A Recombinant Measles Vaccine with Enhanced Resistance to Passive Immunity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cells and Viruses
2.2. Mouse Inoculations and Sera Transfers
2.3. MV Neutralization Assay
2.4. MV Logarithmic Neutralization Index
2.5. Statistical Analyses
3. Results
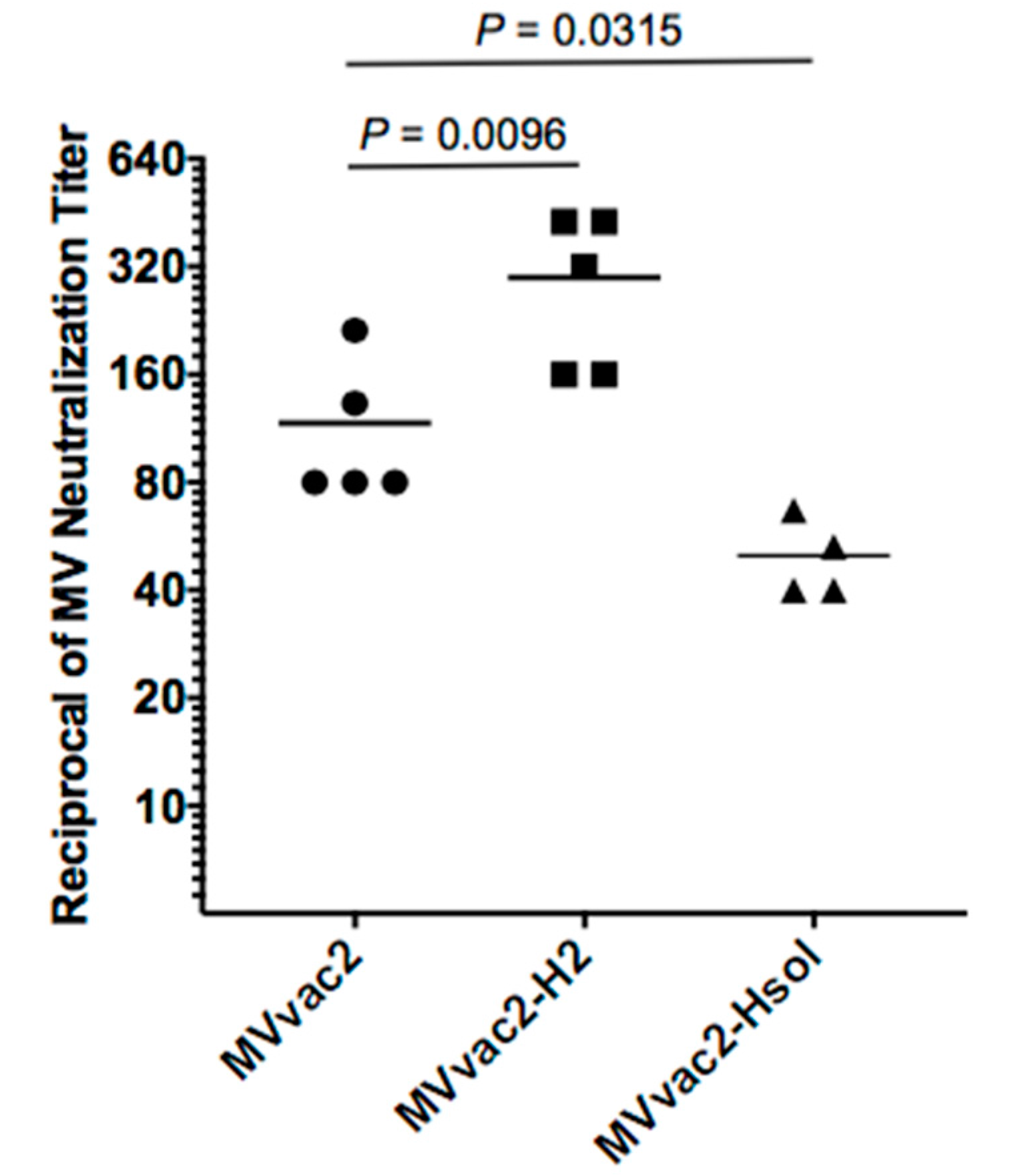
3.1. An MV Incorporating Additional H Is More Immunogenic in Young Mice
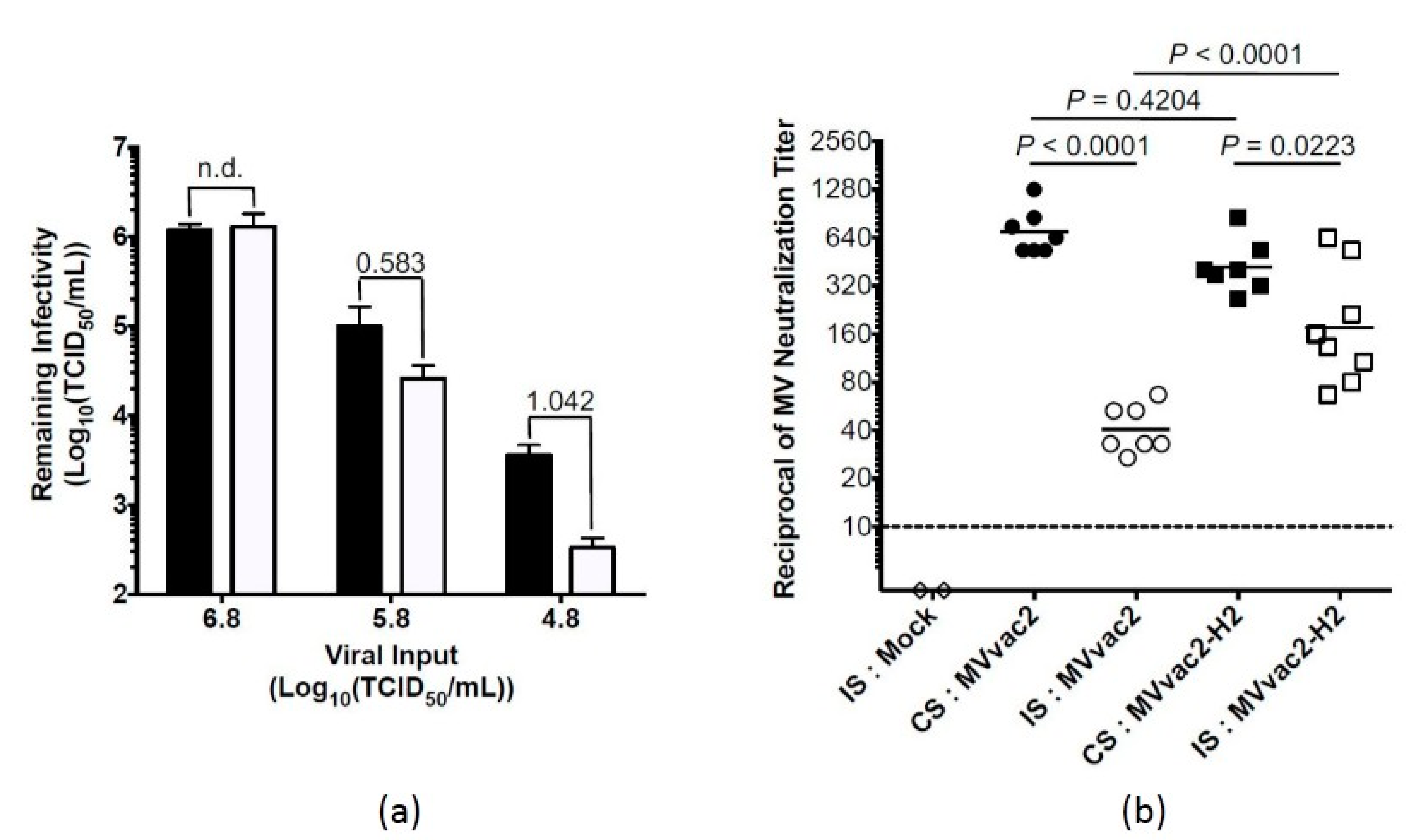
3.2. An MV Incorporating Additional H Is More Immunogenic in the Presence of Artificially Introduced Anti-MV Passive Immunity
3.3. Transfer of Anti-MV Immunity from Dam to Pup and Measles Vaccine Response in Young Mice with Naturally Acquired Passive Immunity
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Perry, R.T.; Murray, J.S.; Gacic-Dobo, M.; Dabbagh, A.; Mulders, M.N.; Strebel, P.M.; Okwo-Bele, J.M.; Rota, P.A.; Goodson, J.L. Progress toward Regional Measles Elimination—Worldwide, 2000–2014. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 1246–1251. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.K.; Gacic-Dobo, M.; Strebel, P.M.; Dabbagh, A.; Mulders, M.N.; Okwo-Bele, J.M.; Dumolard, L.; Rota, P.A.; Kretsinger, K.; Goodson, J.L. Progress toward Regional Measles Elimination—Worldwide, 2000–2015. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 1228–1233. [Google Scholar] [CrossRef] [PubMed]
- Clemmons, N.S.; Gastanaduy, P.A.; Fiebelkorn, A.P.; Redd, S.B.; Wallace, G.S. Measles—United States, January 4–April 2, 2015. MMWR Morb. Mortal. Wkly. Rep. 2016, 64, 373–376. [Google Scholar]
- Haralambieva, I.H.; Kennedy, R.B.; Ovsyannikova, I.G.; Whitaker, J.A.; Poland, G.A. Variability in Humoral Immunity to Measles Vaccine: New Developments. Trends Mol. Med. 2015, 21, 789–801. [Google Scholar] [CrossRef] [PubMed]
- Holzmann, H.; Hengel, H.; Tenbusch, M.; Doerr, H.W. Eradication of Measles: Remaining Challenges. Med. Microbiol. Immunol. 2016, 205, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Moss, W.J.; Strebel, P. Biological Feasibility of Measles Eradication. J. Infect. Dis. 2011, 204, S47–S53. [Google Scholar] [CrossRef] [PubMed]
- Cutts, F.T.; Grabowsky, M.; Markowitz, L.E. The Effect of Dose and Strain of Live Attenuated Measles Vaccines on Serological Responses in Young Infants. Biologicals 1995, 23, 95–106. [Google Scholar] [PubMed]
- Moss, W.J.; Scott, S. Who Immunological Basis for Immunization Series: Measles; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Crowe, J.E., Jr. Influence of Maternal Antibodies on Neonatal Immunization against Respiratory Viruses. Clin. Infect. Dis. 2001, 33, 1720–1727. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, P.; Ennis, F.A.; Saltzman, E.J.; Krugman, S. Persistence of Maternal Antibody in Infants Beyond 12 Months: Mechanism of Measles Vaccine Failure. J. Pediatr. 1977, 91, 715–718. [Google Scholar] [CrossRef]
- Gans, H.; Yasukawa, L.; Rinki, M.; DeHovitz, R.; Forghani, B.; Beeler, J.; Audet, S.; Maldonado, Y.; Arvin, A.M. Immune Responses to Measles and Mumps Vaccination of Infants at 6, 9, and 12 Months. J. Infect. Dis. 2001, 184, 817–826. [Google Scholar] [CrossRef] [PubMed]
- Gans, H.A.; Yasukawa, L.L.; Alderson, A.; Rinki, M.; DeHovitz, R.; Beeler, J.; Audet, S.; Maldonado, Y.; Arvin, A.M. Humoral and Cell-Mediated Immune Responses to an Early 2-Dose Measles Vaccination Regimen in the United States. J. Infect. Dis. 2004, 190, 83–90. [Google Scholar] [CrossRef] [PubMed]
- Gans, H.A.; Arvin, A.M.; Galinus, J.; Logan, L.; DeHovitz, R.; Maldonado, Y. Deficiency of the Humoral Immune Response to Measles Vaccine in Infants Immunized at Age 6 Months. JAMA 1998, 280, 527–532. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, L.J.; Grais, R.F.; Luquero, F.J.; Birmingham, M.E.; Strebel, P.M. Estimates of Measles Case Fatality Ratios: A Comprehensive Review of Community-Based Studies. Int. J. Epidemiol. 2009, 38, 192–205. [Google Scholar] [CrossRef] [PubMed]
- Julik, E.; Valle, J.R.-D. Generation of a More Immunogenic Measles Vaccine by Increasing Its Hemagglutinin Expression. J. Virol. 2016, 90, 5270–5279. [Google Scholar] [CrossRef] [PubMed]
- Markowitz, L.E.; Sepulveda, J.; Diaz-Ortega, J.L.; Valdespino, J.L.; Albrecht, P.; Zell, E.R.; Stewart, J.; Zarate, M.L.; Bernier, R.H. Immunization of Six-Month-Old Infants with Different Doses of Edmonston-Zagreb and Schwarz Measles Vaccines. N. Engl. J. Med. 1990, 322, 580–587. [Google Scholar] [CrossRef] [PubMed]
- Aaby, P.; Jensen, H.; Simondon, F.; Whittle, H. High-Titer Measles Vaccination before 9 Months of Age and Increased Female Mortality: Do We Have an Explanation? Semin. Pediatr. Infect. Dis. 2003, 14, 220–232. [Google Scholar] [CrossRef]
- Del Valle, J.R.; Devaux, P.; Hodge, G.; Wegner, N.J.; McChesney, M.B.; Cattaneo, R. A Vectored Measles Virus Induces Hepatitis B Surface Antigen Antibodies While Protecting Macaques against Measles Virus Challenge. J. Virol. 2007, 81, 10597–10605. [Google Scholar] [CrossRef] [PubMed]
- Mrkic, B.; Pavlovic, J.; Rulicke, T.; Volpe, P.; Buchholz, C.J.; Hourcade, D.; Atkinson, J.P.; Aguzzi, A.; Cattaneo, R. Measles Virus Spread and Pathogenesis in Genetically Modified Mice. J. Virol. 1998, 72, 7420–7427. [Google Scholar] [PubMed]
- Mason, R.A.; Tauraso, N.M.; Spertzel, R.O.; Ginn, R.K. Yellow Fever Vaccine: Direct Challenge of Monkeys Given Graded Doses of 17d Vaccine. Appl. Microbiol. 1973, 25, 539–544. [Google Scholar] [PubMed]
- Harahap-Carrillo, I.S.; Ceballos-Olvera, I.; Valle, J.R. Immunogenic Subviral Particles Displaying Domain Iii of Dengue 2 Envelope Protein Vectored by Measles Virus. Vaccines 2015, 3, 503–518. [Google Scholar] [CrossRef] [PubMed]
- Caceres, V.M.; Strebel, P.M.; Sutter, R.W. Factors Determining Prevalence of Maternal Antibody to Measles Virus Throughout Infancy: A Review. Clin. Infect. Dis. 2000, 31, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Brandler, S.; Ruffie, C.; Combredet, C.; Brault, J.B.; Najburg, V.; Prevost, M.C.; Habel, A.; Tauber, E.; Despres, P.; Tangy, F. A Recombinant Measles Vaccine Expressing Chikungunya Virus-Like Particles Is Strongly Immunogenic and Protects Mice from Lethal Challenge with Chikungunya Virus. Vaccine 2013, 31, 3718–3725. [Google Scholar] [CrossRef] [PubMed]
- Ramsauer, K.; Schwameis, M.; Firbas, C.; Mullner, M.; Putnak, R.J.; Thomas, S.J.; Despres, P.; Tauber, E.; Jilma, B.; Tangy, F. Immunogenicity, Safety, and Tolerability of a Recombinant Measles-Virus-Based Chikungunya Vaccine: A Randomised, Double-Blind, Placebo-Controlled, Active-Comparator, First-in-Man Trial. Lancet Infect. Dis. 2015, 15, 519–527. [Google Scholar] [CrossRef]
- Lin, W.H.; Vilalta, A.; Adams, R.J.; Rolland, A.; Sullivan, S.M.; Griffin, D.E. Vaxfectin Adjuvant Improves Antibody Responses of Juvenile Rhesus Macaques to a DNA Vaccine Encoding the Measles Virus Hemagglutinin and Fusion Proteins. J. Virol. 2013, 87, 6560–6568. [Google Scholar] [CrossRef] [PubMed]
- Mohr, E.; Siegrist, C.A. Vaccination in Early Life: Standing up to the Challenges. Curr. Opin. Immunol. 2016, 41, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Schlereth, B.; Rose, J.K.; Buonocore, L.; Meulen, V.T.; Niewiesk, S. Successful Vaccine-Induced Seroconversion by Single-Dose Immunization in the Presence of Measles Virus-Specific Maternal Antibodies. J. Virol. 2000, 74, 4652–4657. [Google Scholar] [CrossRef] [PubMed]
- Capozzo, A.V.; Ramirez, K.; Polo, J.M.; Ulmer, J.; Barry, E.M.; Levine, M.M.; Pasetti, M.F. Neonatal Immunization with a Sindbis Virus-DNA Measles Vaccine Induces Adult-Like Neutralizing Antibodies and Cell-Mediated Immunity in the Presence of Maternal Antibodies. J. Immunol. 2006, 176, 5671–5681. [Google Scholar] [CrossRef] [PubMed]
- Siegrist, C.A.; Barrios, C.; Martinez, X.; Brandt, C.; Berney, M.; Cordova, M.; Kovarik, J.; Lambert, P.H. Influence of Maternal Antibodies on Vaccine Responses: Inhibition of Antibody but Not T Cell Responses Allows Successful Early Prime-Boost Strategies in Mice. Eur. J. Immunol. 1998, 28, 4138–4148. [Google Scholar] [CrossRef]
- Organization, World Health. Measles Surveillance Data. Available online: http://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/active/measles_monthlydata/en/ (accessed on 3 October 2016).
- Furuse, Y.; Oshitani, H. Global Transmission Dynamics of Measles in the Measles Elimination Era. Viruses 2017, 9. [Google Scholar] [CrossRef] [PubMed]

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Julik, E.; Reyes-del Valle, J. A Recombinant Measles Vaccine with Enhanced Resistance to Passive Immunity. Viruses 2017, 9, 265. https://doi.org/10.3390/v9100265
Julik E, Reyes-del Valle J. A Recombinant Measles Vaccine with Enhanced Resistance to Passive Immunity. Viruses. 2017; 9(10):265. https://doi.org/10.3390/v9100265
Chicago/Turabian StyleJulik, Emily, and Jorge Reyes-del Valle. 2017. "A Recombinant Measles Vaccine with Enhanced Resistance to Passive Immunity" Viruses 9, no. 10: 265. https://doi.org/10.3390/v9100265



