Current Strategies in Cardiovascular Biomaterial Functionalization
Abstract
:1. Introduction
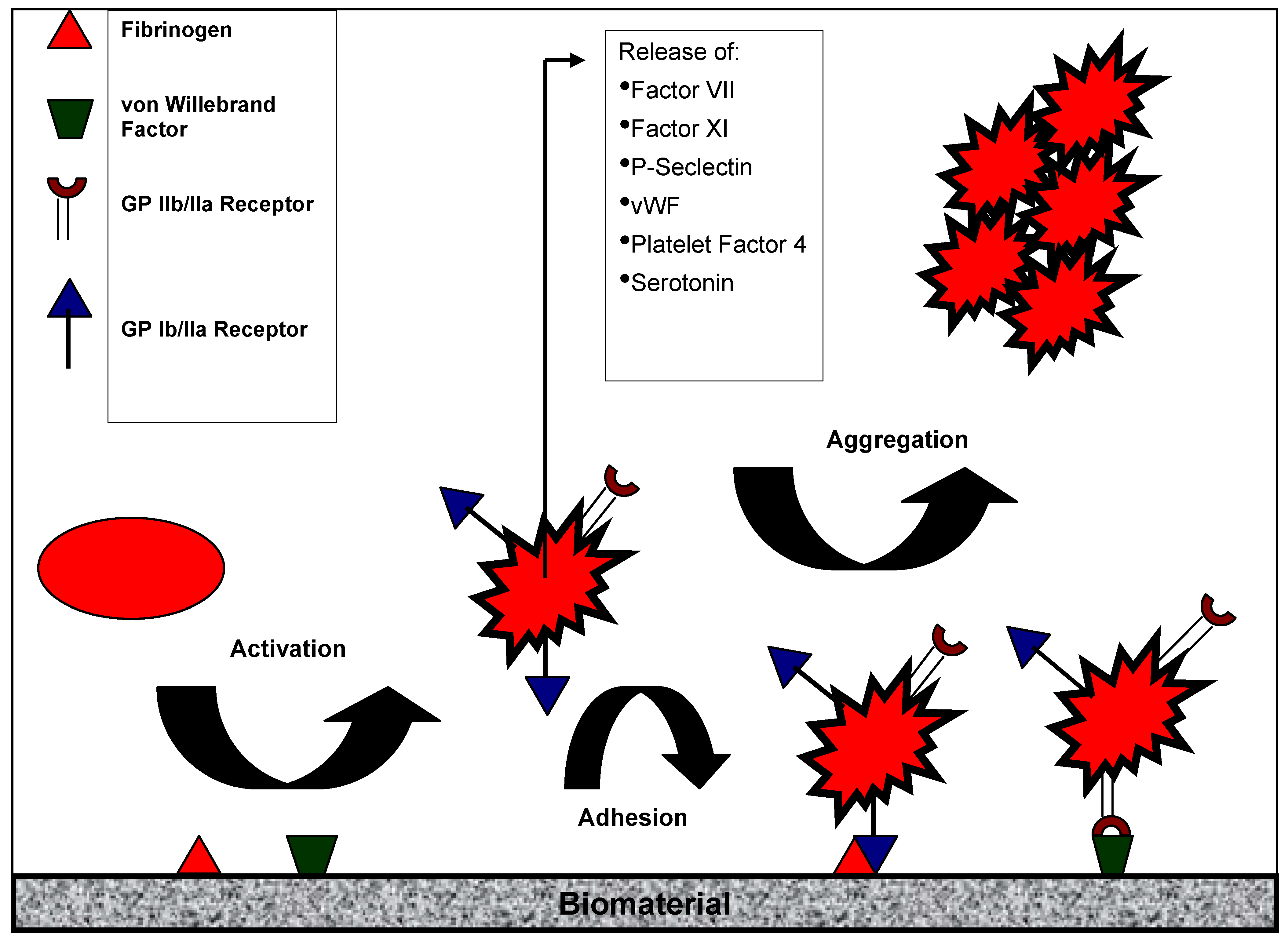
2. Blood Contact Activation

3. Platelet Activation
4. Strategies to Prevent Protein and Platelet Adhesion
| Strategy | Material | Laboratory success | Clinical success | References |
|---|---|---|---|---|
| Inhibition of protein and cell adsorbtion |
| + + + + | - - - - | [26,27] [28,29,30,31,32,33,34,35] [36,37,38,39,40] [41,42] |
| Inhibition of thrombin and fibrin formation |
| + + | + - | [2,3,44,45,46,47,48,49,50] [51,52,53] |
| Inhibition of platelet activation |
| + | + | [54] |
5. Endothelialization
5.1. In Vitro Endothelialization
5.2. In Situ Endothelialization
6. Conclusions
References
- Vogler, E.A.; Siedllecki, C.A. Contact activation of blood plasma coagulation. Biomaterials 2009, 30, 1857–1869. [Google Scholar] [CrossRef] [PubMed]
- Von Segesser, L.K. Heparin-bonded surfaces in extracorporeal membrane oxygenation for cardiac support. Ann. Thorac. Surg. 1996, 61, 330–335. [Google Scholar]
- Hsu, L.C. Heparin-coated cardiopulmonary bypass circuits: Current status. Perfusion 2001, 16, 417–428. [Google Scholar] [CrossRef] [PubMed]
- Bordenave, L.; Fernandez, P.; Remy-Zolghadri, M.; Villars, S.; Daculsi, R.; Midy, D. In vitro endothelialized ePTFE prostheses: Clinical update 20 years after the first realization. Clin. Hemorheol. Microcirc. 2005, 33, 227–234. [Google Scholar] [PubMed]
- Schmaier, A.H. The elusive physiologic role of factor XII. J. Clin. Invest. 2008, 118, 3006–3009. [Google Scholar] [PubMed]
- Colman, R.W.; Schmaier, A.H. Contact system: A vascular biology modulator with anticoagulant, profibrinolytic, antiadhesive, and proinflammatory attributes. Blood 1997, 90, 3819–3843. [Google Scholar] [PubMed]
- Colman, R.W. Contact activation pathway: Inflammatory fibrinolytic, anticoagulant, antiadhesive, and antiangiogenic activities. In Hemostasis and Thrombosis: Basic Principles and Clinical Practice, 4th ed; Colman, R.W., Marder, V.J., Hirsh, J., Clowes, A.W., Eds.; J.B. Lippincott Company: Philadelphia, PA, USA, 2000; pp. 103–121. [Google Scholar]
- Samuel, M.; Pixley, R.A.; Villanueva, M.A.; Colman, R.W.; Villanueva, G.B. Human factor XII (Hageman factor) autoactivation by dextran sulfate. Circular dichroism, fluorescence, and ultraviolet difference spectroscopic studies. J. Biol. Chem. 1992, 267, 19691–19697. [Google Scholar] [PubMed]
- Hanson, S.R. Device thrombosis and thromboembolism. Cardiovasc. Pathol. 1993, 2, 157S–165S. [Google Scholar] [CrossRef]
- Ratner, B.D. The blood compatibility catastrophe. J. Biomed. Mater. Res. 1993, 27, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Gorbet, M.B.; Sefton, M.V. Biomaterial-associated thrombosis: roles of coagulation factors, complement, platelets and leukocytes. Biomaterials 2004, 25, 5681–5703. [Google Scholar] [CrossRef] [PubMed]
- Furie, B.; Furie, B.C. Mechanism of thrombus formation. N. Eng. J. Med. 2008, 359, 938–949. [Google Scholar] [CrossRef]
- Godo, M.N.; Sefton, M.V. Characterization of transient platelet contacts on a polyvinyl alcohol hydrogel by video microscopy. Biomaterials 1999, 20, 1117–1126. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, J.I.; McClung, W.G.; Feuerstein, I.A. Adherent platelet morphology on adsorbed fibrinogen: Effects of protein incubation time and albumin addition. J. Biomed. Mater. Res. 1994, 28, 1175–1186. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Bae, Y.H. Hydrogels based on poly(ethylene oxide) and poly(tetramethylene oxide) or poly(dimethyl siloxane): Synthesis, characterization, in vitro protein adsorption and platelet adhesion. Biomaterials 2002, 23, 1797–1808. [Google Scholar] [CrossRef] [PubMed]
- Gemmell, C.H.; Ramirez, S.M.; Yeo, E.L.; Sefton, M.V. Platelet activation in whole blood by artificial surfaces: Identification of platelet-derived microparticles and activated platelet binding to leukocytes as material-induced activation events. J. Lab. Clin. Med. 1995, 125, 276–287. [Google Scholar] [PubMed]
- Cholakis, C.H.; Zingg, W.; Sefton, M.V. Effect of heparin-PVA hydrogel on platelets in a chronic canine AV shunt. J. Biomed. Mater. Res. 1989, 23, 417–441. [Google Scholar] [CrossRef] [PubMed]
- Hanson, S.R.; Harker, L.A.; Ratner, B.D.; Hoffman, A.S. In vivo evaluation of artificial surfaces with a nonhuman primate model of arterial thrombosis. J. Lab. Clin. Med. 1980, 95, 289–304. [Google Scholar] [PubMed]
- Ip, W.F.; Sefton, M.V. Platelet consumption by NHLBI reference materials and silastic. J. Biomed. Mater. Res. 1991, 25, 1321–1324. [Google Scholar] [CrossRef] [PubMed]
- Grunkemeier, J.M.; Tsai, W.B.; McFarland, C.D.; Horbett, T.A. The effect of adsorbed fibrinogen, fibronectin, von Willebrand factor and vitronectin on the procoagulant state of adherent platelets. Biomaterials 2000, 21, 2243–2252. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Simonovsky, F.I.; Ratner, B.D.; Horbett, T.A. The role of adsorbed fibrinogen in platelet adhesion to polyurethane surfaces: a comparison of surface hydrophobicity, protein adsorption, monoclonal antibody binding, and platelet adhesion. J. Biomed. Mater. Res. A 2005, 74, 722–738. [Google Scholar] [CrossRef] [PubMed]
- Wachtfogel, Y.T.; Hack, C.E.; Nuijens, J.H.; Kettner, C.; Reilly, T.M.; Knabb, R.M.; Bischoff, R.; Tschesche, H.; Wenzel, H.; Kucich, U.; Edmonds, L.H., Jr.; Colman, R.W. Selective kallikrein inhibitors alter human neutrophil elastase release during extracorporeal circulation. Am. J. Physiol. Heart Circ. Physiol. 1995, 26, H1352–H1357. [Google Scholar]
- Simon, P.; Ang, K.S.; Cam, G. Enhanced platelet aggregation and membrane biocompatibility: Possible influence on thrombosis and embolism in haemodialysis patients. Nephron 1987, 45, 172–173. [Google Scholar] [CrossRef] [PubMed]
- Hakim, R.M.; Schafer, A. Hemodialysis-associated platelet activation and thrombocytopenia. Am. J. Med. 1985, 78, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.W.; Chaikof, E.L. Novel thromboresistant materials. J. Vasc. Surg. 2007, 45, A104–A115. [Google Scholar] [CrossRef] [PubMed]
- Merrill, E.W.; Salzman, E.W. Polyethylene oxide as a biomaterial. ASAIO J. 1983, 6, 1. [Google Scholar]
- George, P.A.; Donose, B.C.; Cooper-White, J.J. Self-assembling polystyrene-block-poly(ethylene oxide) copolymer surface coatings: resistance to protein and cell adhesion. Biomaterials 2009, 30, 2449–2456. [Google Scholar] [CrossRef] [PubMed]
- Debski, R.; Borovetz, H.; Haubold, A.; Hardesty, R. Polytetrafluoroethylene grafts coated with Ulti carbon. Trans. Am. Soc. Artif. Intern. Organs 1982, 28, 456–458. [Google Scholar] [PubMed]
- Prunotto, M.; Isaia, C.; Gatti, M.A.; Monari, E.; Pasquino, E.; Galloni, M. Nitinol Carbofilm coated stents for peripheral applications: study in the porcine model. J. Mater. Sci. Mater. Med. 2005, 16, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Sick, P.B.; Gelbrich, G.; Kalnins, U.; Erglis, A.; Bonan, R.; Aengevaeren, W.; Elsner, D.; Lauer, B.; Woinke, M.; Brosteanu, O.; Schuler, G. Comparison of early and late results of a carbofilm-coated stent versus a pure high-grade stainless steel stent (the carbostent-trial). Am. J. Cardiol. 2004, 93, 1351–1356. [Google Scholar] [CrossRef] [PubMed]
- Bartorelli, A.L.; Trabattoni, D.; Montorsi, P.; Fabbiocchi, F.; Galli, S.; Ravagnani, P.; Grancini, L.; Cozzi, S.; Loaldi, A. Aspirin alone antiplatelet regimen after intracoronary placement of the Carbostent (TM): The ANTARES study. Catheter. Cardiovasc. Interv. 2002, 55, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Sick, P.B.; Brosteanu, O.; Ulrich, M.; Thiele, H.; Niebauer, J.; Busch, I.; Schuler, G. Prospective randomized comparison of early and late results of a carbonized stent versus a high-grade stainless steel stent of identical design: The Prevention of Recurrent Venous Thromboembolism (PREVENT) trial. Am. Heart J. 2005, 149, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Lee, C.W.; Hong, M.K.; Park, S.W.; Tahk, S.J.; Yang, J.Y.; Saito, S.; Santoso, T.; Quan, L.; Ge, J.; Weissman, N.J.; Lansky, A.J.; Mintz, G.S.; Park, S.J. Randomized comparison of carbon ion-implanted stent versus bare metal stent in coronary artery disease: The Asian Pacific Multicenter Arthos Stent Study (PASS) trial. Am. Heart J. 2005, 149, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Kornowski, R. A critical appraisal of the Janus carbostent. Catheter Cardiovasc. Interv. 2009, 73, 249–250. [Google Scholar] [CrossRef] [PubMed]
- Arabi, H.; Mirzadeh, H.; Ahmadi, S.H.; Amanpour, S.; Rabbani, S.; Abdi, A. In vitro and in vivo hemocompatibility evaluation of graphite coated polyester vascular grafts. Int. J. Artif. Organs 2004, 27, 691–698. [Google Scholar] [PubMed]
- Tegoulia, V.A.; Rao, W.S.; Kalambur, A.T.; Rabolt, J.R.; Cooper, S.L. Surface properties, fibrinogen adsorption, and cellular interactions of a novel phosphorylcholine-containing self-assembled monolayer on gold. Langmuir 2001, 17, 4396–4404. [Google Scholar] [CrossRef]
- Lu, J.R.; Murphy, E.F.; Su, T.J.; Lewis, A.L.; Stratford, P.W.; Satija, S.K. Reduced protein adsorption on the surface of a chemically grafted phospholipid monolayer. Langmuir 2001, 17, 3382–3389. [Google Scholar] [CrossRef]
- Glasmastar, K.; Larsson, C.; Hook, F.; Kasemo, B. Protein adsorption on supported phospholipid bilayers. J. Colloid. Interface Sci. 2002, 246, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Andersson, A.S.; Glasmastar, K.; Sutherland, D.; Lidberg, U.; Kasemo, B. Cell adhesion on supported lipid bilayers. J. Biomed. Mater. Res. A 2003, 64A, 622–629. [Google Scholar] [CrossRef]
- Jordan, S.W.; Faucher, K.M.; Caves, J.M.; Apkarian, R.P.; Rele, S.S.; Sun, X.L.; Hanson, S.R.; Chaikof, E.L. Fabrication of a phospholipid membrane-mimetic film on the luminal surface of an ePTFE vascular graft. Biomaterials 2006, 27, 3473–3481. [Google Scholar] [CrossRef] [PubMed]
- Barnes, M.J.; Macintyre, D.E. Platelet-reactivity of isolated constituents of the blood-vessel wall. Haemostasis 1979, 8, 158–170. [Google Scholar] [PubMed]
- Jordan, S.W.; Haller, C.A.; Sallach, R.E.; Apkarian, R.P.; Hanson, S.R.; Chaikof, E.L. The effect of a recombinant elastin-mimetic coating of an ePTFE prosthesis on acute thrombogenicity in a baboon arteriovenous shunt. Biomaterials 2007, 28, 1191–1197. [Google Scholar] [CrossRef] [PubMed]
- Defife, K.M.; Hagen, K.M.; Clapper, D.L.; Anderson, J.M. Photochemically immobilized polymer coatings: Effects on protein adsorption, cell adhesion, and leukocyte activation. J. Biomater. Sci. Polym. Ed. 1999, 10, 1063–1074. [Google Scholar] [CrossRef] [PubMed]
- Sperling, C.; Schweiss, R.B.; Streller, U.; Werner, C. In vitro hemocompatibility of self-assembled monolayers displaying various functional groups. Biomaterials 2005, 26, 6547–6557. [Google Scholar] [CrossRef] [PubMed]
- Laredo, J.; Xue, L.; Husak, V.A.; Ellinger, J.; Greisler, H.P. Silyl-heparin adsorption improves the in vivo thromboresistance of carbon-coated polytetrafluoroethylene vascular grafts. Am. J. Surg. 2003, 186, 556–560. [Google Scholar] [CrossRef] [PubMed]
- Luong-Van, E.; Grondahl, L.; Chua, K.N.; Leong, K.W.; Nurcombe, V.; Cool, S.M. Controlled release of heparin from poly(epsilon-caprolactone) electrospun fibers. Biomaterials 2006, 27, 2042–2050. [Google Scholar] [CrossRef] [PubMed]
- Larm, O.; Larsson, R.; Olsson, P. A new non-thrombogenic surface prepared by selective covalent binding of heparin via a modified reducing terminal residue. Biomater. Med. Devices Artif. Organs 1983, 11, 161–173. [Google Scholar] [PubMed]
- Pasche, B.; Elgue, G.; Olsson, P.; Riesenfeld, J.; Rasmuson, A. Binding of antithrombin to immobilized heparin under varying flow conditions. Artif. Organs 1991, 15, 481–491. [Google Scholar] [PubMed]
- Elgue, G.; Blomback, M.; Olsson, P.; Riesenfeld, J. On the mechanism of coagulation inhibition on surfaces with end-point immobilized heparin. Thromb. Haemost. 1993, 70, 289–293. [Google Scholar] [PubMed]
- Edmunds, L.H.; Colman, R.W. Thrombin during cardiopulmonary bypass. Ann. Thorac. Surg. 2006, 82, 2315–2322. [Google Scholar] [CrossRef] [PubMed]
- Kishida, A.; Ueno, Y.; Maruyama, I.; Akashi, M. Immobilization of human thrombomodulin on biomaterials: Evaluation of the activity of immobilized human thrombomodulin. Biomaterials 1994, 15, 1170–1174. [Google Scholar] [CrossRef] [PubMed]
- Vasilets, V.N.; Hermel, G.; König, U.; Werner, C.; Müller, M.; Simon, F.; Grundke, K.; Ikada, Y.; Jacobasch, H.J. Microwave CO2 plasma-initiated vapour phase graft polymerization of acrylic acid onto polytetrafluoroethylene for immobilization of human thrombomodulin. Biomaterials 1997, 18, 1139–1145. [Google Scholar] [CrossRef] [PubMed]
- Yeh, H.Y.; Lin, J.C. Bioactivity and platelet adhesion study of a human thrombomodulin-immobilized nitinol surface. J. Biomater. Sci. Polym. Ed. 2009, 20, 807–819. [Google Scholar] [CrossRef] [PubMed]
- Kidane, A.G.; Salacinski, H.; Tiwari, A.; Bruckdorfer, K.R.; Seifalian, A.M. Anticoagulant and antiplatelet agents: their clinical and device application(s) together with usages to engineer surfaces. Biomacromolecules 2004, 5, 798–813. [Google Scholar] [CrossRef]
- De Mel, A.; Jell, G.; Stevens, M.M.; Seifalian, A.M. Biofunctionalization of biomaterials for accelerated in situ endothelialization: a review. Biomacromolecules 2008, 9, 2969–2679. [Google Scholar] [CrossRef] [PubMed]
- Knight, R.L.; Wilcox, H.E.; Korossis, S.A; Fisher, J.; Ingham, E. The use of acellular matrices for the tissue engineering of cardiac valves. Proc. Inst. Mech. Eng. H 2008, 222, 129–143. [Google Scholar] [CrossRef] [PubMed]
- Bunting, S.; Moncada, S.; Vane, J.R. Antithrombotic properties of vascular endothelium. Lancet 1977, 2, 1075–1076. [Google Scholar] [CrossRef] [PubMed]
- McGuigan, A.; Sefton, M. The influence of biomaterials on endothelial cell thrombogenicity. Biomaterials 2007, 28, 2547–2571. [Google Scholar] [CrossRef] [PubMed]
- Seifalian, A.M.; Tiwari, A.; Rashid, S.T.; Salacinski, H.; Hamilton, G. Impregnation of the the polymeric graft with adhesives molecules, typically oligopeptides or glycoprotein improves retention. Artif. Organs 2002, 26, 209–210. [Google Scholar] [CrossRef] [PubMed]
- Meinhart, J.G.; Deutsch, M.; Fischlein, T.; Howanietz, N.; Froschl, A.; Zilla, P. Clinical autologous in vitro endothelialization of 153 infrainguinal ePTFE grafts. Ann. Thorac. Surg. 2001, 71, S327–S331. [Google Scholar] [CrossRef] [PubMed]
- Thomas, A.C.; Campbell, G.R.; Campbell, J.H. Advances in vascular tissue engineering. Cardiovasc. Pathol. 2003, 12, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Thebaud, N.B.; Pierron, D.; Bareille, R.; Le Visage, C.; Letourneur, D.; Bordenave, L. Human endothelial progenitor cell attachment to polysaccharide-based hydrogels: a pre-requisite for vascular tissue engineering. J. Mater. Sci. Mater. Med. 2007, 18, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Alobaid, N.; Salacinski, H.J.; Sales, K.M.; Hamilton, G.; Seifalian, A.M. Single stage cell seeding of small diameter prosthetic cardiovascular grafts. Clin. Hemorheol. Microcirc. 2005, 33, 209–226. [Google Scholar] [PubMed]
- Wu, Y.F.; Zhang, J.; Gu, Y.Q.; Li, J.X.; Wang, L.C.; Wang, Z.G. Reendothelialization of tubular scaffolds by sedimentary and rotative forces: a first step toward tissue-engineered venous graft. Cardiovasc. Revasc. Med. 2008, 9, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Teebken, O.E.; Puschmann, C.; Breitenbach, I.; Rohde, B.; Burgwitz, K.; Haverich, A. Preclinical development of tissue-engineered vein valves and venous substitutes using re-endothelialised human vein matrix. Eur. J. Vasc. Endovasc. Surg. 2009, 37, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Perea, H.; Aigner, J.; Hopfner, U.; Wintermantel, E. Direct magnetic tubular cell seeding: a novel approach for vascular tissue engineering. Cells Tissues Organs 2006, 183, 156–165. [Google Scholar] [CrossRef] [PubMed]
- Gulbins, H.; Pritisinac, A.; Petzold, R.; Goldemund, A.; Doser, M.; Dauner, M.; Meiser, B.; Reichart, B.; Daebritz, S. A low-flow adaptation phase improves shear-stress resistance of artificially seeded endothelial cells. Thorac. Cardiovasc. Surg. 2005, 53, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Schopka, S.; Schmid, F.X.; Hirt, S.; Birnbaum, D.E.; Schmid, C.; Lehle, K. Recellularization of biological heart valves with human vascular cells: in vitro hemocompatibility assessment. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 88, 130–138. [Google Scholar] [CrossRef] [PubMed]
- Lehle, K.; Stock, M.; Schmid, T.; Schopka, S.; Straub, R.H.; Schmid, C. Cell-type specific evaluation of biocompatibility of commercially available polyurethanes. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 90, 312–318. [Google Scholar] [PubMed]
- Lehle, K.; Buttstaedt, J.; Birnbaum, D.E. Expression of adhesion molecules and cytokines in vitro by endothelial cells seeded on various polymer surfaces coated with titaniumcarboxonitride. J. Biomed. Mater. Res. A 2003, 65, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Lichtenberg, A.; Tudorache, I.; Cebotari, S.; Suprunov, M.; Tudorache, G.; Goerler, H.; Park, J.K.; Hilfiker-Kleiner, D.; Ringes-Lichtenberg, S.; Karck, M.; Brandes, G.; Hilfiker, A.; Haverich, A. Preclinical testing of tissue-engineered heart valves re-endothelialized under stimulated physiological conditions. Circulation 2006, 114, I559–I564. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.J.; Steen, J.; Jordan, J.E.; Kincaid, E.H.; Kon, N.D.; Atala, A.; Berry, J.; Yoo, J.J. Endothelialization of heart valve matrix using a computer.assisted pulsatile bioreactor. Tissue Eng. A 2009, 15, 807–814. [Google Scholar] [CrossRef]
- Herring, M.; Dilley, R.; Jersild, R.J.; Boxer, L.; Gardner, A.; Glover, J. Seeding arterial prostheses with vascular endothelium. The nature of lining. Ann. Surg. 1979, 190, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Graham, L.; Burkel, W.; Ford, J.; Vinter, D.; Kahn, R.; Stanley, J. Immediate seeding of enzymatically derived endothelium in Dacron vascular grafts. Early experimental studies with autologous canine cells. Arch Surg 1980, 115, 1289–1294. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, M.; Meinhart, J.; Zilla, P.; Howanietz, N.; Gorlitzer, M.; Froeschl, A.; Stuempflen, A.; Bezuidenhout, D.; Grabenwoeger, M. Long-term experience in autologous in vitro endothelialization of infrainguinal ePTFE grafts. J. Vasc. Surg. 2009, 49, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Zilla, P.; Bezuidenhout, D.; Human, P. Prosthetic vascular grafts: Wrong models, wrong questions and no healing. Biomaterials 2007, 28, 5009–5027. [Google Scholar] [CrossRef] [PubMed]
- Alobaid, N.; Salacinski, H.J.; Sales, K.M.; Hamilton, G.; Seifalian, A.M. Single stage cell seeding of small diameter prosthetic cardiovascular grafts. Clin. Hemorheol. Microcirc. 2005, 33, 209–226. [Google Scholar] [PubMed]
- Garcia-Honduvilla, N.; Dominguez, B.; Pascual, G.; Escudero, C.; Minguela, F.; Bellon, J.M.; Bujan, J. Viability of engineered vessels as arterial substitutes. Ann. Vasc. Surg. 2008, 22, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Mirenski, T.L.; Nelson, G.N.; Brennan, M.P.; Roh, J.D.; Hibino, N.; Yi, T.; Shinoka, T.; Breuer, C.K. Tissue-engineered arterial grafts: long.term results after implantation in a small animal model. J. Pediatr. Surg. 2009, 44, 1127–1132. [Google Scholar]
- Shinoka, T.; Breuer, C. Tissue-engineered blood vessels in pediatric cardiac surgery. Yale J. Biol. Med. 2008, 1, 161–166. [Google Scholar]
- Melero-Martin, J.M.; Khan, Z.A.; Picard, A.; Wu, X.; Paruchuri, S.; Bischoff, J. In vivo vasculogenic potential of human blood-derived endothelial progenitor cells. Blood 2007, 109, 4761–4768. [Google Scholar] [CrossRef] [PubMed]
- Urbich, C.; Dimmeler, S. Endothelial progenitor cells: Characterization and role in vascular biology. Circ. Res. 2004, 95, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Jevon, M.; Dorling, A.; Hornick, P.I. Progenitor cells and vascular disease. Cell Prolif. 2008, 41, 146–164. [Google Scholar] [CrossRef] [PubMed]
- Krenning, G.; Moonen, J.R.; van Luyn, M.J.; Harmsen, M.C. Generating new blood flow: integrating developmental biology and tissue engineering. Trends Cardiovasc. Med. 2008, 18, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Rothmans, J.I; Heyligers, J.M.M; Stroes, E.S.G; Pasterkamo, G. Endothelial progenitor cell-seeded grafts: Rash and risky. Can. J. Cardiol. 2006, 22, 929–932. [Google Scholar] [CrossRef] [PubMed]
- Rosso, F.; Giordano, A.; Barbarisi, M.; Barbarisi, A. From cell-ECM interactions to tissue engineering. J. Cell Physiol. 2004, 199, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Alobaid, N.; Salacinski, H.J.; Sales, K.M.; Ramesh, B.; Kannan, R.Y.; Hamilton, G.; Seifalian, A.M. Nanocomposite containing bioactive peptides promote endothelialization by circulating progenitor cells: an in vitro evaluation. Eur. J. Vasc. EndoVasc. Surg. 2006, 32, 76–83. [Google Scholar] [CrossRef] [PubMed]
- Hsu, S.H.; Chu, W.P.; Lin, Y.S.; Chiang, Y.L.; Chen, D.C.; Tsai, C.L. The effect of an RGD-containing fusion protein CBD-RGD in promoting cellular adhesion. J. Biotechnol. 2004, 111, 143–154. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.; Kligman, F.; Larsen, C.C.; Kottke-Marchant, K.; Marchant, R.E. Platelet and endothelial adhesion on fluorosurfactant polymers designed for vascular graft modification. J. Biomed. Mater. Res. A 2009, 88, 348–358. [Google Scholar] [CrossRef] [PubMed]
- Massia, S.P.; Hubbell, J.A. An RGD spacing of 440 nm is sufficient for integrin alpha V beta 3-mediated fibroblast spreading and 140 nm for focal contact and stress fiber formation. J. Cell Biol. 1991, 114, 1089–1100. [Google Scholar] [CrossRef] [PubMed]
- Koo, L.Y.; Irvine, D.J.; Mayes, A.M.; Lauffenburger, D.A.; Griffith, L.G.J. Fibronectin matrix assembly regulates alpha5beta1-mediated cell cohesion. Cell Sci. 2002, 115, 1423–1433. [Google Scholar]
- Patel, S.; Tsang, J.; Harbers, G.M.; Healy, K.E.; Li, S. Regulation of endothelial cell function by GRGDSP peptide grafted on interpenetrating polymers. J. Biomed. Mater. Res. A 2007, 83, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Schense, J.C.; Hubbell, J.A. Three-dimensional migration of neurites is mediated by adhesion site density and affinity. J. Biol. Chem. 2000, 275, 6813–6818. [Google Scholar] [CrossRef] [PubMed]
- Koivunen, E.; Wang, B.C.; Ruoslahti, E. Phage libraries displaying cyclic peptides with different ring sizes: ligand specificities of the RGD-directed integrins. Bio-Technology 1995, 13, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Pierschbacher, M.D.; Ruoslahti, E. Influence of stereochemistry of the sequence Arg-Gly-Asp-Xaa on binding specificity in cell adhesion. J. Biol. Chem. 1987, 262, 17294–17298. [Google Scholar] [PubMed]
- Xiao, Y.; Truskey, G.A. Effect of receptor-ligand affinity on the strength of endothelial cell adhesion. Biophys. J. 1996, 71, 2869–2884. [Google Scholar] [CrossRef] [PubMed]
- Cheng, S.; Craig, W.S.; Mullen, D.; Tschopp, J.F.; Dixon, D.; Pierschbacher, M.D. Design and synthesis of novel cyclic RGD-containing peptides as highly potent and selective integrin alpha IIb beta 3 antagonists. J. Med. Chem. 1994, 37, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Avci-Adali, M.; Paul, A.; Ziemer, G.; Wendel, H.P. New strategies for in vivo tissue engineering by mimicry of homing factors for self-endothelialization of blood contacting materials. Biomaterials 2008, 29, 3936–3945. [Google Scholar] [CrossRef] [PubMed]
- Kutryk, M.J.; Kuliszewski, M.A. In vivo endothelial progenitor cell seeding for the accelerated endothelialisation of endovascular devices. Am. J. Cardiol. 2003, 92, 94L–95L. [Google Scholar] [CrossRef]
- Rossi, M.L.; Zavalloni, D.; Gasparini, G.L.; Mango, R.; Belli, G.; Presbitero, P. The first report of late stent thrombosis leading to acute myocardial infarction in patient receiving the new endothelial progenitor cell capture stent. Int. J. Cardiol. 2009, in press. [Google Scholar]
- Wendel, H.P.; Avci-Adali, M.; Ziemer, G. Endothelial progenitor cell capture stents - hype or hope? Int. J. Cardiol. 2009, in press. [Google Scholar]
- Markway, B.D.; McCarty, O.J.; Marzec, U.M.; Courtman, D.W.; Hanson, S.R.; Hinds, M.T. Capture of flowing endothelial cells using surface-immobilized anti-kinase insert domain receptor antibody. Tissue Eng. C Methods 2008, 14, 97–105. [Google Scholar] [CrossRef]
- Consigny, P.M.; Silverberg, D.A.; Vitali, N.J. Use of endothelial cells containing superparamagnetic microspheres to improve endothelial cell delivery to arterial surfaces after angioplasty. J. Vasc. Interv. Radiol. 1999, 10, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Pislaru, S.V.; Harbuzariu, A.; Agarwal, G.; Witt, T.; Gulati, R.; Sandhu, N.P.; Mueske, C.; Kalra, M.; Simari, R.D.; Sandhu, G.S. Magnetic forces enable rapid endothelialization of synthetic vascular grafts. Circulation 2006, 114, I314–I318. [Google Scholar] [CrossRef] [PubMed]
- Guo, K.T.; Schafer, R.; Paul, A.; Gerber, A.; Ziemer, G.; Wendel, H.P. A new technique for the isolation and surface immobilization of mesenchymal stem cells from whole bone marrow using high-specific DNA aptamers. Stem Cells 2006, 24, 2220–2231. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, J.; Paul, A.; Harwardt, M.; Groll, J.; Reeswinkel, T.; Klee, D.; Moeller, M.; Fischer, H.; Walker, T.; Greiner, T.; Ziemer, G.; Wendel, H.P. Immobilized DNA aptamers used as potent attractors for porcine endothelial precursor cells. J. Biomed. Mater. Res. A 2008, 84, 614–621. [Google Scholar] [CrossRef] [PubMed]
© 2010 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Schopka, S.; Schmid, T.; Schmid, C.; Lehle, K. Current Strategies in Cardiovascular Biomaterial Functionalization. Materials 2010, 3, 638-655. https://doi.org/10.3390/ma3010638
Schopka S, Schmid T, Schmid C, Lehle K. Current Strategies in Cardiovascular Biomaterial Functionalization. Materials. 2010; 3(1):638-655. https://doi.org/10.3390/ma3010638
Chicago/Turabian StyleSchopka, Simon, Thomas Schmid, Christof Schmid, and Karla Lehle. 2010. "Current Strategies in Cardiovascular Biomaterial Functionalization" Materials 3, no. 1: 638-655. https://doi.org/10.3390/ma3010638




