Comparison of Growth of Healthy Term Infants Fed Extensively Hydrolyzed Protein- and Amino Acid-Based Infant Formulas
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Design
- is no less than 15 weeks in duration, enrolling infants no more than two weeks old at time of entry into the study;
- includes the collection and maintenance of data on formula intake and anthropometric measures of physical growth, including body weight, recumbent length, head circumference, average daily weight increment, and average daily recumbent length increment;
- includes anthropometric measurements made at the beginning and end of the study, and at least four additional measurements made at intermediate time points with three of the six total measurement made within the first four weeks of the study and three measurements made at approximately four-week intervals over the remaining 11 weeks of the study;
- compares the anthropometric data for the test group to a concurrent control group or groups at each time point and compares the anthropometric data for each infant (body weight for age, body length for age, head circumference for age, and weight for length) in the test group and the control group to the 2009 CDC growth charts, which are incorporated by reference at 106.160; and,
- compares the data on formula intake of the test group with a concurrent control group or groups and a scientifically appropriate reference” [12].
2.2.1. Study Eligibility Criteria
2.3. Study Formulas
2.4. Statistical Methodology
3. Results
3.1. Compilation of Results of EHF and AAF Growth Studies in Healthy Term FF Infants
3.1.1. Extensively Hydrolyzed Protein-Based Infant Formulas
- Mean weight gains from 14 to 112 or 120 days of age ranged from 27.6 to 29.1 g/day for all EHFs except for EHF-C (25.4 g/day) (Table 2). All of the EHFs appeared to support weight gains of infants from 14 to 112 days of age in the range of HM-fed infants reported by Nelson et al. [22] at 27.5 g/day except for infants fed EHF-C that supported mean weight gains of only 25.4 g/day. For EHFs, using unadjusted comparisons, mean weight gain per day for EHF-C was significantly less (p < 0.05) than the mean weight gain per day for each of the other EHFs.
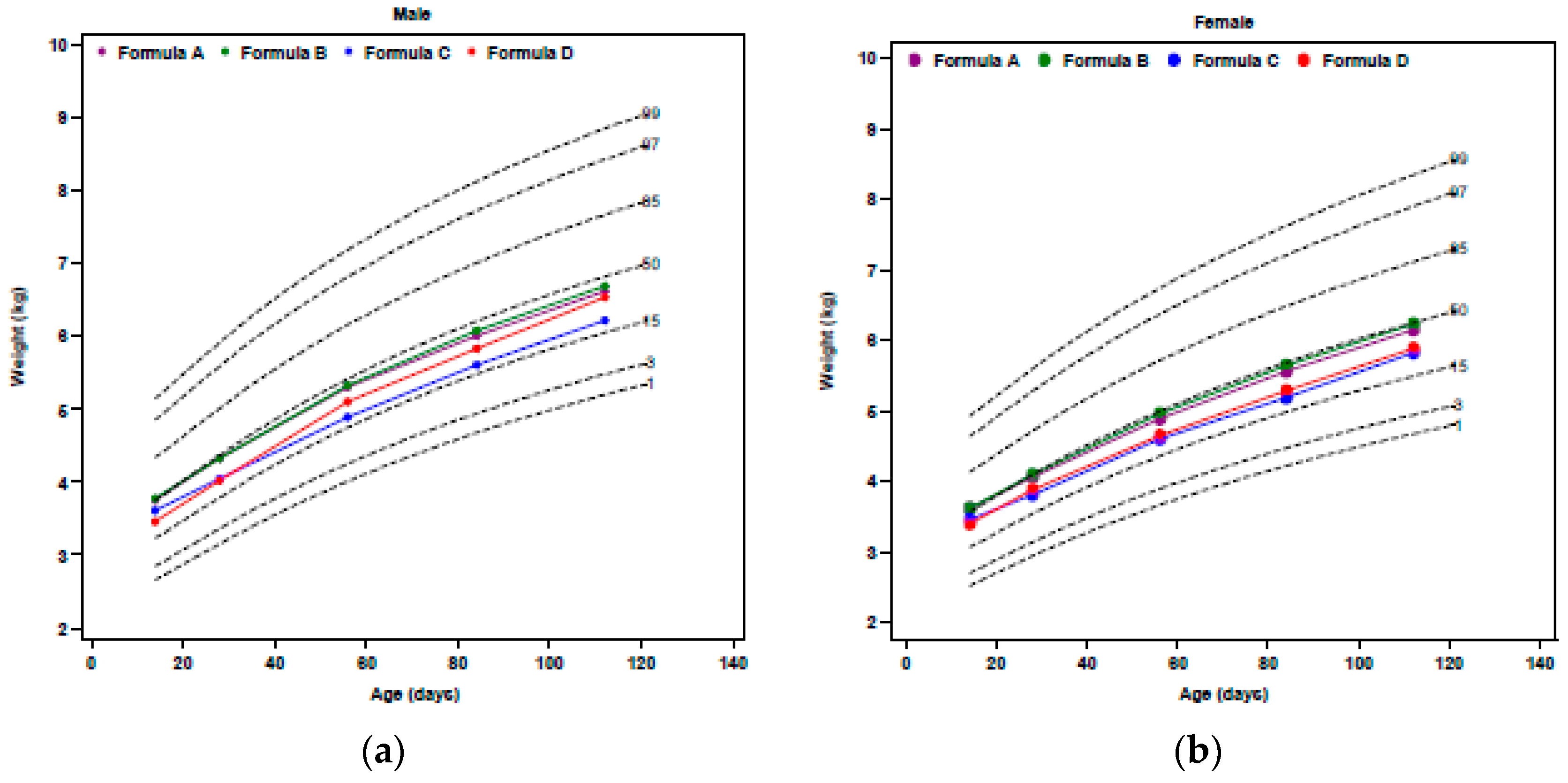
- Mean weight of infants fed EHF-A and EHF-B were not statistically significantly different during the first four months of life (p > 0.05) and were significantly greater than those fed EHF-C and EHF-D at 2 weeks and at one, two, three, and four (EHF-C only) months of age (p ≤ 0.05) (Figure 1).
- Mean weight of infants fed EHF-A and EHF-B maintained BW percentiles (~50th to 60th percentile) more closely than did infants fed EHF-C and EHF-D.
- Fields et al. [17] reported that significantly more ITT healthy term infants fed EHF-C had WHO weight-for-age falling below the 5th percentile than those fed EHF-D. Over the study period, 12 infants (10%) fed EHF-D and 33 infants (22%) fed EHF-C had at least one weight measurement less than the 5th percentile (p = 0.011) [17]. For the evaluable cohort, eight infants (12%) fed EHF-D and 17 infants (21%) fed EHF-C had at least one weight measurement less than the 5th percentile (p = 0.014) [17].
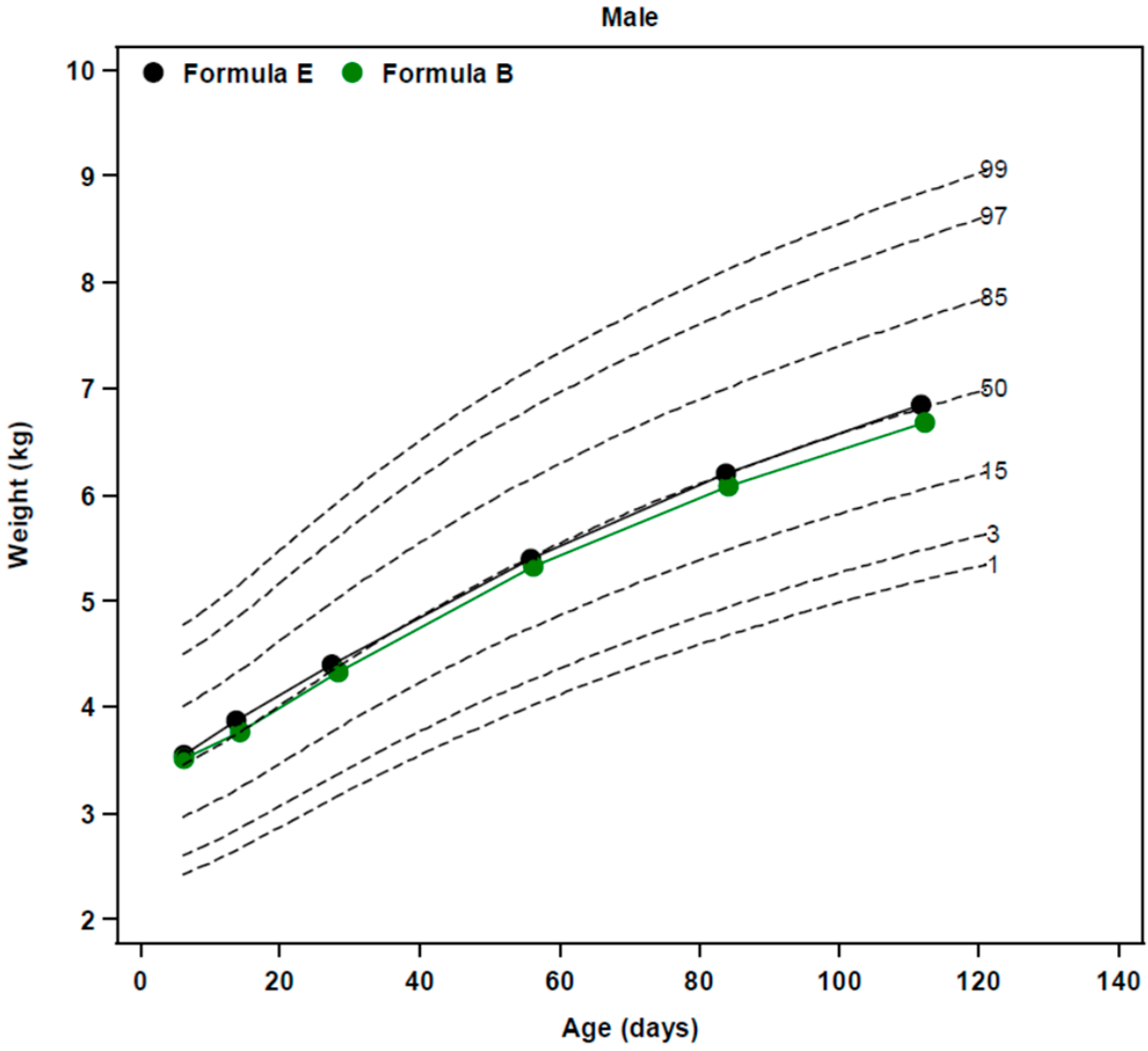
- WHO weight-for-age z-scores were determined in an ad-hoc analysis from two of our reported studies [14,15] and are displayed in Figure 2. No significant differences (p = 0.71) were observed in the change in weight-for-age z-score from 14 to 112 days of age in infants fed EHF-A (−0.23 ± 0.09), EHF-B (−0.15 ± 0.09), and AAF-E (−0.25 ± 0.10). Exact change in weight-for-age z-score for infants fed other EHFs could not be determined as this information was not reported. However, for EHF-C the change in weight-for-age z-score appeared to be considerably greater (approximately −0.45 to −0.55 for ITT and −0.30 to −0.40 for evaluable) than those reported for formulas EHF-A, EHF-B, and EHF-D (Figure 2).
- Body mass index (BMI) of healthy term infants fed EHF-A and EHF-B at 14 and 112 days of age was determined in an ad-hoc analysis from two of our reported studies [14,15] and is displayed in Table 4. Mean BMI of infants was 13.9 and 13.7 kg/m2 at 14 days of age for EHF-A and EHF-B, respectively, increasing to 16.6 and 16.5 kg/m2 at 112 days of age for EHF-A and EHF-B, respectively. BMI data was not reported or could not be calculated for infants receiving EHF-C and EHF-D.
3.1.2. Free Amino Acid-Based Infant Formulas
- In contrast, mean weight percentiles of ITT healthy term male infants fed AAF-F were at the 48th percentile at birth and dropped to between the 28th to 36th percentiles (females ranged from 39th to 47th percentile) over the first four months of life [19].
- Similar to infants fed AAF-F, ITT healthy term male infants fed AAF-H had mean weight percentiles at the 50th percentile at birth that dropped to between the 30th to 37th percentiles (females ranged from 31st to 37th percentile) during the study [19].
- Mean weight gains from 14 to 112 or 120 days of age ranged from 27.3 to 29.8 g/day for all AAFs (Table 2), and were similar to those reported by Nelson et al. [22] for breastfed infants (27.5 g/day). Data for AAF-F were taken from Corkins et al. [19] since they were not reported in Harvey et al. [20]. For AAFs, using unadjusted comparisons, mean weight gain per day for AAF-F was significantly less (p < 0.05) than mean weight gain per day for AAF-G.
- WHO weight-for-age z-score of AAF-E from birth to 112 days of age (Figure 2) and change in WHO weight-for-age z-score was determined in an ad-hoc analysis from one of our reported studies [14]. No significant differences were observed in the change in weight-for-age z-score from 14 to 112 days of age among infants fed EHF-A, EHF-B, and AAF-E (p = 0.71). Healthy term infants fed AAF-E displayed decreases of −0.25 ± 0.10 in weight-for-age z-score from 14 to 112 days of age. Weight-for-age z-score and change in weight-for-age z-score for infants fed other AAFs could not be compared as information was not reported.
- Data for infants fed AAF-G were compared to CDC growth standards and tracked with data for infants fed EHF-B [18]. Mean weights of infants fed AAF-B reported by Borschel et al. [14] tracked closely with those of infants fed AAF-E (Figure 2) and were near the 50th percentile on WHO standards. Therefore, it was assumed that if plotted on WHO growth plots, mean weight of infants fed AAF-G would track close to the 50th percentile.
- Harvey et al. [20] examined infants fed AAF-F (control) when compared to infants fed AAF-I (same formula as AAF-F, but with added pre- and probiotics). Harvey et al. [20] did not detail the protein content of the formulas. AAF-I was commercialized in the US with 2.8 g protein equivalents/100 kcal and the protein content of AAF-F was reduced in the US to this same level shortly before the availability of AAF-I. Thus, it was assumed that both formulas studied by Harvey et al. [20] contained 2.8 g protein equivalents/100 kcal. This was lower in protein content than the AAF-F studied by Corkins et al. [19]. Infant weight comparisons were presented unconventionally as ratios of weight gain (AAF-F/AAF-I = 1.00). Although infants grew similarly on both AAFs, it was impossible to determine how infants grew compared to the other AAFs and to WHO standards as these data, neither percentiles nor z-scores for individual groups, were presented. Thus, it was assumed that this group of infants fed AAF-I grew no better than the 30th to 37th percentiles, as reported for AAF-F in the study of Corkins et al. [19].
- BMI of healthy term infants fed AAF-E at 14 and 112 days of age was determined in an ad-hoc analysis from one of our reported studies [14] and is displayed in Table 4. Mean BMI of infants was 14.1 kg/m2 at 14 days of age for AAF-E increasing to 16.7 kg/m2 at 112 days of age. BMI data was not reported and could not be calculated for infants receiving AAF-F, AAF-G, AAF-H, and AAF-I. Change in BMI of infants fed AAF-E was similar to changes observed in infants fed EHF-A and EHF-B (p = 0.42) (Table 4).
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Dewey, K.G.; Peerson, J.M.; Brown, K.H.; Krebs, N.F.; Michaelsen, K.F.; Persson, L.A.; Salmenpera, L.; Whitehead, R.G.; Yeung, D.L.; World Health Organization Working Group on Infant Growth. Growth of breast-fed infants deviates from current reference data: A pooled analysis of US, Canadian, and European data sets. Pediatrics 1995, 96, 495–503. [Google Scholar] [PubMed]
- Fomon, S.J. Assessment of growth of formula-fed infants: Evolutionary considerations. Pediatrics 2004, 113, 389–393. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Growth Chart: A Tool for Use in Infant and Child Health Case; World Health Organization: Geneva, Switzerland, 1986. [Google Scholar]
- Hamill, P.V.V.; Drizd, T.A.; Johnson, C.L.; Reed, R.B.; Roche, A.F. NCHS Growth Curves for Children, Birth-18 Years; Department of Health, Education, and Welfare, Public Health Service, [Health Resources Administration], National Center for Health Statistics: Washington, DC, USA, 1977.
- World Health Organization Multicentre Growth Reference Study Group. WHO Child Growth Standards: Length/Height-For-Age, Weight-For-Age, Weight-For-Length, Weight-For-Height and Body Mass Index-For-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Infant Formula Act of 1980, Public Law No. 96-359, 94 Stat. 1190 [codified at 21 U.S.C. §350(a), 301, 321(aa), 331, 374(a)]. 26 September 1980. Available online: https://www.gpo.gov/fdsys/pkg/STATUTE-94/pdf/STATUTE-94-Pg1190.pdf (accessed on 28 February 2018).
- Koletzko, B.; von Kries, R.; Closa, R.; Escribano, J.; Scaglioni, S.; Biovannini, M.; Beyer, J.; Demmelmair, H.; Gruszfeld, D.; Dobrzanska, A.; et al. Lower protein in infant formula is associated with lower weight up to age 2 year: A randomized clinical trial. Am. J. Clin. Nutr. 2009, 89, 1836–1845. [Google Scholar] [PubMed]
- EFSA NDA Panel (EFSA Panel on Dietetic Products, Nutrition and Allergies). Scientific Opinion on the essential composition of infant and follow-on formulae. EFSA J. 2014, 12, 3760. [Google Scholar] [CrossRef] [Green Version]
- Giovannini, M.; Agostoni, C.; Fiocchi, A.; Bellú, R.; Trojan, S.; Riva, E. Antigen-reduced infant formulas versus human milk: Growth and metabolic parameters in the first 6 months of life. J. Am. Coll. Nutr. 1994, 13, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Mennella, J.A.; Ventura, A.K.; Beauchamp, G.K. Differential growth patterns among healthy infants fed protein hydrolysate or cow-milk formulas. Pediatrics 2011, 127, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Rzehak, P.; Sausenthaler, S.; Koletzko, S.; Reinhardt, D.; von Berg, A.; Krämer, U.; Berdel, D.; Bollrath, C.; Grübl, A.; Bauer, C.P.; et al. Short- and long-term effects of feeding hydrolyzed protein infant formulas on growth at <6 year of age: Results from the German Infant Nutritional Intervention Study. Am. J. Clin. Nutr. 2009, 89, 1846–1856. [Google Scholar] [PubMed]
- U.S. National Archives and Records Administration. Code of Federal Regulations. Title 21. Section 106. Infant Formula Requirements Pertaining to Good Manufacturing Practice, Quality Control Procedures, Quality Factors, Records and Reports and Notifications. 2015. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm (accessed on 4 September 2017).
- American Academy of Pediatrics, Committee on Nutrition. Clinical Testing of Infant Formulas with Respect to Nutritional Suitability for Term Infants. Report to the FDA; American Academy of Pediatrics: Elk Grove Village, IL, USA, 1988. [Google Scholar]
- Borschel, M.W.; Ziegler, E.E.; Wedig, R.T.; Oliver, J.S. Growth of healthy term infants fed an extensively hydrolyzed casein-based or free amino acid-based infant formula: A randomized, double-blind, controlled trial. Clin. Pediatr. 2013, 52, 910–917. [Google Scholar] [CrossRef] [PubMed]
- Borschel, M.W.; Baggs, G.E.; Barrett-Reis, B. Growth of healthy term infants fed ready-to-feed and powdered forms of an extensively hydrolyzed casein-based infant formula: A randomized, blinded, controlled study. Clin. Pediatr. 2014, 53, 585–592. [Google Scholar] [CrossRef] [PubMed]
- Scalabrin, D.M.; Johnston, W.H.; Hoffman, D.R.; P’Pool, V.L.; Harris, C.L.; Mitmesser, S.H. Growth and tolerance of healthy term infants receiving hydrolyzed infant formulas supplemented with Lactobacillus rhamnosus GG: Randomized, double-blind, controlled trial. Clin. Pediatr. 2009, 48, 734–744. [Google Scholar] [CrossRef] [PubMed]
- Fields, D.; Czerkies, L.; Sun, S.; Storm, H.; Saavedra, J.; Sorensen, R. A randomized controlled trial assessing growth of infants fed a 100% whey extensively hydrolyzed formula compared with a casein-based extensively hydrolyzed formula. Glob. Pediatr. Health 2016, 3, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Burks, W.; Jones, S.M.; Berseth, C.L.; Harris, C.; Sampson, H.A.; Scalabrin, D.M.F. Hypoallergenicity and effects on growth and tolerance of a new amino acid-based formula with docosahexaenoic acid and arachidonic acid. J. Pediatr. 2008, 153, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Corkins, M.; Czerkies, L.; Storm, H.M.; Sun, S.; Saavedra, J.M. Assessment of growth of infants fed an amino acid-based formula. Clin. Med. Insights Pediatr. 2016, 10, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Harvey, B.M.; Langford, J.E.; Harthoom, L.F.; Gillman, S.A.; Green, R.D.; Schwartz, R.H.; Burks, A.W. Effects on growth and tolerance and hypoallergenicity of an amino acid-based formula with synbiotics. Pediatr. Res. 2014, 75, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Kuczmarski, R.J.; Flegal, K.M.; Mei, Z.; Buo, S.; Wei, R.; Grummer-Strawn, L.M.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. Centers for Disease Control and Prevention 2000 growth charts for the United States: Improvements to the 1977 National Center for Health Statistics version. Pediatrics 2002, 109, 45–60. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.E.; Rogers, R.R.; Ziegler, E.E.; Fomon, S.J. Gain in weight and length during early infancy. Early Hum. Dev. 1989, 19, 223–239. [Google Scholar] [CrossRef]
- Turck, D.; Michaelsen, K.F.; Shamir, R.; Braegger, C.; Campoy, C.; Colomb, V.; Desci, T.; Domellöf, M.; Fewtrell, M.; Kolacek, S.; et al. World Health Organization 2006 child growth standards and 2007 growth reference charts: A discussion paper by the Committee on Nutrition of the European Society for Pediatric Gastroenteroloty, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Spalinger, J.; Nydegger, A.; Belli, D.; Furlano, R.I.; Yan, J.; Tanguy, J.; Pecquet, S.; Destaillats, F.; Egli, D.; Steenhout, P. Growth of infants fed formula with evolving nutritional composition: A single-arm non-inferiority study. Nutrients 2017, 9, 219. [Google Scholar] [CrossRef] [PubMed]
- Homan, G.J. Failure to thrive: A practical guide. Am. Fam. Physician 2016, 94, 295–299. [Google Scholar] [PubMed]
- Yoo, S.D.; Hwang, E.-H.; Lee, Y.J.; Park, J.H. Clinical characteristics of failure to thrive in infant and toddler: Organic vs. nonorganic. Pediatr. Gastroenterol. Hepatol. Nutr. 2013, 16, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Dulloo, A.B.; Fathi, M.; Mensi, N.; Girardier, L. Twenty-four-hour energy expenditure and urinary catecholamines of humans consuming low-to-moderate amounts of medium-chain triglycerides: A dose response study in a human respiratory chamber. Eur. J. Clin. Nutr. 1996, 50, 152–158. [Google Scholar] [PubMed]
- Borschel, M.W.; Abbott Nutrition, Abbott Laboratories, Columbus, OH, USA. Unpublished Data. 1993.
- Grimble, G.K. The significance of peptides in clinical nutrition. Annu. Rev. Nutr. 1994, 14, 419–447. [Google Scholar] [CrossRef] [PubMed]
- Grimble, G.K.; Silk, D.B.A. The optimum form of dietary nitrogen in gastrointestinal disease: Proteins, peptides or amino acids? Verh. Dtsch. Ges. Inn. Med. 1986, 92, 674–685. [Google Scholar] [PubMed]
- Borschel, M.W.; Antonson, D.L.; Murray, N.D.; Oliva-Hemker, M.; Mattis, L.E.; Kerzner, B.; Tolia, V.; Baggs, G. Two single group, prospective, baseline-controlled feeding studies in infants and children with chronic diarrhea fed a hypoallergenic free amino acid-based formula. BMC Pediatr. 2014, 14, 136. [Google Scholar] [CrossRef] [PubMed]

| Formula Code | Formula | Manu-Facturer | Formula Type | Protein Source | Protein, g/100 kcal † | Protein, g/L † | % Fat as MCT | MCT, g/100 kcal |
|---|---|---|---|---|---|---|---|---|
| A | Similac® Alimentum® | AN | EHF | Casein, TYR, CYS, TRP | 2.75 | 18.6 | 33 | 1.83 |
| B | Nutramigen® | MJ | EHF | Casein ‡, TYR, CYS, TRP | 2.8 | 18.9 | 0 | 0 |
| C | Pregestimil® | MJ | EHF | Casein ‡, TYR, CYS, TRP | 2.8 | 18.9 | 55 | 3.08 |
| D | Gerber Hypoallergenic HA™ § | NE | EHF | Whey | 2.6 | 17.6 | 49 | 2.50 |
| E | EleCare® Infant | AN | AAF | FAA | 3.1 | 21.0 | 33 | 1.58 |
| F | Neocate® Infant | NU | AAF | FAA | 3.1 ** | 21.0 | 33 | 1.49 |
| G | Nutramigen AA™ *** | MJ | AAF | FAA | 2.8 | 18.9 | 0 | 0 |
| H | Alfamino™ | NE | AAF | FAA | 2.8 | 18.9 | 43 | 2.15 |
| I | Neo-Syn™ | NU | AAF | FAA | 2.8 # | 18.9 | 33 | 1.49 |
| Formula Code | Type of Formula | Number of Infants | Mean Weight Gain, g/Day | Interval of Weight Gain | Reference |
|---|---|---|---|---|---|
| A | EHF | 67 | 27.8 ± 0.7 * | 14–112 | [15] |
| B-1 | EHF | 70 | 27.6 ± 0.7 | 14–120 | [16] |
| B-2 | EHF | 52 ‡ | 29.1 ± 1.0 | 14–120 | [18] |
| B-3 | EHF | 69 | 28.4 ± 0.7 | 14–112 | [14] |
| C | EHF | 58 | 25.4 ± 6.5 † | 14–112 | [17] |
| D | EHF | 68 | 28.1 ± 6.2 † | 14–112 | [17] |
| E | AAF | 65 | 28.3 ± 0.8 | 14–112 | [14] |
| F | AAF | 60 | 27.3 ± 4.9 † | 14–112 | [19] |
| G | AAF | 58 ‡ | 29.8 ± 1.0 | 14–120 | [18] |
| H | AAF | 59 | 27.4 ± 6.4 † | 14–112 | [19] |
| Study | Formula Code | ITT Infants, Number | Evaluable Infants, Number | Country and Number of Sites | Main Results | Funding Source |
|---|---|---|---|---|---|---|
| Borschel et al., 2014 [15] | EHF-A | 95 (54/41) * | 67 | US, 8 sites | Infants fed liquid and powdered forms of EHF-A had similar daily wt gains. Drop-out rate was 29% on EHF-A. | AN |
| Scalabrin et al., 2009 [16] | EHF-B | 94 (44/50) | 70 | US, 14 sites | Mean achieved wt for male and female infants fed EHF-B with and without probiotic were similar and plotted on the CDC charts [21] fell between the 25th and 75th percentiles. Drop-out rate was 36% for EHF-B. | MJ |
| Burks et al., 2008 [18] | EHF-B | 165 total enrolled both groups † | 52 ‡ | US, 14 sites | Infants fed EHF-B and AAF-G had similar wt gains. Overall drop-out rate was 33% (percent not reported for each group). | MJ |
| AAF-G | 58 ‡ | |||||
| Borschel et al., 2013 [14] | EHF-B | 106 (55/51) | 69 | US, 2 sites | Daily wt gain was similar between EHF-B and AAF-E. Drop-out rate was 39% on AAF-E compared to 35% on EHF-B. | AN |
| AAF-E | 107 (57/50) | 65 | ||||
| Fields et al., 2016 [17] | EHF-C | 158 (87/71) | 58 | US, 25 sites | Daily wt gain was significantly higher on EHF-D compared to EHF-C. Drop-out rate was significantly lower (41%) on EHF-D compared to EHF-C (56%). Infants on EHF-C experienced more days with >3 loose stools/day and a higher incidence of vomiting. | NE |
| EHF-D | 124 (67/57) | 68 | ||||
| Corkins et al., 2016 [19] | AAF-F | 119 (59/60) | 60 | US, 17 sites | Infants fed AAF-H had similar daily wt gains compared to those fed AAF-F. Drop-out rate was 40% on AAF-F and 47% on AAF-H. | NE |
| AAF-H | 106 (57/49) | 59 | ||||
| Harvey et al., 2014 [20] | AAF-F | 56 (35/21) | 38 | US, 11 sites | No significant difference in wt gain between AAF-F and AAF-I. Drop-out rate was 46% on AAF-I and 32% on AAF-F. | NU |
| AAF-I | 59 (35/24) | 32 |
| Formula Code | Type of Formula | Number of Infants | Age, Days | Mean Body Mass Index, kg/m2 | Mean BMI-for- Age Z-Score | Mean Change in BMI-for-Age Z-Score from 14–112 Days of Age † | Source of Data for Ad-Hoc Analysis |
|---|---|---|---|---|---|---|---|
| A | EHF | 67 | 14 | 13.9 ± 0.13 * | 0.16 ± 0.10 | - | [15] |
| 67 | 112 | 16.6 ± 0.16 | −0.24 ± 0.11 | −0.16 ± 0.13 | |||
| B | EHF | 69 | 14 | 13.7 ± 0.12 | 0.08 ± 0.10 | - | [14] |
| 69 | 112 | 16.5 ± 0.14 | −0.31 ± 0.09 | −0.39 ± 0.12 | |||
| E | AAF | 65 | 14 | 14.1 ± 0.13 | 0.37 ± 0.09 | - | [14] |
| 65 | 112 | 16.7 ± 0.18 | −0.15 ± 0.12 | −0.41 ± 0.14 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Borschel, M.W.; Baggs, G.E.; Oliver, J.S. Comparison of Growth of Healthy Term Infants Fed Extensively Hydrolyzed Protein- and Amino Acid-Based Infant Formulas. Nutrients 2018, 10, 289. https://doi.org/10.3390/nu10030289
Borschel MW, Baggs GE, Oliver JS. Comparison of Growth of Healthy Term Infants Fed Extensively Hydrolyzed Protein- and Amino Acid-Based Infant Formulas. Nutrients. 2018; 10(3):289. https://doi.org/10.3390/nu10030289
Chicago/Turabian StyleBorschel, Marlene W., Geraldine E. Baggs, and Jeffery S. Oliver. 2018. "Comparison of Growth of Healthy Term Infants Fed Extensively Hydrolyzed Protein- and Amino Acid-Based Infant Formulas" Nutrients 10, no. 3: 289. https://doi.org/10.3390/nu10030289




