1. Introduction
In December 2015, the United Nations officially established global Sustainable Development Goals (SDGs), putting health in a central position due to its inalienable contributions to both individuals and societies [
1]. Globally, the world is facing unprecedented health challenges, such as profound epidemiological and population changes, chronic diseases, mental illness, and injuries—all of which threaten the attainment of the health-related SDGs. There is no doubt that confronting these challenges is critically dependent on governmental and social support. However, health intervention measures cannot be implemented without the proper deployment of the health workforce [
2].
As the most important component of health resources (human, physical, and financial), the health workforce is essential for the operation of a country’s health systems [
3]. The availability of a health workforce shapes the conditions and prospects of population health substantially, and plays an important role in sustainable human development. It has been established that health workforce density (i.e., the ratio of the health workforce population to the overall population, expressed as the number of health workers per 1000 people [
4]) is significantly associated with health outcomes in certain areas. For instance, Anand and Bärnighausen [
5] found that health workforce density was significantly associated with the mortality rate of infants and children aged under 5, as well as maternal mortality rates. The World Health Organization (WHO) [
6] concluded there was a statistically significant relationship between the density and availability of trained birth attendants and measles immunization. Wider and denser coverage of the health workforce will most likely bring positive health outcomes by improving overall capacity for disease detection and response, and therefore contribute towards achieving the SDGs [
1]. However, the studies on the determinants of a health workforce in one area remain insufficient.
A range of studies have discussed the determinants of health workforce density. Generally speaking, this is usually discussed from two perspectives: between countries and within countries. On the one hand, there are widespread health workforce density differences between countries [
7]. Dussault and Vujicic [
8] stated that it is a complex issue, as “history, culture, politics, social structures, and the economy” all have an effect. Dussault and Franceschini [
9] place the “determinants of geographical imbalances” in health workforce distribution into five categories: “individual; organizational; health care and educational systems; institutional structures; and the broader sociocultural environment”. At the empirical level, Kanchanachitra et al. [
10] showed a significant relationship between health workforce density and gross national income (GNI) across ten countries in the Association of Southeast Asian Nations (ASEAN). Freed et al. [
11] showed a linear relationship between the number of practicing physicians and pediatricians in the US and US gross domestic product (GDP; inflation-adjusted), for all years recorded. Zaman et al. [
12] performed a cross-country analysis with 183 United Nation member countries and grouped the indicators for health workforce density into three categories: demographic, economic, and political factors.
On the other hand, health workers are not equally distributed within countries, with the health workforce shortage being much more severe in remote areas [
13]. Numerous researchers have studied health workforce misdistribution within countries from a human resource management (HRM) perspective. For example, the relationship between job satisfaction, burnout, motivation, and health worker turnover explains—to some extent—the outflow and shortage of health workers in some areas [
14,
15,
16]. However, until now, there has not been a widely recognized theoretical framework to systematically classify the factors that influence health workforce distribution within countries, from the macro perspective. At the empirical level, only Scholz et al. [
17] has explored the effects of demand/need factors (population morbidity/financial incentives) on health workforce distribution in Germany.
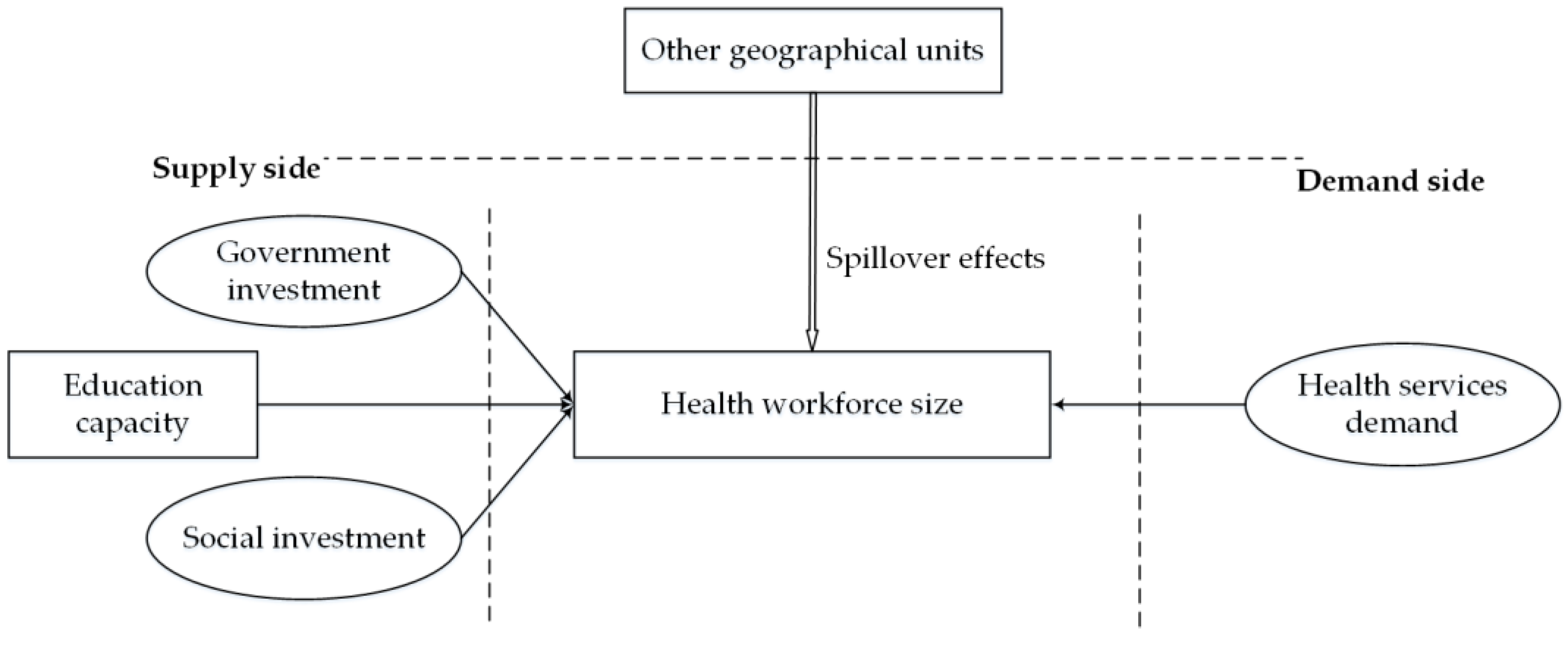
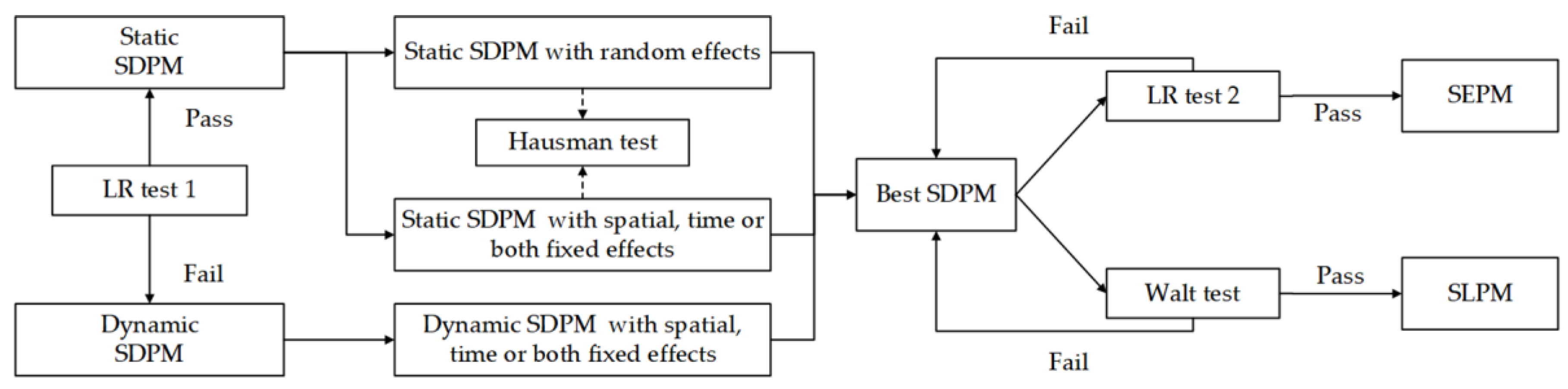
To conclude, the determinants of the health workforce distribution within countries have not been systematically measured, due to the lack of a widely acknowledged theoretical framework. To fill the research gap, this study aimed to theoretically model and empirically measure the dynamics and spillovers of the health labor market within countries, thus helping us understand the health workforce distribution within countries. First, a theoretical model that considered the intra-regional supply-side factors, demand-side factors, and also the inter-regional spillover effects was built in
Section 2 to model the dynamics and spillovers of the health labor market. Additionally, spatial econometric models are introduced in
Section 3 to empirically measure the effects of both the inter-regional determinants and spillovers based on China’s provincial panel data set. This study provides some theoretical references to other more in-depth studies and also further implications for health workforce policies in China. The introduction and literature review are provided in the first section, and the second section focuses on the theoretical model construction and its measurement. The third section describes the data, statistical models, and model specification. The empirical results are displayed in
Section 4,
Section 5 discusses, and
Section 6 concludes.
5. Discussion
The distribution of the health workforce is a topic that has been intensively researched in the health field, and is relevant to the measurement of health equity—an important aspect of social fairness [
48]. This study built a “supply–demand–spillover” theoretical model (
Figure 2) to map the dynamics and spillovers in the health labor market, and employed spatial panel data models to empirically measure the effects of intra-regional supply-side and demand-side factors, as well as inter-regional spillover effects. The findings provide a deeper and more comprehensive understanding of the dynamics of the health labor market, as well as evidence-based health workforce allocation policies in China.
Theoretically, the contribution of this study is twofold. First, supply and demand theory in labor economics is fundamental to modeling the dynamics of the health labor market, and thus helps shape our understanding of the health workforce distribution. This study refined supply-side factors (education capacity, government investment, and social investment) and demand-side factors (health services demand) based on China’s reality; however, this theoretical model cannot explain the health workforce distribution of countries, due to the nuances and variances of health systems. Still, we believe that it provides a systematic perspective to examine the dynamics of the health labor market. Second, this study introduced spillovers into the theoretical model to help better understand the health labor market. To our knowledge, this study represents one of the first attempts to take inter-regional connections into consideration, and thus remedy the supply and demand theory deficits when applied to the health labor markets within countries. As mentioned in
Section 2, the dynamics of the health labor market is closely related with the equity in health workforce distribution and also the health workforce planning. The existence of spillover effects in the health labor market indicates that the health labor submarkets in different provincial units are not independent of each other, which should be an important consideration to balance the health workforce distribution and local health workforce planning.
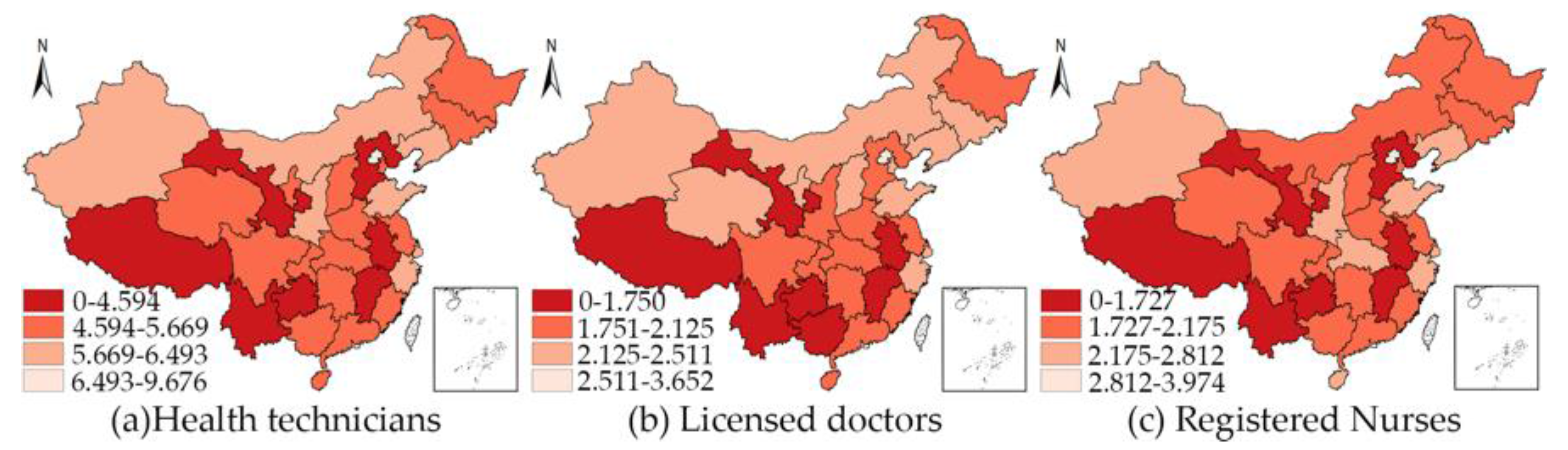
Empirically, the results indicated that the spillover effects of the health labor market do exist, which echoed the rationality of the theoretical model. While there exist great differences among the coefficients and significance levels of the IVs for the three different DVs, this reveals that the dynamics and spillover of the health labor market for HTs, LDs, and RNs are slightly different. We would also like to discuss the results and policy implications in accordance with the theoretical model.
From the demand side, health services demand plays an important role in health labor submarkets. First, even though demand does not solely drive health workforce size, the results confirmed the significant direct effects of health services demand on HTD, LDD, and RND, indicating that health services demand matters in the health labor market. In addition, the results indicate that the spillover effects of OVPA were significant in driving the HTD and RND. The uneven health services demand—as indicated in the results—is likely to induce brain drain of health workforce by siphoning the health talents from surrounding regions. More specifically, if there are high health services demands in one unit, it not only reveals higher health workforce density in local units, but also a likelihood of attracting the health workforce from adjacent units. Second, the results indicated that the different types of health services utilization play different roles in the health labor market. For all of the HTs and LDs, outpatient visits and inpatient visits play almost identical role in driving their densities. Regarding the RNs, the increase of inpatient visits provides more motivation to recruit RNs than outpatient visits, which can be attributed to the different roles of LDs and RNs in health service delivery, as the nurses spend most of their time in providing the inpatient services. The above-mentioned two points imply that we should proactively allocate health workforce via different kinds of health services demand. At first glance, the health services demand is objective and has nothing to do with the government. In effect, the government can also play a role in the demand side, as the medical needs of the general public are not necessarily reflected in the needs for health services proportionately. Therefore, a population’s health services demand can also be stimulated or guided through related health policies—for example, health insurance and medical aid. If we want to increase the health workforce density in one unit by appropriately guiding the health services demand of the public, the coverage of medical insurance and medical aids should be expanded to fulfill the potential medical needs (especially those repressed by economic conditions), and also prevent the potential brain drain.
From the supply side, a two-stage supply chain should be taken into consideration. First, even though the supporting role of education capacity for the intra-regional health industry is not prominent for each type of health workforce, its spillover effects are positive and significant for both HTD and RND. Therefore, it is a feasible strategy to increase the medical education capacity in remote provincial units to enhance the supply of a health workforce. However, admittedly, the supply of qualified medical students is not solely determined by the education capacity of medical institutions [
8]. For one thing, as a qualified medical graduate, one needs to master the matching skills and enter the health labor market at the right time; and for another, one has a relatively long education time. Both of these conditions require the education sector to plan ahead. Second, this study failed to confirm the significant direct effects of health expenditure on health workforce density. However, the spillover effects of government and social health expenditure was both positive and significant for HTD, indicating that those remote provincial units should work together and make good use of the “visible hand” and “invisible hand”.
To conclude, supply-side factors, demand-side factors, and spillovers constitute the dynamics of the health labor market. We can easily draw lessons for health workforce policy-making in China; however, the health labor market is ultimately a complex issue. The supply-and-demand perspective aids our understanding of the health labor market. First, the health labor market is not static over time. It requires constant supply adjustments and changing guidance for supply and demand. Second, the health labor market is not monolithic across space. Although scarcity in the health workforce might be detected in one region, a nuanced picture might be drawn when zooming into smaller scales. For example, when divided into smaller patches of the submarket (e.g., urban–rural, public–private, health institution level, skill mix) [
23], it is possible that health labor is sufficient in some submarkets and greatly in need in others. Third, the supply and demand sides are not mutually independent. For instance, with proper management and intervention, the health workforce allocated to disease control and prevention will reduce medical needs significantly.
This study also bears some limitations. This study only focused on the total quantity—rather than the quality—of the health workforce. It is important to note that effective health service delivery depends not only on health workforce quantity, but also on quality and skill mix [
32]. Rural and remote areas experiencing a health workforce shortage usually lack a high-quality health workforce. Remote areas are confronted with three-fold health workforce challenges at the same time: the supply capacity in these areas is inadequate, they face low workforce quality, and there are draining effects from the surrounding regions. In addition, due to the lack of data in some provincial units before 2012, this study was conducted based on a three-year short panel data set, which limits the model selection. In the future, more detailed studies are suggested to zoom into smaller scales and focus on panel data spanning a longer time.