Parents’ Experience and Views of Vaccinating Their Child against Influenza at Primary School and at the General Practice
Abstract
:1. Introduction
- To explore parents’ understanding of the childhood seasonal influenza immunisation programme and possible benefits of participation;
- To explore parents’ experience with the seasonal influenza vaccination for their four to six-year-old child;
- To ascertain parents preferences on the vaccination programme;
- To understand parents’ decision-making process about whether to have their child vaccinated against seasonal influenza or not;
- To ascertain what would make children’s future participation in the influenza immunisation programme more acceptable to non-consenting parents.
2. Methods
2.1. Study Population, Recruitment, and Sampling
2.2. Data Analysis
2.3. Ethics
3. Results
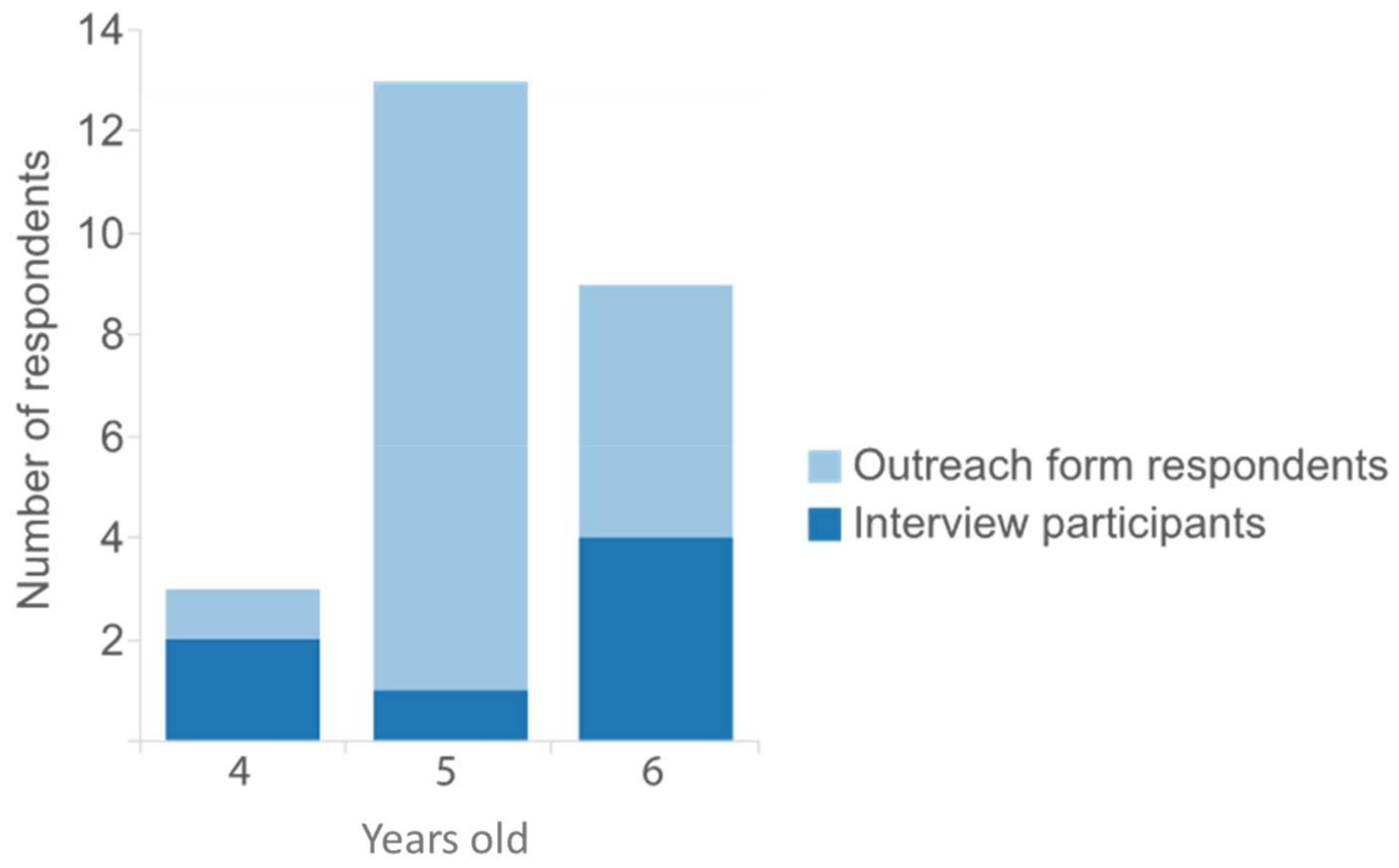
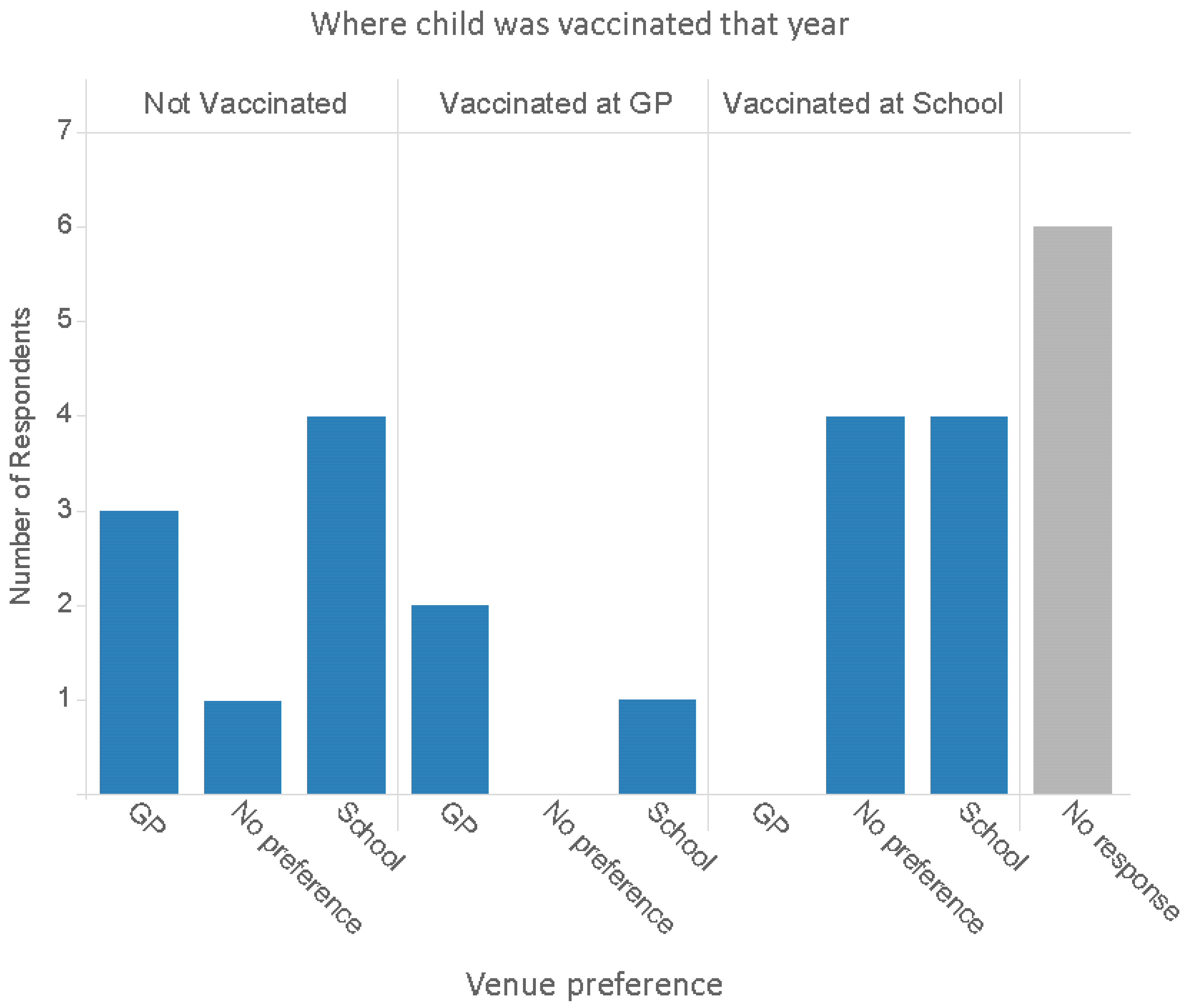
3.1. Descriptive Characteristics
- Parents’ preference for vaccinating in school or at the GP
- Parents’ perceived benefits of vaccinating in school or at the GP
- Parents’ decision-making process about whether or not to have their child vaccinated against seasonal influenza
- ⚬
- Reasons for accepting
- ⚬
- Reasons for refusing
3.2. Venue for Vaccination: School versus GP
“It was inconvenient (at the GP). I work full time, I’m a single parent. So you know, I had to take time out to get them vaccinated… having it done at school is much easier.”(P6 Interview, child vaccinated)
“Usually our GP is quite difficult. You ring up, you’re already like eighth in the queue and you’re waiting 20 min before you get through… then you have got to take your child out of school and get them there (to the GP).”(P23 Interview, child vaccinated)
“At school they all just go in and the child is not going to argue. They are not going to… children play to their parents as well. They know if they give you ‘Oh but mom’ you know you might soften up a little bit and just be like ‘Oh okay, not today’… In school they can’t give you their big sappy eyes and say ‘I want Mummy.’ And it’s just done.”(P4 Interview, child vaccinated)
“At the GP you start now thinking, ‘Please don’t cry. Please don’t show me up, don’t scream the whole place down like you did last year’, and it’s quite a harrowing experience really.”(P23 Interview, child vaccinated)
“I would rather her done at school because her friends are having it done and it’s just less of a drama.”(P6 Interview, child vaccinated)
“He is a little dude at school and he is big and brave in front of his friends, I think if they’re in a queue and they’re all together with their friends, they’d just get on with it…”(P23 Interview, child vaccinated)
“They’re lemmings, literally sheep. They will all do what each other does… it’s quite regimental when you’re at school and it’s more of a confidence thing as well because your friends are doing it.”(P4 Interview, child vaccinated)
“Usual place to get any vaccination.”(P21 Form, child not vaccinated)
“I feel more comfortable with it being done there (at the GP), I know them a lot better.”(P17 Form, child not vaccinated)
“I will say GP, simply because this is the place where kids know they get this treatment or injections, and this is where (the) healing place is, and it might put kids off in school if you start giving vaccinations in school.”(P12 Interview, child not vaccinated)
“Plenty of times going to the GP can be a bit stressful, and you don’t want your child to start to associate pain with the GP visit. So you want, you know, that your children are comfortable in speaking to the doctor, for example, or do you want your child to be hiding from medicine if he’s feeling pain or something because… she doesn’t want to go to the GP.”(P19 Interview, child vaccinated)
“As a parent of course you (want to be there) because you sit at home thinking… ‘My poor baby’. But on the practical side... no. Because they are at school, they are doing what they ‘have to do’, and they can’t pull on anybody’s heart strings… I can imagine this little line of children… and then suddenly a parent is there and ‘Her parent’s there, mine’s not.’ Then that upsets them and they might get nervous and be like ‘I need my mom’.”(P4 Interview, child vaccinated)
“The logistics around (having parents there) that is just a nightmare. You think if they are there with their peers then in theory they should just do it.”(P5 Interview, child not vaccinated)
“I probably would have gone, whether that would have been the right thing to do or not; that was just sort of a mothering instinct really… However, whether that would have backfired on me I don’t know.”(P23 Interview, child vaccinated)
3.3. Reasons for Accepting
“Well I did it for the benefit of my child, because I thought it would benefit my child health-wise. Also if there was the possibility that it would reduce the risk or the blow of full blown flu symptoms, then that is right up there on my list of important things.”(P4 Interview, child vaccinated)
“It can affect your family if… a teacher gets infected and cannot go to school or another kid gets infected… if people start not to vaccinate, that’s a problem… and actually it can spread into the population even if you are vaccinating people.”(P19 Interview, child vaccinated)
“I know this sounds a bit selfish really, but you get to the Christmas holidays and then there’s usually some family that has been hit by flu and that’s Christmas ruined, and we’ve been there. I just think it would ruin a holiday time that we could have been enjoying our family time together and what not, it’s peace of mind that we’re not going to get it...”(P23 Interview, child vaccinated)
“Doctors probably get inundated with people having flu… So if there is something that you can do to stop that epidemic of everybody bombarding the doctors that seems good to me.”(P4 Interview, child vaccinated)
“The doctor reassured me that it’s all been tested and the side effects are minimal and there’s nothing to worry about. Having the Doctors reassurance was like crossing the ‘T’s and dotting the ‘I’s for me. I didn’t actually worry; that was all I needed really.”(P23 Interview, child vaccinated)
“I think I trust the medical profession’s decision really. If they say it’s safe, then that’s good for me… I trust the medical profession to make up the decision as to ‘Yes this is better as opposed to not’.”(P4 Interview, child vaccinated)
“There is obviously a component of balancing risk and benefit. Depends on what kind of vaccination you’re offered too, but obviously it is clear that for some of the diseases you definitely want to be vaccinated.”(P19 Interview, child vaccinated)
“The first time [my child was offered the vaccine] I considered it for a long, long time and I looked it up… I took a few weeks; because obviously you’re wary, you hear horror stories and you don’t know what to trust really… I talked it through with the GP and once I had got her reassurance; I didn’t think about it. I just thought well okay, she knows what she’s doing. She actually did a bit of research for me because it was all quite new to her as well and she printed me off loads of stuff that she had got and sent it to me.”(P23 Interview, child vaccinated)
“Particularly in my daughter’s case I wouldn’t want her to get flu because she has got weakened lungs and things like that… she had actually been in HDU and the hospital advised that we vaccinate her and we vaccinated the whole family.”(P6 Interview, child vaccinated)
“You are weighing it up is what you’re doing; and I’m thinking well, okay, she has got asthma which I have been told it could knock her more for six… and I hadn’t really heard of any side effects or anything happening.”(P23 Interview, child vaccinated)
3.4. Reasons for Refusing
“She is generally in quite good health. I wasn’t sure if it was really necessary.”(P5 Interview, child not vaccinated)
“She is a very healthy girl, who is very rarely poorly, so we chose not to vaccinate.”(P16 Form, child not vaccinated)
“My children rarely get sick.”(P18 Form, child not vaccinated)
“I think if we’d have had a child or somebody else in the house who was immuno-compromised … that would be different but we’re a healthy household, and it [having the vaccine] only seems to be a negative.”(P7 Interview, child not vaccinated)
“Yes, I wanted just more good arguments about why you would do it. If you don’t have a child that gets ill, it does not make any sense to have a flu vaccination, unless it’s like more reasoning say for the school, if it made a big difference to the school the fact that everybody had the vaccination, that would be interesting to know, but I felt that it wasn’t obvious and I couldn’t see any reason to do it.”(P7 Interview, child not vaccinated)
“Because it sounded like something new I wasn’t 100% sure… even though it sounded good I wasn’t 100% sure… I wanted statistics and proof around so many percentage of children didn’t get the flu because of this. I think the thing is you don’t hear of many children actually having the flu. I think that’s the thing. If it was … not an epidemic, but if you knew it was as widespread as a cold or a sickness bug, there is obviously going to be more concrete evidence to prove it was a successful preventative. But because not many children get the flu I suppose it’s difficult to ascertain how successful it would have been. But it would have been nice to maybe find out some more statistics or information.”(P5 Interview, child not vaccinated)
“I believe she should build up her own immunity naturally.”(P25 form, child not vaccinated)
“Nutritional medicine is more effective and healthier than vaccines… Vaccines are unproven and can be toxic.”(P18 form, child not vaccinated)
“Seen too many negative effects from others taking the vaccination.”(P2 form, child not vaccinated)
4. Discussion
4.1. Preferences about Vaccination Venue: School versus GP
4.2. Factors in the Vaccination Decision
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Joint Committee on Vaccination and Immunisation (JCVI). JCVI Statement on the Annual Influenza Vaccination Programme Extension of the Programme to Children. 2012. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/224775/JCVI-statement-on-the-annual-influenza-vaccination-programme-25-July-2012.pdf (accessed on 28 August 2014).
- National Health Service (NHS). Flu Plan—Winter 2014/2015. Available online: https://www.gov.uk/ government/uploads/system/uploads/attachment_data/file/306638/FluPlan2014_accessible.pdf (accessed on 28 August 2014).
- PHE Weekly National Influenza Report—Summary of UK Surveillance of Influenza and other Seasonal Respiratory Illnesses (22 May 2014—Week 21 Report). Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/682855/National_flu_report_wk21_22_May_2014.pdf (accessed on 25 January 2017).
- National Health Service (NHS). Flu Plan—Winter 2015/2016. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/526143/Flu_Plan_Winter_2015_to_2016superseded.pdf (accessed on 31 January 2017).
- Perman, S.; Turner, S.; Ramsay, A.I.G.; Baim-Lance, A.; Utley, M.; Fulop, N.J. School-based vaccination programmes: A systematic review of the evidence on organisation and delivery in high income countries. BMC Pub. Health 2017, 17, 252. [Google Scholar] [CrossRef] [PubMed]
- Paul, P.; Fabio, A. Literature review of HPV vaccine delivery strategies: Considerations for school- and non-school based immunization program. Vaccine 2014, 32, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Pebody, R.G.; Green, H.K.; Andrews, N.; Boddington, N.L.; Hongxin, Z.; Yonova, I.; Ellis, J.; Steinberger, S.; Donati, M.; Elliot, A.J.; et al. Uptake and impact of vaccinating school age children against influenza during a season with circulation of drifted influenza A and B strains, England, 2014/15. Euro Surveill. 2015, 20. [Google Scholar] [CrossRef] [PubMed]
- Boyatizis, R.E. Transforming Qualitative Information: Thematic Analysis and Code Development; Sage: London, UK, 1998. [Google Scholar]
- Strauss, A.; Corbin, J. Basics of Qualitative Research; SAGE: London, UK, 1988. [Google Scholar]
- Herbert, N.L.; Gargano, L.M.; Painter, J.E.; Sales, J.M.; Morfaw, C.; Murray, D.; DiClemente, R.J.; Hughes, J.M. Understanding reasons for participating in a school-based influenza vaccination program and decision-making dynamics among adolescents and parents. Health Educ. Res. 2013, 28, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Siu, W.; Goubert, L. Reducing the burden of pain from vaccination: Updated recommendations for all age groups. Clin. J. Pain 2015, 31, S132–S133. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, S.; Forsner, M.; Finnström, B.; Mörelius, E. Relaxation and guided imagery do not reduce stress, pain and unpleasantness for 11- to 12-year-old girls during vaccinations. Acta Paediatr. 2015, 104, 724–729. [Google Scholar] [CrossRef] [PubMed]
- Gargano, L.M.; Pazol, K.; Sales, J.M.; Painter, J.E.; Morfaw, C.; Jones, L.M.; Weiss, P.; Buehler, J.W.; Murray, D.L.; Wingood, G.M.; et al. Multicomponent Interventions to Enhance Influenza Vaccine Delivery to Adolescents. Pediatrics 2011, 128, e1092–e1099. [Google Scholar] [CrossRef] [PubMed]
- PHE Welcomes Changes to the UK Vaccination Programme. 2013. Available online: https://www.gov.uk/ government/news/phe-welcomes-changes-to-the-uk-vaccination-programme (accessed on 28 August 2014).
- Protecting Your Child against Flu: Information for Parents. 2015. Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/431953/9312_PHE_Protecting_Child_Flu_DL_10_web.pdf (accessed on 8 July 2016).
- Cromer, D.; van Hoek, A.J.; Jit, M.; Edmunds, W.J.; Fleming, D.; Miller, E. The burden of influenza in England by age and clinical risk group: A statistical analysis to inform vaccine policy. J. Infect. 2014, 68, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Wiley, K.E.; Massey, P.D.; Cooper, S.C.; Wood, N.; Quinn, H.E.; Leask, J. Pregnant women’s intention to take up a post-partum pertussis vaccine, and their willingness to take up the vaccine while pregnant: A cross sectional survey. Vaccine 2013, 31, 3972–3978. [Google Scholar] [CrossRef] [PubMed]
- Magazine Advert—Stock up 65+ (2015–2016). 2015. Available online: https://campaignresources.phe.gov.uk/resources/campaigns/34-stay-well-this-winter-2015---2016/resources/1427 (accessed on 12 July 2016).
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paterson, P.; Schulz, W.; Utley, M.; Larson, H.J. Parents’ Experience and Views of Vaccinating Their Child against Influenza at Primary School and at the General Practice. Int. J. Environ. Res. Public Health 2018, 15, 622. https://doi.org/10.3390/ijerph15040622
Paterson P, Schulz W, Utley M, Larson HJ. Parents’ Experience and Views of Vaccinating Their Child against Influenza at Primary School and at the General Practice. International Journal of Environmental Research and Public Health. 2018; 15(4):622. https://doi.org/10.3390/ijerph15040622
Chicago/Turabian StylePaterson, Pauline, Will Schulz, Martin Utley, and Heidi J. Larson. 2018. "Parents’ Experience and Views of Vaccinating Their Child against Influenza at Primary School and at the General Practice" International Journal of Environmental Research and Public Health 15, no. 4: 622. https://doi.org/10.3390/ijerph15040622




