Body Fat Measurements in Singaporean Adults Using Four Methods
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Anthropometry
2.3. PBF Measurements
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Van Gaal, L.F.; Mertens, I.L.; De Block, C.E. Mechanisms linking obesity with cardiovascular disease. Nature 2006, 444, 875–880. [Google Scholar] [CrossRef] [PubMed]
- Renehan, A.G.; Tyson, M.; Egger, M.; Heller, R.F.; Zwahlen, M. Body-mass index and incidence of cancer: A systematic review and meta-analysis of prospective observational studies. Lancet 2008, 371, 569–578. [Google Scholar] [CrossRef]
- Liu, J.; Hong, Y.; D’Agostino, R.B. Predictive value for the Chinese population of the Framingham CHD risk assessment tool compared with the Chinese Multi-Provincial Cohort Study. JAMA 2004, 291, 2591–2599. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Wang, Z.; Zhang, J.; Hua, J.; He, W.; Zhu, S. Estimation of total body skeletal muscle mass in Chinese adults: Prediction model by dual-energy X-ray adsorptiometry. PLoS ONE 2013, 8, e53561. [Google Scholar] [CrossRef] [PubMed]
- Ellis, K.J. Human body composition: In vivo methods. Physiol. Rev. 2000, 80, 649–680. [Google Scholar] [CrossRef] [PubMed]
- Lowry, D.W.; Tomiyama, A.J. Air displacement plethysmography versus dual-energy X-ray absorptiometry in underweight, normal-weight and overweight/obese individuals. PLoS ONE 2015, 10, e0115086. [Google Scholar] [CrossRef] [PubMed]
- Dempster, P.; Aitkens, S. A new air displacement method for the determination of human body composition. Med. Sci. Sports Exerc. 1995, 27, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Fields, D.A.; Goran, M.I.; McCrory, M.A. Body-composition assessment via air-displacement plethysmography in adults and children: A review. Am. J. Clin. Nutr. 2002, 75, 453–467. [Google Scholar] [CrossRef] [PubMed]
- McCrory, M.A.; Gomez, T.D.; Bernauer, E.M.; Mole, P.A. Evaluation of a new air displacement plethysmography for measuring human body composition. Med. Sci. Sports Exerc. 1995, 27, 1686–1691. [Google Scholar] [CrossRef] [PubMed]
- Brodie, D.; Moscrip, V.; Hutcheon, R. Body composition measurement: A review of hydrodensitometry, anthropometry and impedance methods. Nutrition 1998, 14, 296–310. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Gómez, J.M.; Heitmann, B.L.; Kent-Smith, L.; Melchior, J.; Pirlich, M.; et al. Bioelectrical impedance analysis-part II: Utilization in clinical practice. Clin. Nutr. 2004, 23, 1430–1453. [Google Scholar] [CrossRef] [PubMed]
- Montagnese, C.; Williams, J.E.; Haroun, D.; Siervo, M.; Fewtrell, M.S.; Wells, J.C.K. Is a single bioelectrical impedance equation valid for children of wide ranges of age, pubertal status and nutritional status? Evidence from the 4-component model. Eur. J. Clin. Nutr. 2013, 67, S34–S39. [Google Scholar] [CrossRef] [PubMed]
- Jaffrin, M.Y. Body composition determination by bioimpedance: An update. Curr. Opin. Clin. Nutr. Metab. Care 2009, 12, 482–486. [Google Scholar] [CrossRef] [PubMed]
- Pateyjohns, I.R.; Brinkworth, G.D.; Buckley, J.D.; Noakes, M.; Clifton, P.M. Comparison of three bioelectrical impedance methods with DXA in overweight and obese men. Obesity (Silver Spring) 2006, 14, 2064–2070. [Google Scholar] [CrossRef] [PubMed]
- Rush, E.C.; Chandu, V.; Plank, L.D. Prediction of fat-free mass by bioimpedance analysis in migrant Asian Indian men and women: A cross validation study. Int. J. Obes. (Lond.) 2006, 30, 1125–1131. [Google Scholar] [CrossRef] [PubMed]
- International Society for the Advancement of Kinanthropometry. International Standards for Anthropometric Assessment (ISAK); International Society for the Advancement of Kinanthropometry: Glasgow, UK, 2001. [Google Scholar]
- Durnin, J.V.G.A.; Womersley, J. Body fat assessment from total body density and its estimation from skinfold thickness: Measurements on 481 men and women aged from 16 to 72 years. Br. J. Nutr. 1974, 32, 77–97. [Google Scholar] [CrossRef] [PubMed]
- Jackson, A.S.; Pollock, M.L.; Ward, A. Generalized equations for predicting body density of women. Med. Sci. Sports Exerc. 1980, 12, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Heyward, V.H.; Stolarczyk, L.M. Applied Body Composition Assessment; Human Kinetics: Champaign, IL, USA, 1996. [Google Scholar]
- Lanham, D.A.; Stead, M.A.; Tsang, K.; Davies, P.S.W. The prediction of body composition in Chinese Australian females. Int. J. Obes. 2001, 25, 286–291. [Google Scholar] [CrossRef] [PubMed]
- Immink, M.D.; Flores, R.; Diaz, E.O. Body mass index, body composition and the chronic energy deficiency classification of rural adult populations in Guatemala. Eur. J. Clin. Nutr. 1992, 46, 419–427. [Google Scholar] [PubMed]
- Siri, W.E. Body Composition from Fluid Spaces and Density, Analysis of Methods. Techniques for Measuring Body Composition; Brozek, J., Henschel, A., Eds.; National Academy of Sciences: Washington, DC, USA, 1961; pp. 223–244. [Google Scholar]
- Yao, M.; Roberts, S.B.; Ma, G.; Pan, H.; McCrory, M.A. Field methods for body composition assessment are valid in healthy Chinese adults. J. Nutr. 2002, 132, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Cossrow, N.; Falkner, B. Race/ethnic issues in obesity and obesity-related comorbidities. J. Clin. Endocrinol. Metab. 2004, 89, 2590–2594. [Google Scholar] [CrossRef] [PubMed]
- Eveleth, P.B.; Tanner, J.M. World-Wide Variation in Human Growth; Cambridge University Press: Cambridge, UK, 1976. [Google Scholar]
- Lohman, T.; Roche, A.; Martorell, R. Anthropometric Standardization Preference Manual; Human Kinetics: Champaign, IL, USA, 1988. [Google Scholar]
- Laskey, M.A. Dual-energy X-ray absorptiometry and body composition. Nutrition 1996, 12, 45–51. [Google Scholar] [CrossRef]
- Mazess, R.B.; Barden, H.S.; Bisek, J.P.; Hanson, J. Dual-energy X-ray absorptiometry for total-body and regional bone-mineral and soft-tissue composition. Am. J. Clin. Nutr. 1990, 51, 1106–1112. [Google Scholar] [CrossRef] [PubMed]
- Roubenoff, R.; Kehayias, J.J.; Dawson-Hughes, B.; Heysfield, S.B. Use of dual-energy X-ray absorptiometry in body-composition studies: Not yet a “gold standard”. Am. J. Clin. Nutr. 1993, 58, 589–591. [Google Scholar] [CrossRef] [PubMed]
- Tataranni, P.A.; Ravussin, E. Use of dual-energy x-ray absorptiometry in obese individuals. Am. J. Clin. Nutr. 1995, 62, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Goran, M.I.; Toth, M.J.; Poehlman, E.T. Assessment of research-based body composition techniques in healthy elderly men and women using the 4-compartment model as a criterion method. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Kistorp, C.N.; Svendsen, O.L. Body composition analysis by dual energy X-ray absorptiometry in female diabetics differ between manufacturers. Eur. J. Clin. Nutr. 1997, 51, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Wingfield, H.L.; Smith-Ryan, A.E.; Woessner, M.N.; Fultz, S.N.; Graff, R.M. Body composition assessment in overweight women: Validation of air displacement plethysmography. Clin. Physiol. Funct. Imaging 2014, 34, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Ball, S.D.; Altena, T.S. Comparison of the Bod Pod and dual energy X-ray absorptiometry in men. Physiol. Meas. 2004, 25, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Radley, D.; Gately, P.J.; Cooke, C.B.; Carroll, S.; Oldroyd, B.; Truscott, J.G. Estimates of percentage body fat in young adolescents: A comparison of dual-energy X-ray absorptiometry and air displacement plethysmography. Eur. J. Clin. Nutr. 2003, 57, 1402–1410. [Google Scholar] [CrossRef] [PubMed]
- Radley, D.; Gately, P.J.; Cooke, C.B.; Carroll, S.; Oldroyd, B.; Truscott, J.G. Percentage fat in overweight and obese children: Comparison of DXA and air displacement plethysmography. Obes. Res. 2005, 13, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Dehghan, M.; Merchant, A.T. Is bioelectrical impedance accurate for use in large epidemiological studies? Nutr. J. 2008, 7, 26. [Google Scholar] [CrossRef] [PubMed]
- Jakicic, J.M.; Wing, R.R.; Lang, W. Bioelectrical impedance analysis to assess body composition in obese adult women: The effect of ethnicity. Int. J. Obes. Relat. Metab. Disord. 1998, 22, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Going, S.; Nichols, J.; Loftin, M.; Stewart, D.; Lohman, T.; Tuuri, G.; Ring, K.; Pickrel, J.; Blew, R.; Stevens, J. Validation of bioelectrical impedance analysis (BIA) for estimation of body composition in Black, White and Hispanic adolescent girls. Int. J. Body Compos. Res. 2006, 4, 161–167. [Google Scholar] [PubMed]
- Sun, G.; French, C.R.; Martin, G.R.; Younghusband, B.; Green, R.C.; Xie, Y.G.; Mathews, M.; Barron, J.R.; Fitzpatrick, D.G.; Gulliver, W.; et al. Comparison of multifrequency bioelectrical impedance analysis with dual-energy X-ray absorptiometry for assessment of percentage body fat in a large, healthy population. Am. J. Clin. Nutr. 2005, 81, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Eisenkölbl, J.; Kartasurya, M.; Widhalm, K. Underestimation of percentage fat mass measured by bioelectrical impedance analysis compared to dual energy X-ray absorptiometry method in obese children. Eur. J. Clin. Nutr. 2001, 55, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Eston, R.G.; Rowlands, A.V.; Charlesworth, S.; Davies, A.; Hoppitt, T. Prediction of DXA-determined whole body fat from skinfolds: Importance of including skinfolds from the thigh and calf in young, healthy men and women. Eur. J. Clin. Nutr. 2005, 59, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Kalra, S.; Mercuri, M.; Anand, S.S. Measures of body fat in South Asian adults. Nutr. Diabetes 2013, 3, e69. [Google Scholar] [CrossRef] [PubMed]
- Henry, C.J.; Ponnalagu, S.; Bi, X.; Tan, S.Y. New equations to predict body fat in Asian Chinese using age, height, skinfold thickness and waist circumference. J. Acad. Nutr. Diet. 2018, in press. [Google Scholar]
- Kohrt, W.M. Body composition by DEXA: Tried and true? Med. Sci. Sports Exerc. 1995, 27, 1349–1353. [Google Scholar] [CrossRef] [PubMed]


| Total (n = 445) | Men (n = 184) | Women (n = 261) | |
|---|---|---|---|
| Age (years) | 37.5 ± 14.5 | 37.3 ± 14.3 | 37.7 ± 14.7 |
| Ethnicity | |||
| Chinese (n) | 406 (91%) | 162 (88%) | 244 (93%) |
| Non-Chinese (n) | 39 (9%) | 22 (12%) | 17 (7%) |
| Height (cm) | 164.5 ± 8.4 | 171.4 ± 6.0 | 159.7 ± 6.0 ** |
| Weight (kg) | 61.0 ± 12.0 | 68.5 ± 10.3 | 55.7 ± 10.2 ** |
| BMI (kg/m2) | 22.4 ± 3.5 | 23.3 ± 3.2 | 21.8 ± 3.5 ** |
| WC (cm) | 73.6 ± 9.4 | 78.6 ± 8.5 | 70.0 ± 8.3 ** |
| WHR | 0.80 ± 0.07 | 0.85 ± 0.05 | 0.76 ± 0.05 ** |
| DEXA PBF (%) | 30.6 ± 7.8 | 24.2 ± 5.6 | 35.1 ± 5.9 ** |
| BOD POD PBF (%) | 26.7 ± 8.7 | 21.5 ± 7.5 | 30.4 ± 7.5 ** |
| BIA PBF (%) | 24.9 ± 8.1 | 18.7 ± 5.4 | 29.3 ± 6.6 ** |
| SKF PBF (%) | 18.0 ± 7.0 | 12.1 ± 4.2 | 22.1 ± 5.4 ** |
| Tertile 1 (n = 64) BMI ≤ 21.6 kg/m2 | Tertile 2 (n = 60) 21.6 < BMI ≤ 24.5 kg/m2 | Tertile 3 (n = 60) 24.5 < BMI ≤ 37.5 kg/m2 | |
|---|---|---|---|
| DEXA | 20.6 ± 4.6 | 24.6 ± 3.7 | 27.7 ± 5.8 a |
| BOD POD | 16.6 ± 6.0 | 21.7 ± 5.3 | 26.5 ± 7.4 a |
| BIA | 14.2 ± 4.0 | 18.5 ± 3.2 | 23.6 ± 4.2 |
| SKF | 9.9 ± 3.2 | 11.9 ± 2.9 | 14.6 ± 4.9 |
| Tertile 1 (n = 89) BMI ≤ 20.0 kg/m2 | Tertile 2 (n = 86) 20.0 < BMI ≤ 22.4 kg/m2 | Tertile 3 (n = 86) 22.4 < BMI ≤ 34.3 kg/m2 | |
|---|---|---|---|
| DEXA | 30.8 ± 4.5 | 34.7 ± 4.4 | 39.8 ± 4.9 |
| BOD POD | 24.6 ± 5.8 a | 30.2 ± 4.7 | 36.6 ± 6.5 b |
| BIA | 23.2 ± 3.3 a | 28.5 ± 2.7 | 36.4 ± 5.0 b |
| SKF | 18.2 ± 3.8 | 21.7 ± 3.7 | 26.5 ± 4.8 |
| Age (years) | Men | Women | ||
|---|---|---|---|---|
| 21 < Age < 40 (n = 113) | 40 ≤ Age < 70 (n = 71) | 21 < Age < 40 (n = 156) | 40 ≤ Age < 70 (n = 105) | |
| DEXA | 22.9 ± 5.8 ** | 26.3 ± 4.6 a | 33.1 ± 5.7 ** | 38.0 ± 4.7 |
| BOD POD | 19.4 ± 7.3 ** | 24.9 ± 6.4 a | 27.7 ± 7.0 **,b | 34.4 ± 6.5 |
| BIA | 17.5 ± 5.4 ** | 20.4 ± 4.9 | 27.9 ± 6.5 **,b | 31.4 ± 6.2 |
| SKF | 11.6 ± 4.4 | 12.8 ± 3.9 | 21.1 ± 5.4 ** | 23.6 ± 4.9 |
| Total (n = 445) | Men (n = 184) | Women (n = 261) | |
|---|---|---|---|
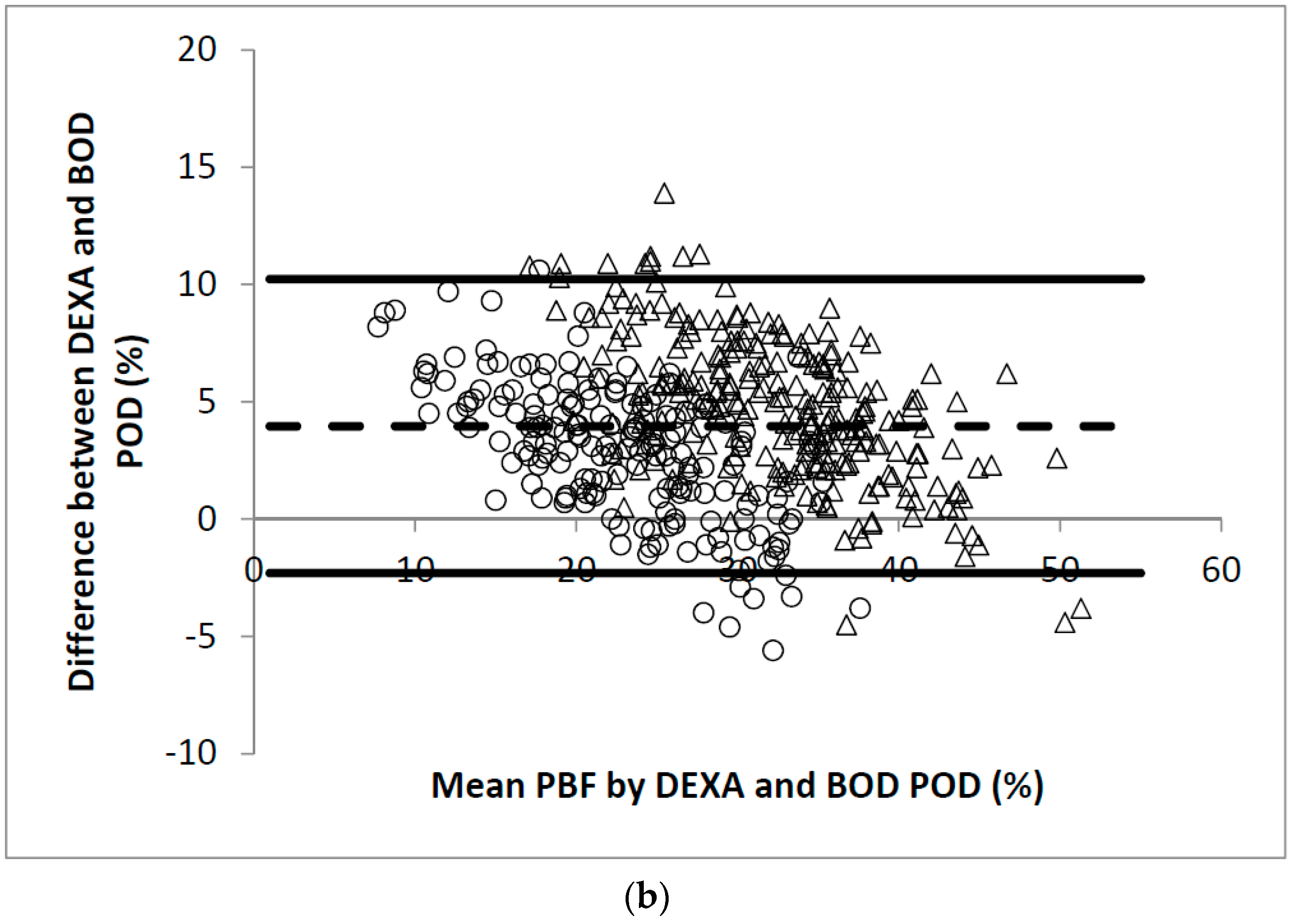
| DEXA vs. BOD POD | 0.93 | 0.86 | 0.82 |
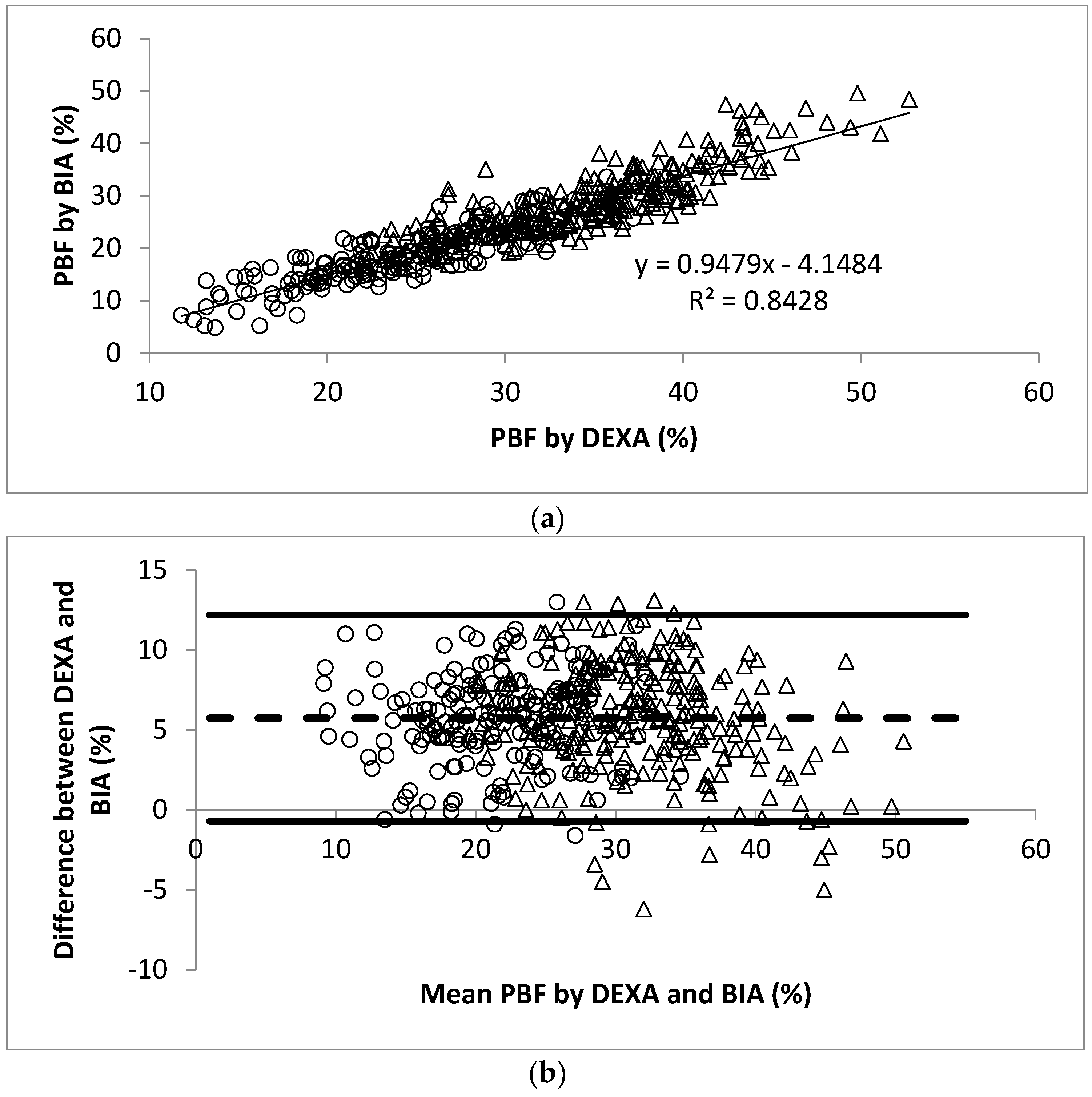
| DEXA vs. BIA | 0.93 | 0.76 | 0.75 |
| DEXA vs. SKF | 0.88 | 0.62 | 0.59 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bi, X.; Loo, Y.T.; Henry, C.J. Body Fat Measurements in Singaporean Adults Using Four Methods. Nutrients 2018, 10, 303. https://doi.org/10.3390/nu10030303
Bi X, Loo YT, Henry CJ. Body Fat Measurements in Singaporean Adults Using Four Methods. Nutrients. 2018; 10(3):303. https://doi.org/10.3390/nu10030303
Chicago/Turabian StyleBi, Xinyan, Yi Ting Loo, and Christiani Jeyakumar Henry. 2018. "Body Fat Measurements in Singaporean Adults Using Four Methods" Nutrients 10, no. 3: 303. https://doi.org/10.3390/nu10030303





