Novel Dental Adhesive with Biofilm-Regulating and Remineralization Capabilities
Abstract
:1. Introduction
2. Results
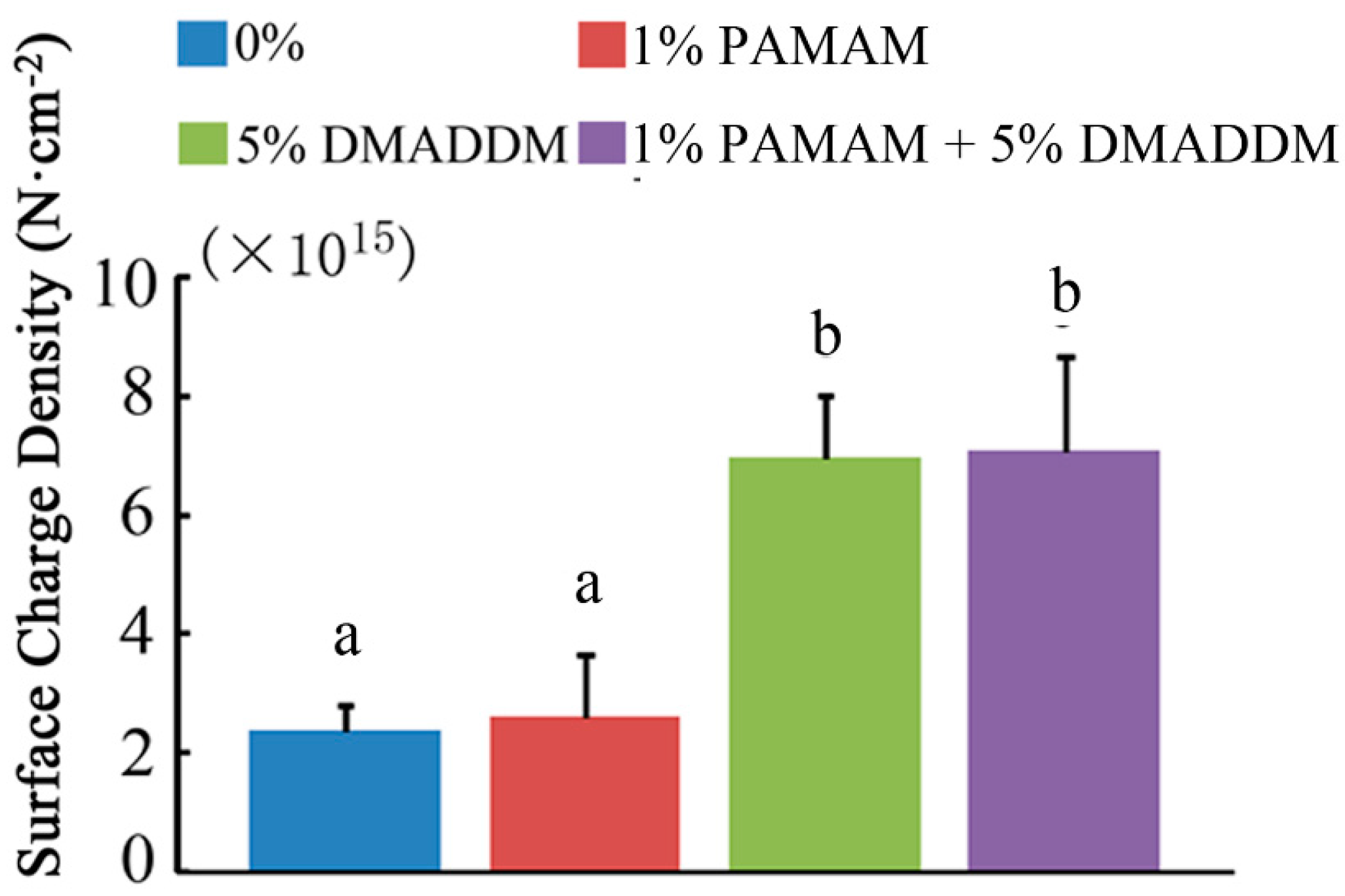
2.1. Microtensile Bond Strength Test and Surface Charge Density
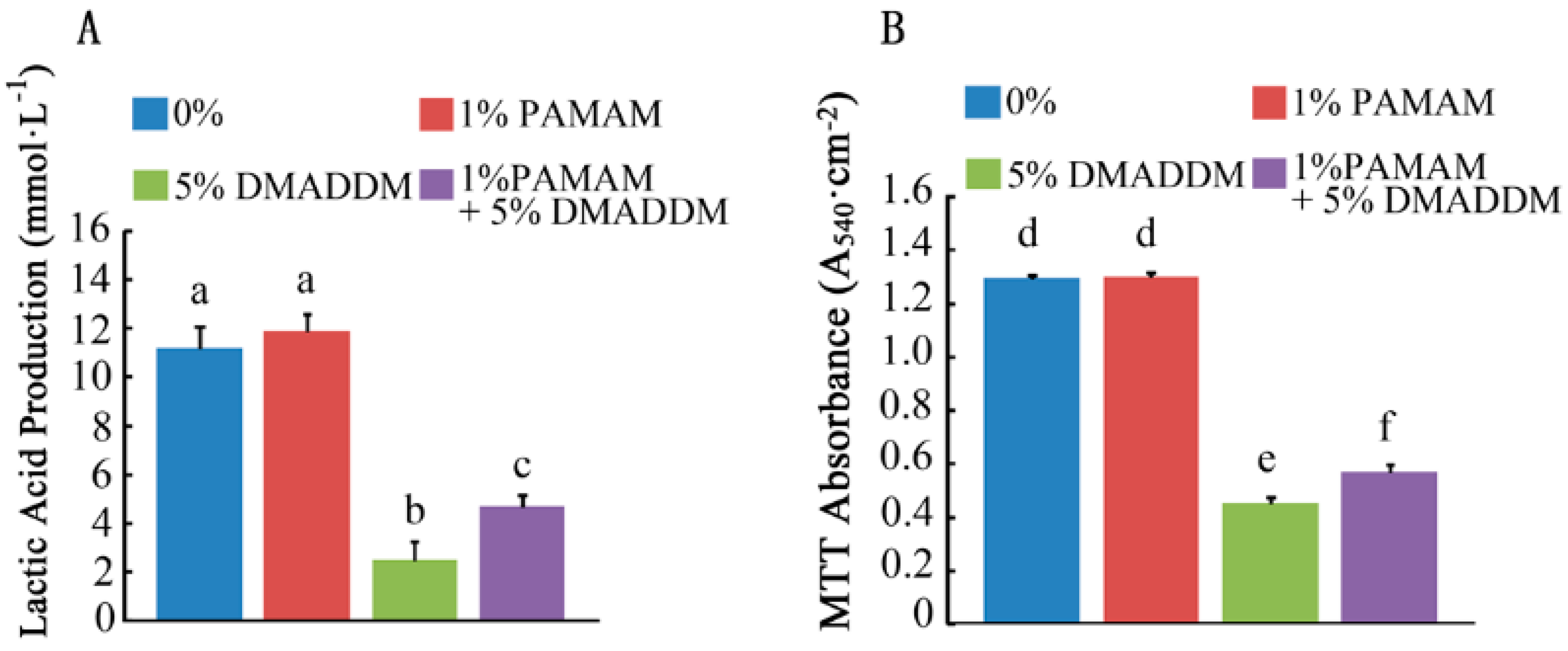
2.2. Lactic Acid Measurement and MTT Assay
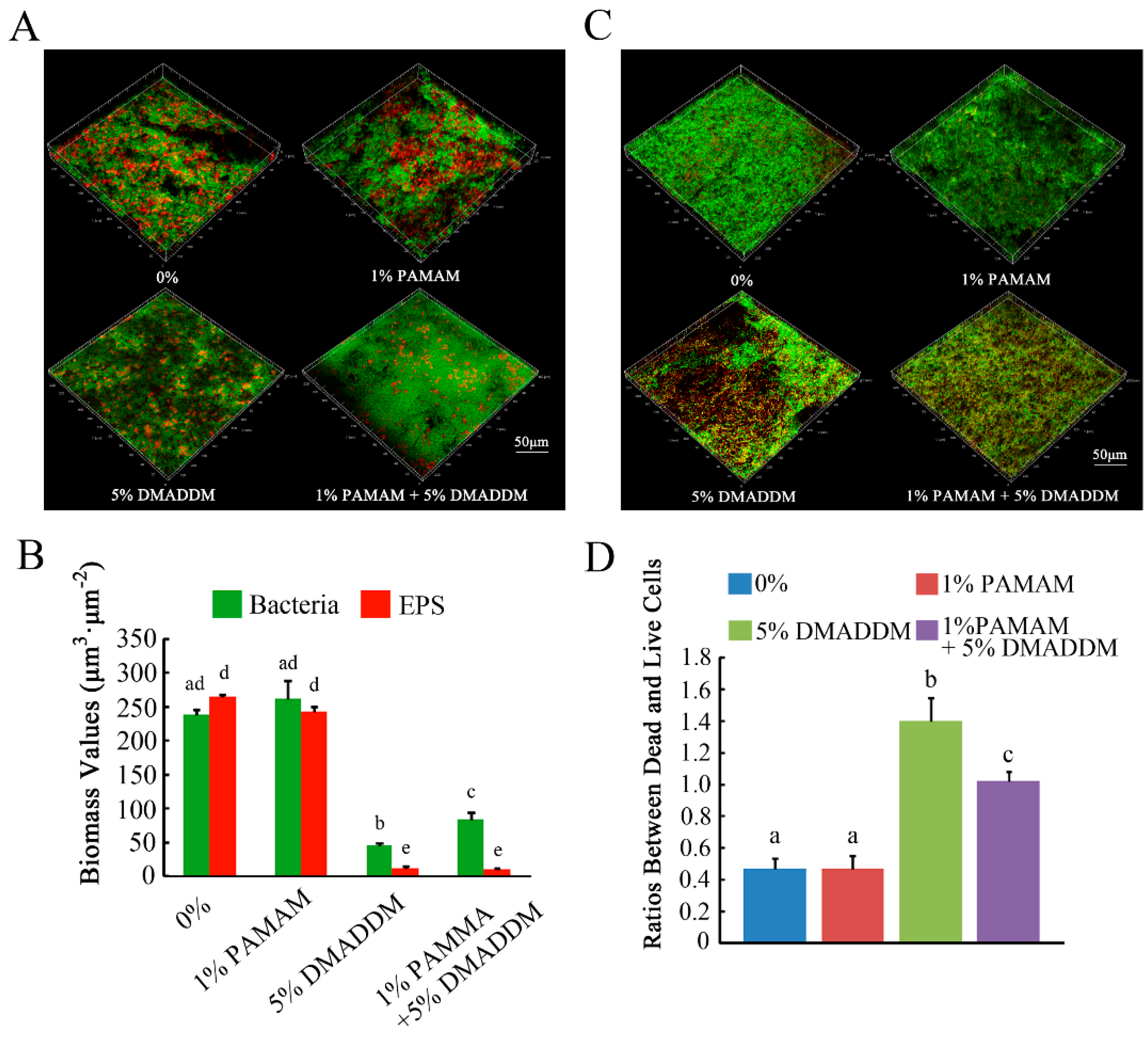
2.3. Live/Dead Bacteria Staining and Exopolysaccharide (EPS) Staining
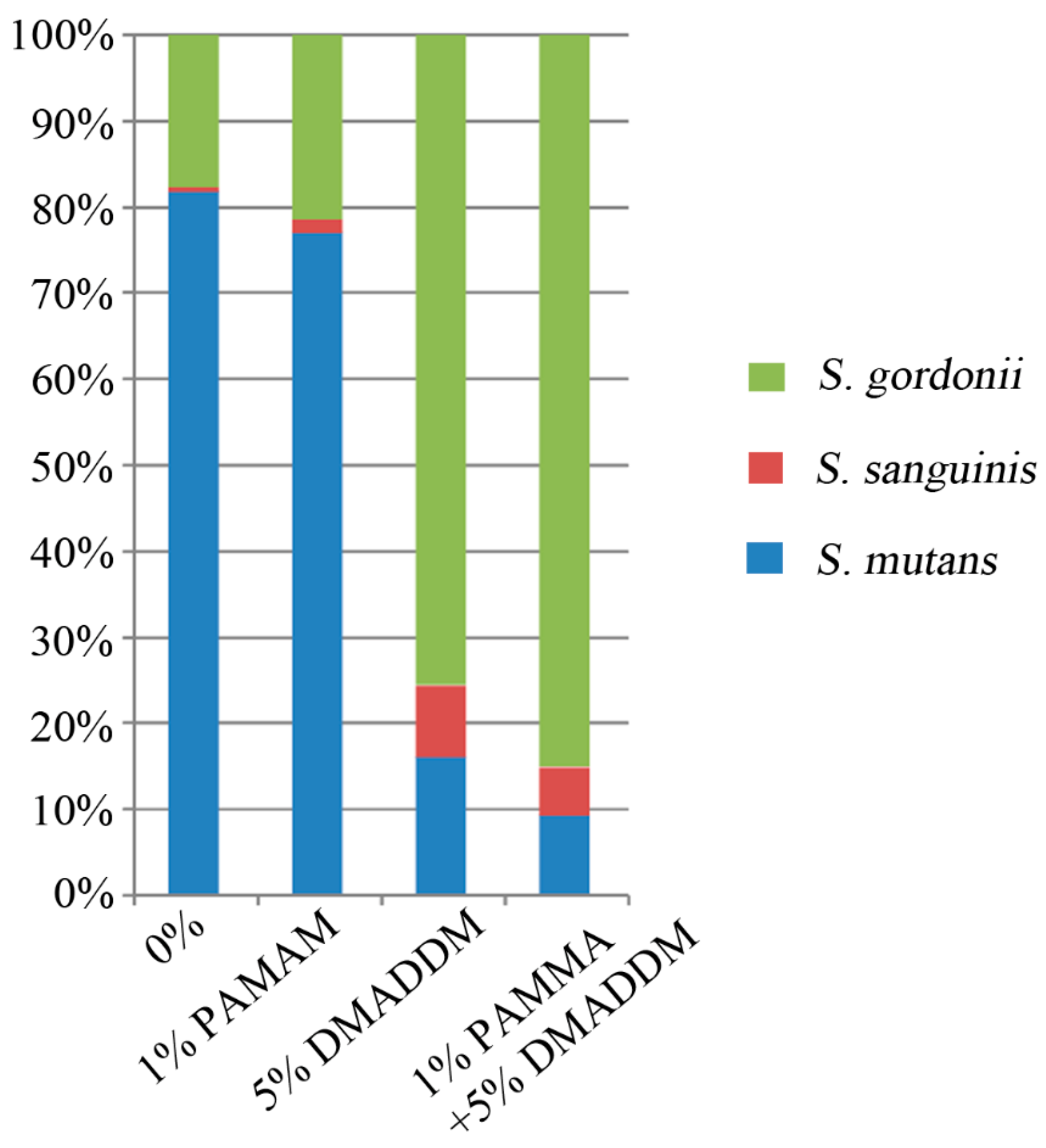
2.4. Real-Time Polymerase Chain Reaction (RT-PCR)
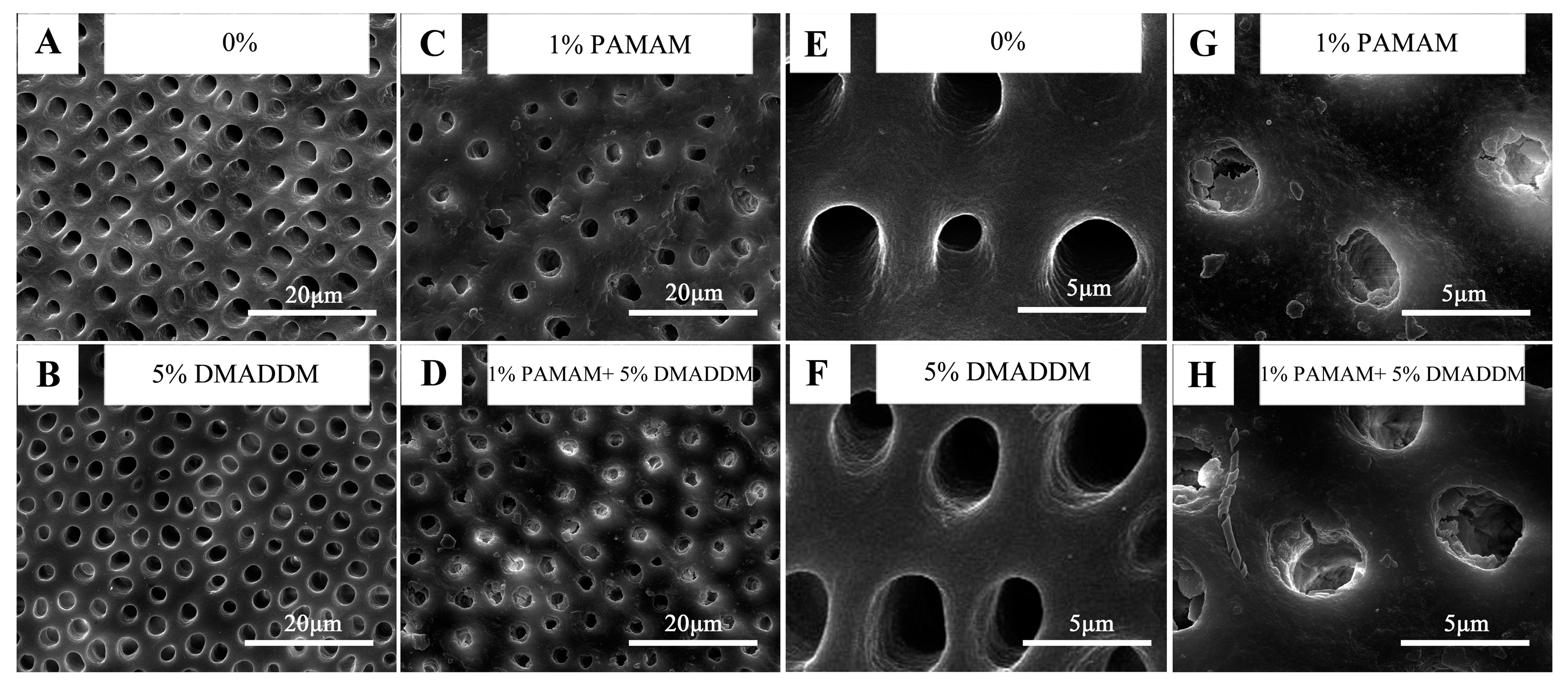
2.5. Remineralization Effect Observed by Scanning Electron Microscope (SEM)
3. Discussion
4. Materials and Methods
4.1. Synthesis of DMADDM and Specimen Preparation for Biofilm Experiments
- (1)
- Clearfil SE Bond control adhesive A (0%, control),
- (2)
- A + 1% PAMAM (1% PAMAM),
- (3)
- A + 5% DMADDM (5% DMADDM),
- (4)
- A + 5% DMADDM + 1% PAMAM (1% PAMAM + 5% DMADDM).
4.2. Microtensile Bond Strength Test
4.3. Surface Charge Density Test
4.4. Bacteria Incubation and Biofilm Formation
4.5. Lactic Acid Measurement and MTT Assay
4.6. EPS Staining and Live/Dead Bacteria Staining
4.7. SEM Observation
4.8. DNA Isolation and Real-Time Polymerase Chain Reaction
4.9. Statistical Analysis
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Imazato, S. Antibacterial properties of resin composites and dentin bonding systems. Dent. Mater. 2003, 6, 449–457. [Google Scholar] [CrossRef]
- Mmond, J.L. Degradation, fatigue, and failure of resin dental composite materials. J. Dent. Res. 2008, 87, 710–719. [Google Scholar]
- Selwitz, R.H.; Ismail, A.I.; Pitts, N.B. Dental caries. Lancet 2007, 369, 51–59. [Google Scholar] [CrossRef]
- Bunek, S.S. Using minimally invasive techniques for the management and detection of dental caries. J. Cosmet. Dent. 2014, 1, 138. [Google Scholar]
- Martinez-Gutierrez, F.; Boegli, L.; Agostinho, A.; Sánchez, E.M.; Bach, H.; Ruiz, F.; James, G. Anti-biofilm activity of silver nanoparticles against different microorganisms. Biofouling 2013, 29, 651–660. [Google Scholar] [CrossRef] [PubMed]
- Behnke, S.; Camper, A.K. Chlorine dioxide disinfection of single and dual species biofilms, detached biofilm and planktonic cells. Biofouling 2012, 28, 635–647. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.; Wang, S.; Zhou, X.; Wang, H.; Xu, H.H.K.; Cheng, L. The use of quaternary ammonium to combat dental caries. Materials 2015, 8, 3532–3549. [Google Scholar] [CrossRef] [PubMed]
- Imazato, S. Bio-active restorative materials with antibacterial effects: New dimension of innovation in restorative dentistry. Dent. Mater. J. 2009, 28, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Weir, M.D.; Zhang, K.; Wu, E.J.; Xu, S.M.; Zhou, X.; Xu, H.H.K. Dental plaque microcosm biofilm behavior on calcium phosphate nanocomposite with quaternary ammonium. Dent. Mater. 2012, 28, 853–862. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Zhang, K.; Xu, N.; Xu, H.H.K.; Weir, M.D.; Ge, Y.; Wang, S.; Li, M.; Li, Y. Antibacterial effect of dental adhesive containing dimethylaminododecyl methacrylate on the development of streptococcus mutans biofilm. Int. J. Mol. Sci. 2014, 15, 12791–12806. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Wang, S.; Zhou, X.; Xu, H.H.K.; Weir, M.D.; Ge, Y.; Li, M.; Wang, S.; Li, Y.; Xu, X. Effect of antibacterial dental adhesive on multispecies biofilms formation. J. Dent. Res. 2015, 94, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.; Yuan, G.; Li, J.; Ying, L.; Xiao, S.; Zhou, X.; Li, J. Biomimetic mineralization of collagen fibrils induced by amine-terminated pamam dendrimers—pamam dendrimers for remineralization. J. Biomater. Sci. Polym. Ed. 2015, 26, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Wang, P.; Weir, M.D.; Fouad, A.F.; Xu, H.H.K. Evaluation of antibacterial and remineralizing nanocomposite and adhesive in rat tooth cavity model. Acta Biomater. 2014, 10, 2804–2813. [Google Scholar] [CrossRef] [PubMed]
- Svenson, S.; Tomalia, D.A. Dendrimers in biomedical applications—Reflections on the field. Adv. Drug Deliv. Rev. 2005, 57, 2106–2129. [Google Scholar] [CrossRef] [PubMed]
- Monica, P.; William, T.B.; Chunlin, Q. Dentin sialophosphoprotein in biomineralization. Connect. Tissue Res. 2010, 51, 404–417. [Google Scholar]
- Liang, K.; Yuan, H.; Li, J.; Yang, J.; Zhou, X.; He, L.; Cheng, L.; Gao, Y.; Xu, X.; Zhou, X. Remineralization of demineralized dentin induced by amine-terminated pamam dendrimer. Macromol. Mater. Eng. 2015, 300, 107–117. [Google Scholar] [CrossRef]
- Sear, R.P. The non-classical nucleation of crystals: Microscopic mechanisms and applications to molecular crystals, ice and calcium carbonate. Int. Mater. Rev. 2013, 57, 328–356. [Google Scholar] [CrossRef]
- Reinke, S.M.G.; Divardin, S.; Raggio, D.; Reis, A.; Loguercio, A.D. Degradation of the resin-dentin bonds after simulated and inhibited cariogenic challenge in an in situ model. J. Biomed. Mater. Res. B Appl. Biomater. 2012, 100, 1466–1471. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imazato, S.; Ma, S.; Chen, J.H.; Xu, H.H.K. Therapeutic polymers for dental adhesives: Loading resins with bio-active components. Dent. Mater. 2014, 30, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Ge, Y.; Zhou, X.; Xu, H.H.K.; Weir, M.D.; Zhang, K.; Wang, H.; Matthias, H.; Stefan, R.; Li, Q.; et al. Effect of dimethylaminododecyl methacrylate containing glass-ionomer cement on the S. Mutans biofilms. Int. J. Oral Sci. 2016, 8, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Weir, M.D.; Zhang, K.; Arola, D.D.; Zhou, X.; Xu, H.H.K. Dental primer and adhesive containing a new antibacterial quaternary ammonium monomer dimethylaminododecyl methacrylate. J. Dent. 2013, 41, 345–355. [Google Scholar] [CrossRef] [PubMed]
- Liang, K.; Gao, Y.; Li, J.; Liao, Y.; Xiao, S.; Lv, H.; He, L.; Cheng, L.; Zhou, X.; Li, J. Effective dentinal tubule occlusion induced by polyhydroxy-terminated pamam dendrimer in vitro. Rsc Adv. 2014, 4, 43496–43503. [Google Scholar] [CrossRef]
- Namba, N.; Yoshida, Y.; Nagaoka, N. Antibacterial effect of bactericide immobilized in resin matrix. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2009, 25, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Beyth, N.; Yudovin-Farber, I.; Ran, B.; Domb, A.J.; Weiss, E.I. Antibacterial activity of dental composites containing quaternary ammonium polyethylenimine nanoparticles against streptococcus mutans. Biomaterials 2006, 27, 3995–4002. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Weir, M.D.; Antonucci, J.M.; Schumacher, G.E.; Zhou, X.D.; Xu, H.H. Evaluation of three-dimensional biofilms on antibacterial bonding agents containing novel quaternary ammonium methacrylates. Int. J. Oral Sci. 2014, 6, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Beyth, N.; Yudovin-Farber, I.; Perez-Davidi, M.; Domb, A.J.; Weiss, E.I. Polyethyleneimine nanoparticles incorporated into resin composite cause cell death and trigger biofilm stress in vivo. Proc. Natl. Acad. Sci. USA 2010, 107, 22038–22043. [Google Scholar] [CrossRef] [PubMed]
- Ge, Y.; Caufield, P.W.; Fisch, G.S.; Li, Y. Streptococcus mutans and streptococcus sanguinis colonization correlated with caries experience in children. Caries Res. 2008, 42, 444–448. [Google Scholar] [CrossRef] [PubMed]
- Gregson, K.S.; Han, S.; Gregory, R.L. The impact of three strains of oral bacteria on the surface and mechanical properties of a dental resin material. Clin. Oral Investig. 2012, 16, 1095–1103. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Cheng, L.; Wu, E.J.; Weir, M.D.; Bai, Y.; Xu, H.H.K. Effect of water-ageing on dentine bond strength and anti-biofilm activity of bonding agent containing new monomer dimethylaminododecyl methacrylate. J. Dent. 2013, 41, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Zhang, K.; Zhou, C.C.; Weir, M.D.; Zhou, X.D.; Xu, H.H.K. One-year water-ageing of calcium phosphate composite containing nano-silver and quaternary ammonium to inhibit biofilms. Int. J. Oral Sci. 2016, 8, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Chen, J.; Chai, Z.G.; Zhang, L.; Xiao, Y.; Fang, M.; Ma, S. Effects of a dental adhesive incorporating antibacterial monomer on the growth, adherence and membrane integrity of streptococcus mutans. J. Dent. 2009, 37, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Tiller, J.C.; Liao, C.J.; Lewis, K.; Klibanov, A.M. Designing surfaces that kill bacteria on contact. Proc. Natl. Acad. Sci. USA 2001, 98, 5981–5985. [Google Scholar] [CrossRef] [PubMed]

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ge, Y.; Ren, B.; Zhou, X.; Xu, H.H.K.; Wang, S.; Li, M.; Weir, M.D.; Feng, M.; Cheng, L. Novel Dental Adhesive with Biofilm-Regulating and Remineralization Capabilities. Materials 2017, 10, 26. https://doi.org/10.3390/ma10010026
Ge Y, Ren B, Zhou X, Xu HHK, Wang S, Li M, Weir MD, Feng M, Cheng L. Novel Dental Adhesive with Biofilm-Regulating and Remineralization Capabilities. Materials. 2017; 10(1):26. https://doi.org/10.3390/ma10010026
Chicago/Turabian StyleGe, Yang, Biao Ren, Xuedong Zhou, Hockin H. K. Xu, Suping Wang, Mingyun Li, Michael D. Weir, Mingye Feng, and Lei Cheng. 2017. "Novel Dental Adhesive with Biofilm-Regulating and Remineralization Capabilities" Materials 10, no. 1: 26. https://doi.org/10.3390/ma10010026




