The Postprandial Anti-Hyperglycemic Effect of Pyridoxine and Its Derivatives Using In Vitro and In Vivo Animal Models
Abstract
:1. Introduction
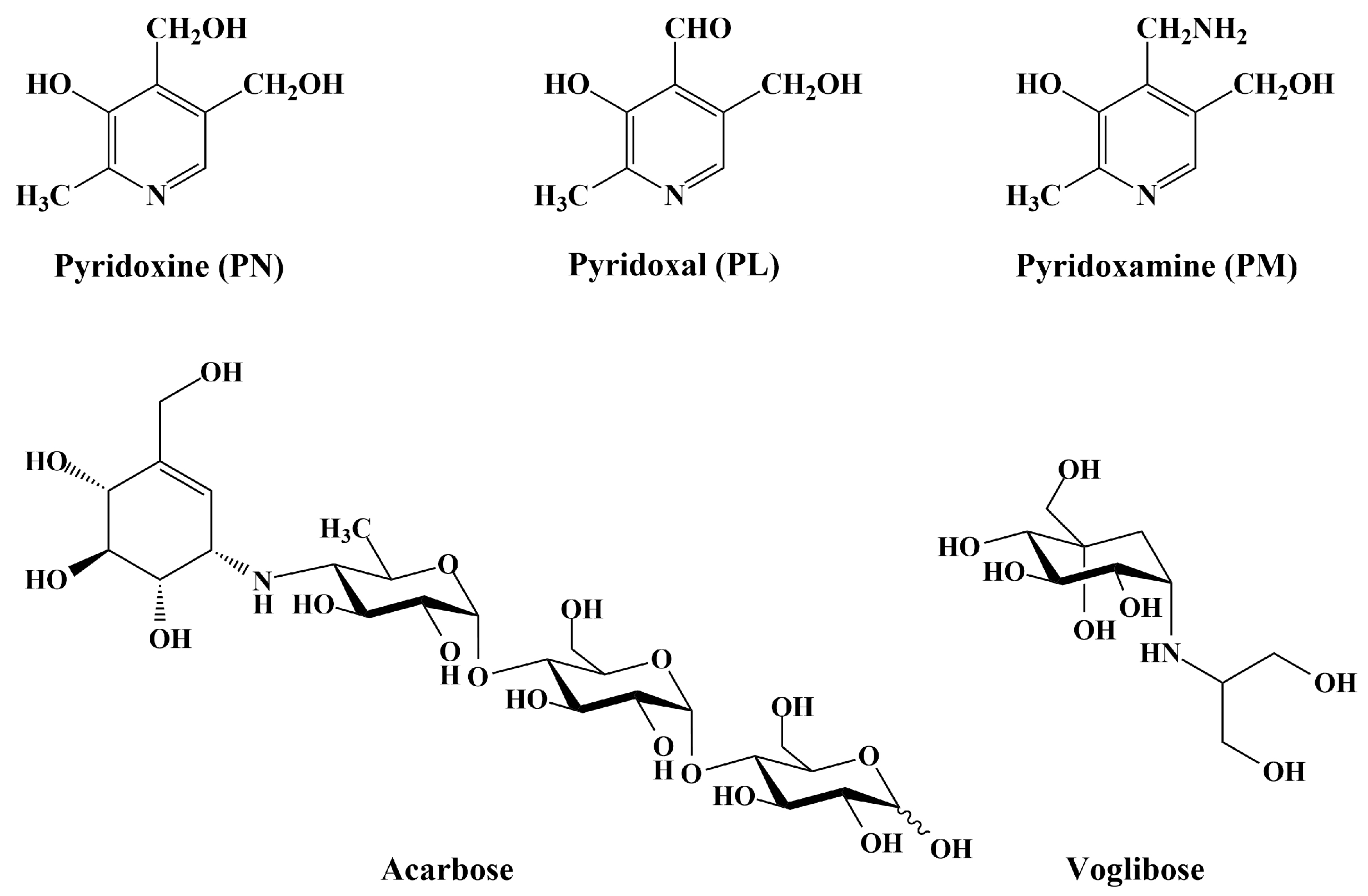
2. Materials and Methods
2.1. Materials
2.2. Carbohydrate-Hydrolyzing Enzyme Inhibition Assay
2.2.1. Rat Intestinal α-Glucosidase Inhibition Assay
2.2.2. Porcine Pancreatic α-Amlyase Inhibition Assay
2.2.3. Maltase, Sucrase, and Glucoamylase Inhibition Assay
2.3. The Sucrose/Starch Loading Test
2.4. Statistical Analysis
3. Results
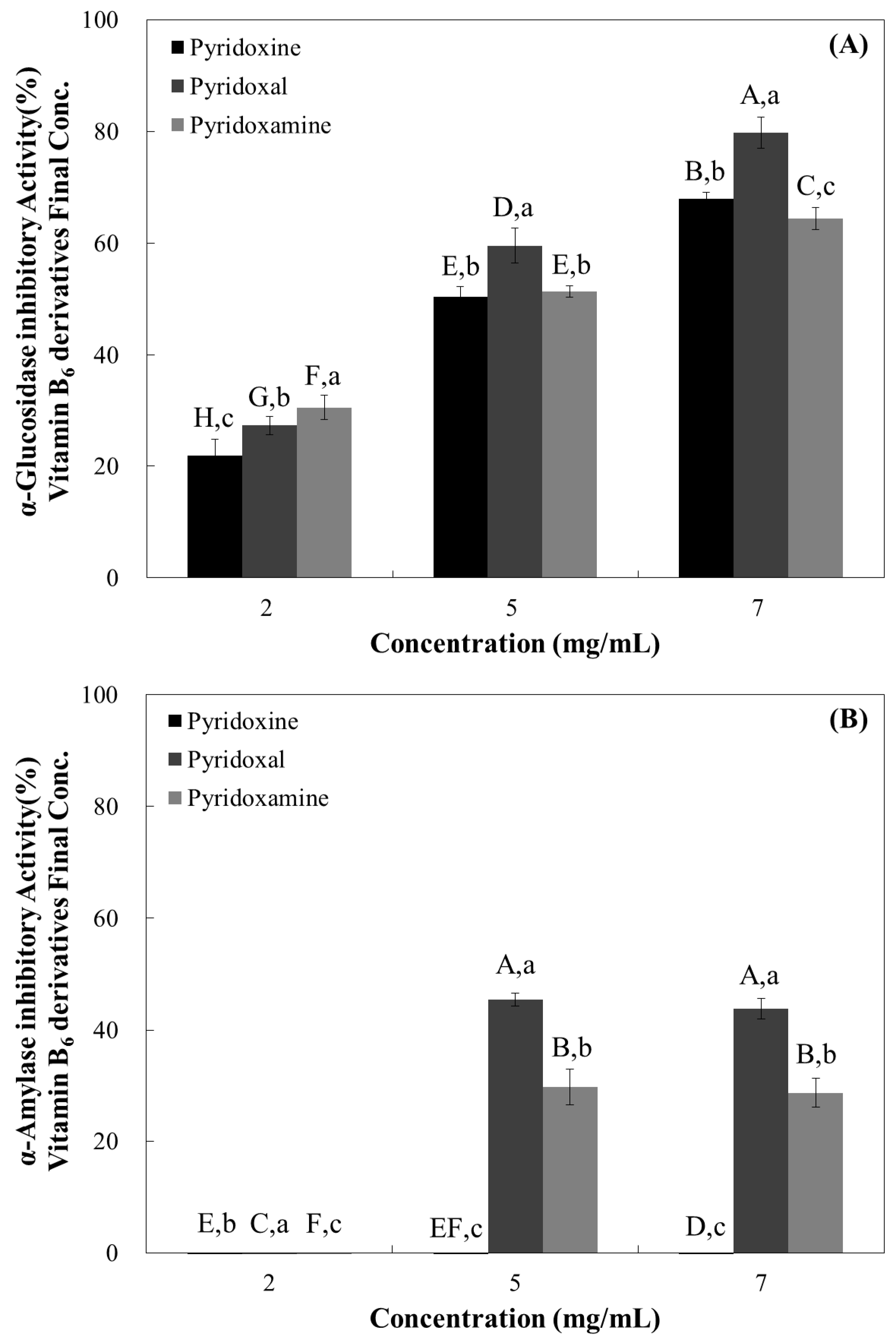
3.1. Rat Intestinal α-Glucosidase Inhibitory Activity of Water-Soluble Vitamins
3.2. Porcine Pancreatic α-Amlyase Inhibition Assay
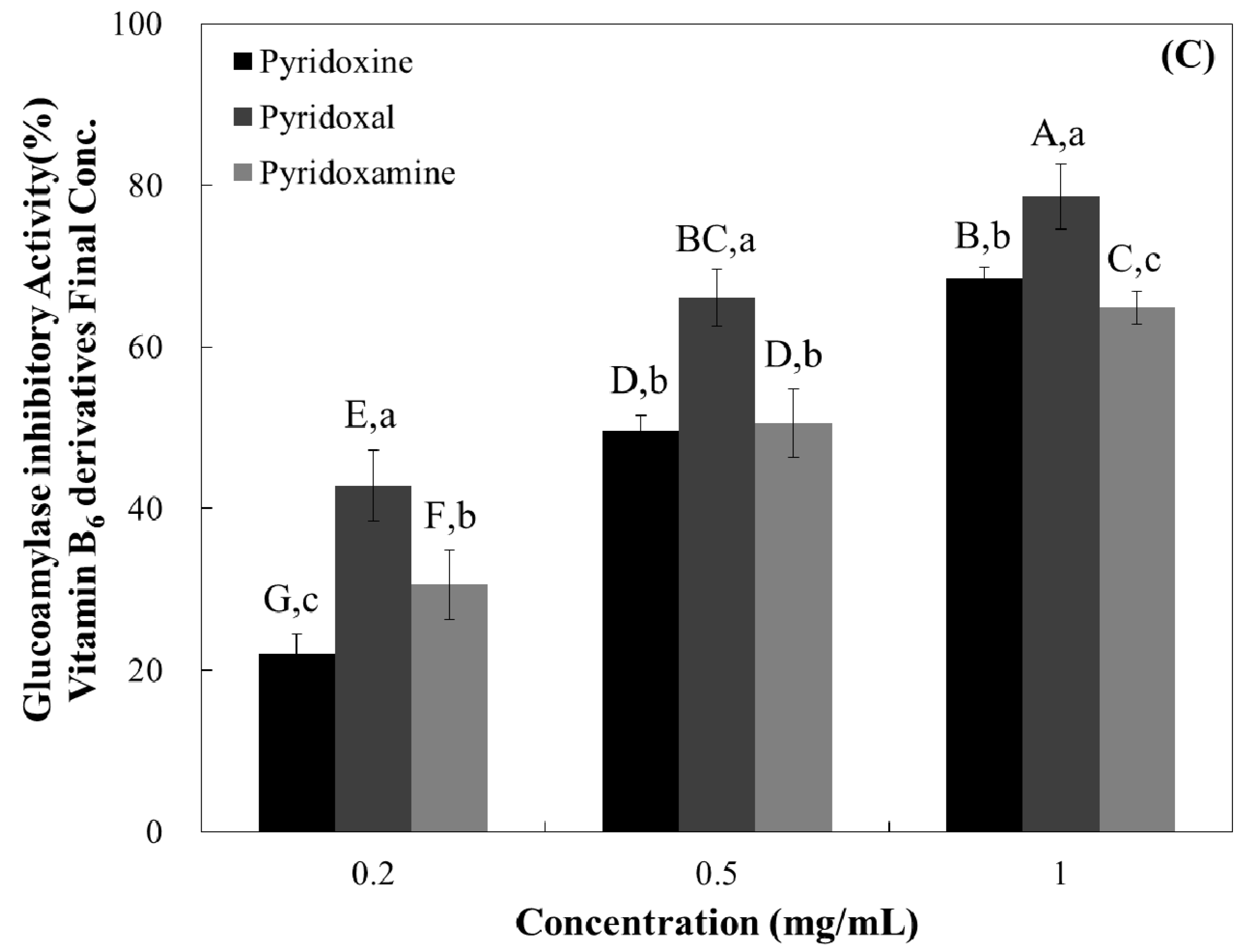
3.3. Maltase, Sucrase, and Glucoamylase Inhibition Assay
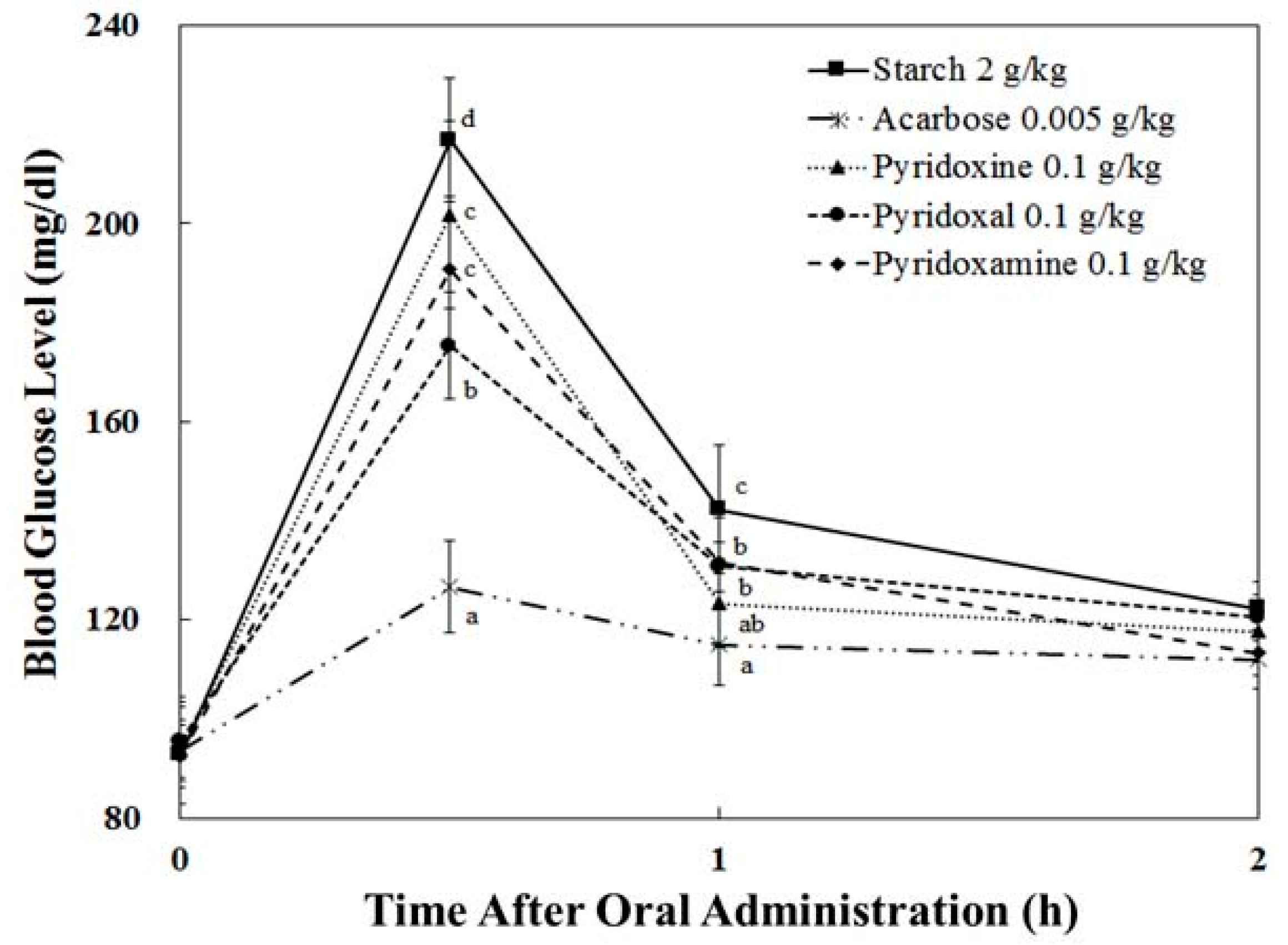
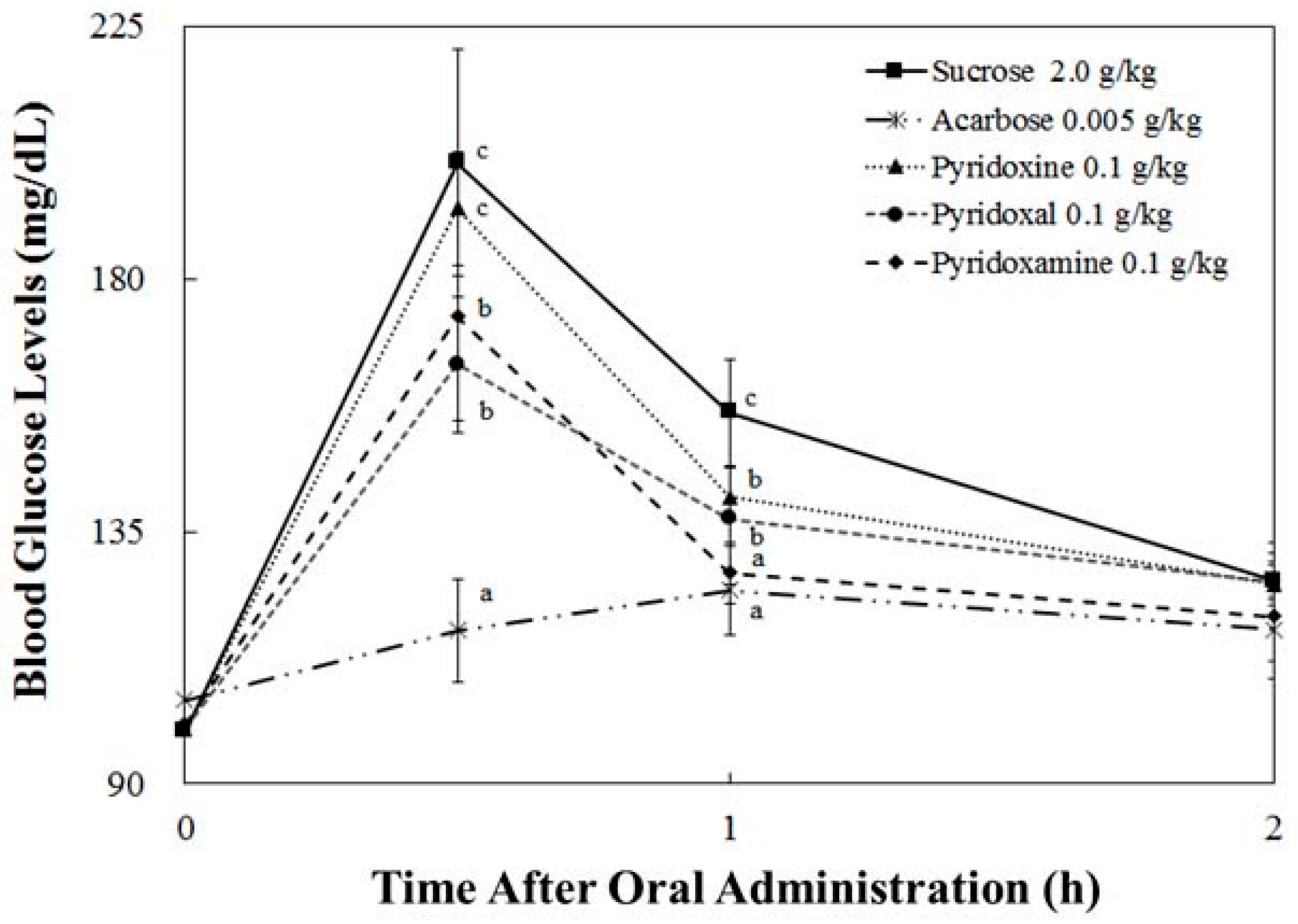
3.4. Starch/Sucrose Loading Test
3.5. Pharmacodynamics Parameters
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Apostolidis, E.; Li, L.; Kang, B.H.; Lee, C.M.; Seeram, N.P. Seasonal influence on phenolic-mediated antihyperglycemic properties of Canadian sugar and red maple leaves using in vitro assay models. Food Sci. Biotechnol. 2012, 21, 753–760. [Google Scholar] [CrossRef]
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2012, 35, S64–S71. [Google Scholar]
- Wild, S.; Roglic, G.; Green, A.; Sicree, R.; King, H. Global prevalence of diabetes: Estimates for the year 2000 and projections for 2030. Diabetes Care 2004, 27, 1047–1053. [Google Scholar] [CrossRef] [PubMed]
- Boyle, J.P.; Thompson, T.J.; Gregg, E.W.; Barker, L.E.; Williamson, D.F. Projection of the year 2050 burden of diabetes in the US adult population: Dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul. Health Metr. 2010, 8, 29. [Google Scholar] [CrossRef] [PubMed]
- Jo, S.H.; Ka, E.H.; Lee, H.S.; Apostolidis, E.; Jang, H.D.; Kwon, Y.I. Comparison of antioxidant potential and rat intestinal α-glucosidases inhibitory activities of quercetin, rutin, and isoquercetin. Int. J. Appl. Res. Nat. Prod. 2009, 2, 52–60. [Google Scholar]
- Tucci, S.A.; Boyland, E.J.; Halford, J.C. The role of lipid and carbohydrate digestive enzyme inhibitors in the management of obesity: A review of current and emerging therapeutic agents. Diabetes Metab. Syndr. Obes. 2010, 10, 125–143. [Google Scholar] [CrossRef]
- Subramanian, R.; Asmawi, M.Z.; Sadikun, A. In vitro α-glucosidase and α-amylase enzyme inhibitory effects of Andrographis paniculata extract and andrographolide. Acta Biochim. Pol. 2008, 55, 391–398. [Google Scholar] [PubMed]
- Gromova, O.A.; Torshin, I.Y.; Nazarenko, A.G.; Kalachev, A.G. Deficiency of magnesium and pyridoxine as a risk factors for coronary heart disease. Kardiologiia 2016, 56, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Friso, S.; Jacques, P.F.; Wilson, P.W.; Rosenberg, I.H.; Selhub, J. Low circulating vitamin B6 is associated with elevation of the inflammation marker C-reactive protein independently of plasma homocysteine levels. Circulation 2001, 103, 2788–2791. [Google Scholar] [CrossRef] [PubMed]
- Robinson, K.; Arheart, K.; Refsum, H.; Brattström, L.; Boers, G.; Ueland, P.; Rubba, P.; Palma-Reis, R.; Meleady, R.; Daly, L.; et al. Low circulating folate and vitamin B6 concentrations: risk factors for stroke, peripheral vascular disease, and coronary artery disease. European COMAC Group. Circulation 1998, 97, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Nix, W.A.; Zirwes, R.; Bangert, V.; Kaiser, R.P.; Schilling, M.; Hostalek, U.; Obeid, R. Vitamin B status in patients with type 2 diabetes mellitus with and without incipient nephropathy. Diabetes Res. Clin. Pract. 2015, 107, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Odum, E.P.; Wakwe, V.C. Plasma concentrations of water-soluble vitamins in metabolic syndrome subjects. Niger. J. Clin. Pract. 2012, 15, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.S.; Picciano, M.F.; Jacques, P.F.; Selhub, J. Plasma pyridoxal 5-phosphate in the US population: the National Health and Nutrition Examination Survey, 2003–2004. Am. J. Clin. Nutr. 2008, 87, 1446–1454. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.K.; Lim, G. Pyridoxine and pyridoxamine inhibits superoxide radicals and prevents lipid peroxidation, protein glycosylation, and (Na+ + K+)-ATPase activity reduction in high glucose-treated human erythrocytes. Free Radic. Biol. Med. 2001, 30, 232–237. [Google Scholar] [CrossRef]
- Levin, E.R.; Hanscom, T.A.; Fisher, M.; Lauvstad, W.A.; Lui, A.; Ryan, A.; Glockner, D.; Levin, S.R. The influence of pyridoxine in diabetic peripheral neuropathy. Diabetes Care 1981, 4, 606–609. [Google Scholar] [CrossRef] [PubMed]
- Nair, A.R.; Biju, M.P.; Paulose, C.S. Effect of pyridoxine and insulin administration on brain glutamate dehydrogenase activity and blood glucose control in streptozotocin-induced diabetic rats. Biochim. Biophys. Acta 1998, 1381, 351–354. [Google Scholar] [CrossRef]
- Solomon, L.R.; Cohen, K. Erythrocyte O2 transport and metabolism and effects of vitamin B6 therapy in type II diabetes mellitus. Diabetes 1989, 38, 881–886. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.; Shahab, U.; Baig, M.H.; Khan, M.S.; Khan, M.S.; Srivastava, A.K.; Saeed, M.; Moinuddin. Inhibitory effect of metformin and pyridoxamine in the formation of early, intermediate and advanced glycation end-products. PLoS ONE 2013, 8, e72128. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.I.; Apostolidis, E.; Kim, Y.C.; Shetty, K. Health benefits of traditional corn, beans, and pumpkin: in vitro studies for hyperglycemia and hypertension management. J. Med. Food 2007, 10, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.I.; Vattem, D.A.; Shetty, K. Evaluation of clonal herbs of Lamiaceae species for management of diabetes and hypertension. Asia Pac. J. Clin. Nutr. 2006, 15, 107–118. [Google Scholar] [PubMed]
- Dahlqvist, A. Method for assay of intestinal disaccharidases. Anal. Biochem. 1964, 7, 18–25. [Google Scholar] [CrossRef]
- Bergmeyer, H.U.; Bernt, E. Determination of Glucose with Glucose Oxidase and Peroxidase. In Methods of Enzymatic Analysis, 2nd ed.; Academic Press: New York, NY, USA, 1974; pp. 1205–1215. ISBN 978–0-12-091302-2. [Google Scholar]
- Middleton, H.M. In vivo absorption and phosphorylation of pyridoxine-HCl in rat jejunum. Gastroenterology 1979, 76, 43–49. [Google Scholar] [PubMed]
- Kim, S.H.; Jo, S.H.; Kwon, Y.I.; Hwang, J.K. Effects of onion (Allium cepa L.) extract administration on intestinal α-glucosidases activities and spikes in postprandial blood glucose levels in SD rats model. Int. J. Mol. Sci. 2011, 12, 3757–3769. [Google Scholar] [CrossRef] [PubMed]

| IC50 (mg/mL) | |||||
|---|---|---|---|---|---|
| Rat intestinal α-Glucosidase | Porcine Pancreatic α-Amylase | Rat Intestinal SUCRASE | Rat Intestinal Maltase | Rat Intestinal Glucoamylase | |
| Pyridoxine | 5.02 ± 0.05 a | 23.17 ± 0.29 a | 0.32 ± 0.03 a | 0.87 ± 0.08 a | 0.63 ± 0.04 a |
| Pyridoxal | 4.15 ± 0.17 b | 12.92 ± 1.22 c | 0.32 ± 0.03 a | 0.37 ± 0.13 b | 0.26 ± 0.08 b |
| Pyridoxamine | 4.85 ± 0.06 a | 14.93 ± 0.96 b | 0.35 ± 0.01 a | 1.08 ± 0.10 a | 0.60 ± 0.06 a |
| Groups | PD Parameters | |||
|---|---|---|---|---|
| Cmax (mg/dL) | Tmax (h) | AUCt (h∙mg/dL) | ||
| BGL (mg/dL) | Starch 2.0 g/kg | 216.92 ± 11.58 d | 0.50 ± 0.00 a | 299.02 ± 12.10 c |
| Acarbose 0.005 g/kg | 126.60 ± 9.44 a | 0.50 ± 0.00 a | 228.88 ± 13.09 a | |
| Pyridoxine 0.1 g/kg | 200.00 ± 20.89 c,d | 0.50 ± 0.00 a | 274.28 ± 15.62 b | |
| Pyridoxal 0.1 g/kg | 172.67 ± 11.45 b | 0.50 ± 0.00 a | 268.27 ± 8.80 b | |
| Pyridoxamine 0.1 g/kg | 191.54 ± 13.70 c | 0.50 ± 0.00 a | 275.10 ± 7.31 b | |
| BGL (mg/dL) | Sucrose 2.0 g/kg | 199.52 ± 22.93 c | 0.50 ± 0.00 a | 303.57 ± 14.71 c |
| Acarbose 0.005 g/kg | 126.92 ± 6.87 a | 0.86 ± 0.24 b | 237.94 ± 8.82 a | |
| Pyridoxine 0.1 g/kg | 192.48 ± 9.03 c | 0.50 ± 0.00 a | 290.64 ± 15.55 c | |
| Pyridoxal 0.1 g/kg | 164.10 ± 10.27 b | 0.50 ± 0.00 a | 272.99 ± 5.96 b | |
| Pyridoxamine 0.1 g/kg | 174.50 ± 18.29 b | 0.50 ± 0.00 a | 269.14 ± 13.40 b | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.H.; Kang, Y.-R.; Lee, J.-Y.; Chang, H.-B.; Lee, K.W.; Apostolidis, E.; Kwon, Y.-I. The Postprandial Anti-Hyperglycemic Effect of Pyridoxine and Its Derivatives Using In Vitro and In Vivo Animal Models. Nutrients 2018, 10, 285. https://doi.org/10.3390/nu10030285
Kim HH, Kang Y-R, Lee J-Y, Chang H-B, Lee KW, Apostolidis E, Kwon Y-I. The Postprandial Anti-Hyperglycemic Effect of Pyridoxine and Its Derivatives Using In Vitro and In Vivo Animal Models. Nutrients. 2018; 10(3):285. https://doi.org/10.3390/nu10030285
Chicago/Turabian StyleKim, Hyuk Hwa, Yu-Ri Kang, Jung-Yun Lee, Hung-Bae Chang, Ki Won Lee, Emmanouil Apostolidis, and Young-In Kwon. 2018. "The Postprandial Anti-Hyperglycemic Effect of Pyridoxine and Its Derivatives Using In Vitro and In Vivo Animal Models" Nutrients 10, no. 3: 285. https://doi.org/10.3390/nu10030285





