Carbonate Apatite Containing Statin Enhances Bone Formation in Healing Incisal Extraction Sockets in Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of Specimens
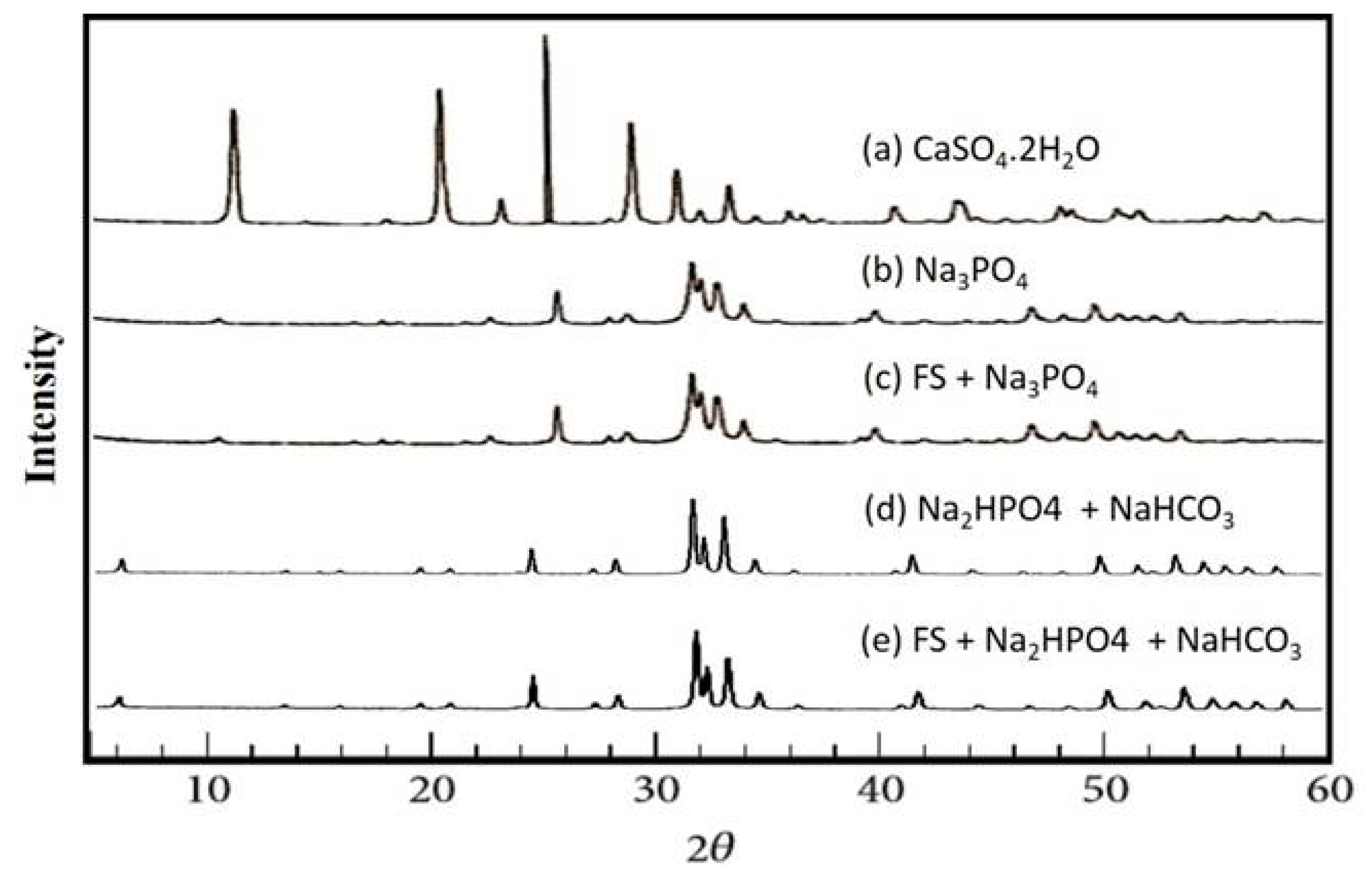
2.2. X-Ray Diffraction Analysis
2.3. Scanning Electron Microscope Analysis
2.4. Animals
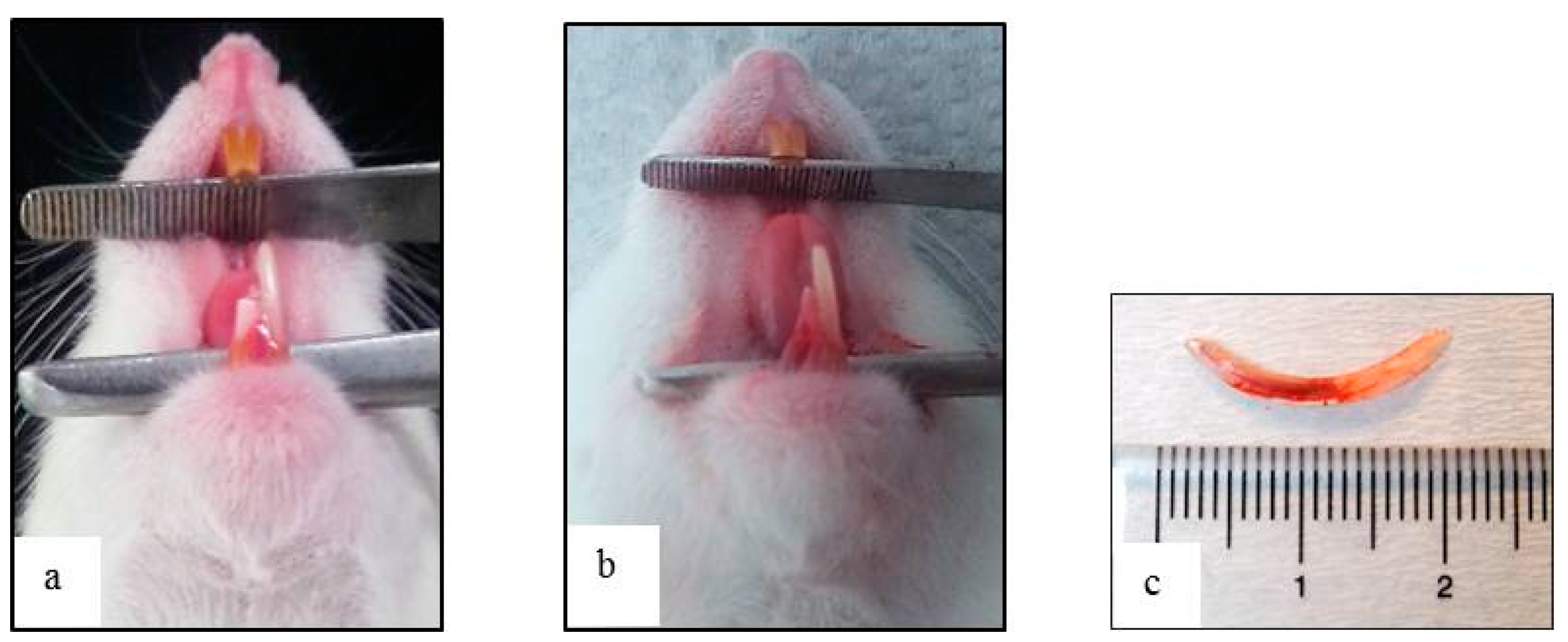
2.5. Anesthesia and Surgical Procedures
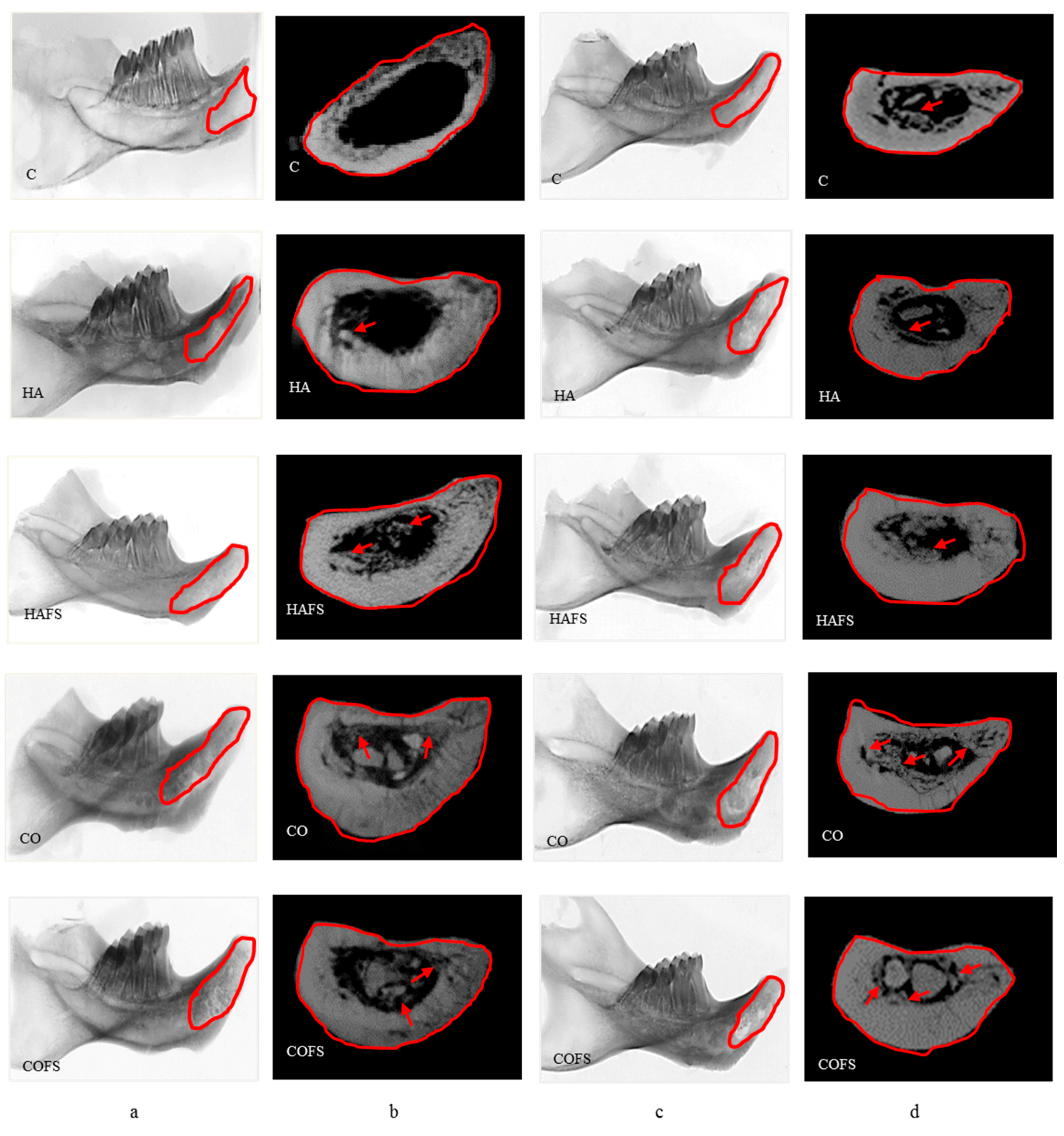
2.6. Micro-Computed Tomography Analysis
2.7. Histological Evaluation
2.8. Statistical Analysis
3. Results
3.1. X-Ray Diffraction Analysis
3.2. Scanning Electron Microscope Analysis
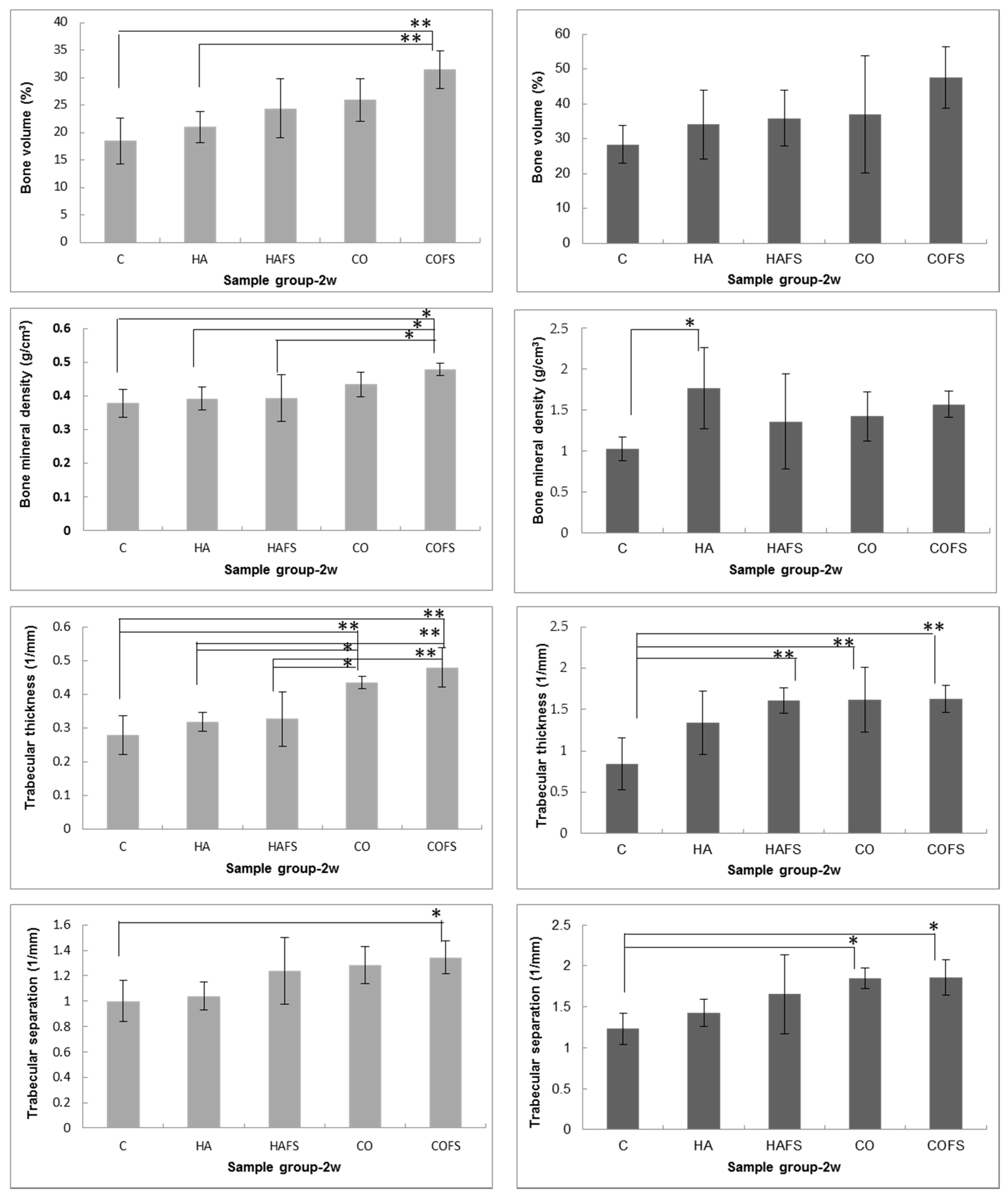
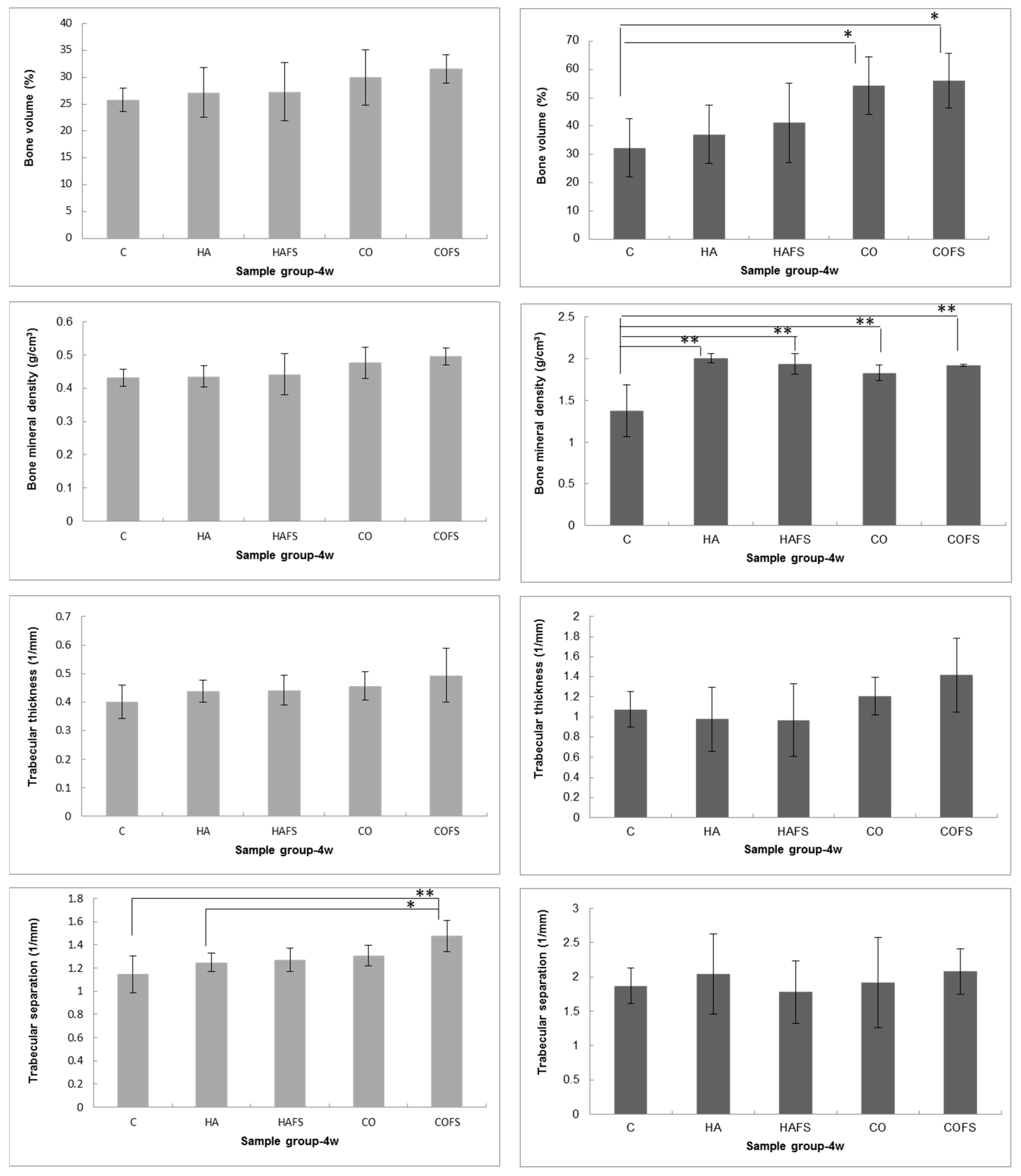
3.3. Micro-Computed Tomography Analysis
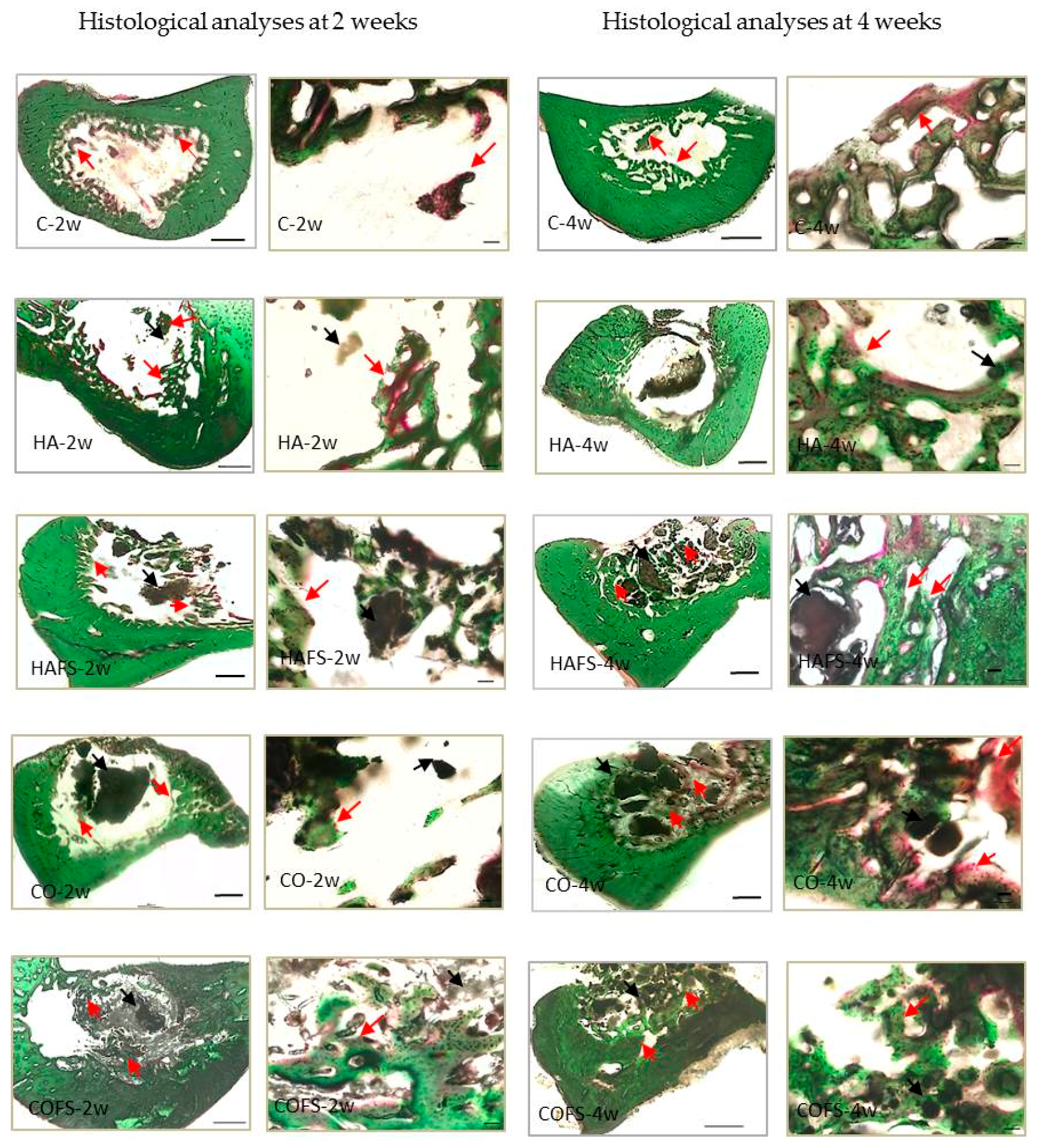
3.4. Histological Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rakhmatia, Y.D.; Ayukawa, Y.; Furuhashi, A.; Koyano, K. Current barrier membranes: Titanium mesh and other membranes for guided bone regeneration in dental applications. J. Prosthodont. Res. 2013, 57, 3–14. [Google Scholar] [CrossRef] [PubMed]
- Shetty, V.; Han, T.J. Alloplastic materials in reconstructive periodontal surgery. Dent. Clin. N. Am. 1991, 35, 521–530. [Google Scholar] [PubMed]
- Burg, K.J.L.; Porter, S.; Kellam, J.F. Biomaterial developments for bone tissue engineering. Biomaterials 2000, 21, 2347–2359. [Google Scholar] [CrossRef]
- Favvas, E.P.; Stefanopoulos, K.L.; Vordos, N.C.; Drosos, G.I.; Mitropoulos, A.C. Structural characterization of calcium sulfate bone graft substitute cements. Mater. Res. 2016, 19, 1108–1113. [Google Scholar] [CrossRef]
- Suzuki, Y.; Matsuya, S.; Udoh, K.; Nakagawa, M.; Tsukiyama, Y.; Koyano, K.; Ishikawa, K. Fabrication of hydroxyapatite block from gypsum block based on (NH4)2HPO4 treatment. Dent. Mater. J. 2005, 24, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Chang, B.S.; Lee, C.K.; Hong, K.S. Osteoconduction at porous hydroxyapatite with various pore configurations. Biomaterials 2000, 21, 1291–1298. [Google Scholar] [CrossRef]
- Moore, W.R.; Graves, S.E.; Bain, G.I. Synthetic bone graft substitutes. ANZ J. Surg. 2003, 71, 354–361. [Google Scholar] [CrossRef]
- Maruta, M.; Matsuya, S.; Nakamura, S.; Ishikawa, K. Fabrication of low-crystalline carbonate apatite foam bone replacement based on phase transformation of calcite foam. Dent. Mater. J. 2011, 30, 14–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morgan, E.F.; Barnes, G.L.; Einhorn, T.A. The bone organ system: Form and function. In Osteoporosis, 3rd ed.; Marcus, R., Feldman, D., Nelson, D.A., Rosen, C.J., Eds.; Academic Press: San Diego, CA, USA, 2007; pp. 3–26. ISBN 978-0-12-370544-0. [Google Scholar]
- Doi, Y.; Aoba, T.; Okazaki, M.; Takahashi, J.; Moriwaki, Y. Analysis of paramagnetic centers in X-ray irradiated enamel, bone, and carbonate-containing hydroxyapatite by electron spin resonance spectroscopy. Calcif. Tissue Int. 1979, 28, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Feng, X. Chemical and biochemical basis of cell-bone matrix interaction in health and disease. Curr. Chem. Biol. 2009, 3, 189–196. [Google Scholar] [CrossRef] [PubMed]
- LeGeros, R.Z. Calcium phosphates in oral biology and medicine. In Monographs in Oral Science; Myers, H.M., Ed.; Karger: Basel, Switzerland, 1991; pp. 110–111, ISBN-13: 978-3805552363. [Google Scholar]
- Tônsuaadu, K.; Peld, M.; Leskelä, T.; Mannonen, R.; Niinistö, L.; Veiderma, M. A thermoanalytical study of synthetic carbonate containing apatites. Themochim. Acta 1995, 256, 55–65. [Google Scholar] [CrossRef]
- Nomura, S.; Tsuru, K.; Maruta, M.; Matsuya, S.; Takahashi, I.; Ishikawa, K. Fabrication of carbonate apatite blocks from set gypsum based on dissolution-precipitation reaction in phosphate-carbonate mixed solution. Dent. Mater. J. 2014, 33, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Landi, E.; Tampieri, A.; Celotti, G.; Vichi, L.; Sandri, M. Influence of synthesis and sintering parameters on the characteristics of carbonate apatite. Biomaterials 2004, 25, 1763–1770. [Google Scholar] [CrossRef] [PubMed]
- Ayukawa, Y.; Suzuki, Y.; Tsuru, K.; Koyano, K.; Ishikawa, K. Histological comparison in rats between carbonate apatite fabricated from gypsum and sintered hydroxyapatite on bone remodeling. Biomed. Res. Int. 2015, 2015, 579541. [Google Scholar] [CrossRef] [PubMed]
- Montagnani, A.; Gonnelli, S.; Cepollaro, C.; Pacini, S.; Campagna, M.S.; Franci, M.B.; Lucani, B.; Gennari, C. Effect of simvastatin treatment on bone mineral density and bone turnover in hypercholesterolemic postmenopausal women: A 1-year longitudinal study. Bone 2003, 32, 427–433. [Google Scholar] [CrossRef]
- Sonobe, M.; Hattori, K.; Tomita, N.; Yoshikawa, T.; Aoki, H.; Takakura, Y.; Suguro, T. Stimulatory effects of statins on bone marrow-derived mesenchymal stem cells: Study of a new therapeutic agent for fracture. Bio-Med Mater. Eng. 2005, 15, 261–267. [Google Scholar]
- Wong, R.W.K.; Rabie, A.B.M. Early healing pattern of statin induced osteogenesis. Br. J. Oral Maxillofac. Surg. 2005, 43, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.W.K.; Rabie, A.B.M. Histologic and ultrastructural study on statin graft in rabbit skulls. J. Oral Maxillofac. Surg. 2005, 63, 1515–1521. [Google Scholar] [CrossRef] [PubMed]
- Ayukawa, Y.; Okamura, A.; Koyano, K. Simvastatin promotes osteogenesis around titanium implants. A histological and histometrical study in rats. Clin. Oral Implant. Res. 2004, 15, 346–350. [Google Scholar] [CrossRef] [PubMed]
- Moriyama, Y.; Ayukawa, Y.; Ogino, Y.; Atsuta, I.; Todo, M.; Takao, Y.; Koyano, K. Local application of fluvastatin improves peri-implant bone quantity and mechanical properities: A rodent study. Acta Biomater. 2010, 6, 1610–1618. [Google Scholar] [CrossRef] [PubMed]
- Masuzaki, T.; Ayukawa, Y.; Moriyama, Y.; Jinno, Y.; Atsuta, I.; Ogino, Y.; Koyano, K. The effect of a single remote injection of statin-impregnated poly(lactic-co-glycolic acid) microspheres on osteogenesis around titanium implants in rat tibia. Biomaterials 2010, 31, 3327–3334. [Google Scholar] [CrossRef] [PubMed]
- Yasunami, N.; Ayukawa, Y.; Furuhashi, A.; Atsuta, I.; Rakhmatia, Y.D.; Moriyama, Y.; Masuzaki, T.; Koyano, K. Acceleration of hard and soft tissue healing in the oral cavity by a single transmucosal injection of fluvastatin-impregnated poly(lactic-co-glycolic acid) microspheres. An in vitro and rodent in vivo study. Biomed. Mater. 2015, 11, 015001. [Google Scholar] [CrossRef] [PubMed]
- Jinno, Y.; Ayukawa, Y.; Ogino, Y.; Atsuta, I.; Tsukiyama, Y.; Koyano, K. Vertical bone augmentation with fluvastatin in an injectable delivery system: A rat study. Clin. Oral Implant. Res. 2009, 20, 756–760. [Google Scholar] [CrossRef] [PubMed]
- Yazawa, H.; Zimmermann, B.; Asami, Y.; Bernimoulin, J.P. Simvastatin promotes cell metabolism, proliferation, and osteoblastic differentiation in human periodontal ligament cells. J. Periodontol. 2005, 76, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Nyan, M.; Sato, D.; Oda, M.; Machida, T.; Kobayashi, H.; Nakamura, T.; Kasugai, S. Bone formation with the combination of simvastatin and calcium sulfate in critical-sized rat calvarial defect. J. Pharmacol. Sci. 2007, 104, 384–386. [Google Scholar] [CrossRef] [PubMed]
- Ting, M.; Whitaker, E.J.; Albandar, J.M. Systematic review of the in vitro effects of statins on oral and perioral microorganisms. Eur. J. Oral Sci. 2016, 124, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Machida, T.; Nyan, M.; Kon, K.; Maruo, K.; Sato, H.; Kasugai, S. Effect of hydroxyapatite fiber material on rat incisor socket healing. J. Oral Tissue Eng. 2009, 7, 153–162. [Google Scholar] [CrossRef]
- Cohen, N.; Cohen-Lévy, J. Healing process following tooth extraction in orthodontic case. J. Dentofac. Anom. Orthod. 2014, 17, 304. [Google Scholar] [CrossRef]
- Kono, T.; Ayukawa, Y.; Moriyama, Y.; Kurata, K.; Takamatsu, H.; Koyano, K. The effect of low-magnitude, high-frequency vibration stimuli on the bone healing of rat incisor extraction socket. J. Biomech. Eng. 2012, 134, 091001. [Google Scholar] [CrossRef] [PubMed]
- Araujo, M.G.; Liljenberg, B.; Lindhe, J. Dynamics of bio-oss collagen incorporation in fresh extraction wounds: An experimental study in the dog. Clin. Oral Implant. Res. 2010, 21, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Araujo, M.G.; Liljenberg, B.; Lindhe, J. Beta-tricalcium phosphate in the early phase of socket healing: An experimental study in the dog. Clin. Oral Implant. Res. 2010, 21, 445–454. [Google Scholar] [CrossRef] [PubMed]
- Fei, W.; Zuo, L.; Hu, J.; Yin, M.; Shen, Z. Basic fibroblast growth factor accelerates wound healing of tooth extraction. Chin. J. Oral Implantol. 2001, 4, 154–156. [Google Scholar]
- Wu, Z.; Liu, C.; Zang, G.; Sun, H. The effect of simvastatin on remodelling of the alveolar bone following tooth extraction. Int. J. Oral Maxillofac. Surg. 2008, 37, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, T.; Onofre Da Silva, A. Histological study on the healing of rat dental sockets after partial removal of the buccal bony plate. J. Nihon Univ. Sch. Dent. 1983, 25, 202–213. [Google Scholar] [CrossRef] [PubMed]
- Vieira, A.E.; Repeke, C.E.; Ferreira Junior Sde, B.; Colavite, P.M.; Biguetti, C.C.; Oliveira, R.C.; Assis, G.F.; Taga, R.; Trombone, A.P.; Garlet, G. Intramembranous bone healing process subsequent to tooth extraction in mice: Micro-computed tomography, histomorphometric and molecular characterization. PLoS ONE 2015, 10, e0128021. [Google Scholar] [CrossRef] [PubMed]
- Lamano Carvalho, T.L.; Bombonato, K.F.; Brentegani, L.G. Histometric analysis of rat alveolar wound healing. Braz. Dent. J. 1997, 8, 9–12. [Google Scholar]
- Elsubeihi, E.S.; Heersche, J.N. Quantitative assessment of post-extraction healing and alveolar ridge remodeling of the mandible in female rats. Arch. Oral Biol. 2004, 49, 401–412. [Google Scholar] [CrossRef] [PubMed]
- Yugoshi, L.I.; Sala, M.A.; Brentegani, L.G.; Lamano Carvalho, T.L. Histometric study of socket healing after tooth extraction in rats treated with diclofenac. Braz. Dent. J. 2002, 13, 92–96. [Google Scholar] [CrossRef] [PubMed]
- Calixto, R.F.; Teófilo, J.M.; Brentegani, L.G.; Lamano, T. Comparison of rat bone healing following intra-alveolar grafting with organic or inorganic bovine bone particles. Braz. J. Oral Sci. 2008, 7, 1512–1519. [Google Scholar]
- Mundy, G.; Garrett, R.; Harris, S.; Chan, J.; Chen, D.; Rossini, G.; Boyce, B.; Zhao, M.; Gutierrez, G. Stimulation of bone formation in vitro and rodents by statins. Science 1999, 286, 1946–1949. [Google Scholar] [CrossRef] [PubMed]
- De Bruijn, J.D.; Bovell, Y.P.; van Blitterswijk, C.A. Structural arrangements at the interface between plasma sprayed calcium phosphates and bone. Biomaterials 1994, 15, 543–550. [Google Scholar] [CrossRef]
- Dhert, W.J.; Thomsen, P.; Blomgren, A.K.; Esposito, M.; Ericson, L.E.; Verbout, A.J. Integration of press-fit implants in cortical bone: A study on interface kinetics. J. Biomed. Mater. Res. 1998, 41, 574–583. [Google Scholar] [CrossRef]
- Wagner, J.R. Clinical and histological case study using resorbable hydroxylapatite for the repair of osseous defects prior to endosseous implant surgery. J. Oral Implantol. 1989, 15, 186–192. [Google Scholar] [PubMed]
- Rakhmatia, Y.D.; Ayukawa, Y.; Jinno, Y.; Furuhashi, A.; Koyano, K. Micro-computed tomography analysis of early stage bone healing using micro-porous titanium mesh for guided bone regeneration: Preliminary experiment in a canine model. Odontology 2017, 105, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, H.; Shi, J.; Wang, Y.; Lai, K.; Yang, X.; Chen, X.; Yang, G. Combination of simvastatin, calcium silicate/gypsum, and gelatin and bone regeneration in rabbit calvarial defects. Sci. Rep. 2016, 6, 23422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bitto, A.; Minutoli, L.; Altavilla, D.; Polito, F.; Fiumara, T.; Marini, H.; Galeano, M.; Calò, M.; Lo Cascio, P.; Bonaiuto, M.; et al. Simvastatin enhances VEGF production and ameliorates impaired wound healing in experimental diabetes. Pharmacol. Res. 2008, 57, 159–169. [Google Scholar] [CrossRef] [PubMed]
- Jerwood, S.; Cohen, J. Unexpected antimicrobial effect of statins. J. Antimicrob. Chemother. 2008, 61, 362–364. [Google Scholar] [CrossRef] [PubMed]
- LeGeros, R.Z.; Ming, S. Chemical stability of carbonate- and fluoride-containing apatites. Caries Res. 1983, 17, 419–429. [Google Scholar] [CrossRef] [PubMed]


| Sample Groups | CaSO4·2H2O (Gypsum) | Statin | Immersion Solution | Hydrothermal Treatment |
|---|---|---|---|---|
| C | X | X | X | X |
| HA | O | X | Na3PO4 | 100 °C for 24 h |
| HAFS | O | O | Na3PO4 | 100 °C for 24 h |
| CO | O | X | Na2HPO4 and NaHCO3 | 200 °C for 24 h |
| COFS | O | O | Na2HPO4 and NaHCO3 | 200 °C for 24 h |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rakhmatia, Y.D.; Ayukawa, Y.; Furuhashi, A.; Koyano, K. Carbonate Apatite Containing Statin Enhances Bone Formation in Healing Incisal Extraction Sockets in Rats. Materials 2018, 11, 1201. https://doi.org/10.3390/ma11071201
Rakhmatia YD, Ayukawa Y, Furuhashi A, Koyano K. Carbonate Apatite Containing Statin Enhances Bone Formation in Healing Incisal Extraction Sockets in Rats. Materials. 2018; 11(7):1201. https://doi.org/10.3390/ma11071201
Chicago/Turabian StyleRakhmatia, Yunia Dwi, Yasunori Ayukawa, Akihiro Furuhashi, and Kiyoshi Koyano. 2018. "Carbonate Apatite Containing Statin Enhances Bone Formation in Healing Incisal Extraction Sockets in Rats" Materials 11, no. 7: 1201. https://doi.org/10.3390/ma11071201





