Free-Living Amoebae as Hosts for and Vectors of Intracellular Microorganisms with Public Health Significance
Abstract
:1. Introduction
2. Pathogenic Free-Living Amoebae
3. FLA as Vectors of Diverse Microorganisms (Biodiversity within FLA)
4. Host-Microorganism Interactions
4.1. Amoebal Co-Culture vs. In Situ Interactions
4.2. Interactions of FLA and Bacteria
4.2.1. Legionella pneumophilia
4.2.2. FLA-Bacteria Interactions Other than Legionella
5. Viruses in Close Association with FLA
5.1. Coxsackievirus and Adenovirus
5.2. Mimiviridae
5.3. Marseilleviridae
5.4. Pandoraviruses and Pithoviruses
5.5. Faustovirus and Mollivirus
5.6. Giant Viruses as Putative Pathogens
5.7. Giant Viruses and Evolution
6. Interactions of FLA with Protozoa or Fungi
7. Conclusions
Acknowledgments
Conflicts of Interest
References
- Walochnik, J.; Aspöck, H. Amöben: Paradebeispiele für Probleme der Phylogenetik, Klassifikation und Nomenklatur. Denisia 2007, 20, 323–350. [Google Scholar]
- Adl, S.M.; Simpson, A.G.B.; Farmer, M.A.; Andresen, R.A.; Anderson, O.R.; Barta, J.R.; Bowser, S.S.; Brugerolle, G.; Fensome, R.A.; Fredericq, S.; et al. The new higher level classification of eukaryotes with emphasis on the taxonomy of protists. J. Eukaryot Microbiol 2005, 52, 399–451. [Google Scholar] [CrossRef] [PubMed]
- Trabelsi, H.; Dendana, F.; Sellami, A.; Sellami, H.; Cheikhrouhou, F.; Neji, S.; Makni, F.; Ayadi, A. Pathogenic free-living amoebae: Epidemiology and clinical review. Pathol. Biol. 2012, 60, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Kurek, R.; Scheid, P.; Michel, R. Darstellung von pilzartigen Endoparasiten bei freilebenden Amöben nach spezifischer Fluoreszenzanfärbung. Mikrokosmos 2010, 99, 327–330. [Google Scholar]
- Scheid, P. Relevance of free-living amoebae as hosts for phylogenetically diverse microorganisms. Parasitol. Res. 2014, 113, 2407–2414. [Google Scholar] [CrossRef] [PubMed]
- Booton, G.C.; Visvesvara, G.S.; Byers, T.J.; Kelly, D.J.; Fuerst, P.A. Identification and distribution of Acanthamoeba species genotypes associated with nonkeratitis infections. J. Clin. Microbiol. 2005, 43, 1689–1693. [Google Scholar] [CrossRef] [PubMed]
- Qvarnstrom, Y.; Nerad, T.A.; Visvesvara, G.S. Characterization of a new pathogenic Acanthamoeba species, A. byersi n. sp., isolated from a human with fatal amoebic encephalitis. J. Eukaryot. Microbiol. 2013, 60, 626–633. [Google Scholar] [CrossRef] [PubMed]
- Grün, A.-L.; Stemplewitz, B.; Scheid, P. First report of an Acanthamoeba genotype T13 isolate as etiological agent of a keratitis in humans. Parasitol. Res. 2014, 113, 2395–2400. [Google Scholar] [CrossRef] [PubMed]
- Walochnik, J.; Aspöck, H. Die Diagnostik von Infektionen mit freilebenden Amöben (FLA). Laboratoriums Medizin 2005, 29, 446–456. [Google Scholar] [CrossRef]
- Butt, C.G. Primary amebic meningoencephalitis. N. Engl. J. Med. 1966, 274, 1473–1476. [Google Scholar] [CrossRef] [PubMed]
- Gardner, H.A.; Martinez, A.J.; Visvesvara, G.S.; Sotrel, A. Granulomatous amebic encephalitis in an AIDS patient. Neurology 1991, 41, 1993–1995. [Google Scholar] [CrossRef] [PubMed]
- Scheid, P.; Zoller, L.; Pressmar, S.; Richard, G.; Michel, R. An extraordinary endocytobiont in Acanthamoeba sp. isolated from a patient with keratitis. Parasitol. Res. 2008, 102, 945–950. [Google Scholar] [CrossRef] [PubMed]
- Wright, P. Acanthamoeba keratitis. In Proceedings of the 5th International Conference on the Biology and Pathogenicity of Free-Living Amoebae (FLAM), Brussels, Belgium, August 1989. [Google Scholar]
- Gupta, N.; Bhaskar, H.; Duggal, S.; Ghalaut, P.S.; Kundra, S.; Arora, D.R. Primary Amoebic Meningoencephalitis: First reported case from Rohtak, North India. Braz. J. Infect. Dis. 2009, 13, 236–237. [Google Scholar] [CrossRef] [PubMed]
- Capewell, L.G.; Harris, A.M.; Yoder, J.S.; Cope, J.R.; Eddy, B.A.; Roy, S.L.; Visvesvara, G.S.; Fox, L.M.; Beach, M.J. Diagnosis, clinical course, and treatment of Primary Amoebic Meningoencephalitis in the United States, 1937–2013. J. Pediat. Infect. Dis. 2015, 4, e68–75. [Google Scholar] [CrossRef] [PubMed]
- Martinez, A.J.; Visvesvara, G.S. Free-living, amphizoic and opportunistic amebas. Brain Pathol. 1997, 7, 583–598. [Google Scholar] [CrossRef] [PubMed]
- Marciano-Cabral, F.; Cabral, G.A. The immune response to Naegleria fowleri amebae and pathogenesis of infection. FEMS Immunol. Med. Microbiol. 2007, 51, 243–259. [Google Scholar] [CrossRef] [PubMed]
- Visvesvara, G. Free-living amebae as opportunistic agents of human disease. J. Neuroparasitol. 2010, 1, N100802. [Google Scholar] [CrossRef]
- Scheid, P. Balamuthiose. In Handbuch der Infektionskrankheiten; Hofmann, F., Ed.; ecomed Verlag: Hamburg, Germany, 2012. [Google Scholar]
- Siddiqui, R.; Khan, N.A. Balamuthia amoebic encephalitis: An emerging disease with fatal consequences. Microb. Pathog. 2008, 44, 89–97. [Google Scholar] [CrossRef] [PubMed]
- Balczun, C.; Scheid, P.L. Detection of Balamuthia mandrillaris DNA in the storage case of contact lenses in Germany. Parasitol. Res. 2016, 115, 2111–2114. [Google Scholar] [CrossRef] [PubMed]
- Gelman, B.B.; Popov, V.; Chaljub, G.; Nader, R.; Rauf, S.J.; Nauta, H.W.; Visvesvara, G.S. Neuropathological and ultrastructural features of amebic encephalitis caused by Sappinia diploidea. J. Neuropathol. Exp. Neurol. 2003, 62, 990–998. [Google Scholar] [CrossRef] [PubMed]
- Qvarnstrom, Y.; da Silva, A.J.; Schuster, F.L.; Gelman, B.B.; Visvesvara, G.S. Molecular confirmation of Sappinia pedata as a causative agent of amoebic encephalitis. J. Infect. Dis. 2009, 199, 1139–1142. [Google Scholar] [CrossRef] [PubMed]
- De Jonckheere, J.F.; Brown, S. Non-Acanthamoeba amoebic keratitis. Cornea 1999, 18, 499–501. [Google Scholar] [CrossRef] [PubMed]
- Tsvetkova, N.; Schild, M.; Panaiotov, S.; Kurdova-Mintcheva, R.; Gottstein, B.; Walochnik, J.; Aspock, H.; Lucas, M.S.; Muller, N. The identification of free-living environmental isolates of amoebae from Bulgaria. Parasitol. Res. 2004, 92, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Aitken, D.; Hay, J.; Kinnear, F.B.; Kirkness, C.M.; Lee, W.R.; Seal, D.V. Amebic keratitis in a wearer of disposable contact lenses due to a mixed Vahlkampfia and Hartmannella infection. Ophthalmology 1996, 103, 485–494. [Google Scholar] [CrossRef]
- Visvesvara, G.S.; Sriram, R.; Qvarnstrom, Y.; Bandyopadhyay, K.; da Silva, A.J.; Pieniazek, N.J.; Cabral, G.A. Paravahlkampfia francinae n. sp. masquerading as an agent of primary amoebic meningoencephalitis. J. Eukaryot. Microbiol. 2009, 56, 357–366. [Google Scholar] [CrossRef] [PubMed]
- Tolba, M.E.M.; Huseein, E.A.M.; Farrag, H.M.M.; Mohamed, H.E.D.; Kobayashi, S.; Suzuki, J.; Ali, T.A.M.; Sugano, S. Allovahlkampfia spelaea causing keratitis in humans. PLoS Negl. Trop. Dis. 2016, 10, e0004841. [Google Scholar] [CrossRef] [PubMed]
- Reddy, A.K.; Balne, P.K.; Garg, P.; Sangwan, V.S.; Das, M.; Krishna, P.V.; Bagga, B.; Vemuganti, G.K. Dictyostelium polycephalum infection of human cornea. Emerg. Infect. Dis. 2010, 16, 1644–1645. [Google Scholar] [CrossRef] [PubMed]
- Ashbolt, N.J. Environmental (saprozoic) pathogens of engineered water systems: Understanding their ecology for risk assessment and management. Pathogens 2015, 4, 390–405. [Google Scholar] [CrossRef] [PubMed]
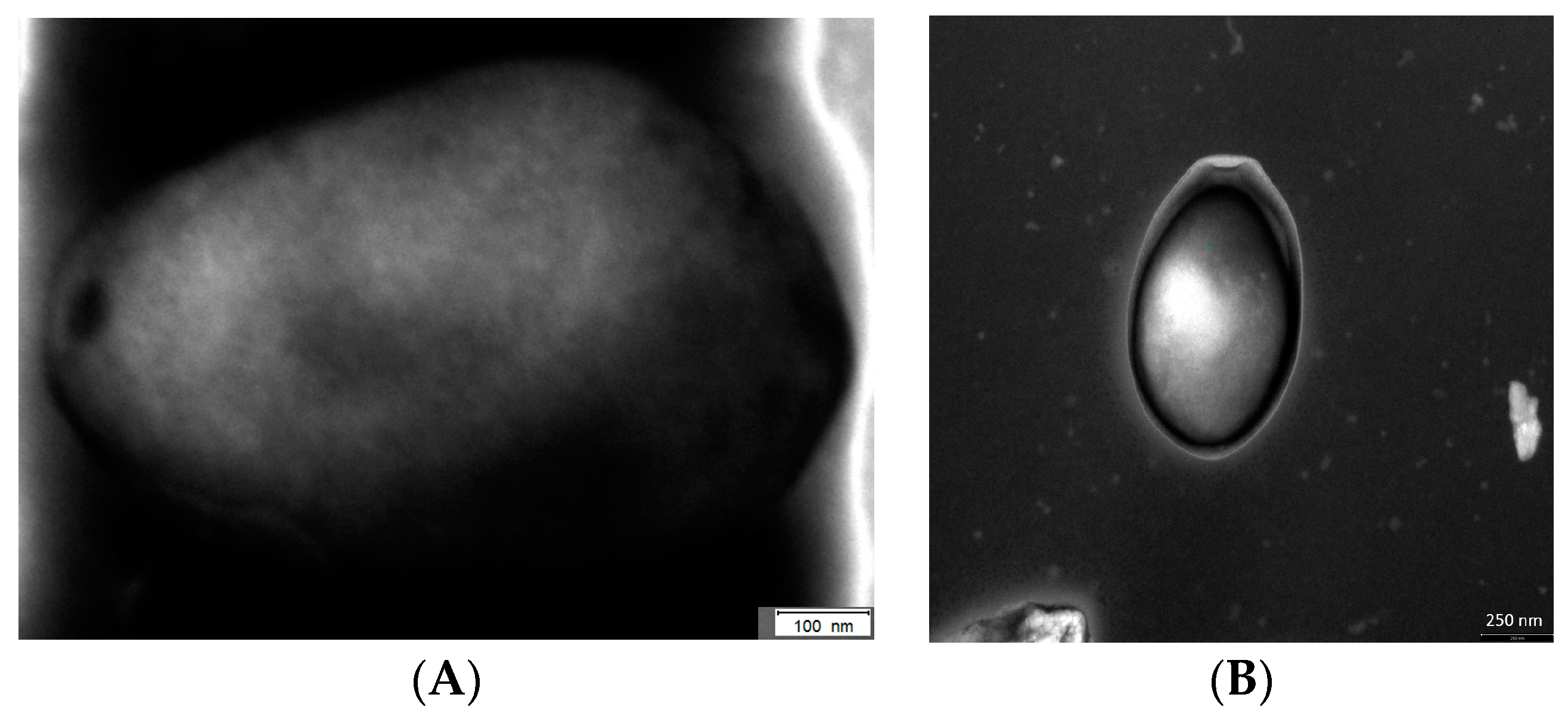
- Scheid, P.; Hauroder, B.; Michel, R. Investigations of an extraordinary endocytobiont in Acanthamoeba sp.: Development and replication. Parasitol. Res. 2010, 106, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Fields, B.S.; Barbaree, J.M.; Shotts, E.B., Jr.; Feeley, J.C.; Morrill, W.E.; Sanden, G.N.; Dykstra, M.J. Comparison of guinea pig and protozoan models for determining virulence of Legionella species. Infect. Immun. 1986, 53, 553–559. [Google Scholar] [PubMed]
- Fenner, L.; Richet, H.; Raoult, D.; Papazian, L.; Martin, C.; La Scola, B. Are clinical isolates of Pseudomonas aeruginosa more virulent than hospital environmental isolates in amebal co-culture test? Crit. Care Med. 2006, 34, 823–828. [Google Scholar] [CrossRef] [PubMed]
- Goy, G.; Thomas, V.; Rimann, K.; Jaton, K.; Prod’hom, G.; Greub, G. The Neff strain of Acanthamoeba castellanii, a tool for testing the virulence of Mycobacterium kansasii. Res. Microbiol. 2007, 158, 393–397. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, K.M.; Levin, B.R. Grazing protozoa and the evolution of the Escherichia coli O157:H7 Shiga toxin-encoding prophage. Proc. Biol. Sci. 2007, 274, 1921–1929. [Google Scholar] [CrossRef] [PubMed]
- Greub, G.; Raoult, D. Microorganisms resistant to free-living amoebae. Clin. Microbiol. Rev. 2004, 17, 413–433. [Google Scholar] [CrossRef] [PubMed]
- Barker, J.; Lambert, P.A.; Brown, M.R. Influence of intra-amoebic and other growth conditions on the surface properties of Legionella pneumophila. Infect. Immun. 1993, 61, 3503–3510. [Google Scholar] [PubMed]
- Steinert, M.; Birkness, K.; White, E.; Fields, B.; Quinn, F. Mycobacterium avium bacilli grow saprozoically in coculture with Acanthamoeba polyphaga and survive within cyst walls. Appl. Environ. Microbiol. 1998, 64, 2256–2261. [Google Scholar] [PubMed]
- Fritsche, T.R.; Sobek, D.; Gautom, R.K. Enhancement of in vitro cytopathogenicity by Acanthamoeba spp. following acquisition of bacterial endosymbionts. FEMS Microbiol. Lett. 1998, 166, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Molmeret, M.; Horn, M.; Wagner, M.; Santic, M.; Abu Kwaik, Y. Amoebae as training grounds for intracellular bacterial pathogens. Appl. Environ. Microbiol. 2005, 71, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Cirillo, J.D.; Falkow, S.; Tompkins, L.S.; Bermudez, L.E. Interaction of Mycobacterium avium with environmental amoebae enhances virulence. Infect. Immun. 1997, 65, 3759–3767. [Google Scholar] [PubMed]
- Steenbergen, J.N.; Shuman, H.A.; Casadevall, A. Cryptococcus neoformans interactions with amoebae suggest an explanation for its virulence and intracellular pathogenic strategy in macrophages. Proc. Natl. Acad. Sci. USA 2001, 98, 15245–15250. [Google Scholar] [CrossRef] [PubMed]
- Brieland, J.K.; Fantone, J.C.; Remick, D.G.; LeGendre, M.; McClain, M.; Engleberg, N.C. The role of Legionella pneumophila-infected Hartmannella vermiformis as an infectious particle in a murine model of Legionaires’ disease. Infect. Immun. 1997, 65, 5330–5333. [Google Scholar] [PubMed]
- Thomas, V.; McDonnell, G.; Denyer, S.P.; Maillard, J.-Y. Free-living amoebae and their intracellular pathogenic microorganisms: Risks for water quality. FEMS Microbiol. Rev. 2010, 34, 231–259. [Google Scholar] [CrossRef] [PubMed]
- Goñi, P.; Fernández, M.T.; Rubio, E. Identifying endosymbiont bacteria associated with free-living amoebae. Environ. Microbiol. 2014, 16, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Reteno, D.G.; Benamar, S.; Khalil, J.B.; Andreani, J.; Armstrong, N.; Klose, T.; Rossmann, M.; Colson, P.; Raoult, D.; La Scola, B. Faustovirus, an asfarvirus-related new lineage of giant viruses infecting amoebae. J. Virol. 2015, 89, 6585–6594. [Google Scholar] [CrossRef] [PubMed]
- Drozanski, W. Fatal bacterial infection in soil amoebae. Acta Microbiol. Pol. 1956, 5, 315–317. [Google Scholar]
- Drozanski, W.J. Sarcobium lyticum gen. nov., sp. nov., an obligate intracellular bacterial parasite of small free-living amoebae. Int. J. System. Bacteriol. 1991, 41, 82–87. [Google Scholar] [CrossRef]
- Adeleke, A.A.; Fields, B.S.; Benson, R.F.; Daneshvar, M.I.; Pruckler, J.M.; Ratcliff, R.M.; Harrison, T.G.; Weyant, R.S.; Birtles, R.J.; Raoult, D.; et al. Legionella drozanskii sp. nov., Legionella rowbothamii sp. nov. and Legionella fallonii sp. nov.: Three unusual new Legionella species. Int. J. Syst. Evol. Microbiol. 2001, 51, 1151–1160. [Google Scholar] [CrossRef] [PubMed]
- Michel, R.; Muller, K.D.; Amann, R.; Schmid, E.N. Legionella-like slender rods multiplying within a strain of Acanthamoeba sp. isolated from drinking water. Parasitol. Res. 1998, 84, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Rowbotham, T.J. Preliminary report on the pathogenicity of Legionella pneumophila for freshwater and soil amoebae. J. Clin. Pathol. 1980, 33, 1179–1183. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.; Keevil, C.W. Immunogold and fluorescein immunolabelling of Legionella pneumophila within an aquatic biofilm visualized by using episcopic differential interference contrast microscopy. Appl. Environ. Microbiol. 1992, 58, 2326–2330. [Google Scholar] [PubMed]
- Boulanger, C.A.; Edelstein, P.H. Precision and accuracy of recovery of Legionella pneumophila from seeded tap water by filtration and centrifugation. Appl. Environ. Microbiol. 1995, 61, 1805–1809. [Google Scholar] [PubMed]
- Hägele, S.; Kohler, R.; Merkert, H.; Schleicher, M.; Hacker, J.; Steinert, M. Dictyostelium discoideum: A new host model system for intracellular pathogens of the genus Legionella. Cell. Microbiol. 2000, 2, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Hookey, J.V.; Saunders, N.A.; Fry, N.K.; Birtles, R.J.; Harrison, T.G. Phylogeny of Legionellaceae based on small-subunit ribosomal DNA sequences and proposal of Legionella lytica comb. nov. for Legionella-like amoebal pathogens. Int. J. System. Bacteriol. 1996, 46, 526–531. [Google Scholar] [CrossRef]
- Akya, A.; Pointon, A.; Thomas, C. Mechanism involved in phagocytosis and killing of Listeria monocytogenes by Acanthamoeba polyphaga. Parasitol. Res. 2009, 105, 1375–1383. [Google Scholar] [CrossRef] [PubMed]
- Ly, T.M.; Muller, H.E. Ingested Listeria monocytogenes survive and multiply in protozoa. J. Med. Microbiol. 1990, 33, 51–54. [Google Scholar] [CrossRef] [PubMed]
- White, C.I.; Birtles, R.J.; Wigley, P.; Jones, P.H. Mycobacterium avium subspecies paratuberculosis in free-living amoebae isolated from fields not used for grazing. Vet. Rec. 2010, 166, 401–402. [Google Scholar] [CrossRef] [PubMed]
- La Scola, B.; Raoult, D. Afipia felis in hospital water supply in association with free-living amoebae. Lancet 1999, 353, 1330. [Google Scholar] [CrossRef]
- Hoffmann, R.; Michel, R. Distribution of free-living amoebae (FLA) during preparation and supply of drinking water. Int. J. Hyg. Environ. Health. 2001, 203, 215–219. [Google Scholar] [CrossRef]
- Michel, R.; Müller, K.-D.; Schmid, E. Ehrlichia-like organismus (KSL1) observed as obligate intracellular parasites of Saccamoeba species. Endocytobio. Cell Res. 1995, 11, 69–80. [Google Scholar]
- Michel, R. Freilebende Amöben als Wirte und Vehikel von Mikroorganismen. Mitteilungen der Österreichischen Gesellschaft für Tropenmedizin und Parasitologie 1997, 19, 11–20. [Google Scholar]
- Corsaro, D.; Muller, K.-D.; Michel, R. Molecular characterization and ultrastructure of a new amoeba endoparasite belonging to the Stenotrophomonas maltophilia complex. Exp. Parasitol. 2013, 133, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Kahane, S.; Dvoskin, B.; Mathias, M.; Friedman, M.G. Infection of Acanthamoeba polyphaga with Simkania negevensis and S. negevensis survival within amoebal cysts. Appl. Environ. Microbiol. 2001, 67, 4789–4795. [Google Scholar] [CrossRef] [PubMed]
- Michel, R.; Muller, K.-D.; Zöller, L.; Walochnik, J.; Hartmann, M.; Schmid, E. Free living amoebae serve as host for the Chlamydia-like bacterium Simkania nevegensis. Acta Protozool. 2005, 44, 113–121. [Google Scholar]
- Hennig, K.; Zöller, L.; Hauröder, B.; Hotzel, H.; Michel, R. Hartmannella vermiformis (Hartmannellidae) harboured a hidden Chlamydia-like endosymbiont. Endocytobio. Cell Res. 2007, 18, 1–10. [Google Scholar]
- Horn, M.; Wagner, M.; Muller, K.D.; Schmid, E.N.; Fritsche, T.R.; Schleifer, K.H.; Michel, R. Neochlamydia hartmannellae gen. nov., sp. nov. (Parachlamydiaceae), an endoparasite of the amoeba Hartmannella vermiformis. Microbiology 2000, 146, 1231–1239. [Google Scholar] [CrossRef] [PubMed]
- Corsaro, D.; Müller, K.D.; Wingender, J.; Michel, R. “Candidatus Mesochlamydia elodeae” (Chlamydiae: Parachlamydiaceae), a novel chlamydia parasite of free-living amoebae. Parasitol. Res. 2013, 112, 829–1838. [Google Scholar] [CrossRef] [PubMed]
- Horn, M.; Fritsche, T.R.; Gautom, R.K.; Schleifer, K.H.; Wagner, M. Novel bacterial endosymbionts of Acanthamoeba spp. related to the Paramecium caudatum symbiont Caedibacter caryophilus. Environ. Microbiol. 1999, 1, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Horn, M.; Fritsche, T.R.; Linner, T.; Gautom, R.K.; Harzenetter, M.D.; Wagner, M. Obligate bacterial endosymbionts of Acanthamoeba spp. related to the beta-Proteobacteria: Proposal of ‘Candidatus Procabacter acanthamoebae’ gen. nov., sp. nov. Int. J. Syst. Evol. Microbiol. 2002, 52, 599–605. [Google Scholar] [CrossRef] [PubMed]
- Horn, M.; Harzenetter, M.D.; Linner, T.; Schmid, E.N.; Muller, K.D.; Michel, R.; Wagner, M. Members of the Cytophaga-Flavobacterium-Bacteroides phylum as intracellular bacteria of acanthamoebae: Proposal of ‘Candidatus Amoebophilus asiaticus’. Environ. Microbiol. 2001, 3, 440–449. [Google Scholar] [CrossRef] [PubMed]
- Gaze, W.H.; Burroughs, N.; Gallagher, M.P.; Wellington, E.M.H. Interactions between Salmonella typhimurium and Acanthamoeba polyphaga, and observation of a new mode of intracellular growth within contractile vacuoles. Microb. Ecol. 2003, 46, 358–369. [Google Scholar] [CrossRef] [PubMed]
- Tezcan-Merdol, D.; Ljungstrom, M.; Winiecka-Krusnell, J.; Linder, E.; Engstrand, L.; Rhen, M. Uptake and replication of Salmonella enterica in Acanthamoeba rhysodes. Appl. Environ. Microbiol. 2004, 70, 3706–3714. [Google Scholar] [CrossRef] [PubMed]
- King, C.H.; Shotts, E.B., Jr.; Wooley, R.E.; Porter, K.G. Survival of coliforms and bacterial pathogens within protozoa during chlorination. Appl. Environ. Microbiol. 1988, 54, 3023–3033. [Google Scholar] [PubMed]
- Snelling, W.J.; McKenna, J.P.; Lecky, D.M.; Dooley, J.S.G. Survival of Campylobacter jejuni in waterborne protozoa. Appl. Environ. Microbiol. 2005, 71, 5560–5571. [Google Scholar] [CrossRef] [PubMed]
- Medina, G.; Flores-Martin, S.; Fonseca, B.; Otth, C.; Fernandez, H. Mechanisms associated with phagocytosis of Arcobacter butzleri by Acanthamoeba castellanii. Parasitol. Res. 2014, 113, 1933–1942. [Google Scholar] [CrossRef] [PubMed]
- Fernández, H.; Villanueva, M.P.; Medina, G. Endosimbiosis de Arcobacter butzleri en Acanthamoeba castellanii. Rev. Argent. Microbiol. 2012, 44, 133. [Google Scholar] [PubMed]
- Mella, C.; Medina, G.; Flores-Martin, S.; Toledo, Z.; Simaluiza, R.J.; Péréz-Péréz, G.; Fernández, H. Interaction between zoonotic bacteria and free living amoebas. A new angle of an epidemiological polyhedron of public health importance? Archivos de Medicina Veterinaria 2016, 48, 1–10. [Google Scholar] [CrossRef]
- Jadin, J.; Francois, J.; Bisoux, M.; Languillon, J.; Moris, R. Dévelopment intranucléaire de Mycobacterium leprae dans les cellules histiocytaires chez l‘animal. Bull. Acad. Natl. Med. 1968, 152, 89–91. [Google Scholar] [PubMed]
- Krishna-Prasad, B.; Gupta, S. Preliminary report on engulfment and retention of mycobacteria by trophozoites of axenically grown Acanthamoeba castellanii Douglas. Curr. Sci. 1978, 47, 245–247. [Google Scholar]
- Alsam, S.; Khan, N. (Eds.) Methicillin resistant Staphylococcus aureus interactions with Acanthamoeba. In Proceedings of the Booklet Free Living Amoebae (FLAM) Meeting, Tenerife Spain, May 2009. [Google Scholar]
- Tomov, A.T.; Tsvetkova, E.D.; Tomova, I.A.; Michailova, L.I.; Kassovski, V.K. Persistence and multiplication of obligate anaerobe bacteria in amebae under aerobic conditions. Anaerobe 1999, 5, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Drancourt, M.; Adekambi, T.; Raoult, D. Interactions between Mycobacterium xenopi, amoeba and human cells. J. Hosp. Infect. 2007, 65, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Dey, R.; Hoffman, P.S.; Glomski, I.J. Germination and amplification of anthrax spores by soil-dwelling amoebas. Appl. Environ. Microbiol. 2012, 78, 8075–8081. [Google Scholar] [CrossRef] [PubMed]
- Thomas, V.; Loret, J.-F.; Jousset, M.; Greub, G. Biodiversity of amoebae and amoebae-resisting bacteria in a drinking water treatment plant. Environ. Microbiol. 2008, 10, 2728–2745. [Google Scholar] [CrossRef] [PubMed]
- Landers, P.; Kerr, K.G.; Rowbotham, T.J.; Tipper, J.L.; Keig, P.M.; Ingham, E.; Denton, M. Survival and growth of Burkholderia cepacia within the free-living amoeba Acanthamoeba polyphaga. Eur. J. Clin. Microbiol. Infect. Dis. 2000, 19, 121–123. [Google Scholar] [CrossRef] [PubMed]
- Barker, J.; Humphrey, T.J.; Brown, M.W. Survival of Escherichia coli O157 in a soil protozoan: Implications for disease. FEMS Microbiol. Lett. 1999, 173, 291–295. [Google Scholar] [CrossRef] [PubMed]
- Winiecka-Krusnell, J.; Wreiber, K.; von Euler, A.; Engstrand, L.; Linder, E. Free-living amoebae promote growth and survival of Helicobacter pylori. Scand. J. Infect. Dis. 2002, 34, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Wagner, Y.; Noack, B.; Hoffmann, T.; Jacobs, E.; Christian Luck, P. Periodontopathogenic bacteria multiply in the environmental amoeba Acanthamoeba castellani. Int. J. Hyg. Environ. Health. 2006, 209, 535–539. [Google Scholar] [CrossRef] [PubMed]
- Essig, A.; Heinemann, M.; Simnacher, U.; Marre, R. Infection of Acanthamoeba castellanii by Chlamydia pneumoniae. Appl. Environ. Microbiol. 1997, 63, 1396–1399. [Google Scholar] [PubMed]
- Michel, R.; Hauröder-Philippczyk, B.; Müller, K.-D.; Weishaar, I. Acanthamoeba from human nasal mucosa infected with an obligate intracellular parasite. Europ. J. Protistol. 1994, 30, 104–110. [Google Scholar] [CrossRef]
- Amann, R.; Springer, N.; Schonhuber, W.; Ludwig, W.; Schmid, E.N.; Muller, K.D.; Michel, R. Obligate intracellular bacterial parasites of acanthamoebae related to Chlamydia spp. Appl. Environ. Microbiol. 1997, 63, 115–121. [Google Scholar] [PubMed]
- Everett, K.D.; Bush, R.M.; Andersen, A.A. Emended description of the order Chlamydiales, proposal of Parachlamydiaceae fam. nov. and Simkaniaceae fam. nov., each containing one monotypic genus, revised taxonomy of the family Chlamydiaceae, including a new genus and five new species, and standards for the identification of organisms. Int. J. System. Bacteriol. 1999, 49 Pt 2, 415–440. [Google Scholar]
- Michel, R.; Muller, K.D.; Hoffmann, R. Enlarged Chlamydia-like organisms as spontaneous infection of Acanthamoeba castellanii. Parasitol. Res. 2001, 87, 248–251. [Google Scholar] [CrossRef] [PubMed]
- Michel, R.; Steinert, M.; Zöller, L.; Hauröder, B.; Hennig, K. Cocultivation of protozoa and the Chlamydia-like bacterium Waddlia chondrophila isolated from an aborted bovine foetus in Germany. Acta Protozool. 2004, 43, 37–42. [Google Scholar]
- Collingro, A.; Poppert, S.; Heinz, E.; Schmitz-Esser, S.; Essig, A.; Schweikert, M.; Wagner, M.; Horn, M. Recovery of an environmental Chlamydia strain from activated sludge by co-cultivation with Acanthamoeba sp. Microbiology 2005, 151, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Heinz, E.; Kolarov, I.; Kastner, C.; Toenshoff, E.R.; Wagner, M.; Horn, M. An Acanthamoeba sp. containing two phylogenetically different bacterial endosymbionts. Environ. Microbiol. 2007, 9, 1604–1609. [Google Scholar] [CrossRef] [PubMed]
- La Scola, B.; Raoult, D. Survival of Coxiella burnetii within free-living amoeba Acanthamoeba castellanii. Clin. Microbiol. Infect. 2001, 7, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, K. Growth and survival of four strains of Francisella tularensis in a rich medium preconditioned with Acanthamoeba palestinensis. Can. J. Microbiol. 1989, 35, 1100–1104. [Google Scholar] [CrossRef] [PubMed]
- Scheid, P.; Schwarzenberger, R.; Schacht, E.; Splettstoesser, W. Free-living amoebae as hosts and vehicles of Francisella sp. In Proceedings of the Medical Biodefense conference, Medical Corps International Forum 2011. Munich, Germany, 2011. [Google Scholar]
- Abd, H.; Johansson, T.; Golovliov, I.; Sandstrom, G.; Forsman, M. Survival and growth of Francisella tularensis in Acanthamoeba castellanii. Appl. Environ. Microbiol. 2003, 69, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Abd, H. Interaction between waterborne pathogenic bacteria and Acanthamoeba castellanii; Dissertation: Stockholm, Sweden, 2006. [Google Scholar]
- Corsaro, D.; Walochnik, J.; Venditti, D.; Steinmann, J.; Muller, K.-D.; Michel, R. Microsporidia-like parasites of amoebae belong to the early fungal lineage Rozellomycota. Parasitol. Res. 2014, 113, 1909–1918. [Google Scholar] [CrossRef] [PubMed]
- Koehsler, M.; Walochnik, J.; Michel, R.; Lugauer, J.; Wylezich, C. Molecular identification and classification of Cochlonema euryblastum, a zoopagalean parasite of Thecamoeba quadrilineata. Mycologia 2007, 99, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Scheid, P.L.; Schwarzenberger, R. Free-living amoebae as vectors of cryptosporidia. Parasitol. Res. 2011, 109, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Ryan, U.; Zahedi, A.; Paparini, A. Cryptosporidium in humans and animals-a one health approach to prophylaxis. Parasite Immunol. 2016, 38, 535–547. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Couso, H.; Paniagua-Crespo, E.; Ares-Mazas, E. Acanthamoeba as a temporal vehicle of Cryptosporidium. Parasitol. Res. 2007, 100, 1151–1154. [Google Scholar] [CrossRef] [PubMed]
- Lorenzo-Morales, J.; Coronado-Alvarez, N.; Martinez-Carretero, E.; Maciver, S.K.; Valladares, B. Detection of four adenovirus serotypes within water-isolated strains of Acanthamoeba in the Canary Islands, Spain. Am. J. Trop. Med. Hyg. 2007, 77, 753–756. [Google Scholar] [PubMed]
- La Scola, B.; Audic, S.; Robert, C.; Jungang, L.; de Lamballerie, X.; Drancourt, M.; Birtles, R.; Claverie, J.-M.; Raoult, D. A giant virus in amoebae. Science 2003, 299, 2033. [Google Scholar] [PubMed]
- Hoffmann, R.; Michel, R.; Muller, K.D.; Schmid, E. Archaea-like endocytobiotic organisms isolated from Acanthamoeba sp. (Gr II). Endocytobio. Cell Res. 1998, 12, 185–188. [Google Scholar]
- Scheid, P.; Schwarzenberger, R. Acanthamoeba spp. as vehicle and reservoir of adenoviruses. Parasitol. Res. 2012, 111, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Mattana, A.; Serra, C.; Mariotti, E.; Delogu, G.; Fiori, P.L.; Cappuccinelli, P. Acanthamoeba castellanii promotion of in vitro survival and transmission of coxsackie b3 viruses. Eukaryotic Cell 2006, 5, 665–671. [Google Scholar] [CrossRef] [PubMed]
- Boyer, M.; Yutin, N.; Pagnier, I.; Barrassi, L.; Fournous, G.; Espinosa, L.; Robert, C.; Azza, S.; Sun, S.; Rossmann, M.G.; et al. Giant Marseillevirus highlights the role of amoebae as a melting pot in emergence of chimeric microorganisms. Proc. Natl. Acad. Sci. USA 2009, 106, 21848–21853. [Google Scholar] [CrossRef] [PubMed]
- Arslan, D.; Legendre, M.; Seltzer, V.; Abergel, C.; Claverie, J.-M. Distant Mimivirus relative with a larger genome highlights the fundamental features of Megaviridae. Proc. Natl. Acad. Sci. USA 2011, 108, 17486–17491. [Google Scholar] [CrossRef] [PubMed]
- Philippe, N.; Legendre, M.; Doutre, G.; Coute, Y.; Poirot, O.; Lescot, M.; Arslan, D.; Seltzer, V.; Bertaux, L.; Bruley, C.; et al. Pandoraviruses: Amoeba viruses with genomes up to 2.5 Mb reaching that of parasitic eukaryotes. Science 2013, 341, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Legendre, M.; Bartoli, J.; Shmakova, L.; Jeudy, S.; Labadie, K.; Adrait, A.; Lescot, M.; Poirot, O.; Bertaux, L.; Bruley, C.; et al. Thirty-thousand-year-old distant relative of giant icosahedral DNA viruses with a pandoravirus morphology. Proc. Natl. Acad. Sci. USA 2014, 111, 4274–4279. [Google Scholar] [CrossRef] [PubMed]
- Legendre, M.; Lartigue, A.; Bertaux, L.; Jeudy, S.; Bartoli, J.; Lescot, M.; Alempic, J.-M.; Ramus, C.; Bruley, C.; Labadie, K.; et al. In-depth study of Mollivirus sibericum, a new 30,000-y-old giant virus infecting Acanthamoeba. Proc. Natl. Acad. Sci. USA 2015, 112, E5327–E5335. [Google Scholar] [CrossRef] [PubMed]
- Ecke, D.J.; Sampath, R.; Willett, P.; Samant, V.; Massire, C.; Hall, T.A.; Hari, K.; McNeil, J.A.; Buchen-Osmond, C.; Budowle, B. The Microbial Rosetta Stone database: A common structure for microbial biosecurity threat agents. J. Forensic Sci. 2005, 50, 1380–1385. [Google Scholar] [PubMed]
- Adékambi, T.; Ben Salah, S.; Khlif, M.; Raoult, D.; Drancourt, M. Survival of environmental mycobacteria in Acanthamoeba polyphaga. Appl. Environ. Microbiol. 2006, 72, 5974–5981. [Google Scholar] [CrossRef] [PubMed]
- Thomas, V.; McDonnell, G. Relationship between mycobacteria and amoebae: Ecological and epidemiological concerns. Lett. Appl. Microbiol. 2007, 45, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Kilvington, S.; Price, J. Survival of Legionella pneumophila within cysts of Acanthamoeba polyphaga following chlorine exposure. J. Appl. Bacteriol. 1990, 68, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Fallon, R.J.; Rowbotham, T.J. Microbiological investigations into an outbreak of Pontiac fever due to Legionella micdadei associated with use of a whirlpool. J. Clin. Pathol. 1990, 43, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Thom, S.; Warhurst, D.; Drasar, B.S. Association of Vibrio cholerae with fresh water amoebae. J. Med. Microbiol. 1992, 36, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Howard, K.; Inglis, T.J.J. Disinfection of Burkholderia pseudomallei in potable water. Water Res. 2005, 39, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Bruggemann, H.; Hagman, A.; Jules, M.; Sismeiro, O.; Dillies, M.-A.; Gouyette, C.; Kunst, F.; Steinert, M.; Heuner, K.; Coppee, J.-Y.; et al. Virulence strategies for infecting phagocytes deduced from the in vivo transcriptional program of Legionella pneumophila. Cell. Microbiol. 2006, 8, 1228–1240. [Google Scholar] [CrossRef] [PubMed]
- Steinert, M.; Emody, L.; Amann, R.; Hacker, J. Resuscitation of viable but nonculturable Legionella pneumophila Philadelphia JR32 by Acanthamoeba castellanii. Appl. Environ. Microbiol. 1997, 63, 2047–2053. [Google Scholar] [PubMed]
- Barker, J.; Brown, M.R.; Collier, P.J.; Farrell, I.; Gilbert, P. Relationship between Legionella pneumophila and Acanthamoeba polyphaga: Physiological status and susceptibility to chemical inactivation. Appl. Environ. Microbiol. 1992, 58, 2420–2425. [Google Scholar] [PubMed]
- Axelsson-Olsson, D.; Waldenstrom, J.; Broman, T.; Olsen, B.; Holmberg, M. Protozoan Acanthamoeba polyphaga as a potential reservoir for Campylobacter jejuni. Appl. Environ. Microbiol. 2005, 71, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Axelsson-Olsson, D.; Svensson, L.; Olofsson, J.; Salomon, P.; Waldenstrom, J.; Ellstrom, P.; Olsen, B. Increase in acid tolerance of Campylobacter jejuni through coincubation with amoebae. Appl. Environ. Microbiol. 2010, 76, 4194–4200. [Google Scholar] [CrossRef] [PubMed]
- Snelling, W.J.; Stern, N.J.; Lowery, C.J.; Moore, J.E.; Gibbons, E.; Baker, C.; Dooley, J.S.G. Colonization of broilers by Campylobacter jejuni internalized within Acanthamoeba castellanii. Arch. Microbiol. 2008, 189, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Henkle, E.; Winthrop, K.L. Nontuberculous mycobacteria infections in immunosuppressed hosts. Clin. Chest. Med. 2015, 36, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, M.P.; Medina, G.; Fernandez, H. Arcobacter butzleri survives within trophozoite of Acanthamoeba castellanii. Rev. Argent. Microbiol. 2016, 48, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Lambrecht, E.; Bare, J.; van Damme, I.; Bert, W.; Sabbe, K.; Houf, K. Behavior of Yersinia enterocolitica in the presence of the bacterivorous Acanthamoeba castellanii. Appl. Environ. Microbiol. 2013, 79, 6407–6413. [Google Scholar] [CrossRef] [PubMed]
- Bleasdale, B.; Lott, P.J.; Jagannathan, A.; Stevens, M.P.; Birtles, R.J.; Wigley, P. The Salmonella pathogenicity island 2-encoded type III secretion system is essential for the survival of Salmonella enterica serovar Typhimurium in free-living amoebae. Appl. Environ. Microbiol. 2009, 75, 1793–1795. [Google Scholar] [CrossRef] [PubMed]
- Carlson, S.A.; Sharma, V.K.; McCuddin, Z.P.; Rasmussen, M.A.; Franklin, S.K. Involvement of a Salmonella genomic island 1 gene in the rumen protozoan-mediated enhancement of invasion for multiple-antibiotic-resistant Salmonella enterica serovar Typhimurium. Infect. Immun. 2007, 75, 792–800. [Google Scholar] [CrossRef] [PubMed]
- Brewer, M.T.; Xiong, N.; Dier, J.D.; Anderson, K.L.; Rasmussen, M.A.; Franklin, S.K.; Carlson, S.A. Comparisons of Salmonella conjugation and virulence gene hyperexpression mediated by rumen protozoa from domestic and exotic ruminants. Vet. Microbiol. 2011, 151, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, M.A.; Carlson, S.A.; Franklin, S.K.; McCuddin, Z.P.; Wu, M.T.; Sharma, V.K. Exposure to rumen protozoa leads to enhancement of pathogenicity of and invasion by multiple-antibiotic-resistant Salmonella enterica bearing SGI1. Infect. Immun. 2005, 73, 4668–4675. [Google Scholar] [CrossRef] [PubMed]
- Colson, P.; Raoult, D. Gene repertoire of amoeba-associated giant viruses. Intervirology 2010, 53, 330–343. [Google Scholar] [CrossRef] [PubMed]
- Raoult, D.; La Scola, B.; Birtles, R. The discovery and characterization of Mimivirus, the largest known virus and putative pneumonia agent. Clin. Infect. Dis. 2007, 45, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Schuster, F.L.; Dunnebacke, T.H. Virus-like particles and an unassociated infectious agent in amoebae of the genus Naegleria. Ann. Soc. Belge Méd. trop. 1974, 54, 359–370. [Google Scholar]
- Suzan-Monti, M.; La Scola, B.; Raoult, D. Genomic and evolutionary aspects of Mimivirus. Virus Res. 2006, 117, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Aherfi, S.; Colson, P.; La Scola, B.; Raoult, D. Giant viruses of amoebas: An update. Front. Microbiol. 2016, 7, 349. [Google Scholar] [CrossRef] [PubMed]
- Colson, P.; Pagnier, I.; Yoosuf, N.; Fournous, G.; La Scola, B.; Raoult, D. “Marseilleviridae”, a new family of giant viruses infecting amoebae. Arch. Virol. 2013, 158, 915–920. [Google Scholar] [CrossRef] [PubMed]
- Colson, P.; de Lamballerie, X.; Fournous, G.; Raoult, D. Reclassification of giant viruses composing a fourth domain of life in the new order Megavirales. Intervirology 2012, 55, 321–332. [Google Scholar] [CrossRef] [PubMed]
- Scheid, P. A strange endocytobiont revealed as largest virus. Curr. Opin. Microbiol. 2016, 31, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Scheid, P. Viruses in close associations with free-living amoebae. Parasitol. Res. 2015, 114, 3959–3967. [Google Scholar] [CrossRef] [PubMed]
- Scheid, P.; Balczun, C.; Schaub, G.A. Some secrets are revealed: Parasitic keratitis amoebae as vectors of the scarcely described pandoraviruses to humans. Parasitol. Res. 2014, 113, 3759–3764. [Google Scholar] [CrossRef] [PubMed]
- Antwerpen, M.H.; Georgi, E.; Zoeller, L.; Woelfel, R.; Stoecker, K.; Scheid, P. Whole-genome sequencing of a Pandoravirus isolated from keratitis-inducing acanthamoeba. Genome Announc. 2015, 3. [Google Scholar] [CrossRef] [PubMed]
- Abergel, C.; Legendre, M.; Claverie, J.-M. The rapidly expanding universe of giant viruses: Mimivirus, Pandoravirus, Pithovirus and Mollivirus. FEMS Microbiol. Rev. 2015, 39, 779–796. [Google Scholar] [CrossRef] [PubMed]
- Sharma, V.; Colson, P.; Chabrol, O.; Pontarotti, P.; Raoult, D. Pithovirus sibericum, a new bona fide member of the “Fourth TRUC” club. Front. Microbiol. 2015, 6, 722. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.C.F.; Almeida, G.M.F.; Oliveira, D.B.; Dornas, F.P.; Campos, R.K.; La Scola, B.; Ferreira, P.C.P.; Kroon, E.G.; Abrahao, J.S. A resourceful giant: APMV is able to interfere with the human type I interferon system. Microbes Infect. 2014, 16, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Colson, P.; La Scola, B.; Raoult, D. Giant viruses of amoebae as potential human pathogens. Intervirology 2013, 56, 376–385. [Google Scholar] [CrossRef] [PubMed]
- Margulis, L.; Schwartz, K.V. Die fünf Reiche der Organismen: Ein Leitfaden; Spektrum d. Wiss: Heidelberg, Germany, 1989. [Google Scholar]
- Desnues, C.; La Scola, B.; Yutin, N.; Fournous, G.; Robert, C.; Azza, S.; Jardot, P.; Monteil, S.; Campocasso, A.; Koonin, E.V.; et al. Provirophages and transpovirons as the diverse mobilome of giant viruses. Proc. Natl. Acad. Sci. USA 2012, 109, 18078–18083. [Google Scholar] [CrossRef] [PubMed]
- Boyer, M.; Azza, S.; Barrassi, L.; Klose, T.; Campocasso, A.; Pagnier, I.; Fournous, G.; Borg, A.; Robert, C.; Zhang, X.; et al. Mimivirus shows dramatic genome reduction after intraamoebal culture. Proc. Natl. Acad. Sci. USA 2011, 108, 10296–10301. [Google Scholar] [CrossRef] [PubMed]
- Maumus, F.; Blanc, G. Study of gene trafficking between Acanthamoeba and giant viruses suggests an undiscovered family of amoeba-infecting viruses. Genome Biol. Evol. 2016, 8, 3351–3363. [Google Scholar] [CrossRef] [PubMed]
- Verneau, J.; Levasseur, A.; Raoult, D.; La Scola, B.; Colson, P. MG-Digger: An automated pipeline to search for giant virus-related sequences in metagenomes. Front. Microbiol. 2016, 7, 428. [Google Scholar] [CrossRef] [PubMed]
- Winiecka-Krusnell, J.; Dellacasa-Lindberg, I.; Dubey, J.P.; Barragan, A. Toxoplasma gondii: Uptake and survival of oocysts in free-living amoebae. Exp. Parasitol. 2009, 121, 124–131. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Smith, L.M.; May, R.C. New weapons in the Cryptococcus infection toolkit. Curr. Opin. Microbiol. 2016, 34, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Steenbergen, J.N.; Nosanchuk, J.D.; Malliaris, S.D.; Casadevall, A. Cryptococcus neoformans virulence is enhanced after growth in the genetically malleable host Dictyostelium discoideum. Infect. Immun. 2003, 71, 4862–4872. [Google Scholar] [CrossRef] [PubMed]
- Mylonakis, E.; Casadevall, A.; Ausubel, F.M. Exploiting amoeboid and non-vertebrate animal model systems to study the virulence of human pathogenic fungi. PLoS Pathog. 2007, 3, e101. [Google Scholar] [CrossRef] [PubMed]
- Cursons, R.T.; Brown, T.J.; Keys, E.A. Effect of disinfectants on pathogenic free-living amoebae: In axenic conditions. Appl. Environ. Microbiol. 1980, 40, 62–66. [Google Scholar] [PubMed]
- Hiti, K.; Walochnik, J.; Haller-Schober, E.M.; Faschinger, C.; Aspock, H. Viability of Acanthamoeba after exposure to a multipurpose disinfecting contact lens solution and two hydrogen peroxide systems. Br. J. Ophthalmol. 2002, 86, 144–146. [Google Scholar] [CrossRef] [PubMed]
| Species | Host Amoeba | References (Selection) |
|---|---|---|
| BACTERIA | ||
| In Situ Interaction | ||
| Legionella-like, Legionella lytica (Sarcobium lyticum) | Acanthamoebae, Naegleriae, Hartmanellae | [47,48,49,50] |
| Legionella pneumophila | Several FLA, e.g., Acanthamoebae | [51,52,53,54,55] |
| Listeria monocytogenes | Acanthamoebae | [56,57] |
| Mycobacterium avium | Acanthamoebae | [41,58] |
| Afipia felis | Acanthamoebae | [59] |
| Pseudomonas saccharophilia | Acanthamoebae | [60] |
| Pseudomonas aeruginosa | Echinamoebae; Acanthamoebae; Hartmannellae | [61,62] |
| Ralstonia (Burkholderia) picketti | Acanthamoebae | [62] |
| Stenotrophomonas maltophilia-Komplex | Acanthamoebae; Naegleriae | [63] |
| Rickettsia-like | Acanthamoebae | [39] |
| Simkania nevegensis (Chlamydia-like) | Acanthamoebae, Naegleriae, Hartmannellae; Balamuthia mandrillaris | [64,65,66] |
| Neochlamydia hartmannellae | Hartmannellae; Hartmannella (Vermamoeba) vermiformis | [67] |
| Candidatus Mesochlamydia elodeae | Vannellae, Saccamoebae | [68] |
| Ehrlichia-like | Saccamoebae | [61] |
| Candidatus Paracaedibacter symbiosus | Acanthamoebae | [69] |
| Procabacter acanthamoebae (Betaproteobacterium) | Acanthamoebae | [70] |
| Amoebophilus asiaticus | Acanthamoebae | [71] |
| In Vitro Interaction | ||
| Salmonella enterica, S. thyphimurium (and other Salmonellae) | Acanthamoebae | [72,73] |
| Yersinia enterocolitica | Acanthamoebae | [74] |
| Campylobacter jejuni | Acanthamoebae (Acanthamoeba polyphaga) | [75] |
| Arcobacter butzleri | Acanthamoebae (Acanthamoeba castellanii) | [76,77,78] |
| Mycobacterium spp., M. leprae | Acanthamoebae | [38,79,80] |
| Staphylococcus aureus (incl.MRSA) | Acanthamoebae | [81] |
| Mobiluncus curtisii | Acanthamoebae | [82] |
| Mycobacterium leprae | Acanthamoebae | [79] |
| Mycobacterium xenopi | Acanthamoebae | [83] |
| Mycobacterium spp; Mycobacterium avium | Acanthamoebae | [38,79,80] |
| Opportunistic Mycobacteria | Acanthamoebae | [41,80] |
| Bacillus anthracis | Acanthamoeba castellanii Hartmannella (Vermamoeba) vermiformis | [84] |
| Acidovorax temperans | Naegleriae | [85] |
| Burkholderia cepacia and Burkholderia pickettii | Acanthamoebae | [86] |
| Caulobacter vibrioides | Echinamoebae | [85] |
| Flavobacterium johnsoniae | Naegleriae | [85] |
| Escherichia coli O157 | Acanthamoebae | [87] |
| Helicobacter pylori | Acanthamoebae | [88] |
| Porphyromonas gingivalis | Acanthamoebae | [89] |
| Prevotella intermedia | Acanthamoebae | [89] |
| Chlamydophila pneumoniae | Acanthamoebae | [90] |
| Parachlamydia acanthamoebae | Acanthamoebae | [91,92,93] |
| Waddlia sp., Waddlia chondrophila, other Chlamydia-like endocytobionts | Acanthamoebae, Naegleriae, Hartmannellae, Hyperamoebae, Vahlkampfiae, Dictyostelium discoideum | [85,94,95] |
| Other Parachlamydia-like endocytobionts | Acanthamoebae | [96,97] |
| Coxiella burnetii | Acanthamoebae | [98] |
| Francisella tularensis | Acanthamoebae | [99,100,101,102] |
| PROTISTS AND FUNGI | ||
| In Situ Interaction | ||
| Paramicrosporidium gen. nov | Vannella sp. | [103] |
| Cochlonema euryblastum | Thecamoebae; Thecamoeba quadrilineata | [104] |
| In Vitro Interaction | ||
| Cryptosporidium parvum | Acanthamoebae | [105,106,107] |
| Cryptococcus neoformans | Acanthamoebae | [42] |
| VIRUSES | ||
| In Situ Interaction | ||
| Adenoviridae | Acanthamoebae | [108] |
| Acanthamoeba polyphaga Mimivirus | Acanthamoebae | [109] |
| Pandoravirus inopinatum | Acanthamoebae | [12,31] |
| Pithovirus | Acanthamoebae | [110] |
| In Vitro Interaction | ||
| Adenoviridae | Acanthamoebae | [111] |
| Coxackie virus | Acanthamoeba | [112] |
| Marseillevirus | Acanthamoebae | [113] |
| Megavirus chilensis | Acanthamoebae | [114] |
| Pandoravirus salinus, Pandoravirus dulcis | Acanthamoebae | [115] |
| Pithovirus sibericum | Acanthamoebae | [116] |
| Faustovirus | Vermamoeba vermiformis | [46] |
| Mollivirus sibericum | Acanthamoebae | [117] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balczun, C.; Scheid, P.L. Free-Living Amoebae as Hosts for and Vectors of Intracellular Microorganisms with Public Health Significance. Viruses 2017, 9, 65. https://doi.org/10.3390/v9040065
Balczun C, Scheid PL. Free-Living Amoebae as Hosts for and Vectors of Intracellular Microorganisms with Public Health Significance. Viruses. 2017; 9(4):65. https://doi.org/10.3390/v9040065
Chicago/Turabian StyleBalczun, Carsten, and Patrick L. Scheid. 2017. "Free-Living Amoebae as Hosts for and Vectors of Intracellular Microorganisms with Public Health Significance" Viruses 9, no. 4: 65. https://doi.org/10.3390/v9040065





