Duty of Notification and Aviation Safety—A Study of Fatal Aviation Accidents in the United States in 2015
Abstract
:1. Background
1.1. Special Features from New Zealand, Norway, Finland and United States
1.2. Germanwings Accident and Safety Recommendations
2. Methods
3. Results
4. Discussion
4.1. Medications and Conditions
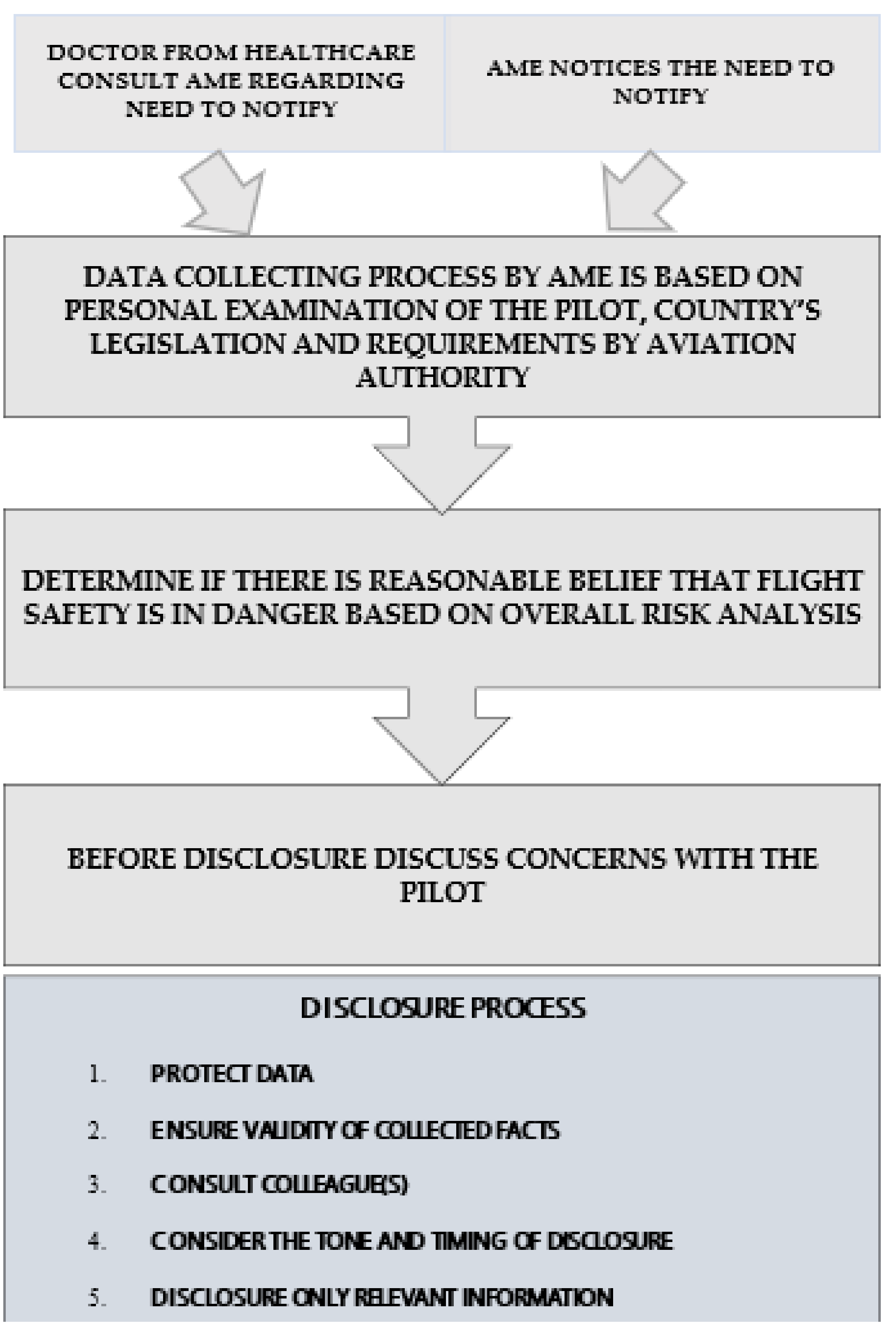
4.2. Timing and Decision Process in Duty of Notification
4.3. Duty of Notification as a Part of Safety Management System (SMS)
4.4. Implications for the Notification System
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Medical Association (WMA). WMA Declaration of Geneva 2018. Available online: https://www.wma.net/policies-post/wma-declaration-of-geneva/ (accessed on 7 April 2018).
- Sankar, P.; Moran, S.; Merz, J.; Jones, N.L. Patient perspectives on medical confidentiality. A review of literature. J. Gen. Intern. Med. 2003, 18, 659–669. [Google Scholar] [CrossRef] [PubMed]
- Federal Aviation Administration (FAA). Pilot Fitness Aviation Rulemaking Committee Report. 2015. Available online: https://www.asma.org/asma/media/AsMA/PDF-News/july-2016/Pilot-Fitness-Aviation-Rulemaking-Committee-Report.pdf (accessed on 12 May 2018).
- Griffiths, R. Doctors and the transport sector. In Cole’s Medical Practice in New Zealand, 13th ed.; Morris, K.A., Ed.; Medical Council of New Zealand: Wellington, New Zeland, 2017; Chapter 33. [Google Scholar]
- Finnish Safety Investigation Authority. Pilot Incapacitation during Landing at Vampula Aerodrome on 24 September 2016. 2017. Available online: http://www.turvallisuustutkinta.fi/material/attachments/otkes/tutkintaselostukset/en/ilmailuonnettomuuksientutkinta/2016/d0tdxocRT/L2016-01_final_report_.pdf (accessed on 5 April 2018).
- Finnish Safety Investigation Authority. Ultralight Airplane Accident in Sysmä. 2013. Available online: http://www.turvallisuustutkinta.fi/en/index/tutkintaselostukset/ilmailuonnettomuuksientutkinta/tutkintaselostuksetvuosittain/ilmailu2013/l2013-03ultralightairplaneaccidentinsysma3.5.2013.html (accessed on 5 April 2018).
- Bureau d’Enquêtes et d’Analyses France (BEA). Germanwings Accident Investigation. 2016. Available online: https://www.bea.aero/uploads/tx_elydbrapports/BEA2015-0125.en-LR.pdf (accessed on 27 February 2018).
- Rieder, P.; Louis-Courvoisier, M.; Huber, P. The end of medical confidentiality? Patients, physicians and the state in history. Med. Hum. 2016, 42, 149–154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- European Aviation Safety Authority (EASA). EASA’s Response to the Germanwings Flight 9525 Accident. 2016. Available online: https://www.easa.europa.eu/easa-and-you/aircrew-and-medical/follow-up-germanwings-flight-9525-accident#0 (accessed on 5 April 2018).
- Vuorio, A.; Laukkala, T.; Navathe, P.; Budowle, B.; Sajantila, A. On doctor’s accountability and flight deck safety. Croat. Med. J. 2015, 56, 385–386. [Google Scholar] [CrossRef] [PubMed]
- National Transportation Safety Board Office of Public Affairs. NTSB Study on Drug Use in Aviation Shows Upward Trend in Use of Potentially Impairing Medications; First Step in Understanding Drug Use and Accident Risk; Federal Information & News Dispatch, Inc.: Washington, DC, USA, 2014. [Google Scholar]
- National Transportation Safety Board (NTSB). Accident Database and Synopsis. 2018. Available online: http://www.ntsb.gov/aviationquery/index.aspx (accessed on 6 March 2018).
- Federal Aviation Authority. Guide for Aviation Medical Examiners. Decision Consideration—Aerospace Medical Dispositions. Item 47. Psychiatric Conditions—Use of Antidepressants. 2018a. Available online: www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/app_process/exam_tech/item47/amd/antidepressants (accessed on 11 April 2018).
- Vuorio, A.; Asmayawati, S.; Budowle, B.; Griffiths, R.; Strandberg, T.; Kuoppala, J.; Sajantila, A. General aviation pilots over 70 years old. Aerosp. Med. Hum. Perform. 2017, 88, 142–145. [Google Scholar] [CrossRef] [PubMed]
- Federal Aviation Authority. Guide for Aviation Medical Examiners. 2018c. Available online: https://www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/media/guide.pdf (accessed on 7 April 2018).
- Vuorio, A.; Laukkala, T.; Navathe, P. Major depression and fitness to fly by different aviation authorities. Aviat. Space Environ Med. 2012, 83, 909–911. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. NICE Clinical Guidelines [CG72]. Available online: www.nice.org.uk (accessed on 5 April 2018).
- Federal Aviation Authority. Guide for Aviation Medical Examiners. Decision Considerations Disease Protocols—Attention/Deficit Hyperactivity Disorder. 2018c. Available online: www.faa.gov/about/office_org/headquarters_offices/avs/offices/aam/ame/guide/dec_cons/disease_prot/adhd/ (accessed on 7 April 2018).
- Laukkala, T.; Bor, R.; Budowle, B.; Sajantila, A.; Navathe, P.; Sainio, M.; Vuorio, A. Attention-deficit/hyperactivity disorder and fatal accidents in aviation medicine. Aerosp. Med. Hum. Perform. 2017, 88, 871–875. [Google Scholar] [CrossRef] [PubMed]
- Vuorio, A.; Laukkala, T.; Navathe, P.; Budowle, B.; Eyre, A.; Sajantila, A. Aircraft-assisted pilot suicides: Lessons to be learned. Aviat. Space Environ. Med. 2014, 85, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Vuorio, A.; Laukkala, T.; Navathe, P.; Budowle, B.; Bor, R.; Sajantila, A. Bipolar disorder in aviation medicine. Aerosp. Med. Hum. Perform. 2017, 88, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Australian Civil Aviation Authority (CASA). Grounding, DAME Consultation and CASA Notification. Available online: https://www.casa.gov.au/licences-and-certification/aviation-medicine/grounding-dame-consultation-and-casa-notification (accessed on 1 April 2018).
- Vaughan, D. The Challenger Launch Decision: Risky Technology, Culture, and Deviance at NASA; University of Chicago Press: Chicago, IL, USA, 1996. [Google Scholar]
- Hsu, Y.; Li, W.; Chen, K. Structuring critical success factors of airline safety management system using a hybrid model. Transp. Res. Part E 2010, 46, 222–235. [Google Scholar] [CrossRef]
- Lofquist, E.A. The art of measuring nothing: The paradox of measuring safety in a changing civil aviation industry using traditional safety metrics. Saf. Sci. 2010, 48, 1520–1529. [Google Scholar] [CrossRef] [Green Version]
- Niveau, G.; Burkhardt, S.; Chiesa, S. Medical confidentiality and the competent patient. J. Med. Ethics 2013, 39, 686–689. [Google Scholar] [CrossRef] [PubMed]
- Crook, M.A. The risks of absolute medical confidentiality. Sci. Eng. Ethics 2013, 19, 107–122. [Google Scholar] [CrossRef] [PubMed]
- Choong, K.A.; Bonnici, J.P.M. Posthumous medical confidentiality. Eur. J. Comp. Law Gov. 2014, 1, 106–119. [Google Scholar] [CrossRef]
| Country | Policy |
|---|---|
| Norway | Duty of notification covering all doctors since 1982 |
| New Zealand | Duty of notification covering all doctors since 2003. Practical protocol created and implemented |
| Finland | Bill of reform that duty of notification will cover all doctors |
| United States | Notification responsibilities vary state by state |
| Accident Date, State, Pilot Age (Years), Gender (M = Male), No. of Deceased | Last Medical Certification and Comments * | Reason of Incompatibility with Flying | NTSB Cause of Accident |
|---|---|---|---|
| 11 December 2015, PA 68, M 3 | 02/22/2014 Class 3 | Amphetamine | The pilot’s failure to maintain control of the airplane after a cabin door came open in flight. Contributing to the accident was the pilot’s misuse of amphetamine. |
| 6 December 2015, MO 40, M 2 | 05/26/2012 Class 3 Convictions for driving under the influence, possession of a controlled substance thrice, reported last using methamphetamines 2011. | Methamphetamine | The non-instrument-rated pilot’s loss of control due to spatial disorientation. Contributing to the accident was the pilot’s use of methamphetamine, which impaired his decision-making abilities. |
| 18 November 2015, CA 65, M 2 | 01/19/2015 Class 3 Pilot reported hypertension and the use of medications including nebivolol, pantoprazole and rosuvastatin. | Alprazolam diphenhydramine | The pilot’s loss of control during landing on a dolly. Contributing were the pilot’s decision to conduct the flight without an instructor despite recommendations, failure to land on the ramp when there was difficulty landing on the dolly, and his impaired decision-making, judgment, and psychomotor performance, due to use of two psychoactive drugs. |
| 9 November 2015, GA 40, M 2 | 05/07/2013 Class 3 | Amphetamine (possible medical use), tramadol, cetirizine, doxylamine, marihuana, ethanol ingested or post-mortem | The pilot’s loss of airplane control due to spatial disorientation. Also causal to the accident was the pilot’s impairment by the combined effects of multiple medications and drugs. |
| 9 November 2015, CO 63, M 2 | 11/04/2013 Class 3 Pilot reported the use of rosuvastatin and niacin. | Sertraline, diphenhydramine, cetirizine, marihuana | The pilot’s loss of airplane control in high density altitude conditions, which resulted in an inadvertent stall. Contributing was the pilot’s impaired performance due to his use of potentially impairing medications. |
| 17 October 2015, CA 71, M 2 | 01/01/2014 Class 3 Pilot reported hypertension treated with atenolol and amlodipine | Quetiapine, hydrocodone | The non-instrument-rated pilot’s improper inflight decision-making to attempt to outclimb clouds along his planned route, which resulted in his inadvertent entry into instrument meteorological conditions, spatial disorientation, and a loss of control. The pilot’s preexisting medical conditions and his use of impairing medications contributed to his degraded performance. |
| 2 September 2015, TN 66, M 1 | 06/10/2015 Class 2 | Autopsy: scarring due to recent heart attacks. | The pilot’s incapacitation from complications of a recent heart attack, which resulted in a loss of control during cruise flight. |
| 16 August 2015, NY 59, M 1 | 12/22/2014 Class 2 | Amphetamine (possible medical use), oxycodone oxymorphone, clonazepam | Decision to delay turning after engine failure, and controller provided erroneous info. Contributing were (1) the FAA’s lack of requirement to validate radar video maps, (2) the failure of the engine crankshaft due to a bearing shift, (3) the pilot’s impairment due to amphetamine abuse and underlying medical condition(s). |
| 1 August 2015, AR 38 M 1 | 01/23/2015 Class 2 Pilot reported a previous eye problem, surgery, and earlier hospitalization related to a vehicle crash | Buprenorfine, diphenhydramine | The pilot’s inability to maintain control of the airplane as a result of incapacitation by drug effects or an acute cardiac event. |
| 4 July 2015, TX 28, M 2 | 07/18/2014 Class 2 | Alprazolam, hydrocodone, ethanol, evidence on cocaine withdrawal | The pilot’s low-altitude aerobatic display, which resulted in an aerodynamic stall/spin when he exceeded the airplane’s critical angle of attack. Contributing to the accident was the pilot’s impairment due to alcohol and drugs. |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vuorio, A.; Budowle, B.; Sajantila, A.; Laukkala, T.; Junttila, I.; Kravik, S.E.; Griffiths, R. Duty of Notification and Aviation Safety—A Study of Fatal Aviation Accidents in the United States in 2015. Int. J. Environ. Res. Public Health 2018, 15, 1258. https://doi.org/10.3390/ijerph15061258
Vuorio A, Budowle B, Sajantila A, Laukkala T, Junttila I, Kravik SE, Griffiths R. Duty of Notification and Aviation Safety—A Study of Fatal Aviation Accidents in the United States in 2015. International Journal of Environmental Research and Public Health. 2018; 15(6):1258. https://doi.org/10.3390/ijerph15061258
Chicago/Turabian StyleVuorio, Alpo, Bruce Budowle, Antti Sajantila, Tanja Laukkala, Ilkka Junttila, Stein E. Kravik, and Robin Griffiths. 2018. "Duty of Notification and Aviation Safety—A Study of Fatal Aviation Accidents in the United States in 2015" International Journal of Environmental Research and Public Health 15, no. 6: 1258. https://doi.org/10.3390/ijerph15061258





