Temperature and Cardiovascular Mortality Associations in Four Southern Chinese Cities: A Time-Series Study Using a Distributed Lag Non-Linear Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Data Collection
2.3. Data Analysis
2.4. Sensitivity Analyses
3. Results
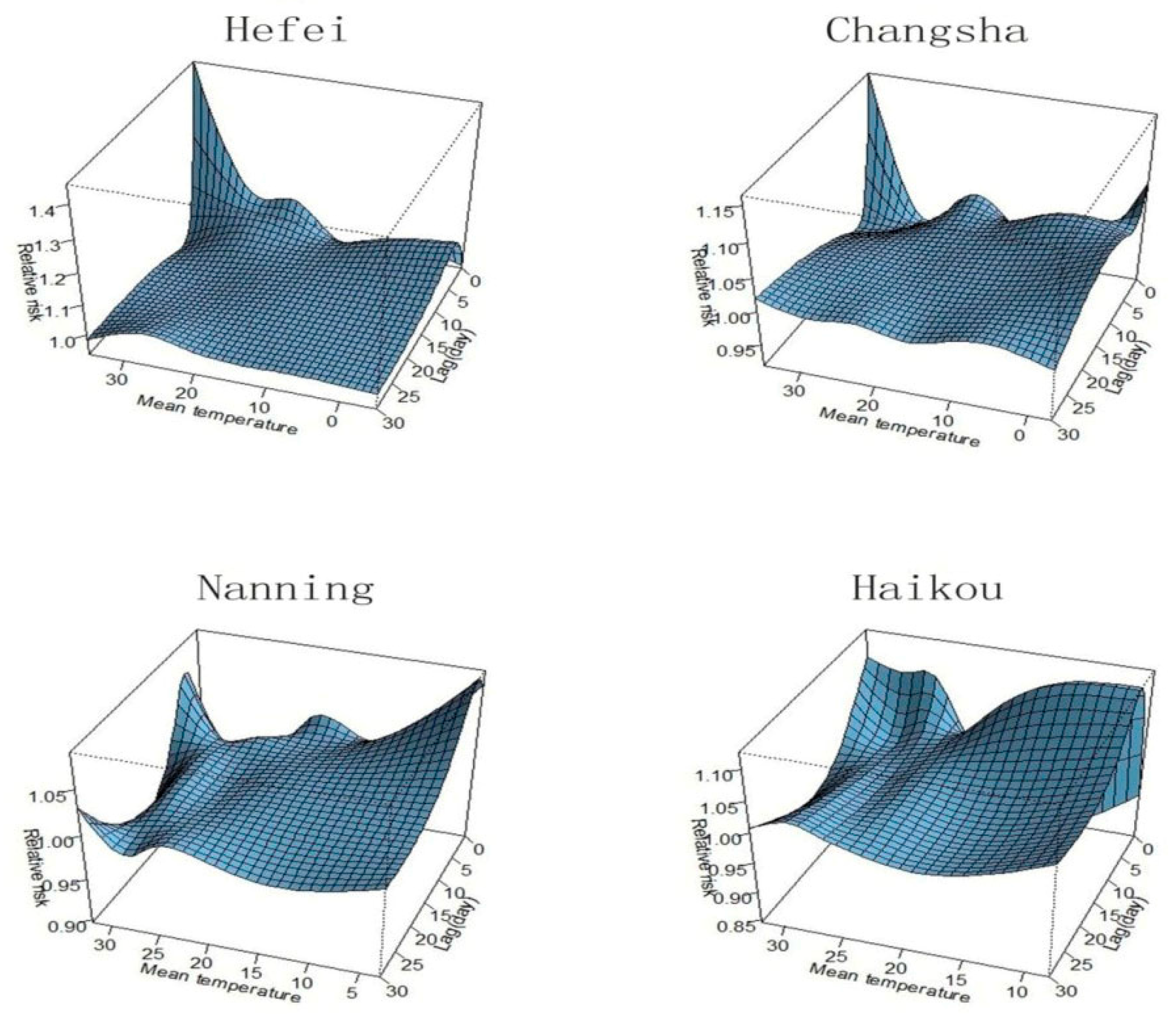
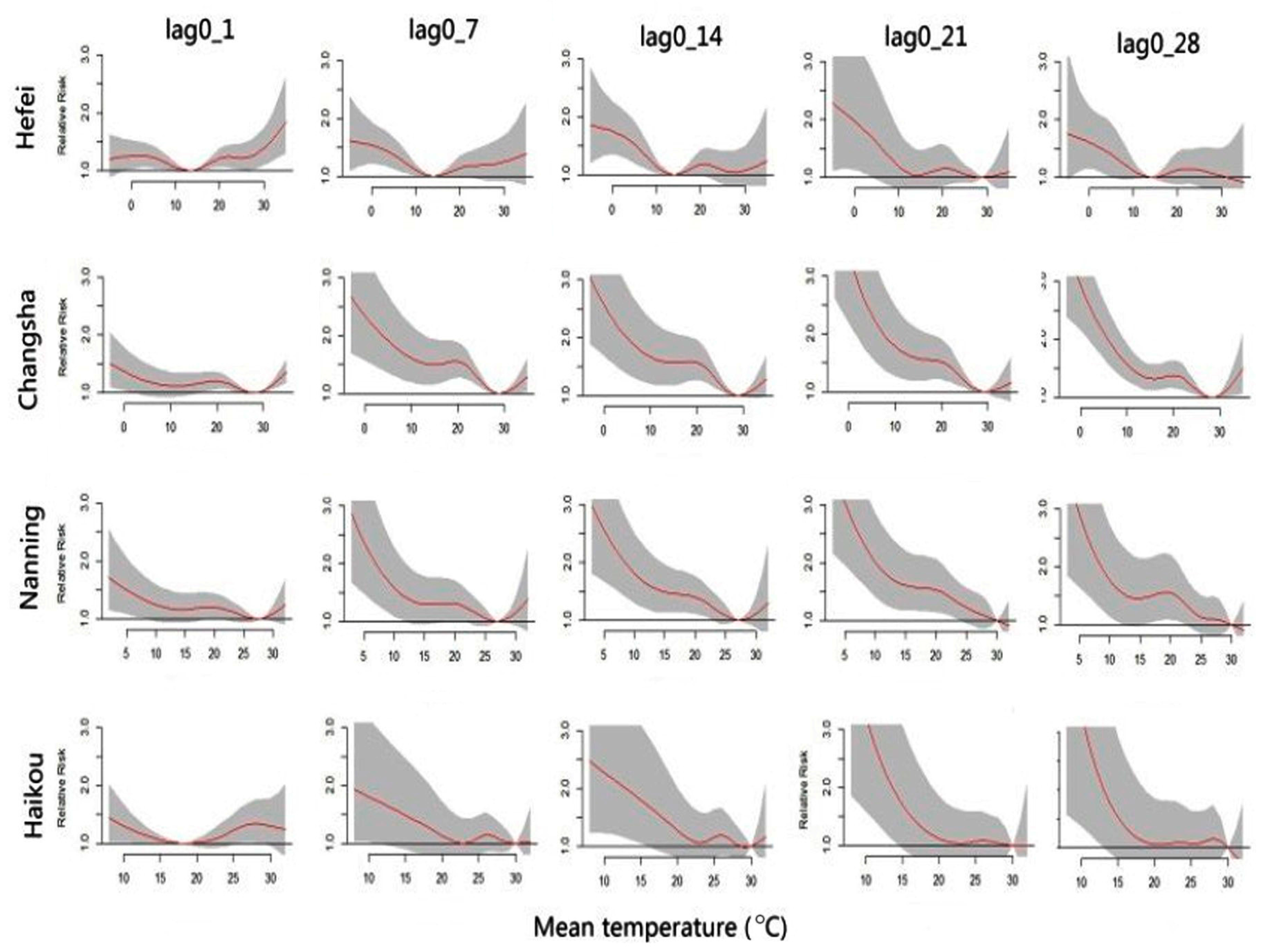
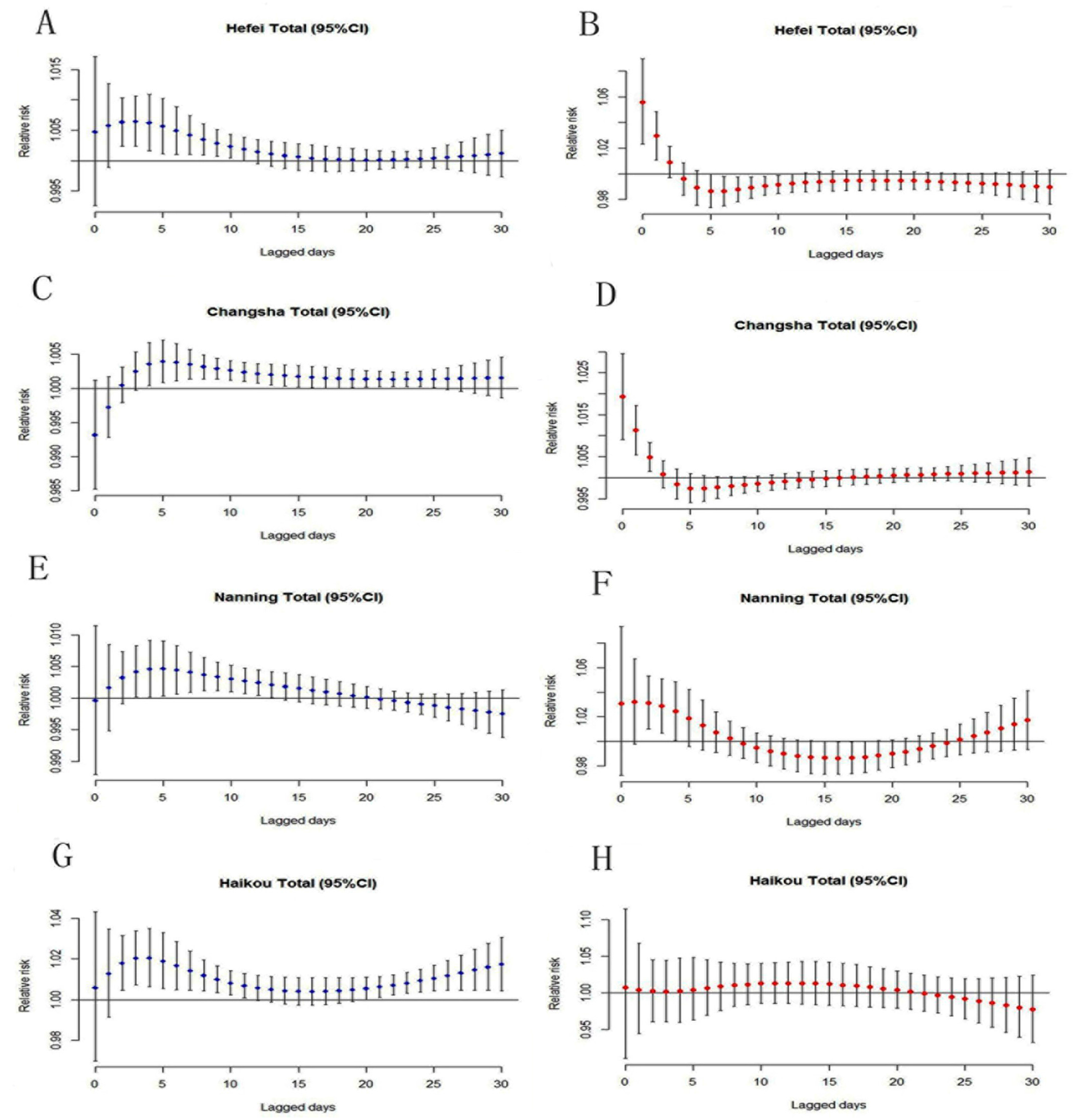
3.1. Temperature Thresholds and Lag Periods
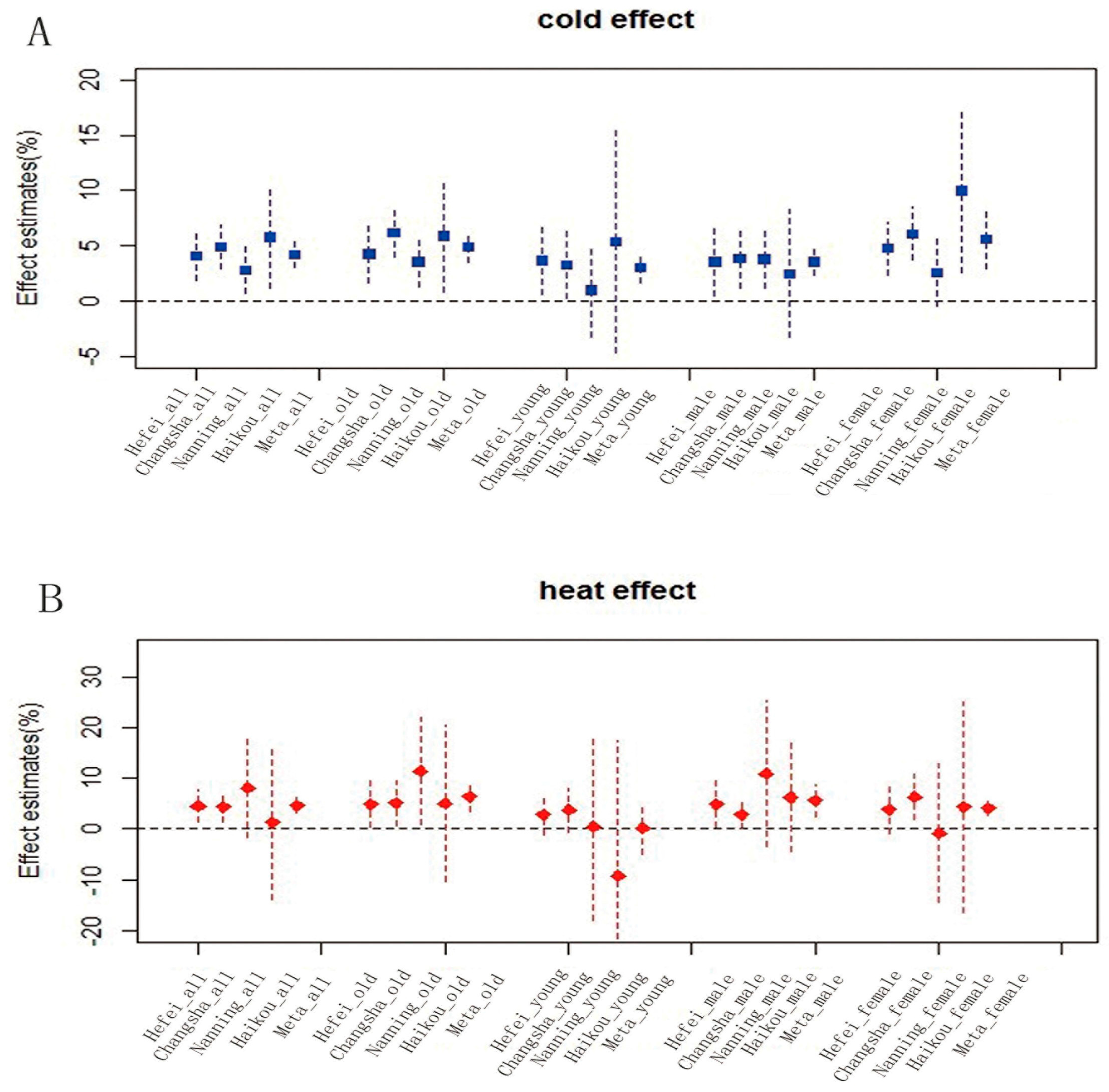
3.2. Temperature-Related CVD Mortality Effects
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Medina-Ramon, M.; Schwartz, J. Temperature, temperature extremes, and mortality: A study of acclimatization and effect modification in 50 US cities. Occup. Environ. Med. 2007, 64, 827–833. [Google Scholar] [CrossRef] [PubMed]
- Alexander, L.V.; Zhang, X.; Peterson, T.C.; Caesar, J.; Gleason, B.; Klein Tank, A.M.G.; Haylock, M.; Collins, D.; Trewin, B.; Rahimzadeh, F.; et al. Global observed changes in daily climate extremes of temperature and precipitation. J. Geophys. Res. Atmos. 2006, 111. [Google Scholar] [CrossRef]
- Peterson, T.C.; Zhang, X.; Brunet-India, M.; Vazquez-Aguirre, J.L. Changes in North American extremes derived from daily weather data. J. Geophys. Res. Atmos. 2008, 113. [Google Scholar] [CrossRef]
- Trenberth, K.E.; Jones, P.D.; Ambenje, P. Observations: Surface and atmospheric climate change. In Climate Change 2007: The Physical Science Basis; Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change; Solomon, S., Qin, D., Manning, M., Chen, Z., Marquis, M., Averyt, K.B., Tignorand, M., Miller, H.L., Eds.; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2007; pp. 235–336. [Google Scholar]
- Intergovernmental Panel on Climate Change. Climate Change. The Physical Science Basis; Working Group I Contribution to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2013. [Google Scholar]
- Anderson, B.G.; Bell, M.L. Weather-related mortality: How heat, cold, and heat waves affect mortality in the United States. Epidemiology 2009, 20, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.Y.; Honda, Y.; Hong, Y.C.; Pan, X.C.; Guo, Y.L.; Kim, H. Ambient temperature and mortality: An international study in four capital cities of East Asia. Sci. Total Environ. 2009, 408, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Douglas, A.S.; Dunnigan, M.G.; Allan, T.M.; Rawles, J.M. Seasonal variation in coronary heart disease in Scotland. J. Epidemiol. Community Health 1995, 49, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Lawlor, D.A.; Smith, G.D.; Mitchell, R.; Ebrahim, S. Temperature at birth, coronary heart disease, and insulin resistance: Cross sectional analysis of the brithsh women’s heart and health study. Heart 2004, 90, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Zhang, J.; Lu, C. Review of researches on relationship of meteorological factors and cardiovascular diseases in China. Meteorol. Sci. Technol. 2004, 32, 425–428. (In Chinese) [Google Scholar]
- Basu, R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ. Health 2009, 8, 40. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Guo, Y.; Hashizume, M.; Lavigne, E.; Zanobetti, A.; Schwartz, J.; Tobias, A.; Tong, S.; Rocklöv, J.; Forsber, B.; et al. Mortality risk attributable to high and low ambient temperature: A multi country observational study. Lancet 2015, 386, 369–375. [Google Scholar] [CrossRef]
- Amegah, A.K.; Rezza, G.; Jaakkola, J.J. Temperature-related morbidity and mortality in Sub-Saharan Africa: A systematic review of the empirical evidence. Environ. Int. 2016, 91, 133–149. [Google Scholar] [CrossRef] [PubMed]
- Spencer, F.A.; Goldberg, R.J.; Becker, R.C.; Gore, J.M. Seasonal distribution of acute myocardial infarction in the second national registry of myocardial infarction. J. Am. Coll. Cardiol. 1998, 31, 1226–1233. [Google Scholar] [CrossRef]
- Pan, W.H.; Li, L.A.; Tsai, M.J. Temperature extremes and mortality from coronary heart disease and cerebral infarction in elderly Chinese. Lancet 1995, 345, 353–355. [Google Scholar] [CrossRef]
- Filleul, L.; Cassadou, S.; Medina, S.; Fabres, P.; Lefranc, A.; Eilstein, D.; Le Tertre, A.; Pascal, L.; Chardon, B.; Blanchard, M.; et al. The relation between temperature, ozone, and mortality in nine French cities during the heat waves of 2003. Environ. Health Perspect. 2006, 114, 1344–1347. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.M.; Barnett, A.G.; Pan, X.C.; Yu, W.W.; Tong, S.L. The impact of temperature on mortality in Tianjin, China: A case-crossover design with a distributed lag nonlinear model. Environ. Health Perspect. 2011, 119, 1719–1725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tian, Z.X.; Li, S.S.; Zhang, J.L.; Jaakkola, J.; Guo, Y.M. Ambient temperature and coronary heart disease mortality in Beijing, China: A time series study. Environ. Health 2012, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.X.; Wang, J.F.; Yu, W.W. The lag Effects and Vulnerabilities of Temperature Effects on Cardiovascular Disease Mortality in a Subtropical Climate Zone in China. Int. J. Environ. Res. Public Health 2014, 11, 3982–3994. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Wang, L.; Lin, H.; Zhang, Y.; Rutherford, S.; Luo, Y.; Zeng, W.; Zhang, Y.; Wang, X.; et al. The temperature-mortality relationship in China: An analysis from 66 Chinese communities. Environ. Res. 2015, 137, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Ou, C.Q.; Ding, Y.; Zhou, Y.X.; Chen, P.Y. Daily temperature and mortality: A study of distributed lag non-linear effect and effect modification in Guangzhou. Environ. Health 2012, 11, 63. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, T.T.; Tan, J.G.; Huang, C.R.; Kan, H.D. Impact of temperature on mortality in three major Chinese cities. Biomed. Environ. Sci. 2014, 27, 485–494. [Google Scholar] [PubMed]
- Zeng, W.L.; Li, G.C.; Xiao, Y.Z.; Xu, Y.J.; Xu, X.J.; Liu, T.; Luo, Y.; Xiao, J.P.; Ma, W.J. The impact of temperature on cardiovascular disease deaths in 4 cities, China: A time-series study. Chin. J. Epidemiol. 2012, 33, 1021–1025. (In Chinese) [Google Scholar]
- Lin, Y.K.; Ho, T.J.; Wang, Y.C. Mortality risk associated with temperature and prolonged temperature extremes in elderly populations in Taiwan. Environ. Res. 2011, 111, 1156–1163. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.W.; Hu, W.B.; Mengersen, K.; Guo, Y.; Pan, X.; Connel, D.; Tong, S. Time course of temperature effects on cardiovascular mortality in Brisbane, Australia. Heart 2011, 97, 1089–1093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bayentin, L.; EI Adlouni, S.; Quarda, T.B.; Gosselin, P.; Doyon, B.; Chebana, F. Spatial variability of climate effects on ischemic heart disease hospitalization rates for the period 1989–2006 in Quebec, Canada. Int. J. Health Geogr. 2010, 9, 5. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Xiao, Y.; Li, G.; Zeng, W.; Lin, H.; Rutherford, S.; Xu, Y.; Luo, Y.; Xu, X.; Chu, C.; et al. Temperature-mortality relationship in four subtropical Chinsese cities: A time-series study using a distributed lag non-linear model. Sci. Total Environ. 2013, 449, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Healy, J.D. Excess winter mortality in Europe: A cross county analysis identifying key risk factors. J. Epidemiol. Community Health 2003, 57, 784–789. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J. The distributed lag between air pollution and daily deaths. Epidemiology 2000, 11, 320–326. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, J. Who is sensitive to extremes of temperature?: A case-only analysis. Epidemiology 2005, 16, 67–72. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, M.S.; Zanobetti, A.; Schwartz, J. Modifiers of the temperature and mortality association in seven US cities. Am. J. Epidemiol. 2003, 157, 1074–1082. [Google Scholar] [CrossRef] [PubMed]
- National Bureau of Statistics of China. China Statistic Year Book 2010; China Statistics Press: Beijing, China, 2010.
- Maynard, R.L.; Coster, S.M. Informing the Public about Air Pollution. In Air Pollution and Health; Academic Press: London, UK, 1999. [Google Scholar]
- Hu, M.; Jia, L.; Wang, J.; Pan, Y. Spatial and temporal characteristics of particulate matter in Beijing, China using the Empirical Mode Decomposition method. Sci. Total Environ. 2013, 458–460, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; McDermott, A.; Hastie, T.J. Improved semiparametric time series models of air pollution and mortality. J. Am. Stat. Assoc. 2004, 99, 938–949. [Google Scholar] [CrossRef]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [PubMed]
- Akaike, H. Information theory and an extension of the maximum likelihood principle. In Second International Symposium on Information Theory; Petrov, B.N., Caski, F., Eds.; AkademiaiKiado: Budapest, Hungary, 1973; pp. 267–281. [Google Scholar]
- Analitis, A.; Katsouyanni, K.; Biggeri, A.; Baccini, M. Effects of cold weather on mortality: Results from 15 European cities within the PHEWE project. Am. J. Epidemiol. 2008, 168, 1397–1408. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Vaneckova, P.; Mengersen, K.; Pan, X.; Tong, S. Is the association between temperature and mortality modified by age, gender and socio-economic status? Sci. Total Environ. 2010, 408, 3513–3518. [Google Scholar] [CrossRef] [PubMed]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Berkey, C.S.; Hoaglin, D.C.; Mosteller, F.; Colditz, G.A. A random-effects regression model for meta-analysis. Stat. Med. 1995, 14, 395–411. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Yavar, Z.; Sun, Q. Cardiovascular response to thermoregulatory challenges. Am. J. Physiol. Heart Circ. Physiol. 2015, 309, 1793–1812. [Google Scholar] [CrossRef] [PubMed]
- Eurowinter Group. Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease and all causes in warm and cold regions of Europe. Lancet 1997, 349, 1341–1346. [Google Scholar]
- Yang, C.; Meng, X.; Chen, R.; Cai, J.; Zhao, Z.; Wan, Y.; Kan, H. Long-term variations in the association between ambient temperature and daily cardiovascular mortality in Shanghai, China. Sci. Total Environ. 2015, 538, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Keatinge, W.R.; Coleshaw, S.R.; Easton, J.C.; Cotter, F.; Mattock, M.B.; Chelliah, R. Increased platelet and red cell counts, blood viscosity, and plasma cholesterol levels during heat stress, and mortality from coronary and cerebral thrombosis. Am. J. Med. 1986, 81, 795–800. [Google Scholar] [PubMed]
- Nordio, F.; Zanobetti, A.; Colicino, E.; Kloog, I.; Schwartz, J. Changing patterns of the temperature-mortality association by time and location in the US, and implications for climate change. Environ. Int. 2015, 81, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Barnett, A.G. Temperature and cardiovascular deaths in the US elderly: Changes over time. Epidemiology 2007, 18, 369–372. [Google Scholar] [CrossRef] [PubMed]
- Curriero, F.C.; Heiner, K.S.; Samet, J.M.; Zeger, S.L.; Strug, L.; Patz, J.A. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 2002, 155, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Kalkstein, L.S.; Davis, R.E. Weather and human mortality: An evaluation of demographic and inter regional responses in the United States. Ann. Assoc. Am. Geogr. 1989, 79, 44–64. [Google Scholar] [CrossRef]
- Xiao, J.; Peng, J.; Zhang, Y.; Liu, T.; Rutherford, S.; Lin, H. How much does latitude modify temperature-mortality relationship in 13 eastern US cities? Int. J. Biometeorol. 2015, 59, 365–372. [Google Scholar] [CrossRef] [PubMed]
- Braga, A.L.; Zanobetti, A.; Schwartz, J. The time course of weather-related deaths. Epidemiology 2001, 12, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Pattenden, S.; Nikiforov, B.; Armstrong, B.G. Mortality and temperature in Sofia and London. J. Epidemiol. Community Health 2003, 57, 628–633. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.C.; Rha, J.H.; Lee, J.T.; Ha, E.H.; Kwon, H.J.; Kim, H. Ischemic stroke associated with decrease in temperature. Epidemiology 2003, 14, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Stewart, S.; Mcintyre, K.; Capewell, S.; McMurray, J. Heart failure in a cold climate: seasonal variation in heart failure-related morbidity and mortality. J. Am. Coll. Cardiol. 2002, 39, 760–766. [Google Scholar] [CrossRef]
- Zeka, A.; Browne, S.; McAvoy, H.; Goodman, P. The association of cold weather and all-cause and cause-specific mortality in the island of Ireland between 1984 and 2007. Environ. Health 2014, 13, 104. [Google Scholar] [CrossRef] [PubMed]
- Meehl, G.; Tebaldi, C.; Walton, G.; Easterling, D.; McDaniel, L.R. Relative increase of record high maximum temperatures compared to record low minimum temperatures in the U.S. Geophys. Res. Lett. 2009, 36. [Google Scholar] [CrossRef]
- Guo, C.Y.; Pan, W.C.; Chen, M.J.; Tsai, C.W.; Chen, N.T.; Su, H.J. When are we most vulnerable to temperature variations in a day? PLoS ONE 2014, 9, e113195. [Google Scholar] [CrossRef] [PubMed]
- Chen, R.; Wang, C.; Meng, X.; Chen, H.; Thach, T.Q.; Wong, C.M. Both low and high temperature may increase the risk of stroke mortality. Neurology 2013, 81, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Xie, H.; Yao, Z.; Zhang, Y.; Xu, Y.; Xu, X.; Liu, T.; Lin, H.; Lao, X.; Rutherford, S.; Chu, C.; et al. Short-term effects of the 2008 cold spell on mortality in three subtropical cities in Guangdong province, China. Environ. Health Perspect. 2013, 121, 210–216. [Google Scholar] [PubMed]
- Ayyappan, R.; Sankar, S.; Rajkumar, P.; Balakrishnan, K. Work-related heat stress concerns in automotive industries: A case study from Chennai, India. Glob. Health Action 2009, 2. [Google Scholar] [CrossRef] [PubMed]

| Variables | City | Daily Min | Daily Max | Total | Death Per 100,000 | Proportion |
|---|---|---|---|---|---|---|
| All ages | Hefei | 0 | 18 | 7483 | 958 | 100% |
| Changsha | 1 | 38 | 19,418 | 1107 | 100% | |
| Nanning | 0 | 19 | 9242 | 1181 | 100% | |
| Haikou | 0 | 16 | 5434 | 598 | 100% | |
| ≥65 years | Hefei | 0 | 16 | 6392 | 819 | 85.4% |
| Changsha | 0 | 34 | 16,014 | 913 | 82.5% | |
| Nanning | 0 | 17 | 7409 | 947 | 80.2% | |
| Haikou | 0 | 16 | 4257 | 469 | 78.3% | |
| <65 years | Hefei | 0 | 5 | 1091 | 139 | 14.6% |
| Changsha | 0 | 9 | 3404 | 194 | 17.5% | |
| Nanning | 0 | 6 | 1832 | 234 | 19.8% | |
| Haikou | 0 | 6 | 1177 | 129 | 21.7% | |
| Male | Hefei | 0 | 11 | 3884 | 497 | 51.9% |
| Changsha | 0 | 23 | 10,912 | 622 | 56.2% | |
| Nanning | 0 | 12 | 5165 | 660 | 55.9% | |
| Haikou | 0 | 12 | 3150 | 347 | 58.0% | |
| Female | Hefei | 0 | 9 | 3599 | 461 | 48.1% |
| Changsha | 0 | 21 | 8506 | 485 | 43.8% | |
| Nanning | 0 | 13 | 4077 | 521 | 44.1% | |
| Haikou | 0 | 12 | 2284 | 251 | 42.0% |
| Variables | City | Mean | STD | Median | Min | Max |
|---|---|---|---|---|---|---|
| Daily temperature (°C) | Hefei | 16.4 | 9.6 | 17.8 | −4.3 | 34.3 |
| Changsha | 18.3 | 9.3 | 19.2 | −2.8 | 35 | |
| Nanning | 21.4 | 6.7 | 23.2 | 3.7 | 31.3 | |
| Haikou | 23.9 | 4.7 | 25.4 | 8.7 | 31.6 | |
| Relative humidity (%) | Hefei | 73.6 | 16.1 | 76 | 23 | 100 |
| Changsha | 74.8 | 12.5 | 76 | 29 | 97 | |
| Nanning | 76.2 | 9.3 | 77 | 39 | 96 | |
| Haikou | 80.5 | 8.0 | 81 | 47 | 98 | |
| Air Press | Hefei | 10,132 | 95 | 10,133 | 9944 | 10,386 |
| Changsha | 10,086 | 92.1 | 10,085 | 9911 | 10,322 | |
| Nanning | 9982 | 71.6 | 9977 | 9798 | 10,167 | |
| Haikou | 10,036 | 60.8 | 10,029 | 9781 | 10,207 | |
| API | Hefei | 83.5 | 37.1 | 80 | 0 | 500 |
| Changsha | 68.7 | 27.1 | 67 | 11 | 443 | |
| Nanning | 52.4 | 22.9 | 52 | 0 | 163 | |
| Haikou | 38.4 | 14.4 | 35 | 0 | 99 |
| City | Group | Cold Effect | Heat Effect | ||
|---|---|---|---|---|---|
| Estimate (%) | 95% CI | Estimate (%) | 95% CI | ||
| Hefei | All ages | 4.1 * | 1.9–6.2 | 4.5 * | 1.2–7.9 |
| ≥65 | 4.3 * | 1.6–7.0 | 4.9 * | 0.4–9.4 | |
| <65 | 3.7 * | 0.6–6.8 | 2.8 | −1.2–6.8 | |
| Males | 3.6 * | 0.5–6.8 | 4.9 * | 0.4–9.7 | |
| Females | 4.8 * | 2.4–7.2 | 3.9 | −0.9–8.9 | |
| Changsha | All ages | 4.9 * | 2.9–6.9 | 4.4 * | 1.4–7.5 |
| ≥65 | 6.2 * | 4.0–8.3 | 5.1 * | 0.6–9.6 | |
| <65 | 3.3 * | 0.2–6.5 | 3.7 | −0.6–7.6 | |
| Males | 3.9 * | 1.2–6.6 | 2.8 * | 0.2–5.4 | |
| Females | 6.1 * | 3.7–8.5 | 6.3 * | 1.9–10.8 | |
| Nanning | All ages | 2.8 * | 0.7–5.1 | 9.8 | −1.7–18.7 |
| ≥65 | 3.6 * | 1.3–5.9 | 11.4 * | 0.9–22.8 | |
| <65 | 1.0 | −3.1–5.3 | 0.4 | −17.9–20.2 | |
| Males | 3.8 * | 1.2–6.4 | 10.9 | −3.5–25.3 | |
| Females | 2.6 | −0.4–5.7 | 6.2 | −4.6–17 | |
| Haikou | All ages | 5.8 * | 1.2–10.7 | 4.2 | −13.9–17.9 |
| ≥65 | 5.9 * | 0.8–11.2 | 5.0 | −11.4–24.5 | |
| <65 | 5.4 | −5.5–17.4 | −9.3 | −35.9–28.3 | |
| Males | 2.5 | −3.3–8.6 | −3.1 | −20.9–18.7 | |
| Females | 10.0 * | 2.6–17.9 | 4.3 | −16.5–30.4 | |
| Group | Cold Effect | Heat Effect | ||
|---|---|---|---|---|
| Estimate (%) | 95%CI | Estimate (%) | 95%CI | |
| All ages | 4.2 | 3.0–5.4 | 4.6 | 3.0–6.2 |
| ≥65 | 4.9 | 3.5–6.3 | 6.4 | 3.4–9.4 |
| <65 | 3.1 | 1.7–4.5 | 0.2 | −4.8–5.2 |
| Males | 3.6 | 2.2–5.0 | 5.6 | 2.5–8.7 |
| Females | 5.6 | 3.9–8.3 | 4.1 | 2.7–5.5 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, J.; Tan, J.; Yu, W. Temperature and Cardiovascular Mortality Associations in Four Southern Chinese Cities: A Time-Series Study Using a Distributed Lag Non-Linear Model. Sustainability 2017, 9, 321. https://doi.org/10.3390/su9030321
Huang J, Tan J, Yu W. Temperature and Cardiovascular Mortality Associations in Four Southern Chinese Cities: A Time-Series Study Using a Distributed Lag Non-Linear Model. Sustainability. 2017; 9(3):321. https://doi.org/10.3390/su9030321
Chicago/Turabian StyleHuang, Jixia, Jing Tan, and Weiwei Yu. 2017. "Temperature and Cardiovascular Mortality Associations in Four Southern Chinese Cities: A Time-Series Study Using a Distributed Lag Non-Linear Model" Sustainability 9, no. 3: 321. https://doi.org/10.3390/su9030321





