Metrological Characterization for Vital Sign Detection by a Bioradar
Abstract
:1. Introduction
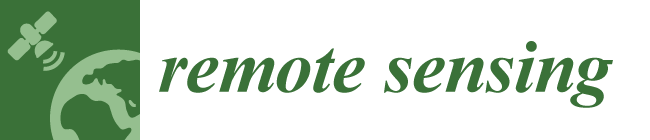
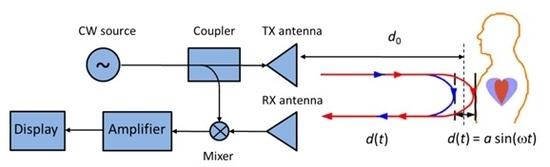
2. Bioradar Prototype
3. Measurement Results
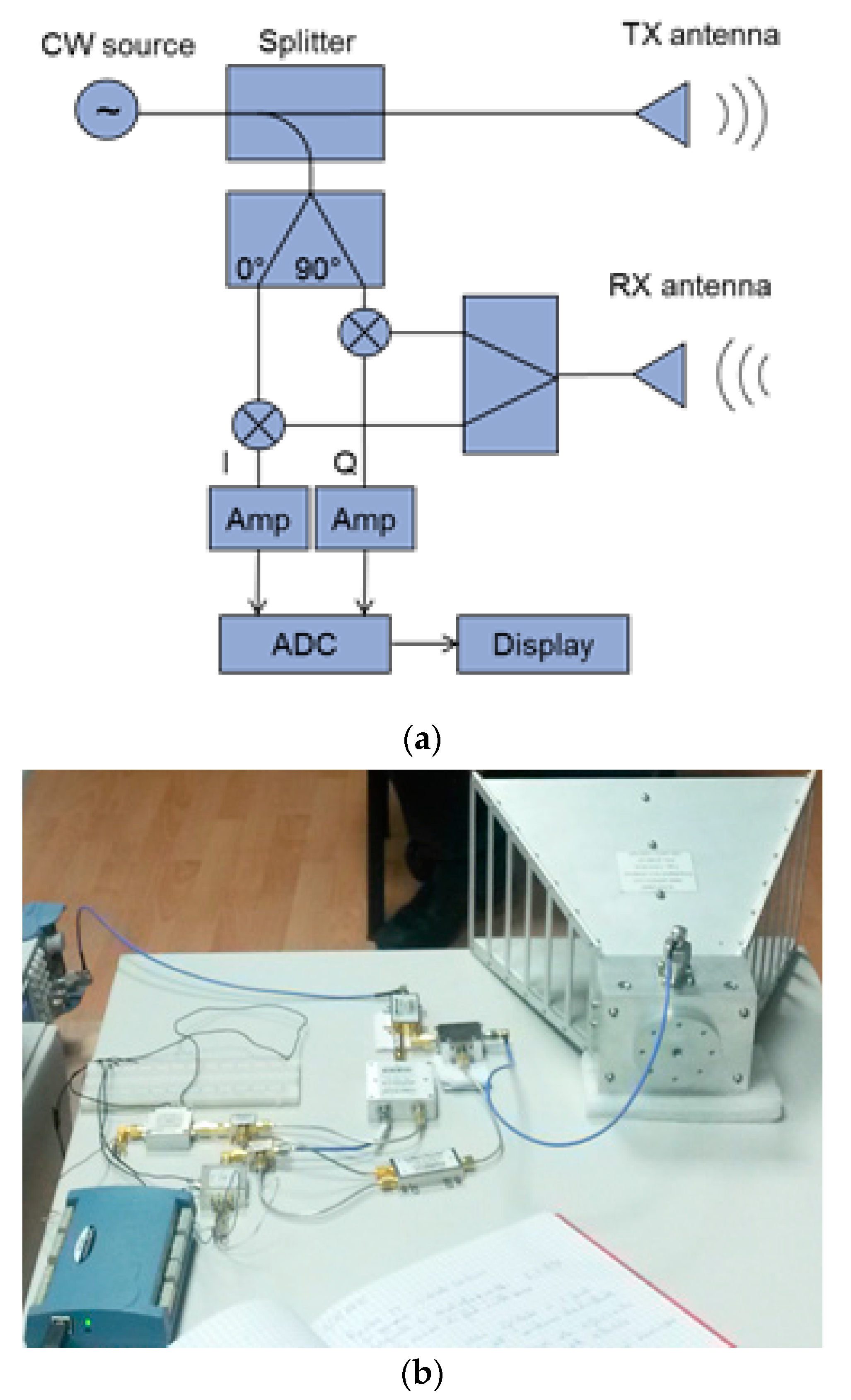
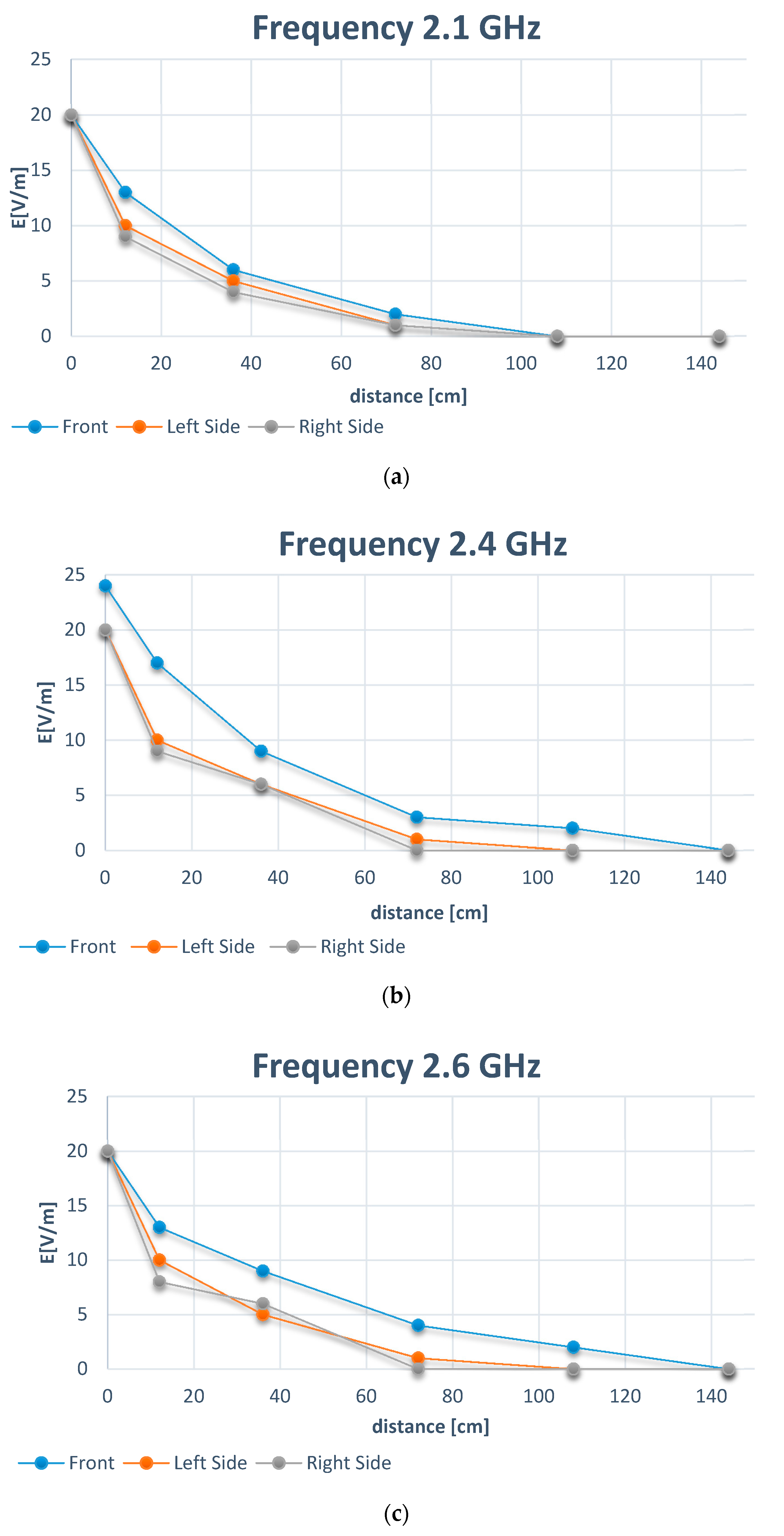
3.1. Electromagnetic Field Levels
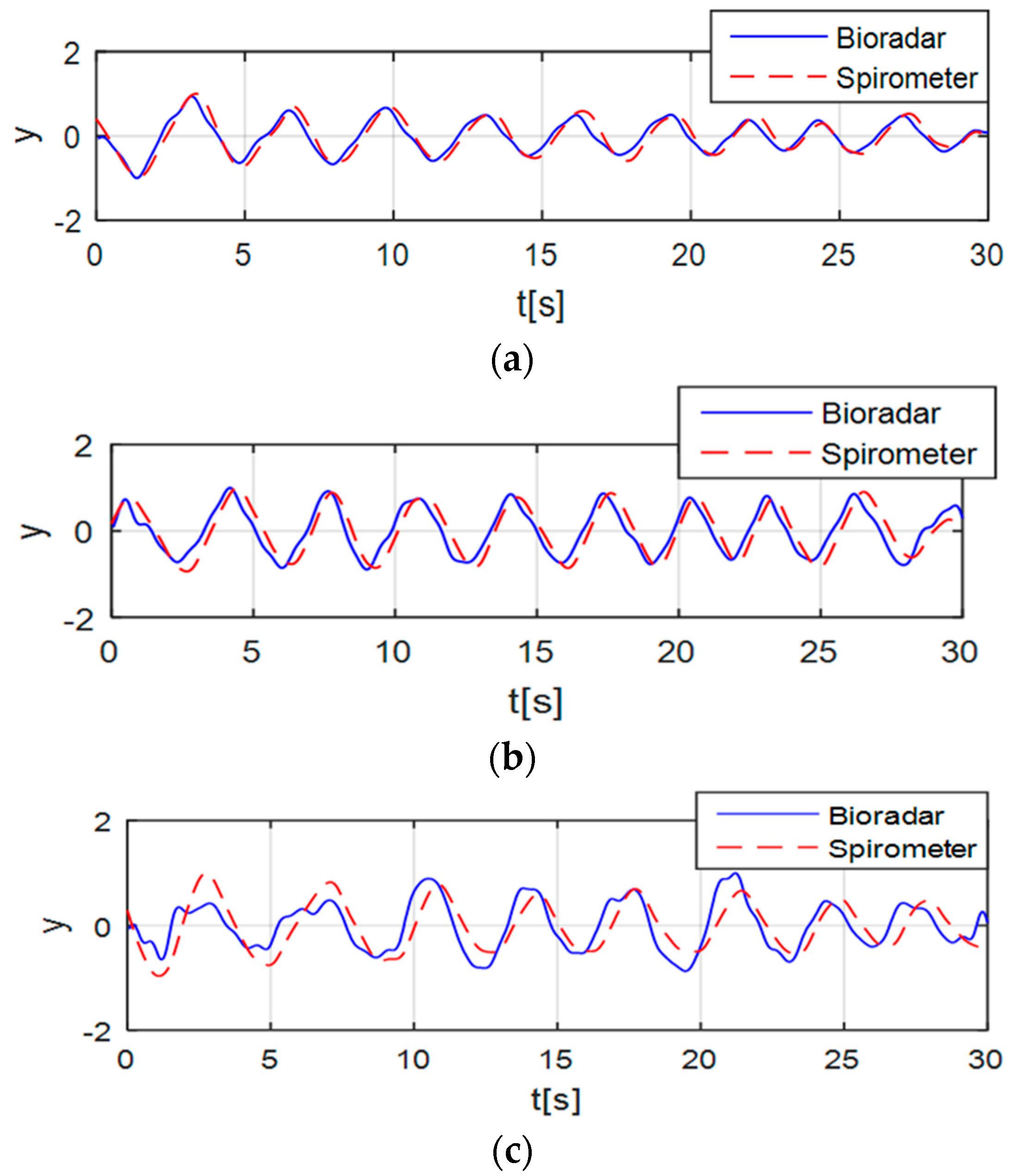
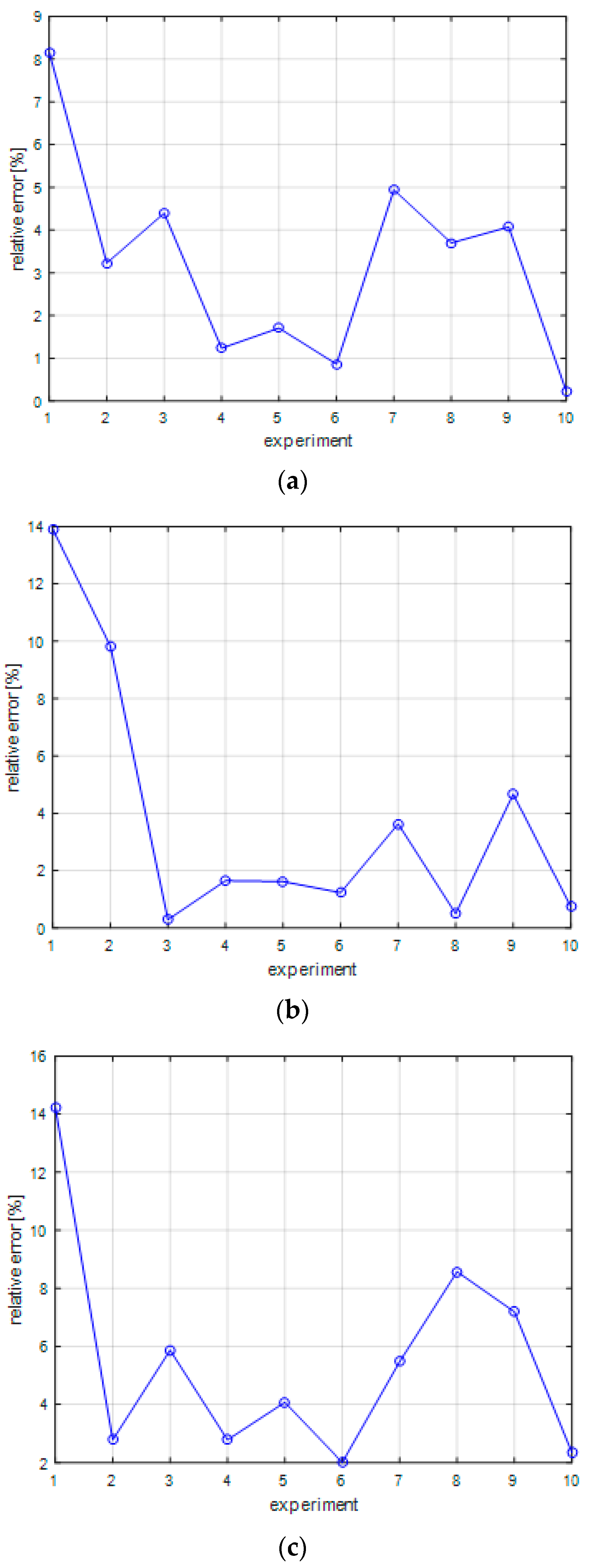
3.2. Experimental Results
4. Bioradar Measurement Uncertainty
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Lin, J.C. Non-invasive microwave measurement of respiration. Proc. IEEE 1975, 63, 557–565. [Google Scholar] [CrossRef]
- Li, C.; Lin, J. Microwave Non-Contact Motion Sensing and Analysis; Wiley: Hoboken, NJ, USA, 2014. [Google Scholar]
- Zhang, Y.; Chen, F.; Xue, H.; Li, Z.; An, Q.; Wang, J.; Zhang, Y. Detection and identification of multiple stationary human targets via bio-radar based on the cross-correlation method. Sensors 2016, 16, 1793. [Google Scholar] [CrossRef] [PubMed]
- Gennarelli, G.; Ludeno, G.; Soldovieri, F. Real-time through-wall situation awareness using a microwave Doppler radar sensor. Remote Sens. 2016, 8, 621. [Google Scholar] [CrossRef]
- Anishchenko, L.N.; Demendeev, A.A.; Ivashov, S.I. Use of Radiolocation for Non-contact Estimation of Patterns of Respiration and Motion Activity in Sleeping Humans. Biomed. Eng. 2013, 47, 7–11. [Google Scholar] [CrossRef]
- Li, C.; Lubecke, V.M.; Boric-Lubecke, O.; Lin, J. A review on recent advances in Doppler radar sensors for non-contact healthcare monitoring. IEEE Trans. Microw. Theory Tech. 2013, 61, 2046–2060. [Google Scholar] [CrossRef]
- Lee, Y.S.; Pathirana, P.N.; Steinfort, C.L.; Caelli, T. Monitoring and Analysis of Respiratory Patterns Using Microwave Doppler Radar. IEEE J. Transl. Eng. Health Med. 2014, 2, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Dei, D.; Grazzini, G.; Luzi, G.; Pieraccini, M.; Atzeni, C.; Boncinelli, S.; Camiciottoli, G.; Castellani, W.; Marsili, M.; Dico, J.L. Non-contact detection of breathing using a microwave sensor. Sensors 2009, 9, 2574–2585. [Google Scholar] [CrossRef] [PubMed]
- Baboli, M.; Singh, A.; Soll, B.; Boric-Lubecke, O.; Lubecke, V.M. Good night: Sleep monitoring using a physiological radar monitoring system integrated with a polysomnography system. IEEE Microw. Mag. 2015, 16, 34–41. [Google Scholar] [CrossRef]
- Wang, J.; Wang, X.; Zhu, Z.; Huangfu, J.; Li, C.; Ran, L. 1D microwave imaging of human cardiac motion: An ab-initio investigation. IEEE Trans. Microw. Theory Tech. 2013, 61, 2101–2107. [Google Scholar] [CrossRef]
- Lv, H.; Qi, F.; Zhang, Y.; Jiao, T.; Liang, F.; Li, Z.; Wang, J. Improved Detection of Human Respiration Using Data Fusion Based on a Multistatic UWB Radar. Remote Sens. 2016, 8, 773. [Google Scholar] [CrossRef]
- Gennarelli, G.; Soldovieri, F.; Marciano, L.; Cerasuolo, G.; Petrella, O. Measurements Performance of a Bioradar for Human Respiration Monitoring. Procedia Eng. 2016, 168, 1200–1203. [Google Scholar] [CrossRef]
- Anishchenko, L.; Ivashov, S.; Soldovieri, F.; Catapano, I.; Crocco, L. Comparison study of two approaches for bioradar data processing. In Proceedings of the IET International Radar Conference, Xi’an, China, 14–16 April 2013. [Google Scholar]
- Catapano, I.; Crocco, L.; Gennarelli, G.; Soldovieri, F. Radar for vital signs characterization: A comparison between two different frequency bad systems. In Proceedings of the IEEE 7th International Workshop on Advanced Ground Penetrating Radar, Nantes, France, 2–5 July 2013. [Google Scholar]
- Girbau, D.; Lazaro, A.; Ramos, A.; Villarino, R. Remote sensing of vital signs using a Doppler radar and diversity to overcome null detection. IEEE Sens. J. 2012, 12, 512–518. [Google Scholar] [CrossRef]
- Jang, B.J.; Wi, S.-H.; Yook, J.-G.; Lee, M.-Q.; Lee, K.-J. Wireless bio-radar sensor for heartbeat and respiration detection. Prog. Electromagn. Res. C 2008, 5, 149–168. [Google Scholar]
- Anishchenko, L.; Gennarelli, G.; Tataraidze, A.; Gaysina, E.; Soldovieri, F. Evaluation of rodents’ respiratory activity using a bioradar. IET Radar Sonar Navig. 2015, 9, 1296–1302. [Google Scholar] [CrossRef]
- Art. 3 DPCM 8 July 2003, 1 of Italian Law n. 36. 2001. Available online: http://www.regione.piemonte.it/ambiente/elettromagnetismo/dwd/normativa/statale/dpcm_08_07_03_2.pdf (accessed on 26 September 2017).
- Evaluation of Measurement Data—Guide to the Expression of Uncertainty in Measurement, Joint Committee for Guides in Metrology. 2008. Available online: http://www.sci.utah.edu/~kpotter/Library/Papers/jcgm:2008:EMDG/index.html (accessed on 26 September 2017).
| Frequency Range | RMS Electric Field (V/m) | RMS Magnetic Field (A/m) | Irradiance (W/m2) |
|---|---|---|---|
| 0.1–300 GHz | 6 | 0.016 | 0.10 (3 MHz–300 GHz) |
| Test | 2.1 GHz | 2.4 GHz | 2.6 GHz | |||
|---|---|---|---|---|---|---|
| Bioradar [Hz] | Spirometer [Hz] | Bioradar [Hz] | Spirometer [Hz] | Bioradar [Hz] | Spirometer [Hz] | |
| 1 | 0.322 | 0.350 | 0.327 | 0.287 | 0.301 | 0.350 |
| 2 | 0.365 | 0.383 | 0.299 | 0.331 | 0.325 | 0.334 |
| 3 | 0.332 | 0.347 | 0.340 | 0.341 | 0.275 | 0.293 |
| 4 | 0.331 | 0.335 | 0.310 | 0.315 | 0.302 | 0.292 |
| 5 | 0.306 | 0.301 | 0.324 | 0.329 | 0.251 | 0.261 |
| 6 | 0.348 | 0.350 | 0.325 | 0.329 | 0.279 | 0.274 |
| 7 | 0.349 | 0.333 | 0.317 | 0.328 | 0.275 | 0.292 |
| 8 | 0.272 | 0.262 | 0.320 | 0.319 | 0.250 | 0.273 |
| 9 | 0.251 | 0.262 | 0.338 | 0.323 | 0.252 | 0.272 |
| 10 | 0.349 | 0.348 | 0.312 | 0.314 | 0.273 | 0.280 |
| Bioradar Frequency | 2.1 GHz | 2.4 GHz | 2.6 GHz |
|---|---|---|---|
| ximax | 0.365 Hz | 0.340 Hz | 0.325 Hz |
| ximin | 0.251 Hz | 0.299 Hz | 0.250 Hz |
| Bioradar Frequency | 2.1 GHz | 2.4 GHz | 2.6 GHz |
|---|---|---|---|
| Measured value ± uncertainty | (0.320 ± 0.06) Hz | (0.321 ± 0.02) Hz | (0.270 ± 0.04) Hz |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cerasuolo, G.; Petrella, O.; Marciano, L.; Soldovieri, F.; Gennarelli, G. Metrological Characterization for Vital Sign Detection by a Bioradar. Remote Sens. 2017, 9, 996. https://doi.org/10.3390/rs9100996
Cerasuolo G, Petrella O, Marciano L, Soldovieri F, Gennarelli G. Metrological Characterization for Vital Sign Detection by a Bioradar. Remote Sensing. 2017; 9(10):996. https://doi.org/10.3390/rs9100996
Chicago/Turabian StyleCerasuolo, Giovanni, Orsola Petrella, Luigi Marciano, Francesco Soldovieri, and Gianluca Gennarelli. 2017. "Metrological Characterization for Vital Sign Detection by a Bioradar" Remote Sensing 9, no. 10: 996. https://doi.org/10.3390/rs9100996