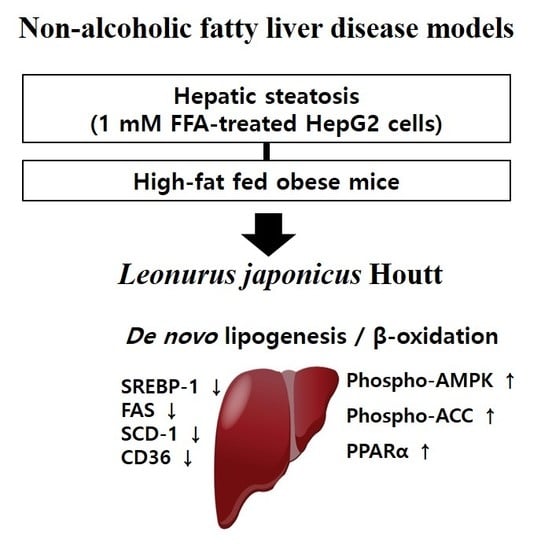
Leonurus japonicus Houtt Attenuates Nonalcoholic Fatty Liver Disease in Free Fatty Acid-Induced HepG2 Cells and Mice Fed a High-Fat Diet
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of L. japonicus Ethanol Extract (LJE)
2.2. Cell Culture
2.3. Cell Viability
2.4. Oil Red O Staining
2.5. Fluorometric Determination of TG Content by Nile Red
2.6. Immunoblot Analysis
2.7. Analysis of mRNA Expression
2.8. Animal Experiment
2.9. Biochemical Assays
2.10. Liver Lipids, TG, and TC
2.11. Hematoxylin and Eosin Staining (HE)
2.12. Statistical Analysis
3. Results
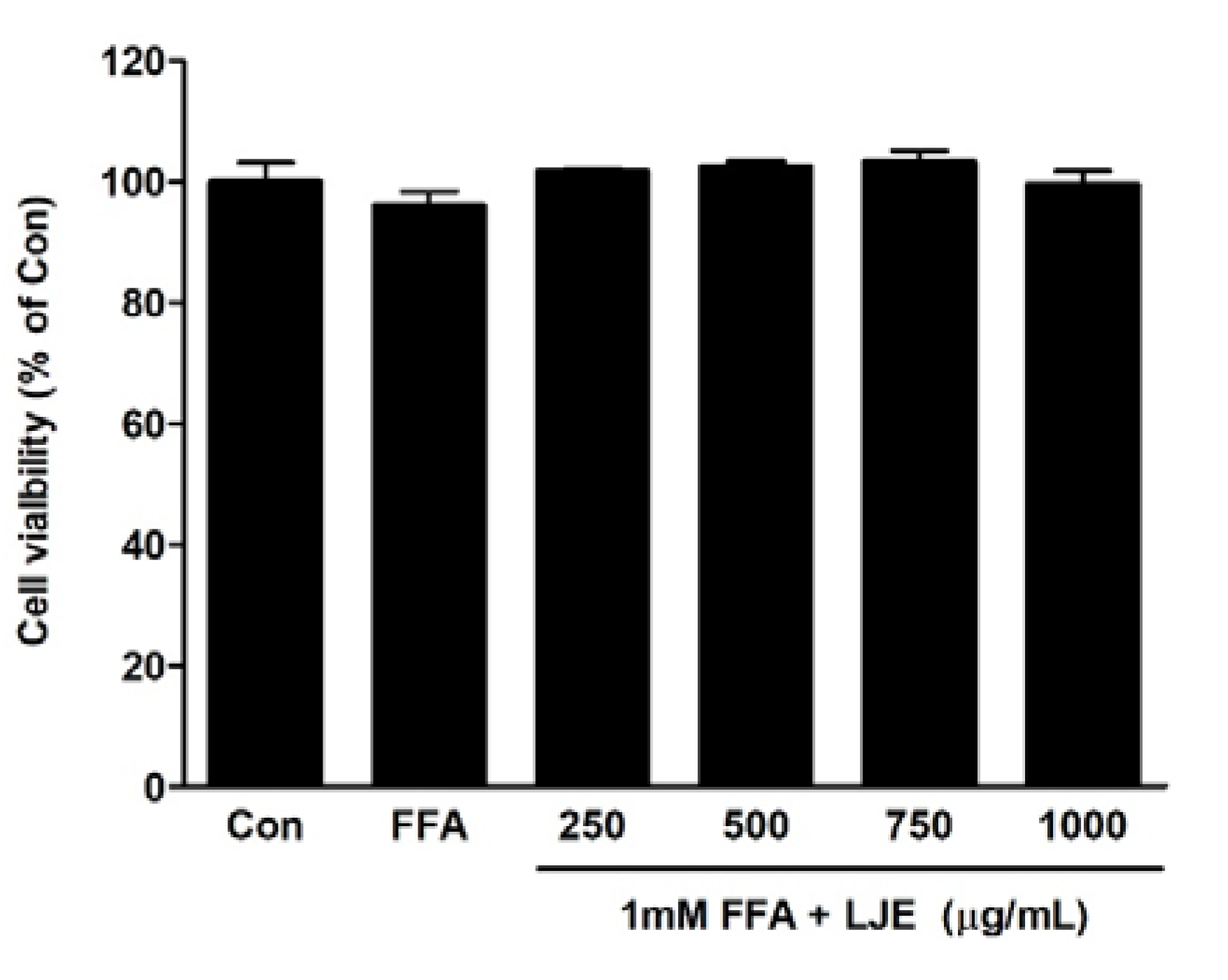
3.1. Cell Viability of LJE
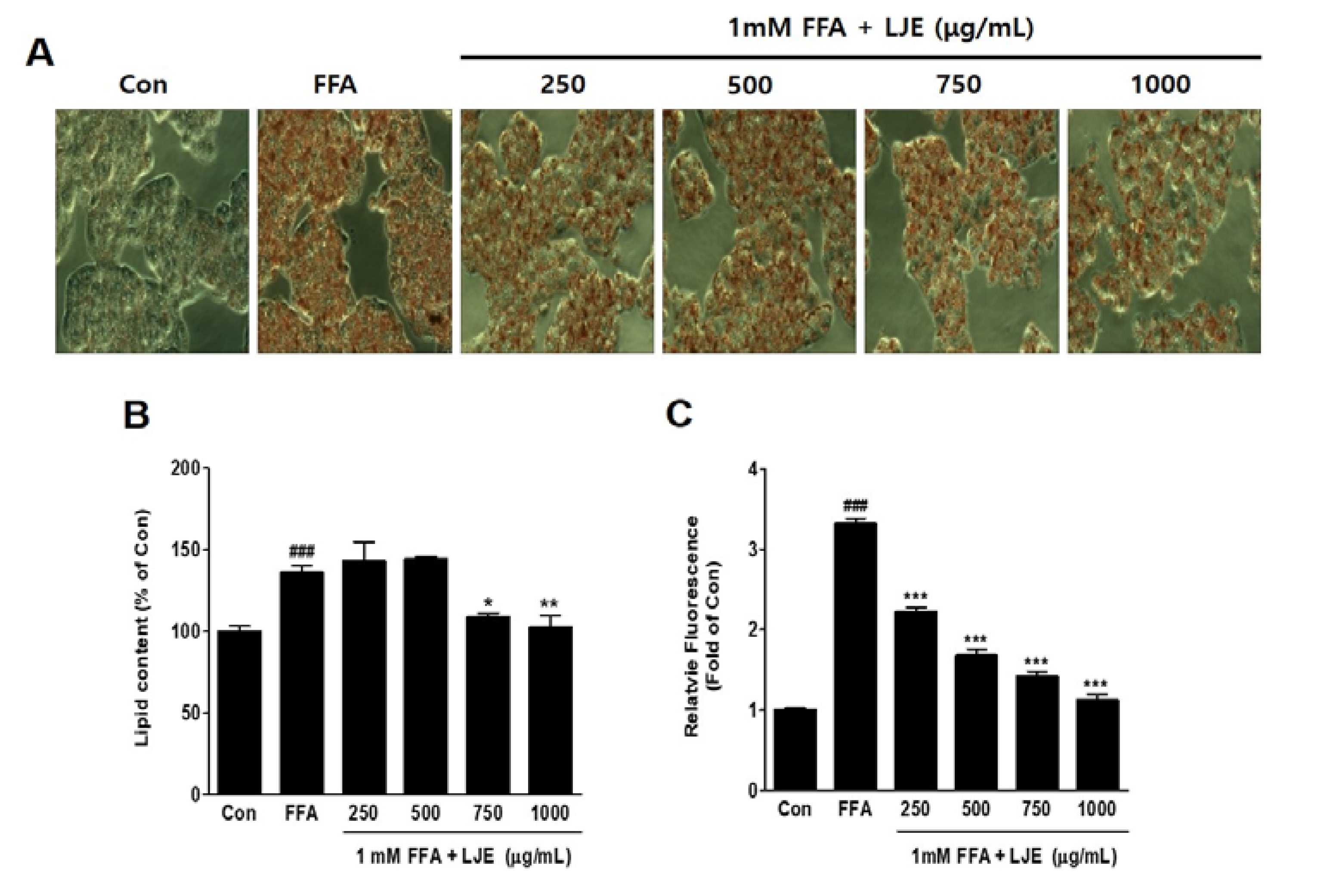
3.2. Effects of LJE on Lipid Accumulation in HepG2 Cells
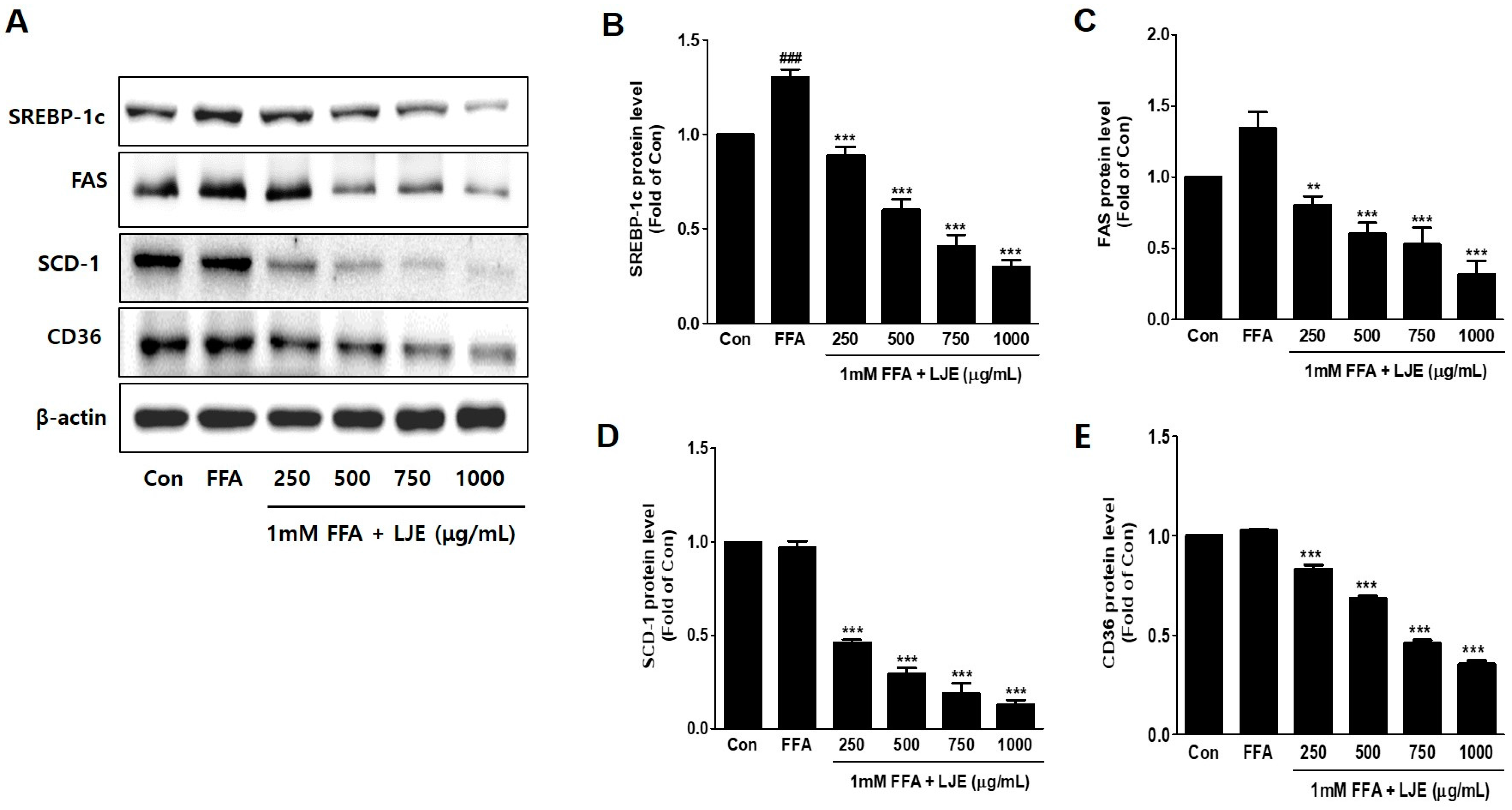
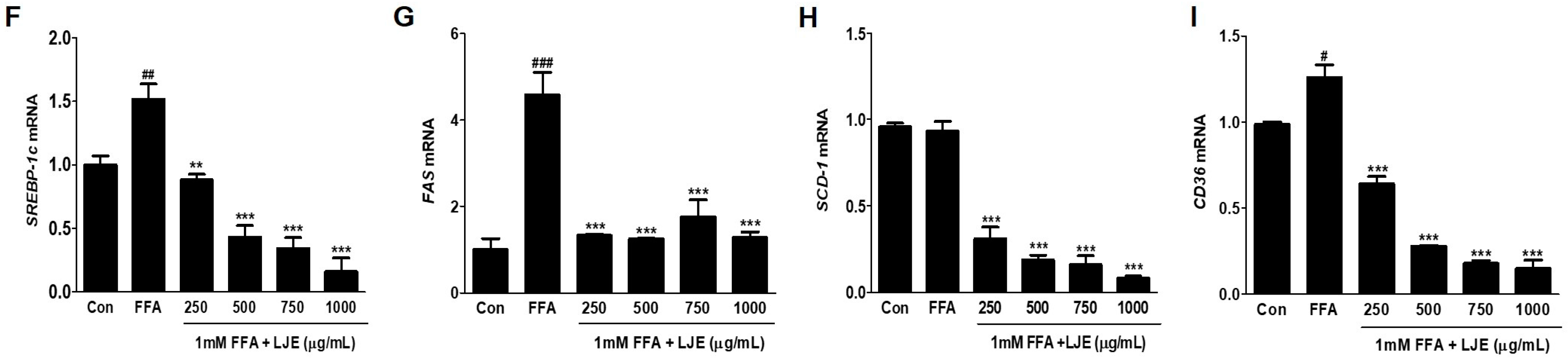
3.3. Effects of LJE on Lipogenesis in HepG2 Cells
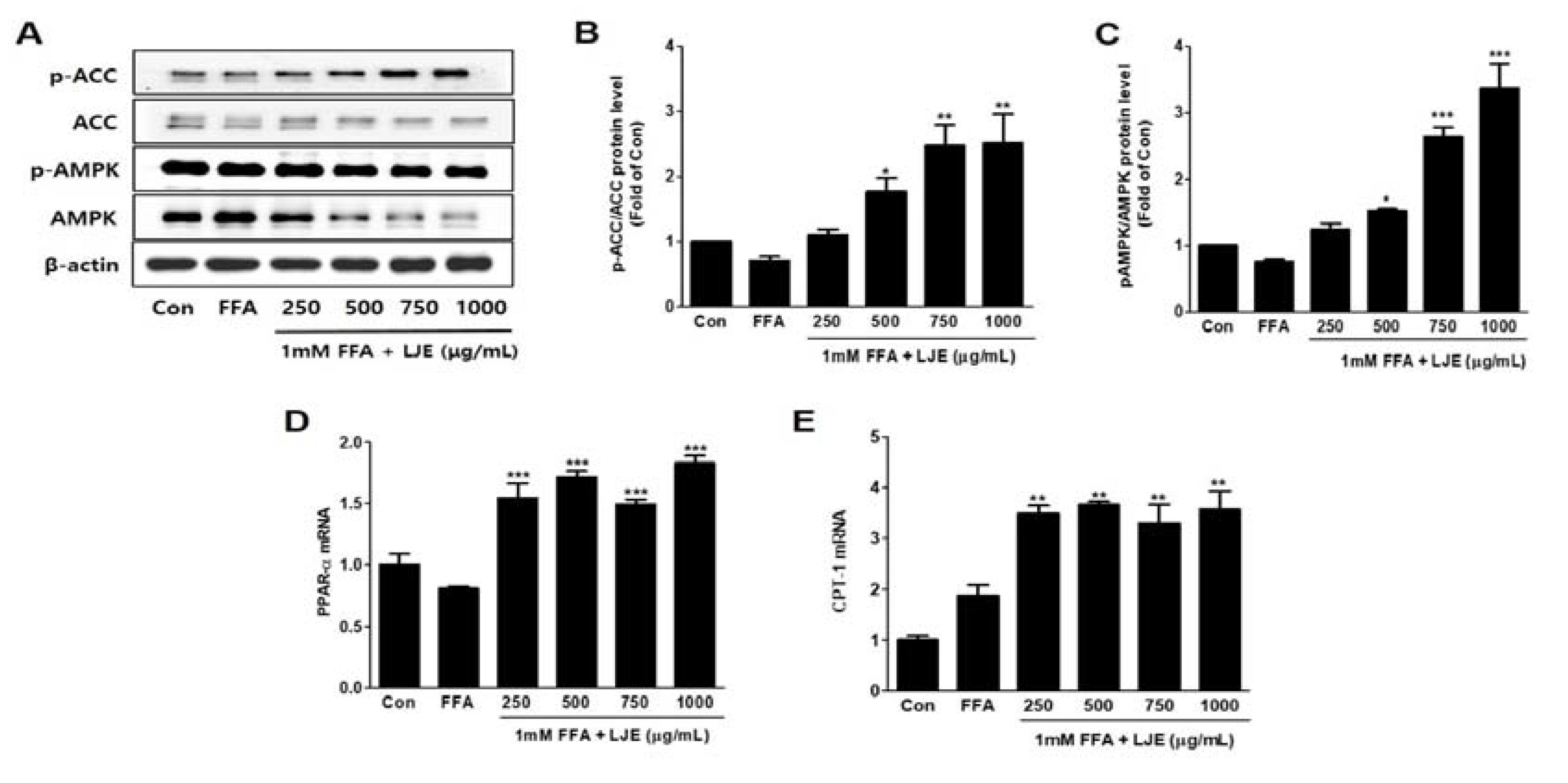
3.4. Effects of LJE on Phosphorylation of AMP-activated Protein Kinase (AMPK) and Acetyl-CoA Carboxylase (ACC) and mRNA Expression of PPARα and CPT-1 in HepG2 Cells
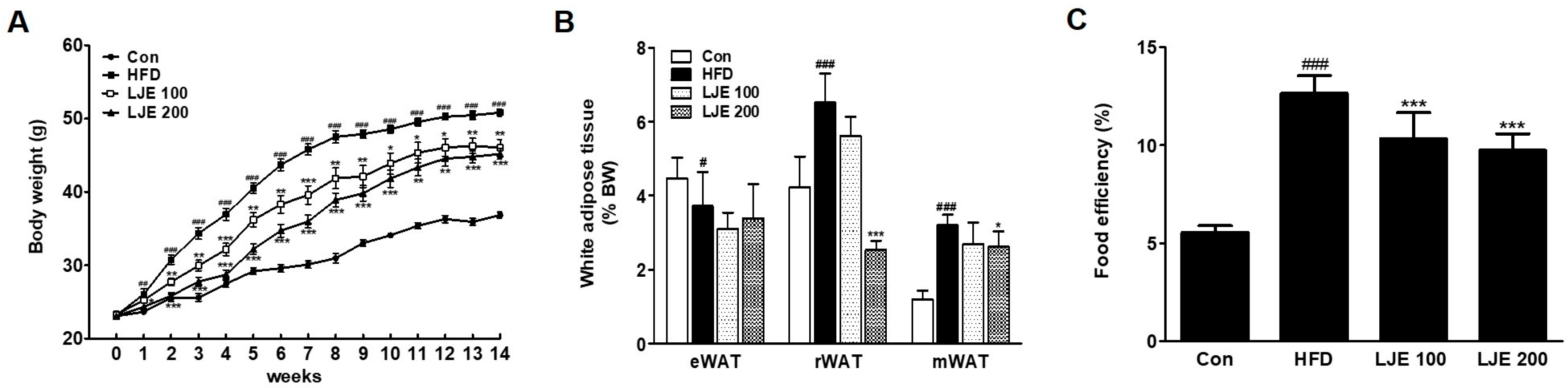
3.5. Effects of LJE on Body Weight and Visceral White Adipose Tissues in HFD-Fed Mice
3.6. Effects of LJE on Serum Lipids, Liver Enzymes, and MDA Levels in Serum
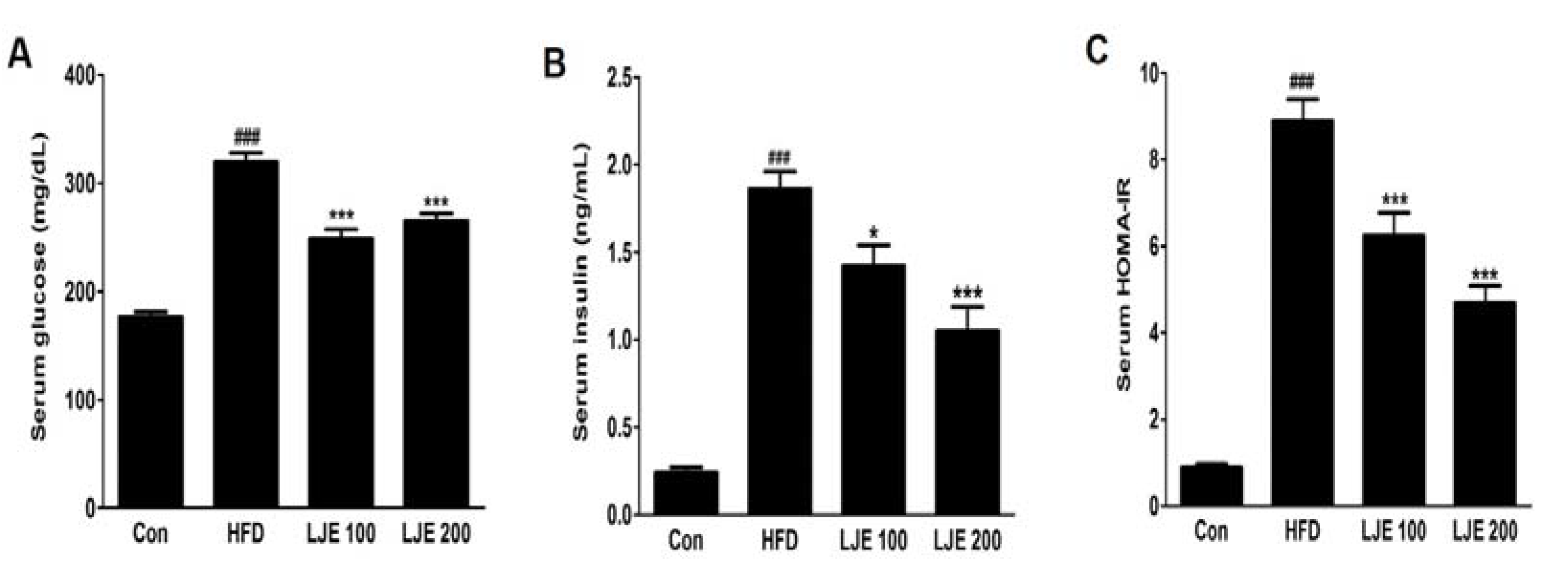
3.7. Effects of LJE on Serum Glucose and Insulin in HFD-Fed Mice
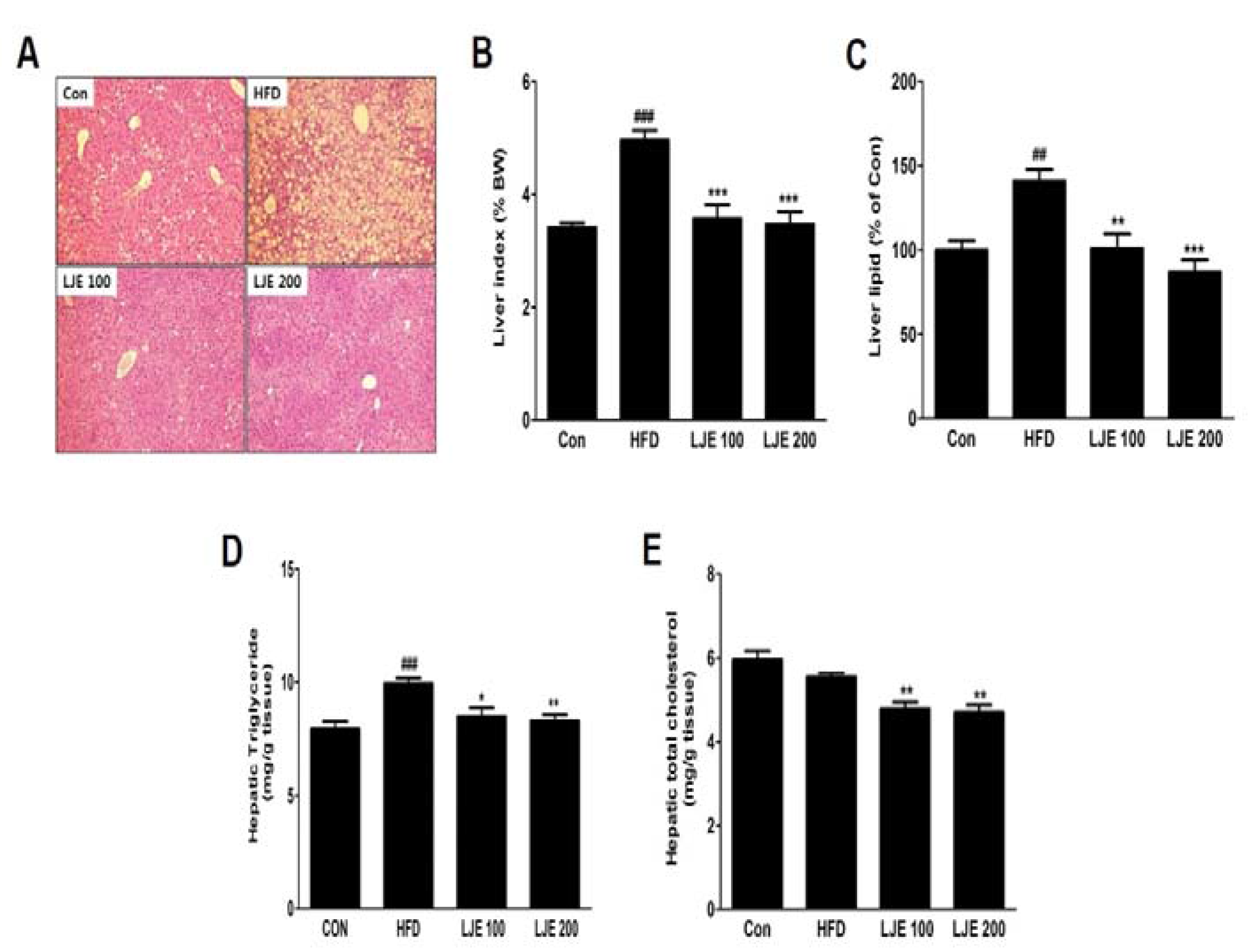
3.8. Effects of LJE on the Liver Steatosis in HFD-Fed Mice
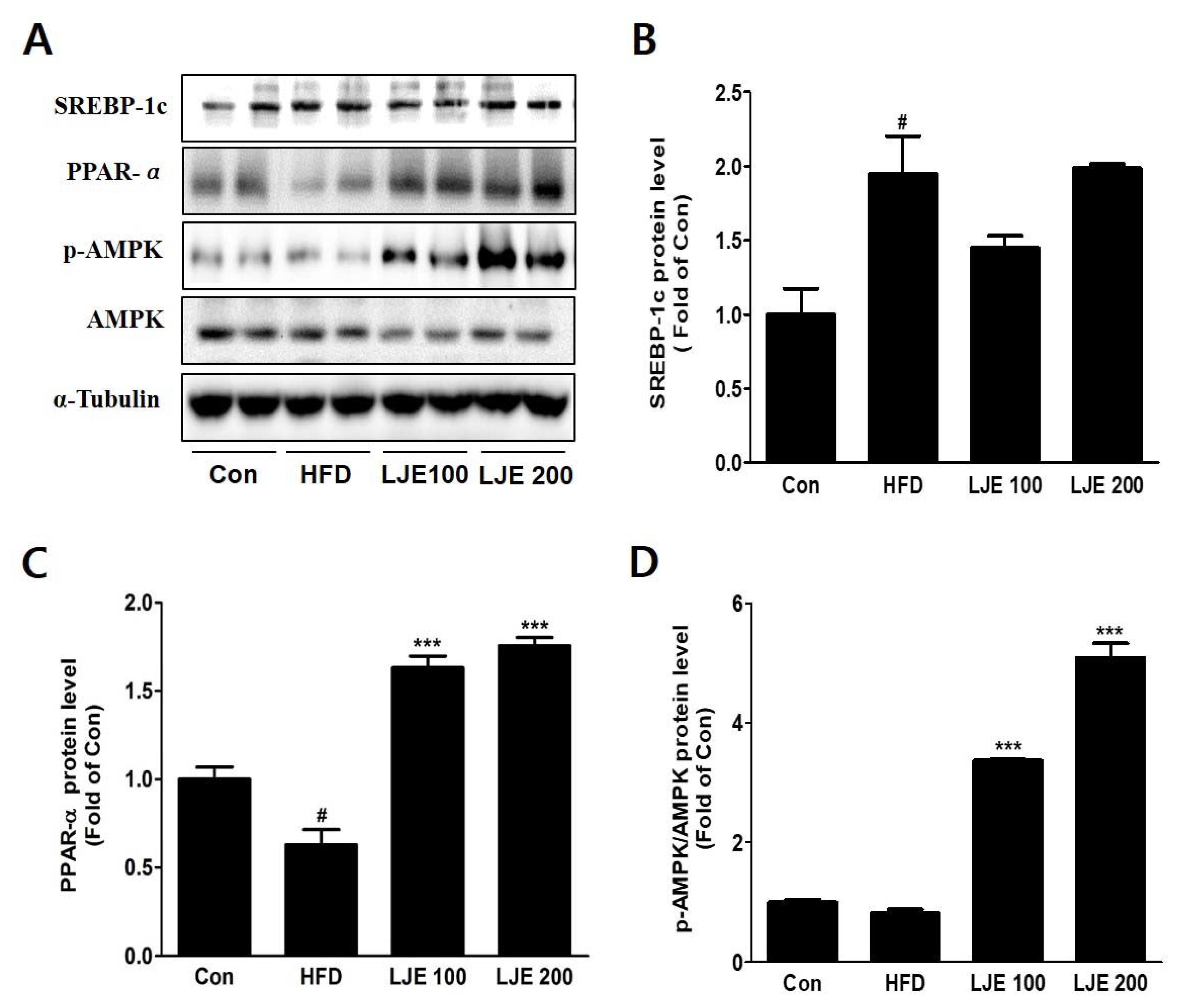
3.9. Effects of LJE on Hepatic Lipid Metabolism in HFD-Fed Mice
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Farrell, G.C.; Larter, C.Z. Nonalcoholic fatty liver disease: From steatosis to cirrhosis. Hepatology 2006, 43, S99–S112. [Google Scholar] [CrossRef] [PubMed]
- Parekh, S.; Anania, F.A. Abnormal lipid and glucose metabolism in obesity: Implications for nonalcoholic fatty liver disease. Gastroenterology 2007, 132, 2191–2207. [Google Scholar] [CrossRef] [PubMed]
- Hardy, T.; Oakley, F.; Anstee, Q.M.; Day, C.P. Nonalcoholic Fatty Liver Disease: Pathogenesis and Disease Spectrum. Annu. Rev. Pathol. 2016, 11, 451–496. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Ma, Y.; Liu, D. High-fat diet-induced adiposity, adipose inflammation, hepatic steatosis and hyperinsulinemia in outbred CD-1 mice. PLoS ONE 2015, 10, e0119784. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, A.; Terauchi, Y. Lessons from mouse models of high-fat diet-induced NAFLD. Int. J. Mol. Sci. 2013, 14, 21240–21257. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, Y.; Soejima, Y.; Fukusato, T. Animal models of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J. Gastroenterol. 2012, 18, 2300–2308. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Lechon, M.J.; Donato, M.T.; Martinez-Romero, A.; Jimenez, N.; Castell, J.V.; O’Connor, J.E. A human hepatocellular In Vitro model to investigate steatosis. Chem. Biol. Interact. 2007, 165, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Kanuri, G.; Bergheim, I. In Vitro and In Vivo models of non-alcoholic fatty liver disease (NAFLD). Int. J. Mol. Sci. 2013, 14, 11963–11980. [Google Scholar] [CrossRef] [PubMed]
- Beaton, M.D. Current treatment options for nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Can. J. Gastroenterol. 2012, 26, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Bahmani, M.; Eftekhari, Z.; Saki, K.; Fazeli-Moghadam, E.; Jelodari, M.; Rafieian-Kopaei, M. Obesity Phytotherapy: Review of Native Herbs Used in Traditional Medicine for Obesity. J. Evid.-Based Complement. Altern. Med. 2016, 21, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Bahmani, M.; Mirhoseini, M.; Shirzad, H.; Sedighi, M.; Shahinfard, N.; Rafieian-Kopaei, M. A review on promising natural agents effective on hyperlipidemia. J. Evid.-Based Complement. Altern. Med. 2015, 20, 228–238. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Fronczek, F.R.; Ferreira, D.; Burandt, C.L., Jr.; Zjawiony, J.K. Labdane diterpenoids from Leonurus sibiricus. J. Nat. Prod. 2011, 74, 831–836. [Google Scholar] [CrossRef] [PubMed]
- Shang, X.; Pan, H.; Wang, X.; He, H.; Li, M. Leonurus japonicus Houtt.: Ethnopharmacology, phytochemistry and pharmacology of an important traditional Chinese medicine. J. Ethnopharmacol. 2014, 152, 14–32. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.Y.; Kim, S.H.; Kang, S.M.; Chang, I.J.; Kim, S.Y.; Jeon, H.; Leem, K.H.; Park, W.H.; Lim, J.P.; Shin, T.Y. Anti-inflammatory activity of Motherwort (Leonurus sibiricus L.). Immunopharmacol. Immunotoxicol. 2009, 31, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Pan, L.; Gong, Q.; Zhu, Y. Leonurine (SCM-198) improves cardiac recovery in rat during chronic infarction. Eur. J. Pharmacol. 2010, 649, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kim, M.H.; Choi, Y.Y.; Hong, J.; Yang, W.M. Inhibitory effects of Leonurus sibiricus on weight gain after menopause in ovariectomized and high-fat diet-fed mice. J. Nat. Med. 2016, 70, 522–530. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Lee, J.J.; Cho, W.K.; Yim, N.H.; Kim, H.K.; Yun, B.; Ma, J.Y. KBH-1, an herbal composition, improves hepatic steatosis and leptin resistance in high-fat diet-induced obese rats. BMC Complement. Altern. Med. 2016, 16, 355. [Google Scholar] [CrossRef] [PubMed]
- Toye, A.A.; Dumas, M.E.; Blancher, C.; Rothwell, A.R.; Fearnside, J.F.; Wilder, S.P.; Bihoreau, M.T.; Cloarec, O.; Azzouzi, I.; Young, S.; et al. Subtle metabolic and liver gene transcriptional changes underlie diet-induced fatty liver susceptibility in insulin-resistant mice. Diabetologia 2007, 50, 1867–1879. [Google Scholar] [CrossRef] [PubMed]
- Misra, A.; Bhardwaj, S. Obesity and the metabolic syndrome in developing countries: Focus on South Asians. In International Nutrition: Achieving Millennium Goals and Beyond; Karger Publishers: Basel, Switzerland, 2014; Volume 78, pp. 133–140. [Google Scholar]
- Zhang, Y.; Deng, S.; Qu, L.; An, Y.T.; Wu, C.H.; Han, L.F.; Gao, X.M.; Wang, T. Rare syringyl acylated flavonol glycosides from the aerial parts of Leonurus japonicus Houtt. Molecules 2013, 18, 2967–2977. [Google Scholar] [CrossRef] [PubMed]
- Cui, B.; Liu, S.; Lin, X.; Wang, J.; Li, S.; Wang, Q.; Li, S. Effects of Lycium barbarum aqueous and ethanol extracts on high-fat-diet induced oxidative stress in rat liver tissue. Molecules 2011, 16, 9116–9128. [Google Scholar] [CrossRef] [PubMed]
- Yu, A.S.; Keeffe, E.B. Elevated AST or ALT to nonalcoholic fatty liver disease: Accurate predictor of disease prevalence? Am. J. Gastroenterol. 2003, 98, 955–956. [Google Scholar] [CrossRef] [PubMed]
- Day, C.P.; James, O.F. Steatohepatitis: A tale of two “hits”? Gastroenterology 1998, 114, 842–845. [Google Scholar] [CrossRef]
- Schmidt, S.; Jakab, M.; Jav, S.; Streif, D.; Pitschmann, A.; Zehl, M.; Purevsuren, S.; Glasl, S.; Ritter, M. Extracts from Leonurus sibiricus L. increase insulin secretion and proliferation of rat INS-1E insulinoma cells. J. Ethnopharmacol. 2013, 150, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Fabbrini, E.; Sullivan, S.; Klein, S. Obesity and nonalcoholic fatty liver disease: Biochemical, metabolic, and clinical implications. Hepatology 2010, 51, 679–689. [Google Scholar] [CrossRef] [PubMed]
- Kawano, Y.; Cohen, D.E. Mechanisms of hepatic triglyceride accumulation in non-alcoholic fatty liver disease. J. Gastroenterol. 2013, 48, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Reddy, J.K.; Rao, M.S. Lipid metabolism and liver inflammation. II. Fatty liver disease and fatty acid oxidation. Am. J. Physiol. Gastrointest. Liver Physiol. 2006, 290, G852–G858. [Google Scholar] [CrossRef] [PubMed]
- Horton, J.D.; Goldstein, J.L.; Brown, M.S. SREBPs: Activators of the complete program of cholesterol and fatty acid synthesis in the liver. J. Clin. Investig. 2002, 109, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.H.; Byrne, C.D. Modulation of sterol regulatory element binding proteins (SREBPs) as potential treatments for non-alcoholic fatty liver disease (NAFLD). Drug Discov. Today 2007, 12, 740–747. [Google Scholar] [CrossRef] [PubMed]
- Ota, T.; Takamura, T.; Kurita, S.; Matsuzawa, N.; Kita, Y.; Uno, M.; Akahori, H.; Misu, H.; Sakurai, M.; Zen, Y.; et al. Insulin resistance accelerates a dietary rat model of nonalcoholic steatohepatitis. Gastroenterology 2007, 132, 282–293. [Google Scholar] [CrossRef] [PubMed]
- Koonen, D.P.; Jacobs, R.L.; Febbraio, M.; Young, M.E.; Soltys, C.L.; Ong, H.; Vance, D.E.; Dyck, J.R. Increased hepatic CD36 expression contributes to dyslipidemia associated with diet-induced obesity. Diabetes 2007, 56, 2863–2871. [Google Scholar] [CrossRef] [PubMed]
- Mao, J.; DeMayo, F.J.; Li, H.; Abu-Elheiga, L.; Gu, Z.; Shaikenov, T.E.; Kordari, P.; Chirala, S.S.; Heird, W.C.; Wakil, S.J. Liver-specific deletion of acetyl-CoA carboxylase 1 reduces hepatic triglyceride accumulation without affecting glucose homeostasis. Proc. Natl. Acad. Sci. USA 2006, 103, 8552–8557. [Google Scholar] [CrossRef] [PubMed]
- Henin, N.; Vincent, M.F.; Gruber, H.E.; Van den Berghe, G. Inhibition of fatty acid and cholesterol synthesis by stimulation of AMP-activated protein kinase. FASEB J. 1995, 9, 541–546. [Google Scholar] [PubMed]
- Ruderman, N.B.; Carling, D.; Prentki, M.; Cacicedo, J.M. AMPK, insulin resistance, and the metabolic syndrome. J. Clin. Investig. 2013, 123, 2764–2772. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.S.; Cho, H.C.; Lee, J.H.; Oh, G.T.; Koo, S.H.; Park, B.H.; Lee, I.K.; Choi, H.S.; Song, D.K.; Im, S.S. Metformin stimulates IGFBP-2 gene expression through PPARalpha in diabetic states. Sci. Rep. 2016, 6, 23665. [Google Scholar] [CrossRef] [PubMed]
- Bruce, C.R.; Hoy, A.J.; Turner, N.; Watt, M.J.; Allen, T.L.; Carpenter, K.; Cooney, G.J.; Febbraio, M.A.; Kraegen, E.W. Overexpression of carnitine palmitoyltransferase-1 in skeletal muscle is sufficient to enhance fatty acid oxidation and improve high-fat diet-induced insulin resistance. Diabetes 2009, 58, 550–558. [Google Scholar] [CrossRef] [PubMed]
- Musso, G.; Gambino, R.; Cassader, M. Emerging molecular targets for the treatment of nonalcoholic fatty liver disease. Annu. Rev. Med. 2010, 61, 375–392. [Google Scholar] [CrossRef] [PubMed]
| Gene | Primers | Sequence (5′ to 3′) |
|---|---|---|
| SREBP-1c | Forward | TGCATTTTCTGACACGCTTC |
| Reverse | CCAAGCTGTACAGGCTCTCC | |
| FAS | Forward | CCCCTGATGAAGAAGGATCA |
| Reverse | ACTCCACAGGTGGGAACAAG | |
| SCD-1 | Forward | TTGGAGAAGCGGTGGATAAC |
| Reverse | AAAAATCCCACCCAATCACA | |
| CD36 | Forward | TGGAACAGAGGCTGACAACT |
| Reverse | TTGATTTTTGATAGATATGGG | |
| PPAR-α | Forward | ACGATTCGACTCAAGCTGGT |
| Reverse | GTTGTGTGACATCCCGACAG | |
| CPT-1 | Forward | CCT CCG TAG CTG ACT CGG TA |
| Reverse | GGA GTG ACC GTG AAC TGA AA | |
| β-actin | Forward | CTCTTCCAGCCTTCCTTCCT |
| Reverse | AGCACTGTGTTGGCGTACAG |
| Con | HFD | LJE 100 | LJE 200 | |
|---|---|---|---|---|
| TC (mg/dL) | 165.63 ± 10.50 | 232.50 ± 18.10 ### | 188.33 ± 27.87 ** | 179.29 ± 23.88 *** |
| LDL-C (mg/dL) | 20.44 ± 1.24 | 25.93 ± 3.60 ## | 22.58 ± 2.35 * | 19.08 ± 2.85 *** |
| TG (mg/dL) | 114.17 ± 10.21 | 113.33 ± 15.71 | 116.25 ± 9.16 | 107.50 ± 9.64 |
| AST (IU/L) | 113.00 ± 34.21 | 155.00 ± 39.79 | 120.00 ± 32.79 | 95.63 ± 26.92 * |
| ALT (IU/L) | 81.43 ± 26.73 | 215.00 ± 40.74 ### | 106.43 ± 47.58 ** | 92.86 ± 40.50 *** |
| LDH (IU/L) | 570.00 ± 182.30 | 872.86 ± 113.94 ## | 628.75 ± 171.85 * | 524.29 ± 120.33 ** |
| MDA (μM) | 1.05 ± 0.26 | 1.91 ± 0.25 ### | 1.30 ± 0.36 * | 1.10 ± 0.53 ** |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, M.-R.; Park, K.I.; Ma, J.Y. Leonurus japonicus Houtt Attenuates Nonalcoholic Fatty Liver Disease in Free Fatty Acid-Induced HepG2 Cells and Mice Fed a High-Fat Diet. Nutrients 2018, 10, 20. https://doi.org/10.3390/nu10010020
Lee M-R, Park KI, Ma JY. Leonurus japonicus Houtt Attenuates Nonalcoholic Fatty Liver Disease in Free Fatty Acid-Induced HepG2 Cells and Mice Fed a High-Fat Diet. Nutrients. 2018; 10(1):20. https://doi.org/10.3390/nu10010020
Chicago/Turabian StyleLee, Mi-Ra, Kwang Il Park, and Jin Yeul Ma. 2018. "Leonurus japonicus Houtt Attenuates Nonalcoholic Fatty Liver Disease in Free Fatty Acid-Induced HepG2 Cells and Mice Fed a High-Fat Diet" Nutrients 10, no. 1: 20. https://doi.org/10.3390/nu10010020