Relative Validity of a 24-h Recall in Assessing Intake of Key Nutrients in a Cohort of Australian Toddlers
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Australian Institute of Health and Welfare. 2010 Australian National Infant Feeding Survey: Indicator Results; Australian Institute of Health and Welfare (AIHW): Canberra, Australia, 2011.
- Australian Bureau of Statistics. Australian Health Survey: Nutrition First Results—Food and Nutrients, 2011–2012; Australian Bureau of Statistics (ABS): Canberra, Australia, 2014.
- Nicklaus, S. Children’s acceptance of new foods at weaning. Role of practices of weaning and of food sensory properties. Appetite 2011, 57, 812–815. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.; Magarey, A.; Daniels, L. Food and beverage intake in Australian children aged 12–16 months participating in the NOURISH and SAIDI studies. Aust. N. Z. J. Public Health 2014, 38, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.; Magarey, A.M.; Daniels, L.A. Maternal Feeding Practices and Feeding Behaviors of Australian Children Aged 12–36 Months. Matern. Child Health J. 2010, 15, 1363–1371. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lioret, S.; McNaughton, S.A.; Spence, A.C.; Crawford, D.; Campbell, K.J. Tracking of dietary intakes in early childhood: The Melbourne InFANT Program. Eur. J. Clin. Nutr. 2013, 67, 275–281. [Google Scholar] [CrossRef] [PubMed]
- Lennox, A.; Sommerville, J.; Ong, K.; Henderson, H.; Allen, R. Diet and Nutrition Survey of Infants and Young Children, 2011; Department of Health and Food Standards Agency: Britain, UK, 2013.
- Watson, E.O.; Heath, A.-L.M.; Taylor, R.W.; Mills, V.C.; Barris, A.C.; Skidmore, P.M. Relative validity and reproducibility of an FFQ to determine nutrient intakes of New Zealand toddlers aged 12–24 months. Public Health Nutr. 2015, 18, 3265–3271. [Google Scholar] [CrossRef] [PubMed]
- Webb, K.; Rutishauser, I.; Knezevic, N. Foods, nutrients and portions consumed by a sample of Australian children aged 16–24 months. Nutr. Diet. 2008, 65, 56–65. [Google Scholar] [CrossRef]
- Lombard, M.J.; Steyn, N.P.; Charlton, K.E.; Senekal, M. Application and interpretation of multiple statistical tests to evaluate validity of dietary intake assessment methods. Nutr. J. 2015, 14, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Emmett, P.M.; Jones, L.R. Diet and growth in infancy: Relationship to socioeconomic background and to health and development in the Avon Longitudinal Study of Parents and Children. Nutr. Rev. 2014, 72, 483–506. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, P.; Briefel, R.; Clusen, N.; Devaney, B. Feeding Infants and Toddlers Study (FITS): Development of the FITS Survey in Comparison to Other Dietary Survey Methods. J. Am. Diet. Assoc. 2006, 106, 12.e11–12.e50. [Google Scholar] [CrossRef] [PubMed]
- Amezdroz, E.; Carpenter, L.; O’Callaghan, E.; Johnson, S.; Waters, E. Transition from milks to the introduction of solid foods across the first 2 years of life: Findings from an Australian birth cohort study. J. Hum. Nutr. Diet. 2015, 28, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.; Hesketh, K.; Crawford, D.; Salmon, J.; Ball, K.; McCallum, Z. The Infant Feeding Activity and Nutrition Trial (INFANT) an early intervention to prevent childhood obesity: Cluster-randomised controlled trial. BMC Public Health 2008, 8, 103. [Google Scholar] [CrossRef] [PubMed]
- Daniels, L.A.; Magarey, A.; Battistutta, D.; Nicholson, J.M.; Farrell, A.; Davidson, G.; Cleghorn, G. The NOURISH randomised control trial: Positive feeding practices and food preferences in early childhood—A primary prevention program for childhood obesity. BMC Public Health 2009, 9, 387. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rutishauser, I.H.E. Dietary intake measurements. Public Health Nutr. 2005, 8, 1100–1107. [Google Scholar] [CrossRef] [PubMed]
- Thompson, F.E.; Subar, A.F. Dietary Assessment Methodology. In Nutrition in the Prevention and Treatment of Disease, 3rd ed.; Coulston, A., Boushey, C.J., Ferruzzi, M.G., Eds.; Academic Press: London, UK, 2013; pp. 5–46. [Google Scholar]
- Bel-Serrat, S.; Mouratidou, T.; Pala, V.; Huybrechts, I.; Börnhorst, C.; Fernández-Alvira, J.M.; Hadjigeorgiou, C.; Eiben, G.; Hebestreit, A.; Lissner, L.; et al. Relative validity of the Children’s Eating Habits Questionnaire-food frequency section among young European children: The IDEFICS Study. Public Health Nutr. 2014, 17, 266–276. [Google Scholar] [CrossRef] [PubMed]
- Vereecken, C.; Covents, M.; Maes, L. Comparison of a food frequency questionnaire with an online dietary assessment tool for assessing preschool children’s dietary intake. J. Hum. Nutr. Diet. 2010, 23, 502–510. [Google Scholar] [CrossRef] [PubMed]
- Cheng, G.; Hilbig, A.; Drossard, C.; Alexy, U.; Kersting, M. Relative validity of a 3 d estimated food record in German toddlers. Public Health Nutr. 2013, 16, 645–652. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.O.; Butte, N.F.; Mendoza, P.M.; Wilson, T.A.; Hodges, E.A.; Reidy, K.C.; Deming, D. Overestimation of infant and toddler energy intake by 24-h recall compared with weighed food records. Am. J. Clin. Nutr. 2008, 88, 407–415. [Google Scholar] [PubMed]
- Huybrechts, I.; De Backer, G.; De Bacquer, D.; Maes, L.; De Henauw, S. Relative Validity and Reproducibility of a Food-Frequency Questionnaire for Estimating Food Intakes among Flemish Preschoolers. Int. J. Environ. Res. Public Health 2009, 6, 382–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marriott, L.D.; Inskip, H.M.; Borland, S.E.; Godfrey, K.M.; Law, C.M.; Robinson, S.M. What do babies eat? Evaluation of a food frequency questionnaire to assess the diets of infants aged 12 months. Public Health Nutr. 2009, 12, 967–972. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.; Bingham, S. Assessment of food consumption and nutrient intake. In Design Concepts in Nutritional Epidemiology, 2nd ed.; Margetts, B.M., Nelson, M., Eds.; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Erkkola, M.; Kyttälä, P.; Takkinen, H.-M.; Kronberg-Kippilä, C.; Nevalainen, J.; Simell, O.; Ilonen, J.; Veijola, R.; Knip, M.; Virtanen, S.M. Nutrient intake variability and number of days needed to assess intake in preschool children. Br. J. Nutr. 2011, 106, 130–140. [Google Scholar] [CrossRef] [PubMed]
- Lanigan, J.A.; Wells, J.C.K.; Lawson, M.S.; Cole, T.J.; Lucas, A. Number of days needed to assess energy and nutrient intake in infants and young children between 6 months and 2 years of age. Eur. J. Clin. Nutr. 2004, 58, 745. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Australian Health Survey: Users’ Guide, 2011–2013; Cat. No. 4363.0.55.001; Australian Bureau of Statistics (ABS): Canberra, Australia, 2014.
- Food Standards Australia New Zealand. AUSNUT 2011–2013—Australian Food Composition Database. Available online: http://www.foodstandards.gov.au/science/monitoringnutrients/ausnut/foodnutrient/Pages/default.aspx (accessed on 10 February 2017).
- National Health and Medical Research Council and Ministry of Health. Nutrient Reference Values for Australia and New Zealand; National Health and Medical Research Council (NHMRC): Canberra, Australia, 2006.
- Scott, J.; Davey, K.; Ahwong, E.; Devenish, G.; Ha, D.; Do, L. A Comparison by Milk Feeding Method of the Nutrient Intake of a Cohort of Australian Toddlers. Nutrients 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Bland, M.J.; Altman, D.G. Statistical Methods for Assessing Agreement between Two Methods of Clinical Measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Watson, J.F.; Collins, C.E.; Sibbritt, D.W.; Dibley, M.J.; Garg, M.L. Reproducibility and comparative validity of a food frequency questionnaire for Australian children and adolescents. Int. J. Behav. Nutr. Phys. Act. 2009, 6, 62. [Google Scholar] [CrossRef] [PubMed]
- Magarey, A.; Golley, R.; Spurrier, N.; Goodwin, E.; Ong, F. Reliability and validity of the Children’s Dietary Questionnaire: A new tool to measure children’s dietary patterns. Int. J. Pediatr. Obes. 2009, 4, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Dietary Assessment Primer. Available online: https://dietassessmentprimer.cancer.gov/learn/distribution.html (accessed on 18 October 2016).
- Barrett, J.S.; Gibson, P.R. Development and Validation of a Comprehensive Semi-Quantitative Food Frequency Questionnaire that Includes FODMAP Intake and Glycemic Index. J. Am. Diet. Assoc. 2010, 110, 1469–1476. [Google Scholar] [CrossRef] [PubMed]
- Do, L.; Scott, J.; Thomson, W.; Stamm, J.; Rugg-Gunn, A.; Levy, S.; Wong, C.; Devenish, G.; Ha, D.; Spencer, A. Common risk factor approach to address socioeconomic inequality in the oral health of preschool children—A prospective cohort study. BMC Public Health 2014, 14, 429. [Google Scholar] [CrossRef] [PubMed]
- Mejía-Rodríguez, F.; Neufeld, L.M.; García-Guerra, A.; Quezada-Sanchez, A.D.; Orjuela, M.A. Validation of a Food Frequency Questionnaire for Retrospective Estimation of Diet During the First 2 Years of Life. Matern. Child Health J. 2014, 18, 268–285. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.; Black, A.E.; Morris, J.A.; Cole, T.J. Between- and within-subject variation in nutrient intake from infancy to old age: Estimating the number of days required to rank dietary intakes with desired precision. Am. J. Clin. Nutr. 1989, 50, 155–167. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Dietary Reference Intakes: Applications in Dietary Assessment; National Academy Press: Washington, DC, USA, 2000. Available online: https://www.nap.edu/catalog/9956/dietary-reference-intakes-applications-in-dietary-assessment (accessed on 31 December 2017).
| 24HR | 24HR + 2DFR | Difference 1 | ||||||
|---|---|---|---|---|---|---|---|---|
| Nutrient | Mean (±SD) | Median | Skewness | Mean (±SD) | Median | Skewness | Mean (±SD) | p2 |
| Energy (kJ) | 3849 (928) | 3793 | 0.461 | 3783 (701) | 3827 | −0.174 | 65.6 (656.1) | 0.008 |
| Protein (g) | 36.8 (13.5) | 35.5 | 0.586 | 36.3 (10.8) | 35.6 | 0.223 | 0.6 (8.4) | 0.078 |
| Calcium (mg) | 665.9 (282.1) | 627.8 | 0.528 | 662.1 (247.2) | 651.9 | 0.214 | 3.78 (138.8) | 0.471 |
| Iron (mg) | 6.9 (3.7) | 6.5 | 1.398 | 6.7 (3.3) | 6.0 | 1.096 | 0.22 (1.88) | 0.002 |
| Iron (mg) 3 | 0.01 (0.29) | 0.257 | ||||||
| Added sugars (g) | 4.5 (6.8) | 2.0 | 3.095 | 4.5 (5.2) | 2.6 | 2.431 | −0.003 (4.77) | 0.987 |
| Added sugars (g) 3 | −0.18 (0.69) | <0.001 | ||||||
| Nutrient | 24HR vs. 24HR + 2DFR | |
|---|---|---|
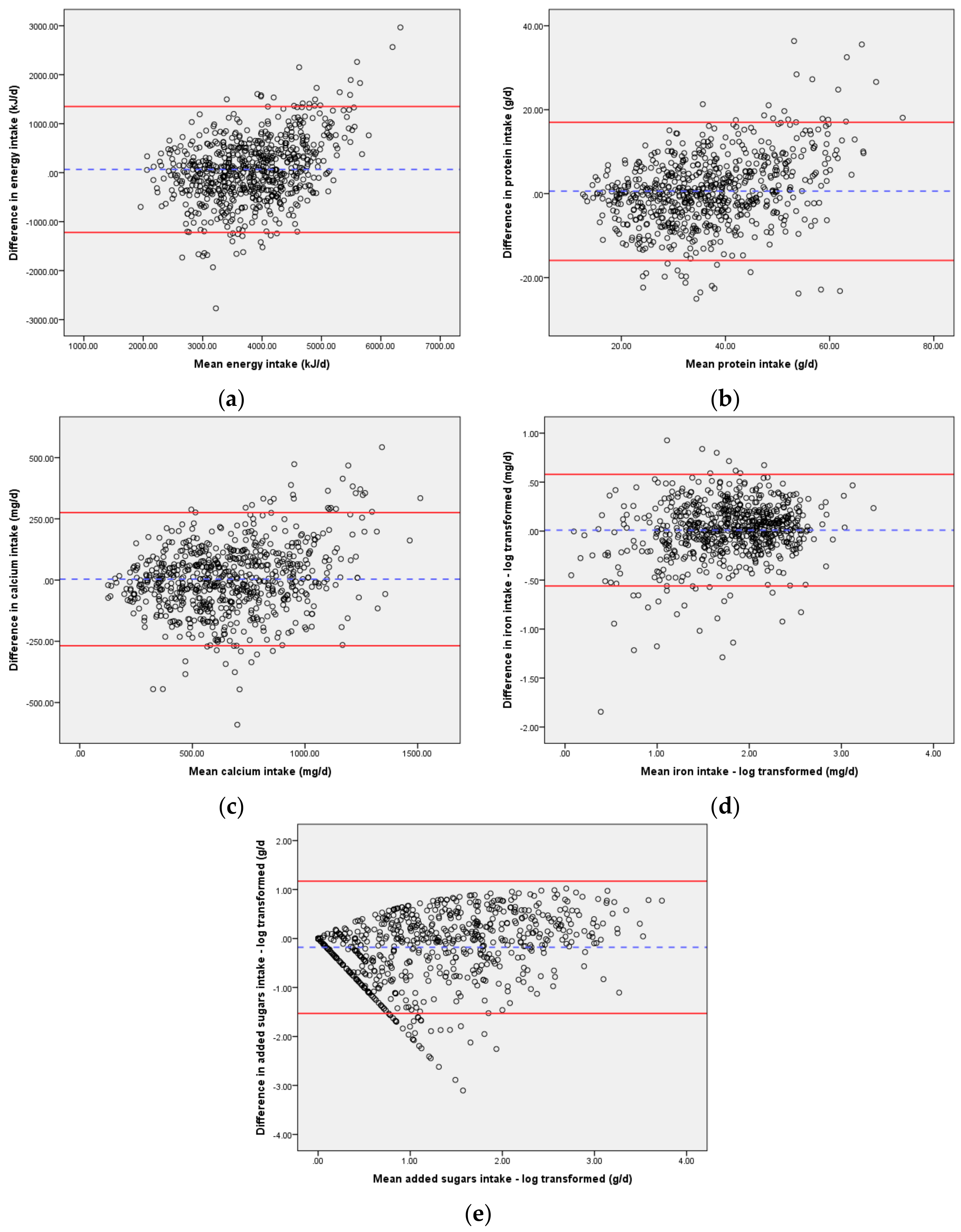
| Mean Difference 1 (95% LOA) | Slope of Bias 2 | |
| Energy (kJ) | 65.6 (−1220.4, 1351.7) | 0.326 |
| Protein (g) | 0.6 (−15.9, 17.0) | 0.259 |
| Calcium (mg) | 3.8 (−268.3, 275.8) | 0.141 |
| Iron (mg) 3 | 0.01 (−0.56, 0.58) | 0.100 |
| Added sugars (g) 3 | −0.18 (−1.53, 1.17) | 0.209 |
| 24HR vs. 24HR + 2DFR | |||
|---|---|---|---|
| Nutrient | % Correctly Classified 1 | % Grossly Misclassified 2 | κ |
| Energy (kJ) | 60.8 | 2.6 | 0.412 |
| Protein (g) | 67.8 | 2.7 | 0.517 |
| Calcium (mg) | 70.8 | 0.6 | 0.562 |
| Iron (mg) 3 | 77.3 | 1.0 | 0.659 |
| Added sugars (g) 3 | 57.9 | 3.6 | 0.369 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beaton, E.; Wright, J.; Devenish, G.; Do, L.; Scott, J. Relative Validity of a 24-h Recall in Assessing Intake of Key Nutrients in a Cohort of Australian Toddlers. Nutrients 2018, 10, 80. https://doi.org/10.3390/nu10010080
Beaton E, Wright J, Devenish G, Do L, Scott J. Relative Validity of a 24-h Recall in Assessing Intake of Key Nutrients in a Cohort of Australian Toddlers. Nutrients. 2018; 10(1):80. https://doi.org/10.3390/nu10010080
Chicago/Turabian StyleBeaton, Elizabeth, Janine Wright, Gemma Devenish, Loc Do, and Jane Scott. 2018. "Relative Validity of a 24-h Recall in Assessing Intake of Key Nutrients in a Cohort of Australian Toddlers" Nutrients 10, no. 1: 80. https://doi.org/10.3390/nu10010080






