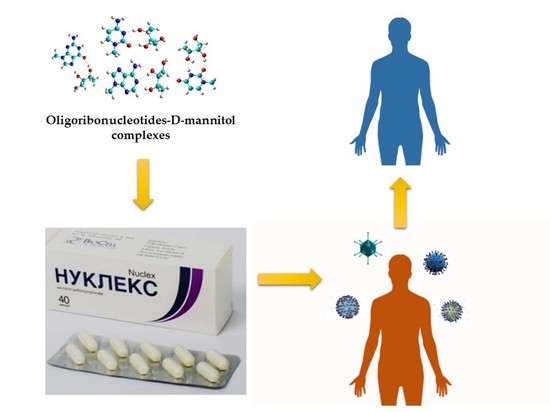
Pre-Clinical and Clinical Efficiency of Complexes of Oligoribonucleotides with D-Mannitol against Respiratory Viruses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. ORNs-D-M Antiviral Activity against PIV-3
2.2.2. ORNs-D-M Antiviral Activity against Pandemic Influenza CA709 and AIV in Vitro
2.2.3. Neuraminidase Activity Assay
2.2.4. Clinical Assay of ORNs-D-M Efficiency
3. Results
3.1. Inhibition of PIV3 Activity by Capsule and Injection Forms of ORNs-D-M In Vitro
3.2. Antiviral Activity of ORNs-D-M against the Pandemic Influenza CA709 and AIV In Vitro
3.3. Antiviral Activity of the Capsule and Injection Forms of ORNs-D-M against the Influenza Virus PR834 In Vitro
3.4. Clinical Efficiency of ORNs-D-M
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Bisno, A.L. Acute pharyngitis. N. Engl. J. Med. 2001, 344, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Scholtissek, C. Molecular evolution of influenza viruses. Virus Genes 1995, 11, 209. [Google Scholar] [CrossRef] [PubMed]
- Verhagen, J.; Sander, H.; Fouchier Ron, A.M. Infectious disease: How a virus travels the world. Science 2015, 347, 616–617. [Google Scholar] [CrossRef] [PubMed]
- Ghedin, E.; Fitch, A.; Boyne, A.; Griesemer, S.; DePasse, J. Mixed infection and the genesis of influenza virus diversity. J. Virol. 2009, 83, 8832–8841. [Google Scholar] [CrossRef] [PubMed]
- Tsalik, E.L.; Henao, R.; Nichols, M. Host gene expression classifiers diagnose acute respiratory illness etiology. Sci. Transl. Med. 2016, 8, 322. [Google Scholar] [CrossRef] [PubMed]
- Talbot, H.K.; Falsey, A.R. The diagnosis of viral respiratory disease in older adults. Clin. Infect. Dis. 2010, 50, 747–751. [Google Scholar] [CrossRef] [PubMed]
- Sloots, T.P.; Whiley, D.M.; Lambert, S.B. Emerging respiratory agents: New viruses for old diseases? J. Clin. Virol. 2008, 42, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Jacques, J.; Moret, H.; Minette, D. Epidemiological, molecular, and clinical features of enterovirus respiratory infections in French children between 1999 and 2005. J. Clin. Microbiol. 2008, 46, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Weiss, S.R.; Navas-Martin, S. Coronavirus pathogenesis and the emerging pathogen severe acute respiratory syndrome coronavirus. Microbiol. Mol. Biol. 2005, 69, 635–664. [Google Scholar] [CrossRef] [PubMed]
- Kahn, J.S. Newly discovered respiratory viruses: Significance and implications. Curr. Opin. Pharmacol. 2007, 7, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Esper, F.P.; Spahlinger, T.; Zhou, L. Rate and influence of respiratory virus co-infection on pandemic (H1N1) influenza disease. J. Infect. 2011, 63, 260–266. [Google Scholar] [CrossRef] [PubMed]
- Cilla, G.; Onate, E.; Perez-Yarza, E.G. Viruses in community acquired pneumonia in children aged less than 3 years old: High rate of viral coinfection. J. Med. Virol. 2008, 80, 1843–1849. [Google Scholar] [CrossRef] [PubMed]
- Martin, E.T.; Kuypers, J.; Wald, A. Multiple versus single virus respiratory infections: Viral load and clinical disease severity in hospitalized children. Influenza Other Respir. Viruses 2012, 6, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Drews, A.L.; Atmar, R.L.; Glezen, W.P. Dual respiratory virus infections. Clin. Infect. Dis. 1997, 25, 1421–1429. [Google Scholar] [CrossRef] [PubMed]
- Portnoy, B.E.; Eckert, H.L.; Hanes, B. Multiple respiratory virus infections in hospitalised children. Am. J. Epidemiol. 1965, 82, 262–272. [Google Scholar] [CrossRef] [PubMed]
- Semple, M.G.; Cowell, A.; Dove, W. Dual infection of infants by human metapneumovirus and human respiratory syncytial virus is strongly associated with severe bronchiolitis. J. Infect. Dis. 2005, 191, 382–386. [Google Scholar] [CrossRef] [PubMed]
- Cunha, B.A.; Corbett, M.; Mickail, N. Human parainfluenza virus type 3 (HPIV 3) viral community-acquired pneumonia (CAP) mimicking swine influenza (H1N1) during the swine flu pandemic. Heart Lung 2011, 40, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Nichols, W.G.; Corey, L.; Gooley, T. Parainfluenza virus infections after hematopoietic stem cell transplantation: Risk factors, response to antiviral therapy, and effect on transplant outcome. Blood 2001, 98, 573–578. [Google Scholar] [CrossRef] [PubMed]
- Abed, Y.; Boivin, G. Treatment of respiratory virus infections. Antivir. Res. 2006, 70, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Davlin, S.L. Influenza activity—United States, 2015–2016 season and composition of the 2016–2017 influenza vaccine. Morb. Mortal. Wkly. Rep. 2016, 65, 567–575. [Google Scholar] [CrossRef] [PubMed]
- Houser, K.; Subbarao, K. Influenza vaccines: Challenges and solutions. Cell Host Microbe. 2015, 17, 295–300. [Google Scholar] [CrossRef] [PubMed]
- El-Sahly, H. Spectrum of clinical illness in hospitalized patients with “common cold” virus infections. Clin. Infect. Dis. 2000, 31, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Kamimoto, L.; Bramley, A.M. Hospitalized Patients with H1N1 Influenza in the United States, April–June 2009. N. Engl. J. Med. 2009, 361, 1935–1944. [Google Scholar] [CrossRef] [PubMed]
- Bright, R.A.; Shay, D.K.; Shu, B. Adamantane resistance among influenza A viruses isolated early during the 2005–2006 influenza season in the United States. JAMA 2006, 295, 891–894. [Google Scholar] [CrossRef] [PubMed]
- Moscona, A. Global transmission of oseltamivir-resistant influenza. N. Engl. J. Med. 2009, 360, 953–956. [Google Scholar] [CrossRef] [PubMed]
- Sheu, T.G. Dual resistance to adamantanes and oseltamivir among seasonal influenza A (H1N1) viruses: 2008–2010. J. Infect. Dis. 2011, 203, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Matthew, P.; Hall, R.J.; Sonnberg, S. Pandemic (H1N1) 2009 and Seasonal Influenza A (H1N1) Co-infection, New Zealand, 2009. Emerg. Infect. Dis. 2010, 16, 1618–1620. [Google Scholar] [CrossRef]
- Chertow, D.S.; Memoli, M.J. Bacterial coinfection in Influenza A. JAMA 2013, 309, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Tkachuk, Z. Multiantivirus Compound, Composition and Method for Treatment of Virus Diseases. U.S. Patent 20,120,232,129, 16 April 2013. [Google Scholar]
- Tkachuk, Z.Y.; Rybalko, S.L.; Zharkova, L.D. Antiinfluenzal activity of drug Nuclex. Rep. Natl. Acad. Sci. Ukr. 2010, 9, 191–196. [Google Scholar]
- Melnichuk, N.; Semernikova, L.; Tkachuk, Z. Complexes of Oligoribonucleotides with d-Mannitol Inhibit Hemagglutinin–Glycan Interaction and Suppress Influenza A Virus H1N1 (A/FM/1/47) Infectivity In Vitro. Pharmaceuticals 2017, 10, 71. [Google Scholar] [CrossRef] [PubMed]
- Tkachuk, Z. Antiherpetic drug Nuclex effect. Rep. Natl. Acad. Sci. Ukr. 2011, 4, 182–188. [Google Scholar]
- Tkachuk, Z.Y.; Frolov, V.M.; Sotska, Y.A.; Kruglova, O.V. Nuclex therapy for patients with chronic hepatitis C. Int. J. Immunol. Stud. 2012, 1, 349–364. [Google Scholar] [CrossRef]
- Zelyoniy, I.I.; Tkachuk, Z.Y.; Afonin, D.N.; Tiutiunnyk, A.A. Influence of Preparation Nucleх on the Cytokine Profile of the Patients with Diabetes Type 2 and Neuropathic Form of Diabetic Foot. J. Diabetes Res. 2013, 2, 21–26. [Google Scholar] [CrossRef]
- Reed, L.J.; Muench, H. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 1938, 27, 493–497. [Google Scholar] [CrossRef]
- Potier, M.; Belislem, M.; Dallaire, L.; Melanxson, S.B. Fluorometric assay of neurominidase with a sodium (4-methylumbelliferyl-a-d-N ctylneuraminate) substrate. Anal. Biochem. 1979, 94, 287–296. [Google Scholar] [CrossRef]
- Bonzel, L.; Tenenbaum, T.; Schroten, H. Frequent detection of viral coinfection in children hospitalized with acute respiratory tract infection using a real-time polymerase chain reaction. Ped. Infect. Dis. J. 2008, 27, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Beigel, J.; Bray, M. Current and future antiviral therapy of severe seasonal and avian influenza. Antivir. Res. 2008, 78, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Nayak, D.P.; Hui, E.K.; Barman, S. Assembly and budding of influenza virus. Virus Res. 2004, 106, 147–165. [Google Scholar] [CrossRef] [PubMed]
- Melnichuk, N.; Tkachuk, Z. Influence of the oligoribonucleotides-d-mannitol complexes on upexpression of some genes induced by influenza virus in vivo. In Proceedings of the 3rd International Electronic Conference on Medicinal Chemistry MDPI AG, 1–30 November 2017; Volume 3. Available online: http://www.sciforum.net/conference/ecmc-3 (assessed on 19 May 2018). [CrossRef]



| Syndromes | Main Group | Control Group | ||
|---|---|---|---|---|
| Severity of Disease | ||||
| Moderate, n = 26 | Severe, n = 28 | Moderate, n = 33 | Severe, n = 21 | |
| Fever | 1.9 ± 0.1 | 2.9 ± 0.2 *** | 2.4 ± 0.2 * | 3.4 ± 0.2 **,*** |
| Intoxication | 1.8 ± 0.2 | 2.6 ± 0.2 *** | 2.6 ± 0.2 * | 3.9 ± 0.5 **,*** |
| Catarrhal | 2.9 ± 0.3 | 4.4 ± 0.5 *** | 4.4 ± 0.3 * | 8.6 ± 0.9 **,*** |
| Duration of hospitalization | 7.8 ± 0.3 | 9.4 ± 1.8 *** | 9.9 ± 0.6 * | 14.7 ± 1.9 **,*** |
| Syndromes | Main Group | Control Group | ||
|---|---|---|---|---|
| ARI, n = 44 | ARI and Pneumonia, n = 10 | ARI, n = 39 | ARI and Pneumonia, n = 15 | |
| Fever | 1.9 ± 0.2 | 2.8 ± 0.5 * | 2.3 ± 0.2 ** | 4.2 ± 0.3 *,** |
| Intoxication | 1.9 ± 0.1 | 3.0 ± 0.3 * | 2.6 ± 0.2 ** | 4.3 ± 0.6 *,** |
| Catarrhal | 3.6 ± 0.3 | 5.1 ± 0.4 * | 4.1 ± 0.3 ** | 7.5 ± 0.8 *,** |
| Duration of hospital stay | 8.1 ± 0.4 | 12.9 ± 0.9 * | 10.3 ± 0.6 ** | 17.2 ± 1.8 *,** |
| Viruses | Main Group | Control Group | ||
|---|---|---|---|---|
| (n = 40) | (n = 38) | |||
| Before Treatment | After Treatment | Before Treatment | After Treatment | |
| Influenza A virus | 16 | 0 | 9 | 6 |
| PIV | 8 | 2 | 13 | 4 |
| AdV | 5 | 0 | 5 | 2 |
| RSV | 14 | 1 | 13 | 9 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Melnichuk, N.; Zarubaev, V.; Iosyk, I.; Andreychyn, M.; Semernikova, L.; Tkachuk, Z. Pre-Clinical and Clinical Efficiency of Complexes of Oligoribonucleotides with D-Mannitol against Respiratory Viruses. Pharmaceutics 2018, 10, 59. https://doi.org/10.3390/pharmaceutics10020059
Melnichuk N, Zarubaev V, Iosyk I, Andreychyn M, Semernikova L, Tkachuk Z. Pre-Clinical and Clinical Efficiency of Complexes of Oligoribonucleotides with D-Mannitol against Respiratory Viruses. Pharmaceutics. 2018; 10(2):59. https://doi.org/10.3390/pharmaceutics10020059
Chicago/Turabian StyleMelnichuk, Nataliia, Vladimir Zarubaev, Iaryna Iosyk, Mychaylo Andreychyn, Larisa Semernikova, and Zenoviy Tkachuk. 2018. "Pre-Clinical and Clinical Efficiency of Complexes of Oligoribonucleotides with D-Mannitol against Respiratory Viruses" Pharmaceutics 10, no. 2: 59. https://doi.org/10.3390/pharmaceutics10020059