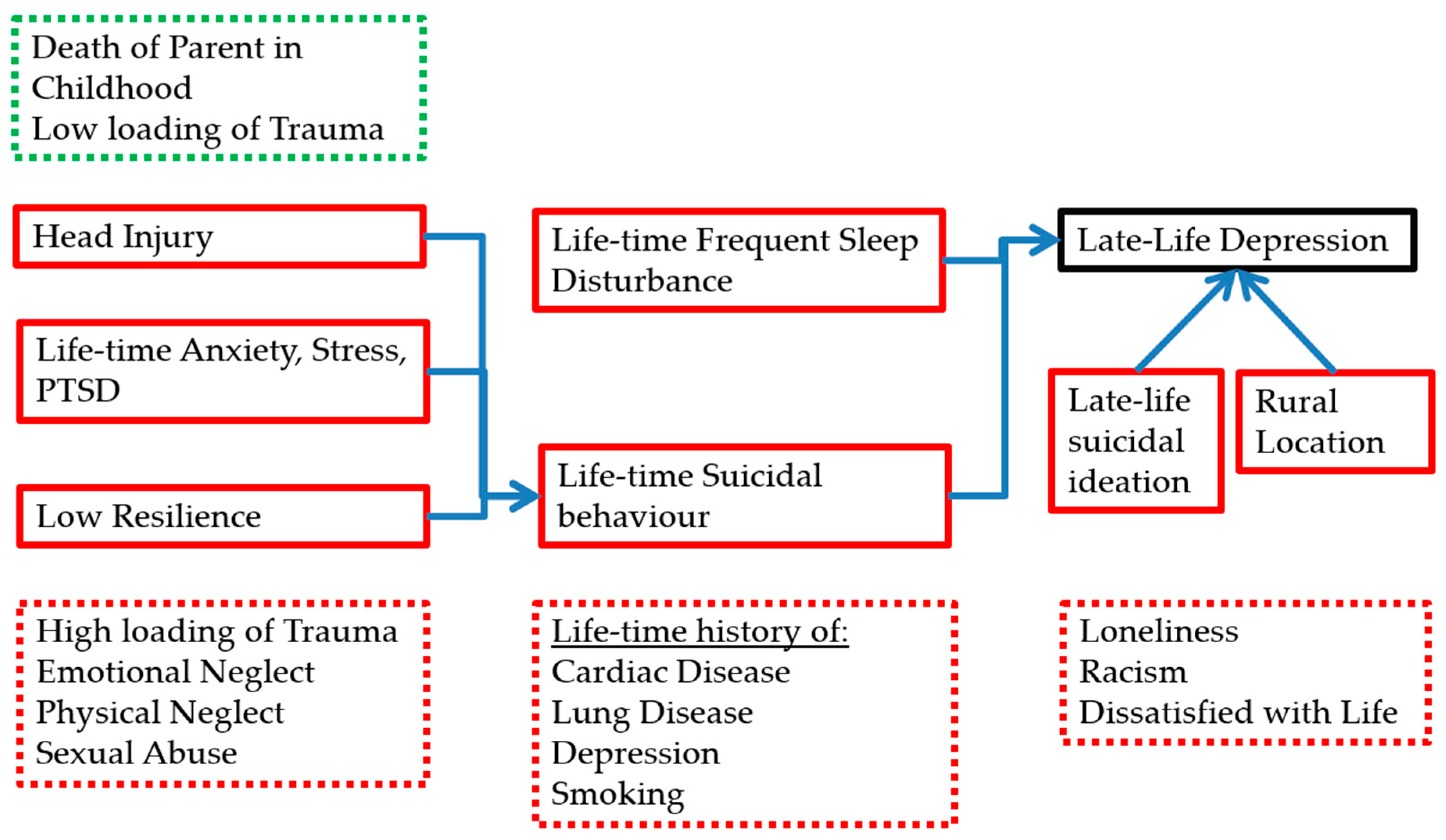
3.4. Multivariate Analysis of Current Late-life Depression
3.5. Multivariate Analysis of Suicidal Behaviour History
4. Discussion
4.1. Limitations
4.2. Implications for Prevention and Intervention
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Krieg, A. The experience of collective trauma in Australian Indigenous communities. Australas. Psychiatry 2009, 17, S28–S32. [Google Scholar] [CrossRef] [PubMed]
- Brown, R. Australian Indigenous mental health. Aust. N. Z. J. Ment. Health Nurs. 2001, 10, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Gubhaju, L.; McNamara, B.J.; Banks, E.; Joshy, G.; Raphael, B.; Williamson, A.; Eades, S.J. The overall health and risk factor profile of Australian Aboriginal and Torres Strait Islander participants from the 45 and up study. BMC Public Health 2013, 13, 661. [Google Scholar] [CrossRef] [PubMed]
- Turale, S. Ballarat Koorie life experiences: Learning about Koorie perceptions of mental health and illness. Aust. N. Z. J. Ment. Health Nurs. 1994, 3, 16–28. [Google Scholar]
- Markwick, A.; Ansari, Z.; Sullivan, M.; Parsons, L.; McNeil, J. Inequalities in the social determinants of health of Aboriginal and Torres Strait Islander People: A cross-sectional population-based study in the Australian state of Victoria. Int. J. Equity Health 2014, 13, 91. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. The Health and Welfare of Australia’s Aboriginal and Torres Strait Islander Peoples; Australian Bureau of Statistics: Canberra, Australia, 2010.
- Australian Bureau of Statistics. Causes of Death: Deaths of Aboriginal and Torres Strait Islander Australians; Australian Bureau of Statistics: Canberra, Australia, 2015.
- Almeida, O.P.; Flicker, L.; Fenner, S.; Smith, K.; Hyde, Z.; Atkinson, D.; Skeaf, L.; Malay, R.; LoGiudice, D. The Kimberley Assessment of Depression of Older Indigenous Australians: Prevalence of depressive disorders, risk factors and validation of the KICA-dep Scale. PLoS ONE 2014, 9, e94983. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Life Tables for Aboriginal and Torres Strait Islander Australians, 2010–2012; Australian Bureau of Statistics: Canberra, Australia, 2013.
- Dube, S.R.; Anda, R.F.; Felitti, V.J.; Chapman, D.P.; Williamson, D.F.; Giles, W.H. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the Adverse Childhood Experiences Study. JAMA 2001, 286, 3089–3096. [Google Scholar] [CrossRef] [PubMed]
- Chapman, D.P.; Whitfield, C.L.; Felitti, V.J.; Dube, S.R.; Edwards, V.J.; Anda, R.F. Adverse childhood experiences and the risk of depressive disorders in adulthood. J. Affect Disord. 2004, 82, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Patten, S.B.; Wilkes, T.C.R.; Williams, J.V.A.; Lavorato, D.H.; el-Guebaly, N.; Wild, T.C.; Colman, I.; Bulloch, A.G.M. Childhood adversity and subsequent mental health status in adulthood: Screening for associations using two linked surveys. Epidemiol. Psychiatr. Sci. 2016, 25, 160–170. [Google Scholar] [CrossRef] [PubMed]
- Draper, B.; Pfaff, J.J.; Pirkis, J.; Snowdon, J.; Lautenschlager, N.T.; Wilson, I.; Almeida, O.P. Long-term effects of childhood abuse on the quality of life and health of older people: Results from the depression and early prevention of suicide in general practice project. J. Am. Geriatr. Soc. 2008, 56, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Danese, A.; Moffitt, T.E.; Harrington, H.; Milne, B.J.; Polanczyk, G.; Pariante, C.M.; Poulton, R.; Caspi, A. Adverse childhood experiences and adult risk factors for age-related disease: Depression, inflammation, and clustering of metabolic risk markers. Arch. Pediatr. Adolesc. Med. 2009, 163, 1135–1143. [Google Scholar] [CrossRef]
- Radford, K.; Delbaere, K.; Draper, B.; Mack, H.A.; Daylight, G.C.M.; Cumming, R.; Chalkley, S.; Minoque, C.; Broe, G.A. Childhood stress and adversity is associated with late-life dementia in Aboriginal Australians. Am. J. Geriatr. Psychiatry 2017, 25, 1097–1106. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Leicht, A.; Slatcher, A.; Kraeuter, A.K.; Ketheesan, S.; Larkins, S.; Sarnyai, Z. Cortisol awakening response and acute stress reactivity in first nations people. Sci. Rep. 2017, 7, 41760. [Google Scholar] [CrossRef] [PubMed]
- Sarnyai, Z.; Berger, M.; Jawan, I. Allostatic load mediates the impact of stress and trauma on physical and mental health in Indigenous Australians. Australas. Psychiatry 2016, 24, 72–75. [Google Scholar] [CrossRef]
- Aziz, R.; Steffens, D.C. What are the causes of late-life depression? Psychiatr. Clin. N. Am. 2013, 36, 497–516. [Google Scholar] [CrossRef] [PubMed]
- Radford, K.; Mack, H.A.; Robertson, H.; Draper, B.; Chalkley, S.; Daylight, G.; Cumming, R.; Bennett, H.; Pulver, L.J.; Broe, G.A. The Koori Growing Old Well Study: Investigating aging and dementia in urban Aboriginal Australians. Int. Psychogeriatr. 2014, 26, 1033–1043. [Google Scholar] [CrossRef] [PubMed]
- Esler, D.; Johnston, F.; Thomas, D.; David, B. The validity of a depression screening tool modified for use with Aboriginal and Torres Strait Islander people. Aust. N. Z. J. Public Health 2008, 32, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Scher, C.D.; Stein, M.B.; Asmundson, G.J.G.; McCreary, D.R.; Forde, D.R. The Childhood Trauma Questionnaire in a Community Sample: Psychometric Properties and Normative Data. J. Trauma. Stress 2001, 14, 843–857. [Google Scholar] [CrossRef] [PubMed]
- Kenny, D.T.; Lennings, J.L. Cultural group differences in social disadvantage, offence characteristics, and experience of childhood trauma and psychopathology in incarcerated juvenile offenders in NSW, Australia: Implications for service delivery. Psychiatry Psychol. Law 2011, 14, 294–305. [Google Scholar] [CrossRef]
- Calabria, B.; Clifford, A.; Shakeshaft, A.P.; Conigrave, K.M.; Simpsons, L.; Bliss, D.; Allan, J. Identifying Aboriginal-specific AUDIT-C and AUDIT-3 cutoff scores for at-risk, high-risk, and likely dependent drinkers using measures of agreement with the 10-item Alcohol Use Disorders Identification Test. Addict. Sci. Clin. Pract. 2014, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- Goins, R.; Gregg, J.; Fiske, A. Psychometric properties of the Connor-Davidson Resilience Scale with older American Indians: The Native Elder Care Study. Res. Aging 2013, 35, 123–143. [Google Scholar] [CrossRef] [PubMed]
- Lamond, A.; Depp, C.; Allison, M.; Langer, R.; Reichstadt, J.; Moore, D.; Golshan, S.; Ganiats, T.; Jeste, D. Measurement and predictors of resilience among community-dwelling older women. J. Psychiatr. Res. 2008, 43, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Paradies, Y.C.; Cunningham, J. Development and validation of the measure of indigenous racism experiences (MIRE). Int. J. Equity Health 2008, 7, 9. [Google Scholar] [CrossRef] [PubMed]
- Pavot, W.G.; Diener, E. Review of the Satisfaction with Life Scale. Psychol. Assess. 1993, 5, 164–172. [Google Scholar] [CrossRef]
- Folstein, M.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Radford, K.; Mack, H.A.; Draper, B.; Chalkley, S.; Delbaere, K.; Daylight, G.; Cumming, R.G.; Bennett, H.; Broe, G.A. Comparison of three cognitive screening tools in older urban and regional Aboriginal Australians. Dement. Geriatr. Cogn. Disord. 2015, 40, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Almeida, O.P.; Draper, B.; Snowdon, J.; Lautenschlager, N.T.; Pirkis, J.; Byrne, G.; Sim, M.; Stocks, N.; Flicker, L.; Pfaff, J.J. Factors associated with suicidal thoughts in a large community study of older adults. Br. J. Psychiatry 2012, 201, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Causes of Death: Intentional Self-harm (Suicide); Australian Bureau of Statistics: Canberra, Australia, 2015.
- Hinton, R.; Kavanagh, D.; Barclay, L.; Chenhall, R.; Nagel, T. Developing a best practice pathway to support improvements in Indigenous Australians’ mental health and well-being: A qualitative study. BMJ Open. 2015, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turpin, M.; Bartlett, H.; Kavanagh, D.; Gallois, C. Mental health issues and resources in rural and regional communities: An exploration of perceptions of service providers. Aust. J. Rural Health 2007, 15, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Cosgrave, C.; Hussain, R.; Maple, M. Retention challenge facing Australia’s rural community mental health services: Service managers’ perspectives. Aust. J. Rural Health 2015, 23, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Pigeon, W.R.; Hegel, M.; Unützer, J.; Fan, M.Y.; Sateia, M.J.; Lyness, J.M.; Phillips, C.; Perlis, M.L. Is insomnia a perpetuating factor for late-life depression in the IMPACT cohort? Sleep 2008, 31, 481–488. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.D.; Thompson, A.; King, L.; Corbett, B.; Shnaider, P.; St. Cyr, K.; Nelson, C.; Sareen, J.; Elhai, J.; Zamorski, M. Insomnia, psychiatric disorders and suicidal ideation in a national representative sample of active Canadian forces members. BMC Psychiatry 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, Z. The association between depression and suicide when hopelessness is controlled for. Compr. Psychiatry 2013, 54, 790–796. [Google Scholar] [CrossRef] [PubMed]
- Keilp, J.G.; Grunebaum, M.F.; Gorlyn, M.; LeBlanc, S.; Burke, A.K.; Galfalvy, H.; Oquendo, M.A.; Mann, J.J. Suicidal ideation and the subjective aspects of depression. J. Affect Disord. 2012, 140, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Mackelprang, J.L.; Bombardier, C.H.; Fann, J.R.; Temkin, N.R.; Barber, J.K.; Dikmen, S.S. Rates and predictors of suicidal ideation during the first year after traumatic brain injury. Am. J. Public Health 2014, 104, e100–e107. [Google Scholar] [CrossRef] [PubMed]
- Wisco, B.E.; Marx, B.P.; Holowka, D.W.; Vasterling, J.J.; Han, S.C.; Chen, M.S.; Gradus, J.L.; Nock, M.K.; Rosen, R.C.; Keane, T.M. Traumatic brain injury, PTSD, and current suicidal ideation among Iraq and Afghanistan U.S. veterans. J. Trauma. Stress 2014, 27, 244–248. [Google Scholar] [CrossRef] [PubMed]
- Ilie, G.; Mann, R.E.; Boak, A.; Adlaf, E.M.; Hamilton, H.; Asbridge, M.; Rehm, J.; Cusimano, M.D. Suicidality, bullying and other conduct and mental health correlates of traumatic brain injury in adolescents. PLoS ONE 2014, 9, e94936. [Google Scholar] [CrossRef] [PubMed]
- Simpson, G.; Tate, R. Suicidality after traumatic brain injury: Demographic, injury and clinical correlates. Psychol. Med. 2002, 32, 687–697. [Google Scholar] [CrossRef] [PubMed]
- Bentley, K.H.; Franklin, J.C.; Ribeiro, J.D.; Kleiman, E.M.; Fox, K.R.; Nock, M.K. Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: A meta-analytic review. Clin. Psychol. Rev. 2016, 43, 30–46. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.W.; Fairweather-Schmidt, A.K.; Roberts, R.M.; Burns, R.; Anstey, K.J. Does resilience predict suicidality? A lifespan analysis. Arch. Suicide Res. 2014, 18, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.W.; Fairweather-Schmidt, A.K.; Burns, R.; Roberts, R.M.; Anstey, K.J. Psychological Resilience Provides No Independent Protection From Suicidal Risk. Crisis 2016, 37, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Comijs, H.C.; van Exel, E.; van der Mast, R.C.; Paauw, A.; Oude Voshaar, R.; Stek, M.L. Childhood abuse in late-life depression. J. Affect Disord. 2013, 147, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.G.; DiNitto, D.M.; Marti, C.N.; Choi, B.Y. Association of adverse childhood experiences with lifetime mental and substance use disorders among men and women aged 50+ years. Int. Psychogeriatr. 2017, 29, 359–372. [Google Scholar] [CrossRef]
- Priest, N.C.; Paradies, Y.C.; Gunthorpe, W.; Cairney, S.J.; Sayers, S.M. Racism as a determinant of social and emotional wellbeing for Aboriginal Australian youth. Med. J. Aust. 2011, 194, 546–550. [Google Scholar] [PubMed]
- Prince, M.J.; Harwood, R.H.; Blizard, R.A.; Thomas, A.; Mann, A.H. Social support deficits, loneliness and life events as risk factors for depression in old age. The Gospel Oak Project VI. Psychol. Med. 1997, 27, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Adams, K.B.; Sanders, S.; Auth, E.A. Loneliness and depression in independent living retirement communities: Risk and resilience factors. Aging Ment. Health 2004, 8, 475–485. [Google Scholar] [CrossRef] [PubMed]
- Holvast, F.; Burger, H.; de Waal, M.M.; van Marwijk, H.W.; Comijs, H.C.; Verhaak, P.F. Loneliness is associated with poor prognosis in late-life depression: Longitudinal analysis of the Netherlands study of depression in older persons. J. Affect Disord. 2015, 185, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Lue, B.H.; Chen, L.J.; Wu, S.C. Health, financial stresses, and life satisfaction affecting late-life depression among older adults: A nationwide, longitudinal survey in Taiwan. Arch. Gerontol. Geriatr. 2010, 50, S34–S38. [Google Scholar] [CrossRef]
- Valkanova, V.; Ebmeier, K.P. Vascular risk factors and depression in later life: A systematic review and meta-analysis. Biol. Psychiatry 2013, 73, 406–413. [Google Scholar] [CrossRef] [PubMed]
- Panagioti, M.; Scott, C.; Blakemore, A.; Coventry, P.A. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int. J. Chron. Obstruct. Pulmon. Dis. 2014, 9, 1289–1306. [Google Scholar] [CrossRef] [PubMed]
- Choi, N.G.; Dinitto, D.M. Drinking, smoking, and psychological distress in middle and late life. Aging Ment. Health 2011, 15, 720–731. [Google Scholar] [CrossRef] [PubMed]
- Jeon, H.J.; Lee, C.; Fava, M.; Mischoulon, D.; Shim, E.J.; Heo, J.Y.; Choi, H.; Park, J.H. Childhood trauma, parental death, and their co-occurrence in relation to current suicidality risk in adults: A nationwide community sample of Korea. J. Nerv. Ment. Dis. 2014, 202, 870–876. [Google Scholar] [CrossRef] [PubMed]
- Berg, L.; Rostila, M.; Hjern, A. Parental death during childhood and depression in young adults—A national cohort study. J. Child Psychol. Psychiatry 2016, 57, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Savikko, N.; Routasalo, P.; Tilvis, R.S.; Strandberg, T.E.; Pitkälä, K.H. Loss of parents in childhood—Associations with depression, loneliness, and attitudes towards life in older Finnish people. Int. J. Older People Nurs. 2006, 1, 17–24. [Google Scholar] [CrossRef] [PubMed]
| Variable | n (Total n = 336) | % | Missing Data (n) |
|---|---|---|---|
| Gender | 0 | ||
| Male | 136 | 40.5 | |
| Female | 200 | 59.5 | |
| Age | 0 | ||
| 60–69 | 246 | 73.2 | |
| 70+ | 90 | 26.8 | |
| Location | 0 | ||
| Urban | 140 | 41.7 | |
| Regional | 196 | 58.3 | |
| Income source | 13 | ||
| Government Pension | 266 | 79.2 | |
| Other source | 57 | 17 | |
| Marital Status | 8 | ||
| Married | 124 | 36.9 | |
| Widowed, divorced or separated | 165 | 49.1 | |
| Never married | 39 | 11.6 | |
| Accommodation | 27 | ||
| Public Accommodation | 175 | 52.1 | |
| Own Home | 81 | 24.1 | |
| Private Rental | 36 | 10.7 | |
| Residential Aged Care Facility | 17 | 5.1 |
| Depression and Comorbidity | n (Total n = 336) | % | Missing Data (n) |
|---|---|---|---|
| Significant Depression on PHQ9 | 57 | 18.1 | 27 |
| Suicidal ideation | 35 | 11.1 | 21 |
| Cognitive impairment | 104 | 31 | |
| Dissatisfied with life | 101 | 30.1 | |
| Loneliness | 162 | 48.1 | 23 |
| Variable (n) | Depressed | Not Depressed | Odds Ratio | 95% Confidence Interval | Missing Data (n) |
|---|---|---|---|---|---|
| n (% of variable) | |||||
| Demographics | |||||
| Male (136) | 23 (16.9) | 113 (83.1) | 0.9 | 0.5–1.5 | |
| Age | |||||
| 60–69 (245) | 44 (18.8) | 113 (81.2) | 1.2 | 0.6–2.2 | |
| 70+ (91) | 15 (16.5) | 76 (83.5) | |||
| Regional (196) | 44 (22.4) | 152 (77.6) | 2.1 * | 1.1–3.8 | |
| Pension (266) | 48 (18) | 218 (82) | 1 | 0.5–2.2 | 13 |
| Marital Status | 8 | ||||
| Married (124) | 26 (21) | 98 (79) | 1.3 | 0.8–2.4 | |
| Widowed, divorced or separated (165) | 28 (17) | 137 (83) | 0.9 | 0.5–1.5 | |
| Never married (39) | 5 (12.8) | 34 (87.2) | 0.6 | 0.2–1.7 | |
| Accommodation | 27 | ||||
| Private rental (36) | 10 (27.8) | 26 (72.2) | 1.9 | 0.9–4.1 | |
| Residential facility (17) | 2 (11.8) | 15 (88.2) | 0.6 | 0.1–1.6 | |
| Public Accommodation (175) | 31 (17.7) | 144 (82.3) | 0.9 | 0.5–1.6 | |
| Own Home (81) | 16 (19.8) | 65 (80.2) | 1.1 | 0.6–2.2 | |
| Childhood Experiences at Home | |||||
| Raised by parents | |||||
| Both parents (166) | 32 (19.3) | 134 (80.7) | 1.2 | 0.7–2 | |
| By mother or father (114) | 21 (18.4) | 93 (81.6) | 1 | 0.6–1.9 | |
| By neither (56) | 8 (14.3) | 48 (85.7) | 0.7 | 0.3–1.6 | |
| Death of parent(s) in childhood (74) | 6 (8.1) | 68 (91.9) | 0.3 * | 0.1–0.8 | 2 |
| Taken away from family (33) | 8 (24.2) | 25 (75.8) | 0.6 | 0.7–3.7 | 9 |
| CTQ | 37 | ||||
| Lower tertile (109) | 11 (10.1) | 98 (89.9) | 0.4 * | 0.2–0.8 | |
| Mid tertile (115) | 22 (19.1) | 93 (80.9) | 1.1 | 0.6–2 | |
| Upper tertile (111) | 28 (25.2) | 83 (74.8) | 2 * | 1.1–3.4 | |
| Social Formative Experiences | |||||
| Behavioural disturbances at school (154) | 33 (21.4) | 121 (78.6) | 1.6 | 0.9–2.1 | 11 |
| Highest Education at school | 4 | ||||
| Year 6 or less (73) | 14 (19.2) | 59 (80.8) | 1.1 | 0.6–2.1 | |
| Year 7–9 (190) | 34 (17.9) | 156 (82.1) | 1.1 | 0.6–2.1 | |
| Year 10–12 (69) | 13 (18.8) | 56 (81.2) | 1 | 0.5–2 | |
| Further Education (161) | 31 (19.3) | 130 (80.7) | 1.1 | 0.7–2 | 1 |
| Previous Employment (302) | 57 (18.9) | 245 (81.1) | 1.3 | 0.3–5.9 | 21 |
| Previous Custody (109) | 19 (17.4) | 90 (82.6) | 1 | 0.5–1.8 | 13 |
| Chronic Illness | |||||
| Head injury (95) | 19 (20) | 76 (80) | 1.2 | 0.7–2.3 | 10 |
| Stroke (78) | 19 (24.4) | 59 (75.6) | 1.7 | 0.9–3.1 | 10 |
| Hypertension (205) | 34 (16.6) | 171 (83.4) | 0.8 | 0.4–1.4 | 12 |
| Hypercholesterolaemia (141) | 29 (20.6) | 112 (79.4) | 1.4 | 0.8–2.4 | 33 |
| Cardiac Disease (140) | 32 (22.9) | 108 (77.1) | 1.7 * | 1–3.1 | 10 |
| Diabetes (140) | 24 (17.1) | 116 (82.9) | 0.9 | 0.5–1.6 | 19 |
| Sleep Difficulties | 23 | ||||
| Never (138) | 13 (9.4) | 125 (90.6) | 0.3 * | 0.2–0.6 | |
| Infrequent (88) | 16 (18.2) | 72 (81.8) | 1 | 0.5–1.9 | |
| Frequent (87) | 29 (33.3) | 58 (66.7) | 3.4 * | 1.9–6.1 | |
| Cancer (38) | 8 (21.1) | 30 (78.9) | 1.2 | 0.5–2.8 | 19 |
| Lung Disease (101) | 28 (27.7) | 73 (72.3) | 2.4 * | 1.3–4.3 | 26 |
| Anxiety, Stress, and PTSD (101) | 34 (33.7) | 67 (66.3) | 4.3 * | 2.4–7.9 | 13 |
| Depression (112) | 32 (28.6) | 80 (71.4) | 2.8 * | 1.6–5.1 | 13 |
| Suicidal behaviour (64) | 28 (43.8) | 36 (56.3) | 5.7 * | 3.1–10.6 | 14 |
| Smoking (228) | 47 (20.6) | 181 (79.4) | 2.1 * | 1–4.3 | 18 |
| Past High-Risk Alcohol Use (187) | 31 (16.6) | 156 (83.4) | 0.8 | 0.5–1.4 | 14 |
| Marijuana use (42) | 11 (26.2) | 31 (73.8) | 1.7 | 0.8–3.6 | 17 |
| Current Psychosocial Factors | |||||
| Frequent Loneliness (162) | 40 (24.7) | 122 (75.3) | 3 * | 1.6–5.6 | 23 |
| Community Support (304) | 55 (18.1) | 249 (81.9) | 0.7 | 0.2–2.5 | 20 |
| Connected to local Aboriginal community (299) | 54 (18.1) | 245 (81.9) | 0.8 | 0.3–2.1 | 9 |
| Strong connection to Country (235) | 39 (16.6) | 196 (83.4) | 0.6 | 0.3–1.1 | 29 |
| Traditional language (120) | 21 (17.5) | 99 (82.5) | 1.0 | 0.5–1.7 | 13 |
| CDRISC (Resilience) | 30 | ||||
| Lower tertile (115) | 34 (29.6) | 81 (70.4) | 3 * | 1.2–5.3 | |
| Mid tertile (105) | 13 (12.4) | 92 (87.6) | 0.5 | 0.3–1 | |
| Upper tertile (116) | 14 (12.1) | 102 (87.9) | 0.5 | 0.3–1 | |
| Previous Experience of Racism (142) | 33 (23.9) | 108 (76.1) | 2.1 * | 1.2–3.8 | 32 |
| Dissatisfied with Life (209) | 28 (27.7) | 73 (72.3) | 2.3 * | 1.3–4.1 | |
| Current Comorbidity | |||||
| Smoking (87) | 17 (19.5) | 70 (80.5) | 1.1 | 0.6–2.1 | 11 |
| High-Risk Alcohol use (31) | 8 (25.8) | 23 (74.2) | 1.7 | 0.7–3.9 | |
| Cognitive Impairment (104) | 19 (18.3) | 85 (81.7) | 1 | 0.6–1.8 | |
| Suicidal ideation (35) | 22 (65.8) | 13 (34.2) | 14 * | 6.6–29.8 | |
| Variable | Odds Ratio | 95% Confidence Interval (p-Value) |
|---|---|---|
| Demographics | ||
| Age | 0.6 | 0.03–1.5 (0.29) |
| Gender | 0.9 | 0.4–1.7 (0.66) |
| Regional | 2.1 | 1.0–4.4 (<0.05) |
| Frequent Sleep Disturbance | 3.1 | 1.5–6.4 (<0.005) |
| Suicidal behaviour History | 4.9 | 2.4–10.3 (<0.005) |
| Current Suicidal ideation | 13.8 | 5.8–32.9 (<0.005) |
| Variable | Odds Ratio | 95% Confidence Interval (p-Value) |
|---|---|---|
| Demographics | ||
| Age | 0.7 | 0.3–1.5 (0.32) |
| Gender | 0.9 | 0.5–1.8 (0.76) |
| Head Injury | 2.3 | 1.2–4.5 (<0.05) |
| Anxiety, Stress and PTSD History | 5.9 | 3.1–11.3 (<0.005) |
| Low CDRISC (Resilience) | 2.5 | 1.4–4.8 (<0.005) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shen, Y.-T.; Radford, K.; Daylight, G.; Cumming, R.; Broe, T.G.A.; Draper, B. Depression, Suicidal Behaviour, and Mental Disorders in Older Aboriginal Australians. Int. J. Environ. Res. Public Health 2018, 15, 447. https://doi.org/10.3390/ijerph15030447
Shen Y-T, Radford K, Daylight G, Cumming R, Broe TGA, Draper B. Depression, Suicidal Behaviour, and Mental Disorders in Older Aboriginal Australians. International Journal of Environmental Research and Public Health. 2018; 15(3):447. https://doi.org/10.3390/ijerph15030447
Chicago/Turabian StyleShen, Yu-Tang, Kylie Radford, Gail Daylight, Robert Cumming, Tony G. A. Broe, and Brian Draper. 2018. "Depression, Suicidal Behaviour, and Mental Disorders in Older Aboriginal Australians" International Journal of Environmental Research and Public Health 15, no. 3: 447. https://doi.org/10.3390/ijerph15030447




