A Systematic Review of Arsenic Exposure and Its Social and Mental Health Effects with Special Reference to Bangladesh
Abstract
:1. Introduction
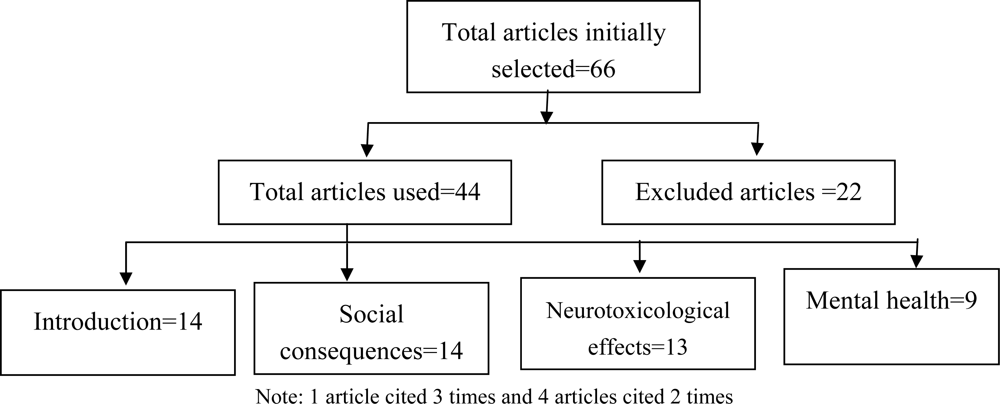
2. Methods
3. Results and Discussion
3.1. Social Hazards and Poverty
3.2. Social Instability
3.3. Ostracism and Marriage Related Problems
3.4. Superstition
3.5. Neurotoxicological Effects
3.6. Mental Health
4. Conclusions
Acknowledgments
References
- Vahidnia, A; van der Voet, GB; de Wolff, FA. Arsenic neurotoxicity – A review. Hum. Exp. Toxicol 2007, 26, 823–832. [Google Scholar]
- WHO. Arsenic and Arsenic Compounds International Programme on Chemical Safety; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- IARC. Some drinking water disinfectants and Contaminants, including Arsenic; International Agency for Research on Cancer: Lyon, France, 2004; Volume 84. [Google Scholar]
- BGS; DPHE. Arsenic contamination of groundwater in Bangladesh. In Summary British Geological Survey WC/00/19; Kinniburgh, DG, Smedley, PL, Eds.; British Geological Survey: Keyworth, UK, 2001; Volume 1, pp. 1–15. [Google Scholar]
- Khan, MMH; Sakauchi, F; Sonoda, T; Washio, M; Mori, M. Magnitude of arsenic toxicity in tube-well drinking water in Bangladesh and its adverse effects on human health including cancer: evidence from a review of the literature. Asian Pac. J. Cancer Prev 2003, 4, 7–14. [Google Scholar]
- Chowdhury, AMR. Arsenic crisis in Bangladesh. Sci. Am 2004, 291, 86–91. [Google Scholar]
- Khan, MMH; Hossain, MK; Kobayashi, K; Sakauchi, F; Yamashita, T; Feroze Ahmed, M; Delwar Hossain, M; Quamruzzaman, Q; Mori, M. Levels of blood and urine chemicals associated with longer duration of having arsenicosis in Bangladesh. Int. J. Environ. Health Res 2005, 15, 289–301. [Google Scholar]
- Mukherjee, A; Sengupta, MK; Hossain, MA; Ahamed, S; Das, B; Nayak, B; Lodh, D; Rahman, MM; Chakraborti, D. Arsenic contamination in groundwater: a global perspective with emphasis on the Asian scenario. J. Health Popul. Nutr 2006, 24, 142–163. [Google Scholar]
- Nasreen, M. Social impacts of arsenicosis. In Arsenic contamination: Bangladesh Perspective; Ahmed, MF, Ed.; ITN-Bangladesh: Dhaka, Bangladesh, 2003; pp. 340–353. [Google Scholar]
- Khan, MMH; Aklimunnessa, K; Kabir, M; Mori, M. Determinants of drinking arsenic-contaminated tubewell water in Bangladesh. Health Policy Plann 2007, 22, 335–343. [Google Scholar]
- Safiullah, S. Arsenic pollution in the groundwater in Bangladesh; an overview. Asian J. Water Environ. Pollut 2006, 4, 47–59. [Google Scholar]
- Khan, MMH; Aklimunnessa, K; Kabir, M; Mori, M. Case-control study of arsenicosis in some arsenic contaminated villages of Bangladesh. Sapporo Med. J 2006, 75, 51–61. [Google Scholar]
- Spallholz, JE; Boylan, LM; Rahman, MM. Environmental hypothesis: is poor dietary selenium intake an underlying factor for arsenicosis and cancer in Bangladesh and West Bengal, India? Sci. Total Environ 2004, 323, 21–32. [Google Scholar]
- Havenaar, JM; van den Brink, W. Psychological factors affecting health after toxicological disasters. Clin. Psychol. Rev 1997, 17, 359–374. [Google Scholar]
- Hassan, MM; Atkins, PJ; Dunn, CE. Social implications of arsenic poisoning in Bangladesh. Soc. Sci. Med 2005, 61, 2201–2211. [Google Scholar]
- Bhuiyan, RH; Islam, N. Coping strategy and health seeking behavior of arsenicosis patients of rural Bangladesh: a case study of Ramganj upzilla, Lakshmipur. Presented at the International Workshop on Arsenic Mitigation, Dhaka, Bangladesh, January 14–16, 2002.
- Health Geneva, WHO. Towards an Assessment of the socioeconomic impact of arsenic poisoning in Bangladesh Protection of the Human Environment; World Health Organization, Water, Sanitation and Health: Geneva, Switzerland, 2000. [Google Scholar]
- Chowdhury, MAI; Uddin, MT; Ahmed, MF; Ali, MA; Rasul, SMA; Hoque, MA; Alam, R; Sharmin, R; Uddin, SM; Islam, MS. Collapse of Socio-economic base of Bangladesh by arsenic contamination in groundwater. Pakistan J. Biol. Sci 2006, 9, 1617–1627. [Google Scholar]
- Argos, M; Parvez, F; Chen, Y; Hussain, I; Momotaj, H; Howe, GR; Graziano, JH; Ahsan, H. Socioeconomic Status and Risk for Arsenic-Related Skin Lesions in Bangladesh. Am. J. Public Health 2007, 97, 825–831. [Google Scholar]
- Sarker, PC. Beliefs and arsenicosis and their impact on social disintegration in Bangladesh: Challenges to social work interventions. In Proceedings of Joint Conference of AASW, IFSW, AASW and AAWWF; Brisbane: Australia, 1999; pp. 217–221. [Google Scholar]
- Tsutsumi, A; Izutsu, T; Islam, MDA; Amed, JU; Nakahara, S; Takagi, F; Wakai, S. Depressive status of leprosy patients in Bangladesh: Association with self-perception of stigma. Leprosy Rev 2004, 75, 57–66. [Google Scholar]
- Grunner, M. Leprosy and human dignity. In Cultural and Environmental Dimension of Health; Chaudhury, B, Ed.; Inter-India Publications: New Delhi, India, 1990; pp. 114–123. [Google Scholar]
- Sarker, PC; Mohiudin, MD. Arsenic poisoning and its impact on the socio-economic and cultural life of the people of Bangladesh. South Asian Anthropol 2002, 2, 97–102. [Google Scholar]
- Keya, MK. Mental health of arsenic victims in Bangladesh. South African Anthropol 2004, 4, 215–223. [Google Scholar]
- Hadi, A. Fighting arsenic at the grassroots: experience of BRAC`s community awareness initiative in Bangladesh. Health Policy Plann 2003, 18, 83–100. [Google Scholar]
- Paul, BK. Arsenic contamination awareness among the rural residents in Bangladesh. Soc. Sci. Med 2004, 59, 1741–1755. [Google Scholar]
- Rosado, JL; Ronquillo, D; Kordas, K; Rojas, O; Alatorre, J; Lopez, P; Garcia-Vargas, G; Caamano, MC; Cebrian, ME; Stoltzfus, R. Arsenic exposure and cognitive performance in mexican schoolchildren. Environ. Health Perspect 2007, 155, 1371–1375. [Google Scholar]
- Morton, WE; Caron, GA. Encephalopathy: An uncommon manifestation of workplace arsenic poisoning? Am. J. Ind. Med 1989, 15, 1–5. [Google Scholar]
- Calderon, J; Navarro, ME; Jiminez-Capdeville, ME; Santos-Diaz, MA; Golden, A; Rodriguez-Leyva, I; Borja-Aburto, V; Diaz-Barriga, F. Exposure to arsenic and lead and neuropsychological development in Mexican children. Environ. Res 2001, 85, 69–76. [Google Scholar]
- Tsai, S-Y; Chou, H-Y; The, HW; Chen, C-M; Chen, C-J. The effects of chronic arsenic exposure on the neurobehavioral development in adolescence. NeuroToxicology 2003, 24, 747–753. [Google Scholar]
- Wasserman, GA; Liu, X; Parvez, F; Ahsan, H; Factor-Litvak, P; Kline, J; van Geen, A; Slavkovich, V; Lolacono, NJ; Cheng, Z; Hussain, I; Momtaj, H; Graziano, JH. Water arsenic exposure and children’s intellectual function in Araihazar, Bangladesh. Environ. Health Perspect 2004, 112, 1329–1333. [Google Scholar]
- Von Ehrenstein, OS; Poddar, S; Yuan, Y; Mazumder, DG; Eskenazi, B; Basu, A; Hira-Smith, M; Ghosh, N; Lahiri, S; Haque, R; Ghosh, A; Kalman, D; Das, S; Smith, AH. Children’s intellectual function in relation to arsenic exposure. Epidemiology 2007, 18, 44–51. [Google Scholar]
- Wasserman, GA; Liu, X; Parvez, F; Ahsan, H; Factor-Litvak, P; Kline, J; van Geen, A; Slavkovich, V; Lolacono, NJ; Levy, D; Cheng, Z; Graziano, JH. Water arsenic exposure and intellectual function in 6-year-old children in Araihazar, Bangladesh. Environ. Health Perspect 2007, 115, 285–289. [Google Scholar]
- Goldman, LR; Koduru, S. Chemicals in the environment and developmental toxicity to children: a public health and policy perspective. Environ. Health Perspect 2000, 108, 443–448. [Google Scholar]
- Schroeder, SR. Mental retardation and development disabilities influenced by environmental neurotoxic insults. Environ. Health Perspect 2000, 108, 395–399. [Google Scholar]
- Agency for toxic substances disease registry (ATSDR). Toxicological profile for arsenic; U.S. Department of Health and Human Services: Atlanta, GA, USA, 2007. [Google Scholar]
- Genuis, SJ. Toxicant exposure and mental health-individual, social, and public health consequences. J. Forensic Sci 2009, 54, 474–477. [Google Scholar]
- Siripitayakunkit, U; Visudhiphan, P; Pradipasen, M; Vorapongsathron, T. Association between chronic arsenic exposure and children’s intelligence in Thailand. In Arsenic Exposure and Health Effects; Chappell, WR, Abernathy, CO, Calderon, RL, Eds.; Elsevier Science: Amsterdam, The Netherlands, 1999; pp. 141–149. [Google Scholar]
- Asadullah, MN; Chaudhury, N. Poisoning the Mind: Arsenic Contamination and Cognitive Achievement of Children.
- Taylor, SE; Aspingwall, LG. Psychological aspects of chronic illness. In Psychological Aspects of Serious Illness; Bos, V, Costa, PT, Jr, Eds.; American Psychological Association: Washington, DC, USA, 1990. [Google Scholar]
- Asuki, N. Mental Health Effects following Manmade Toxic Disasters: The Sarin Attack and the Arsenic Poisoning Case; Prehospital and Disaster Medicine, Department of Social Psychiatry, Tokyo Institute of Psychiatry: Tokyo, Japan, 2003. [Google Scholar]
- Zierold, MK; Knobeloch, L; Anderson, H. Prevalence of Chronic Diseases in Adults Exposed to Arsenic-Contaminated Drinking Water. Am. J. Public Health 2004, 94, 1936–1937. [Google Scholar]
- Fujino, Y; Guo, X; Liu, J; You, L; Miyatake, M; Yoshimura, T. Japan Inner Mongolia Arsenic Pollution (JIAMP) Study group. Mental health burden amongst inhabitants of an arsenic-affected area in Inner Mongolia, China. Soc. Sci. Med 2004, 59, 1969–1973. [Google Scholar]
- Martinez, EJ; Kolb, BL; Bell, A. Moderate perinatal arsenic exposure alters neuroendocrine markers associated with depression and increases depressive-like behaviours in adult mouse offspring. Neurotoxicology 2008, 29, 647–655. [Google Scholar]
| Authors and years of publication | Sample size (target population) and study design | Main results |
|---|---|---|
| Rosado et al. [27]. | n=602 (6–8 years old school children in Mexico); Cross-sectional | Arsenic affected children’s cognitive development after adjusting for age, sex, mother’s education and hemoglobin concentration and so on. |
| Wasserman et al. [33]. | n=301 (6 years old children in Bangladesh); Cross-sectional | Arsenic exposure was negatively associated with children intellectual level after adjusting for many potential variables. |
| Wasserman et al. [31]. | n=201 (10 years old children in Bangladesh); Cross-sectional | Arsenic exposure was negatively associated with children intellectual level after adjusting for many potential variables. |
| Tsai et al. [30]. | n=109 (School adolescents with an average age of 14 years in Taiwan); Case-control | Neurobehavioral development like pattern memory and switching attention were significantly affected by long-term exposure to arsenic after adjusting for education and sex. |
| von Ehrenstein et al. [32]. | n=351 (5 to 15 years old children from the source population in West Bengal, India); Cross-sectional | Current arsenic concentrations in urine were associated with small decrements in intellectual testing in school-aged children. |
| Calderon et al. [29]. | n=80 (6 to 9 years School children in Mexico); Cross-sectional | Higher level of urinary arsenic had negative influences on CNS function like verbal comprehension, long-term memory and attention. |
| Asadullah and Chaudhury [39]. | n=7,710 (Secondary school children (enrolled in grade 8) in Bangladesh); Cross-sectional | Cognitive development of children is significantly negatively affected by arsenic. |
© 2009 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Brinkel, J.; Khan, M.H.; Kraemer, A. A Systematic Review of Arsenic Exposure and Its Social and Mental Health Effects with Special Reference to Bangladesh. Int. J. Environ. Res. Public Health 2009, 6, 1609-1619. https://doi.org/10.3390/ijerph6051609
Brinkel J, Khan MH, Kraemer A. A Systematic Review of Arsenic Exposure and Its Social and Mental Health Effects with Special Reference to Bangladesh. International Journal of Environmental Research and Public Health. 2009; 6(5):1609-1619. https://doi.org/10.3390/ijerph6051609
Chicago/Turabian StyleBrinkel, Johanna, Mobarak H. Khan, and Alexander Kraemer. 2009. "A Systematic Review of Arsenic Exposure and Its Social and Mental Health Effects with Special Reference to Bangladesh" International Journal of Environmental Research and Public Health 6, no. 5: 1609-1619. https://doi.org/10.3390/ijerph6051609





