Dietary Patterns in Pregnancy and Effects on Nutrient Intake in the Mid-South: The Conditions Affecting Neurocognitive Development and Learning in Early Childhood (CANDLE) Study
Abstract
:1. Introduction
2. Experimental Section
2.1. Study Population
2.2. Demographic, Lifestyle and Socioeconomic Assessment
2.3. Dietary Assessment
2.4. Food Pattern Determination
2.5. Statistical Analysis
3. Results
3.1. Description of the Study Participants
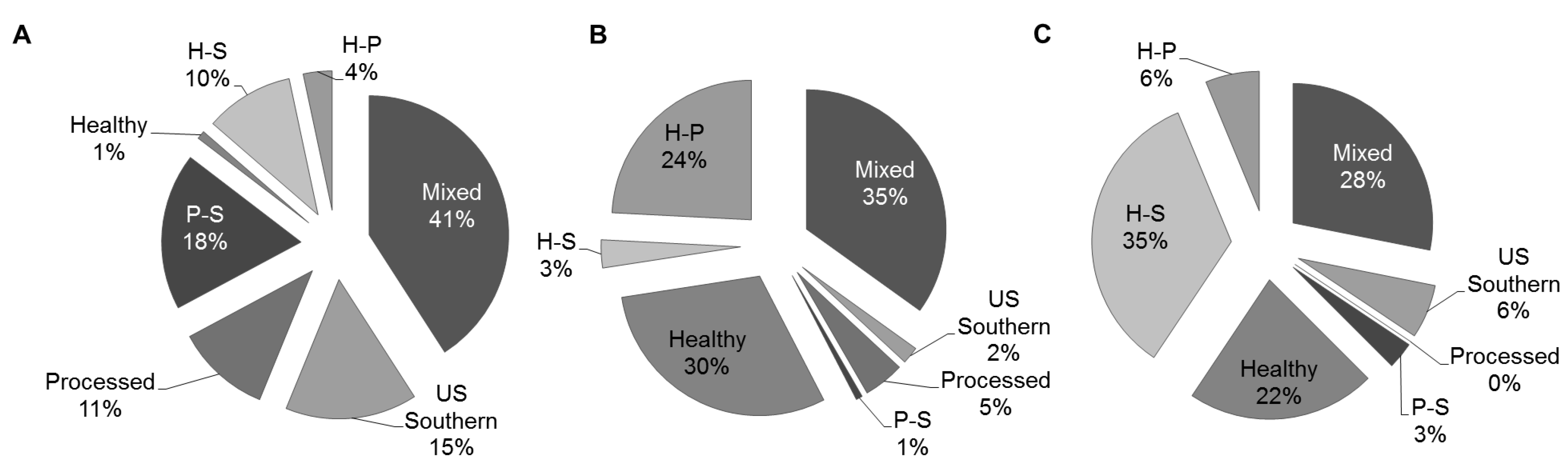
3.2. Dietary Patterns
| Food Item (Variance Explained) | Healthy (5.8%) | Processed (5.1%) | US Southern (4.4%) |
|---|---|---|---|
| BREAKFAST ITEMS | |||
| Eggs | 0.344 | ||
| Breakfast sausage including in sandwiches/biscuits | 0.301 | 0.311 | |
| Bacon | 0.367 | ||
| Cooked cereals (oatmeal, grits, cream of wheat) | 0.320 | ||
| Breakfast or cereal bars | 0.308 | ||
| DAIRY | |||
| Yogurt, including frozen | 0.434 | ||
| Cheese, sliced or spreads | 0.332 | ||
| Milk as a beverage | 0.303 | ||
| FRUITS | |||
| Banana | 0.334 | ||
| Apples or pears | 0.355 | ||
| Peaches or nectarines, fresh | 0.352 | ||
| Canned fruit | 0.374 | ||
| Strawberries or other berries in season | 0.383 | ||
| VEGETABLES | |||
| Broccoli | 0.331 | 0.312 | |
| Carrots or mixed vegetables with carrots | 0.471 | ||
| Corn | 0.316 | ||
| Green beans or green peas | 0.407 | ||
| Spinach, cooked | 0.370 | ||
| Greens (collards, turnip, or mustard) | 0.517 | ||
| Sweet potatoes, yams | 0.360 | ||
| Fried potatoes (French fries, home fries, hash browns) | 0.563 | ||
| Cole slaw, cabbage, Chinese cabbage | 0.444 | ||
| Green salad, lettuce salad | 0.600 | ||
| Tomatoes, raw | 0.524 | ||
| Other vegetables ( squash, cauliflower, okra, peppers) | 0.547 | ||
| Pinto, black or baked beans, chili with beans | 0.304 | ||
| Vegetable, vegetable-beef or tomato soup | 0.337 | ||
| BREADS | |||
| Sandwich buns | 0.469 | ||
| Bagels, English muffins, dinner rolls | 0.339 | ||
| Cornbread, corn muffins, hush puppies | 0.380 | ||
| Sliced bread (white, dark, whole wheat) | 0.310 | ||
| CONDIMENTS | |||
| Salad dressing, regular or low fat | 0.541 | ||
| Mayonnaise, sandwich breads | 0.372 | ||
| Ketchup, salsa or chili peppers | 0.450 | ||
| Mustard, barbecue sauce, soy sauce, gravy etc. | 0.322 | ||
| SWEETS AND SNACKS | |||
| Donuts | 0.304 | ||
| Cake, snack cakes, cupcakes, Ho-Hos, pastries | 0.437 | ||
| Cookies | 0.407 | ||
| Chocolate candy | 0.392 | ||
| Candy, hard, skittles, starburst etc. | 0.358 | ||
| Snack chips like potato chips, tortilla chips, Fritos, Doritos, popcorn | 0.552 | ||
| MEAT, FISH, POULTRY, MEAT SUBSTITUTES | |||
| Pizza | 0.328 | ||
| Meat substitutes (veggie burgers, chicken, hot dogs or lunch meats) | 0.346 | ||
| Hamburgers or cheese burgers | 0.504 | ||
| Hot dogs or sausage (Polish, Italian or chorizo) | 0.342 | ||
| Lunch meats (turkey or regular) | 0.393 | ||
| Tacos, burritos, enchiladas, tamales with meat or chicken | 0.306 | ||
| Ribs, spareribs | 0.373 | ||
| Liver (chicken livers or liverwurst) | 0.319 | ||
| Pigs feet, neck bones, oxtails, tongue | 0.419 | ||
| Beef or pork dishes (beef stew, pot pie, hamburger helper) | 0.319 | ||
| Fried chicken (nuggets, wings or patties) | 0.497 | ||
| Roasted or broiled chicken or turkey | 0.354 | ||
| Fried fish or fish sandwich | 0.378 | ||
| Fish not fried | 0.435 | ||
| Peanut Butter | 0.378 | ||
| Peanuts, sunflower seeds, or other nuts and seeds | 0.348 | ||
| BEVERAGES | |||
| 100% orange or grapefruit juice | 0.310 | ||
| Hi-C, Cranberry Juice Cocktail, Hawaiian Punch, Tang | 0.309 | ||
| Kool-aid, lemonade, sports drinks, or fruit flavored drinks | 0.356 | ||
| Soft drinks (Coke, Sprite, Orange) regular or diet | 0.377 | ||
| Water tap or bottled | 0.320 |
| Healthy | Processed | Southern | H-P | H-S | P-S | Mixed | |
|---|---|---|---|---|---|---|---|
| Food Groups | (n = 135) | (n = 98) | (n = 120) | (n = 123) | (n = 98) | (n = 136) | (n = 445) |
| BREAKFAST ITEMS | |||||||
| Eggs | 4.4 ± 0.6 | 4.6 ± 0.7 | 7.2 ± 0.6 | 4.3 ± 0.6 | 10 ± 0.7 | 7.9 ± 0.6 | 5.7 ± 0.3 |
| Breakfast sausage including in sandwiches/biscuits | 0.8 ± 0.5 | 4.9 ± 0.6 | 5.8 ± 0.5 | 3.0 ± 0.5 | 3.3 ± 0.6 | 9.7 ± 0.5 | 4.0 ± 0.3 |
| Bacon | 1.7 ± 0.6 | 5.5 ± 0.6 | 7.4 ± 0.6 | 2.9 ± 0.6 | 5.2 ± 0.6 | 8.5 ± 0.5 | 4.5 ± 0.3 |
| Cooked cereals (oatmeal, grits, cream of wheat) | 5.2 ± 0.7 | 2.8 ± 0.8 | 7.5 ± 0.7 | 3.1 ± 0.7 | 11.0 ± 0.8 | 5.2 ± 0.7 | 5.1 ± 0.4 |
| Breakfast or cereal bars | 6.6 ± 0.6 | 2.4 ± 0.7 | 2.8 ± 0.6 | 7.0 ± 0.6 | 4.9 ± 0.7 | 1.8 ± 0.6 | 4.6 ± 0.3 |
| DAIRY | |||||||
| Yogurt, including frozen | 11.1 ± 0.7 | 2.0 ± 0.8 | 3.5 ± 0.7 | 7.2 ± 0.7 | 9.6 ± 0.8 | 2.8 ± 0.7 | 5.6 ± 0.4 |
| Cheese, sliced or spreads | 16.3 ± 0.8 | 18.9 ± 1.0 | 10.7 ± 0.9 | 21.2 ± 0.9 | 13.9 ± 1.0 | 15.5 ± 0.8 | 15.5 ± 0.5 |
| Milk as a beverage | 16.7 ± 1.0 | 6.9 ± 1.2 | 8.7 ± 1.1 | 14.7 ± 1.1 | 14.7 ± 1.2 | 7.2 ± 1.0 | 12.0 ± 0.6 |
| FRUITS | |||||||
| Banana | 9.7 ± 0.7 | 3.7 ± 0.8 | 6.2 ± 0.8 | 6.8 ± 0.7 | 11.2 ± 0.8 | 5.4 ± 0.7 | 6.6 ± 0.4 |
| Apples or pears | 11.1 ± 0.7 | 3.2 ± 0.8 | 7.4 ± 0.8 | 6.2 ± 0.7 | 13.7 ± 0.8 | 7.2 ± 0.7 | 7.3 ± 0.4 |
| Canned fruit | 2.5 ± 0.3 | 5.0 ± 0.8 | 7.9 ± 0.8 | 4.3 ± 0.6 | 8.8 ± 1.0 | 7.7 ± 0.8 | 6.1 ± 0.4 |
| Peaches or nectarines, fresh | 2.3 ± 0.5 | 1.3 ± 0.6 | 5.0 ± 0.5 | 1.9 ± 0.5 | 7.4 ± 0.6 | 3.5 ± 0.5 | 3.2 ± 0.3 |
| Strawberries or other berries in season | 9.2 ± 0.6 | 2.8 ± 0.7 | 4.7 ± 0.7 | 6.3 ± 0.7 | 9.8 ± 0.7 | 3.9 ± 0.6 | 5.9 ± 0.3 |
| VEGETABLES | |||||||
| Broccoli | 4.3 ± 0.5 | 1.9 ± 0.6 | 4.2 ± 0.5 | 3.8 ± 0.5 | 8.6 ± 0.6 | 3.7 ± 0.5 | 4.1 ± 0.3 |
| Carrots or mixed vegetables with carrots | 6.6 ± 0.5 | 1.3 ± 0.6 | 2.4 ± 0.5 | 4.5 ± 0.5 | 7.5 ± 0.6 | 2.0 ± 0.5 | 3.7 ± 0.3 |
| Corn | 3.4 ± 0.5 | 3.2 ± 0.5 | 4.9 ± 0.5 | 5.0 ± 0.5 | 6.8 ± 0.5 | 4.9 ± 0.5 | 5.0 ± 0.3 |
| Green beans or green peas | 5.1 ± 0.5 | 3.6 ± 0.6 | 6.5 ± 0.5 | 5.5 ± 0.5 | 10.2 ± 0.6 | 5.6 ± 0.5 | 6.3 ± 0.3 |
| Spinach, cooked | 2.6 ± 0.3 | 0.6 ± 0.4 | 1.3 ± 0.3 | 1.9 ± 0.3 | 4.5 ± 0.4 | 0.6 ± 0.3 | 1.2 ± 0.2 |
| Greens (collards, turnip, or mustard) | 0.6 ± 0.3 | 1.0 ± 0.4 | 3.3 ± 0.4 | 0.9 ± 0.3 | 4.8 ± 0.4 | 3.1 ± 0.3 | 2.3 ± 0.2 |
| Sweet potatoes, yams | 1.4 ± 0.2 | 0.8 ± 0.3 | 1.8 ± 0.2 | 0.8 ± 0.2 | 3.3 ± 0.3 | 1.4 ± 0.2 | 1.3 ± 0.1 |
| Fried potatoes (French fries, home fries, hash browns) | 3.0 ± 0.6 | 13.1 ± 0.7 | 4.6 ± 0.6 | 8.9 ± 0.6 | 4.0 ± 0.7 | 11.7 ± 0.6 | 7.6 ± 0.3 |
| Cole slaw, cabbage, Chinese cabbage | 1.00 ± 0.2 | 0.7 ± 0.3 | 2.0 ± 0.3 | 0.8 ± 0.3 | 4.1 ± 0.3 | 1.7 ± 0.2 | 1.6 ± 0.1 |
| Green salad, lettuce salad | 13.20 ± 0.6 | 3.9 ± 0.7 | 5.0 ± 0.6 | 10.4 ± 0.6 | 12.1 ± 0.7 | 3.5 ± 0.6 | 7.6 ± 0.3 |
| Tomatoes, raw | 10.40 ± 0.6 | 2.6 ± 0.7 | 2.2 ± 0.6 | 9.7 ± 0.6 | 7.5 ± 0.7 | 2.2 ± 0.6 | 5.3 ± 0.3 |
| Other vegetables (squash, cauliflower, okra, peppers) | 7.00 ± 0.4 | 0.7 ± 0.5 | 1.4 ± 0.5 | 5.1 ± 0.5 | 8.4 ± 0.5 | 1.0 ± 0.4 | 2.7 ± 0.2 |
| Pinto, black or baked beans, chili with beans | 3.30 ± 0.3 | 1.6 ± 0.3 | 1.3 ± 0.3 | 2.9 ± 0.3 | 2.3 ± 0.3 | 1.6 ± 0.3 | 2.2 ± 0.1 |
| Vegetable, vegetable-beef or tomato soup | 2.1 ± 0.2 | 0.6 ± 0.3 | 1.2 ± 0.2 | 1.2 ± 0.2 | 2.3 ± 0.3 | 0.7 ± 0.2 | 1.5 ± 0.1 |
| BREADS | |||||||
| Sandwich buns | 3.0 ± 0.5 | 9.4 ± 0.5 | 3.1 ± 0.5 | 7.1 ± 0.5 | 2.5 ± 0.5 | 6.6 ± 0.5 | 5.5 ± 0.3 |
| Bagels, English muffins, dinner rolls | 4.8 ± 0.4 | 2.2 ± 0.5 | 1.6 ± 0.5 | 6.1 ± 0.5 | 3.6 ± 0.5 | 1.9 ± 0.4 | 3.7 ± 0.2 |
| Cornbread, corn muffins, hush puppies | 0.6 ± 0.3 | 2.0 ± 0.4 | 2.1 ± 0.3 | 1.1 ± 0.3 | 2.3 ± 0.4 | 3.8 ± 0.3 | 2.5 ± 0.2 |
| Sliced bread (white, dark, whole wheat) | 12.6 ± 0.8 | 15.8 ± 1.0 | 8.3 ± 0.9 | 16.2 ± 0.9 | 11.1 ± 1 | 11.2 ± 0.8 | 12.2 ± 0.5 |
| CONDIMENTS | |||||||
| Salad dressing, regular or low fat | 12.1 ± 0.6 | 4.9 ± 0.7 | 5.2 ± 0.7 | 10.7 ± 0.7 | 11.9 ± 0.7 | 4.4 ± 0.6 | 8.5 ± 0.3 |
| Mayonnaise, sandwich breads | 3.3 ± 0.6 | 9.8 ± 0.7 | 3.5 ± 0.7 | 6.9 ± 0.6 | 4 ± 0.7 | 8.7 ± 0.6 | 6.1 ± 0.3 |
| Ketchup, salsa or chili peppers | 6.3 ± 0.6 | 11.9 ± 0.7 | 3.4 ± 0.7 | 11 ± 0.6 | 3.7 ± 0.7 | 9 ± 0.6 | 6.7 ± 0.3 |
| Mustard, barbecue sauce, soy sauce, gravy, etc. | 6.3 ± 0.6 | 8.5 ± 0.7 | 3.3 ± 0.6 | 9.3 ± 0.6 | 5.5 ± 0.7 | 6.4 ± 0.6 | 6.0 ± 0.3 |
| SWEETS AND SNACKS | |||||||
| Donuts | 0.7 ± 0.2 | 1.2 ± 0.2 | 0.4 ± 0.2 | 1.6 ± 0.2 | 0.4 ± 0.2 | 1.5 ± 0.2 | 1.1 ± 0.1 |
| Cake, snack cakes, cupcakes, Ho-Hos, pastries | 1.8 ± 0.5 | 8.2 ± 0.5 | 1.5 ± 0.5 | 4.6 ± 0.5 | 1.3 ± 0.5 | 5.3 ± 0.5 | 2.9 ± 0.3 |
| Cookies | 3.6 ± 0.5 | 5.5 ± 0.5 | 1.5 ± 0.5 | 7.1 ± 0.5 | 1.7 ± 0.5 | 4.0 ± 0.5 | 3.7 ± 0.3 |
| Chocolate candy | 4.2 ± 0.6 | 9.6 ± 0.7 | 1.3 ± 0.6 | 8.2 ± 0.6 | 1.9 ± 0.7 | 5.5 ± 0.6 | 4.3 ± 0.3 |
| Candy, hard, skittles, starburst, etc. | 2.3 ± 0.6 | 6.6 ± 0.6 | 2.4 ± 0.6 | 4.8 ± 0.6 | 2.4 ± 0.6 | 6.1 ± 0.6 | 4.3 ± 0.3 |
| Snack chips like potato chips, tortilla chips, Fritos, Doritos, popcorn | 6.3 ± 0.7 | 17.9 ± 0.8 | 4.5 ± 0.7 | 12.1 ± 0.7 | 5.2 ± 0.8 | 14.6 ± 0.7 | 8.7 ± 0.4 |
| MEAT, FISH, POULTRY, MEAT SUSTITUTES | |||||||
| Pizza | 2.7 ± 0.4 | 5.2 ± 0.4 | 2.7 ± 0.4 | 4.6 ± 0.4 | 2.4 ± 0.4 | 5.5 ± 0.4 | 3.7 ± 0.2 |
| Meat substitutes (veggie burgers, chicken, hot dogs or lunch meats) | 1.7 ± 0.2 | 0.0 ± 0.2 | 0 ± 0.2 | 0.8 ± 0.2 | 0.5 ± 0.2 | 0.0 ± 0.2 | 0.2 ± 0.1 |
| Hamburgers or cheese burgers | 1.7 ± 0.4 | 9.0 ± 0.5 | 3.2 ± 0.4 | 4.6 ± 0.4 | 2 ± 0.5 | 7.9 ± 0.4 | 4.2 ± 0.2 |
| Hot dogs or sausage (Polish, Italian or chorizo) | 0.8 ± 0.3 | 3.9 ± 0.4 | 2.6 ± 0.4 | 2.0 ± 0.4 | 1.9 ± 0.4 | 5.8 ± 0.3 | 2.6 ± 0.2 |
| Lunch meats (turkey or regular) | 4.8 ± 0.6 | 9.5 ± 0.7 | 4.1 ± 0.6 | 7.8 ± 0.6 | 4.6 ± 0.7 | 9.0 ± 0.6 | 6.2 ± 0.3 |
| Tacos, burritos, enchiladas, tamales with meat or chicken | 2.2 ± 0.3 | 3.8 ± 0.3 | 1.8 ± 0.3 | 3.8 ± 0.3 | 1.8 ± 0.3 | 3.4 ± 0.3 | 2.7 ± 0.2 |
| Ribs, spareribs | 0.2 ± 0.1 | 0.5 ± 0.1 | 0.6 ± 0.1 | 0.2 ± 0.1 | 0.5 ± 0.1 | 1.2 ± 0.1 | 0.6 ± 0.1 |
| Liver (chicken livers or liverwurst) | 0.1 ± 0.1 | 0.1 ± 0.1 | 0.2 ± 0.1 | 0.0 ± 0.1 | 0.7 ± 0.1 | 0.3 ± 0.1 | 0.2 ± 0.1 |
| Pig’s feet, neck bones, oxtails, tongue | 0.0 ± 0.1 | 0.2 ± 0.1 | 0.4 ± 0.1 | 0.0 ± 0.1 | 0.2 ± 0.1 | 0.8 ± 0.1 | 0.2 ± 0.1 |
| Beef or pork dishes (beef stew, pot pie, hamburger helper) | 0.6 ± 0.1 | 1.5 ± 0.2 | 1.8 ± 0.2 | 0.8 ± 0.2 | 1 ± 0.2 | 2.7 ± 0.2 | 1.3 ± 0.1 |
| Fried chicken (nuggets, wings or patties) | 1.2 ± 0.5 | 8.2 ± 0.6 | 4.4 ± 0.5 | 3.9 ± 0.5 | 3.0 ± 0.6 | 9.5 ± 0.5 | 5.1 ± 0.3 |
| Roasted or broiled chicken or turkey | 5.2 ± 0.4 | 2.6 ± 0.5 | 2.1 ± 0.4 | 4.5 ± 0.4 | 5.9 ± 0.5 | 2.4 ± 0.4 | 3.9 ± 0.2 |
| Fried fish or fish sandwich | 0.3 ± 0.2 | 1.1 ± 0.2 | 1.6 ± 0.2 | 0.6 ± 0.2 | 1.2 ± 0.2 | 2.4 ± 0.2 | 1.4 ± 0.1 |
| Fish not fried | 2.5 ± 0.2 | 0.3 ± 0.2 | 0.4 ± 0.2 | 1.6 ± 0.2 | 1.7 ± 0.2 | 0.3 ± 0.2 | 0.8 ± 0.1 |
| Peanut Butter | 6.7 ± 0.5 | 2.4 ± 0.6 | 1.9 ± 0.6 | 8.6 ± 0.6 | 4.8 ± 0.6 | 2.0 ± 0.5 | 4.1 ± 0.3 |
| Peanuts, sunflower seeds, or other nuts and seeds | 5.5 ± 0.4 | 0.9 ± 0.5 | 1.5 ± 0.5 | 3.7 ± 0.4 | 4.3 ± 0.5 | 1.3 ± 0.4 | 2.3 ± 0.2 |
| BEVERAGES | |||||||
| 100% orange or grapefruit juice | 5.4 ± 0.8 | 8.3 ± 0.9 | 9.4 ± 0.8 | 8.3 ± 0.8 | 12.5 ± 0.9 | 10.5 ± 0.8 | 9.4 ± 0.4 |
| Hi-C, Cranberry Juice Cocktail, Hawaiian Punch, Tang | 0.8 ± 0.6 | 6.6 ± 0.8 | 5.5 ± 0.7 | 2.6 ± 0.7 | 3.3 ± 0.8 | 9.2 ± 0.6 | 4.7 ± 0.4 |
| Kool-aid, lemonade, sports drinks, or fruit flavored drinks | 3.4 ± 0.7 | 10.9 ± 0.9 | 5.8 ± 0.8 | 5.6 ± 0.8 | 3.5 ± 0.9 | 12.8 ± 0.7 | 6.7 ± 0.4 |
| Soft drinks (Coke, Sprite, Orange) regular or diet | 5.9 ± 0.8 | 17.4 ± 0.9 | 2.7 ± 0.8 | 12.6 ± 0.8 | 2.5 ± 0.9 | 11.0 ± 0.8 | 7.5 ± 0.4 |
| Water tap or bottled | 29.9 ± 0.6 | 23 ± 0.7 | 25.3 ± 0.7 | 28.8 ± 0.7 | 29 ± 0.7 | 21.6 ± 0.6 | 26.9 ± 0.3 |
| Coffee, regular or decaffeinated | 9.7 ± 0.6 | 1.7 ± 0.7 | 0.4 ± 0.7 | 7.4 ± 0.7 | 1.2 ± 0.7 | 0.7 ± 0.6 | 2.0 ± 0.3 |
3.3. Characteristics of Participants
| Variable | Healthy | Processed | US Southern | H-P | H-S | P-S | Mixed | p 1 |
|---|---|---|---|---|---|---|---|---|
| N | 135 | 98 | 120 | 123 | 98 | 136 | 445 | |
| Age, y (mean ± SE) | 30.3 ± 0.38 | 24.1 ± 0.49 | 25.2 ± 0.52 | 28.5 ± 4.95 | 27.7 ± 0.74 | 23.4 ± 0.40 | 26.2 ± 0.24 | <0.0001 |
| Height, cm (mean ± SE) | 166 ± 0.64 | 163 ± 0.79 | 163 ± 0.65 | 164 ± 0.67 | 166 ± 0.74 | 163 ± 0.59 | 164 ± 0.24 | 0.0009 |
| Pre-pregnancy weight, kg (mean ± SE) | 68.3 ± 1.40 | 75.1 ± 2.35 | 78.1 ± 2.45 | 72.4 ± 1.69 | 77.5 ± 2.10 | 71.9 ± 1.82 | 76.2 ± 0.99 | 0.0005 |
| Race, n (%) | ||||||||
| Caucasian | 121 (90) | 19 (19) | 8 (7) | 97 (79) | 13 (13) | 3 (2) | 140 (32) | <0.001 |
| African American | 7 (5) | 79 (81) | 110 (92) | 24 (20) | 74 (76) | 131 (98) | 294 (66) | |
| Other | 7 (5) | 0 (0) | 2 (2) | 2 (2) | 11 (11) | 0 (0) | 9 (2) | |
| Ethnicity, n (%) | ||||||||
| Hispanic | 3 (2) | 0 (0) | 1 (1) | 4 (3) | 2 (2) | 1 (1) | 15 (3) | 0.2424 |
| Non-Hispanic | 132 (98) | 97 (100) | 119 (99) | 117 (97) | 95 (98) | 133 (99) | 425 (97) | |
| Pre-pregnancy BMI 2, n (%) | ||||||||
| Underweight | 7 (5) | 3 (3) | 5 (4) | 1 (1) | 3 (3) | 9 (7) | 19 (4) | 0.0044 |
| Normal | 83 (61) | 38 (39) | 48 (40) | 64 (52) | 37 (38) | 55 (40) | 146 (33) | |
| Overweight | 19 (14) | 25 (25) | 17 (14) | 28 (23) | 23 (23) | 36 (26) | 134 (30) | |
| Obese | 26 (19) | 32 (33) | 47 (39) | 30 (24) | 35 (36) | 36 (26) | 145 (33) | |
| Parity, n (%) | ||||||||
| Primipara | 66 (49) | 44 (45) | 57 (48) | 49 (40) | 37 (38) | 47 (65) | 189 (42) | 0.2051 |
| Multipara | 69 (51) | 54 (55) | 63 (53) | 74 (60) | 61 (62) | 89 (35) | 256 (58) | |
| Education, n (%) | ||||||||
| Less than high school | 0 (0) | 16 (16) | 16 (13) | 3 (2) | 7 (7) | 29 (21) | 37 (8) | <0.0001 |
| High school or GED | 23 (17) | 55 (56) | 62 (52) | 37 (30) | 41 (42) | 80 (59) | 216 (49) | |
| Technical school | 8 (6) | 10 (10) | 12 (10) | 9 (7) | 11 (11) | 17 (13) | 49 (11) | |
| College or professional | 102 (77) | 17 (17) | 30 (25) | 74 (60) | 39 (40) | 9 (7) | 143 (32) | |
| Marital Status, n (%) | ||||||||
| Single | 5 (4) | 53 (54) | 71 (59) | 12 (10) | 39 (40) | 84 (62) | 160 (36) | <0.0001 |
| Co-habitation | 127 (95) | 43 (44) | 45 (38) | 110 (90) | 54 (54) | 48 (35) | 272 (61) | |
| Do not know | 2 (1) | 2 (2) | 4 (3) | 0 (0) | 4 (4) | 4 (3) | 12 (3) | |
| Household size, (mean ± SE) | 3.9 ± 0.1 | 4.7 ± 0.2 | 4.4 ± 1.2 | 4.1 ± 0.1 | 4.2 ± 0.2 | 4.6 ± 0.2 | 4.3 ± 0.1 | 0.0188 |
| Insurance, n (%) | ||||||||
| Medicaid (Tenncare) | 17 (13) | 69 (70) | 78 (65) | 31 (25) | 50 (51) | 118 (87) | 246 (55) | <0.0001 |
| Other | 117 (87) | 28 (29) | 39 (33) | 92 (75) | 44 (45) | 17 (13) | 188 (42) | |
| Missing | 1 (0) | 1 (1) | 3 (2) | 0 (0) | 4 (4) | 1 (0) | 11 (3) |
| Nutrient | Healthy (n = 135) | Processed (n = 98) | Southern (n = 120) | H-P (n = 123) | H-S (n = 98) | P-S (n = 136) | Mixed (n = 445) | ANCOVA 1 p |
|---|---|---|---|---|---|---|---|---|
| Energy (kcal/day) | 1801 ± 73.4 a | 2958 ± 86.2 b | 1887 ± 77.9 a | 2579 ± 76.9 c | 2347 ± 86.2 c | 3081 ± 73.2 b | 2360 ± 40.5 c | <0.0001 |
| Fat (% of E) | 34.3 ± 0.43 | 37.6 ± 0.50 | 36.3 ± 0.46 | 36.6 ± 0.45 | 35.8 ± 0.50 | 37.9 ± 0.43 | 36.3 ± 0.24 | <0.0001 |
| Protein (% of E) | 16.5 ± 0.20 | 13.5 ± 0.24 | 14.8 ± 0.21 | 14.9 ± 0.21 | 15.9 ± 0.24 | 14.2 ± 0.20 | 14.9 ± 0.11 | <0.0001 |
| Carbohydrate (% of E) | 52.0 ± 0.56 | 50.4 ± 0.66 | 50.9 ± 0.59 | 50.5 ± 0.59 | 50.7 ± 0.66 | 49.2 ± 0.56 | 50.7 ± 0.31 | 0.0351 |
| Saturated fat (g) | 30.1 ± 0.50 | 33.6 ± 0.59 | 32.5 ± 0.53 | 32.2 ± 0.51 | 29.9 ± 0.58 | 34.0 ± 0.51 | 32.0 ± 0.27 | <0.0001 |
| Omega 3 fatty acids (g) | 2.17 ± 0.05 b | 1.75 ± 0.06 c | 2.09 ± 0.06 b | 2.08 ± 0.05 b | 2.44 ± 0.06 a | 1.82 ± 0.05 c | 2.10 ± 0.03 b | <0.0001 |
| Total Sugar (g) | 10.6 ± 0.64 | 21.7 ± 0.75 | 13.2 ± 0.68 | 16.5 ± 0.67 | 8.60 ± 0.75 | 19.4 ± 0.64 | 15.2 ± 0.35 | <0.0001 |
| Fiber (g) | 27.4 ± 0.48 | 15.4 ± 0.55 | 20.8 ± 0.50 | 22.3 ± 0.49 | 26.0 ± 0.54 | 15.2 ± 0.48 | 20.5 ± 0.26 | <0.0001 |
| Fe (mg) | 19.2 ± 0.32 a,b | 15.6 ± 0.37 d | 17.6 ± 0.34 c | 17.9 ± 0.33 b,c | 19.5 ± 0.37 a | 16.1 ± 0.32 d | 17.7 ± 0.17 c | <0.0001 |
| Zn (mg) | 14.3 ± 0.23 | 12.2 ± 0.26 | 12.9 ± 0.24 | 13.3 ± 0.23 | 13.5 ± 0.26 | 12.5 ± 0.23 | 13.2 ± 0.12 | <0.0001 |
| Vit B6 (mg) | 2.69 ± 0.05 a | 1.93 ± 0.06 c | 2.37 ± 0.05 b | 2.40 ± 0.05 b | 2.72 ± 0.06 a | 2.03 ± 0.05 c | 2.33 ± 0.03 b | <0.0001 |
| Vit B12 (μg) | 6.54 ± 0.20 ab | 5.00 ± 0.23 d | 6.01 ± 0.20 a,b,c | 5.64 ± 0.20 c,d | 6.69 ± 0.22 a | 5.76 ± 0.20 b,c,d | 6.03 ± 0.10 a,b,c | <0.0001 |
| Folate (μg) | 777 ± 17.0 | 544 ± 19.7 | 656 ± 17.9 | 715 ± 17.4 | 775 ± 19.4 | 559 ± 17.1 | 671 ± 9.11 | <0.0001 |
| Thiamine (mg) | 2.09 ± 0.03 a | 1.62 ± 0.04 d | 1.95 ± 0.03 b | 1.89 ± 0.03 b,c | 2.10 ± 0.04 a | 1.76 ± 0.03 c,d | 1.91 ± 0.02 b | <0.0001 |
| Niacin (mg) | 27.4 ± 0.45 a | 23.0 ± 0.53 d | 24.7 ± 0.48 c,d | 25.8 ± 0.46 a,b,c | 27.1 ± 0.52 a,b | 24.0 ± 0.46 c,d | 25.5 ± 0.24 b,c | <0.0001 |
| Riboflavin (mg) | 2.77 ± 0.04 a | 2.00 ± 0.05 d | 2.40 ± 0.05 c | 2.46 ± 0.04 b,c | 2.65 ± 0.05 a,b | 2.11 ± 0.04 d | 2.42 ± 0.02 c | <0.0001 |
| Total Choline (mg) | 386 ± 7.08 b | 272 ± 8.22 f | 377 ± 7.44 b,c | 334 ± 7.23 d,e | 435 ± 8.08 a | 328 ± 7.11 e | 354 ± 3.79 c,d | <0.0001 |
| Free Choline (mg) | 98.3 ± 1.33 a | 63.8 ± 1.54 d | 79.5 ± 1.39 c | 88.2 ± 1.35 b | 94.0 ± 1.51 a,b | 65.9 ± 1.33 d | 81.9 ± 0.71 c | <0.0001 |
4. Discussion
5. Conclusions
Acknowledgments
Conflict of Interest
References
- Barker, D.J. The fetal origins of adult hypertension. J. Hypertens. 1992, 10, S39–S44. [Google Scholar]
- Barker, D.J. The fetal origins of diseases of old age. Eur. J. Clin. Nutr. 1992, 46, S3–S9. [Google Scholar]
- Barker, D.J.; Martyn, C.N. The maternal and fetal origins of cardiovascular disease. J. Epidemiol. Community Health 1992, 46, 8–11. [Google Scholar]
- Christian, P. Micronutrients, birth weight, and survival. Annu. Rev. Nutr. 2010, 30, 83–104. [Google Scholar]
- Haider, B.A.; Yakoob, M.Y.; Bhutta, Z.A. Effect of multiple micronutrient supplementation during pregnancy on maternal and birth outcomes. BMC Public Health 2011, 11. [Google Scholar] [CrossRef]
- Gecz, J.; Mulley, J. Genes for cognitive function: Developments on the X. Genome Res. 2000, 10, 157–163. [Google Scholar]
- Newby, P.K.; Tucker, K.L. Empirically derived eating patterns using factor or cluster analysis: A review. Nutr. Rev. 2004, 62, 177–203. [Google Scholar]
- Dixon, L.B.; Balder, H.F.; Virtanen, M.J.; Rashidkhani, B.; Mannisto, S.; Krogh, V.; van Den Brandt, P.A.; Hartman, A.M.; Pietinen, P.; Tan, F.; et al. Dietary patterns associated with colon and rectal cancer: Results from the Dietary Patterns and Cancer (DIETSCAN) Project. Am. J. Clin. Nutr. 2004, 80, 1003–1011. [Google Scholar]
- Fung, T.; Hu, F.B.; Fuchs, C.; Giovannucci, E.; Hunter, D.J.; Stampfer, M.J.; Colditz, G.A.; Willett, W.C. Major dietary patterns and the risk of colorectal cancer in women. Arch. Intern. Med. 2003, 163, 309–314. [Google Scholar]
- Slattery, M.L.; Boucher, K.M.; Caan, B.J.; Potter, J.D.; Ma, K.N. Eating patterns and risk of colon cancer. Am. J. Epidemiol. 1998, 148, 4–16. [Google Scholar]
- Gittelsohn, J.; Wolever, T.M.; Harris, S.B.; Harris-Giraldo, R.; Hanley, A.J.; Zinman, B. Specific patterns of food consumption and preparation are associated with diabetes and obesity in a Native Canadian community. J. Nutr. 1998, 128, 541–547. [Google Scholar]
- Van Dam, R.M.; Rimm, E.B.; Willett, W.C.; Stampfer, M.J.; Hu, F.B. Dietary patterns and risk for type 2 diabetes mellitus in U.S. men. Ann. Intern. Med. 2002, 136, 201–209. [Google Scholar]
- Fung, T.T.; Stampfer, M.J.; Manson, J.E.; Rexrode, K.M.; Willett, W.C.; Hu, F.B. Prospective study of major dietary patterns and stroke risk in women. Stroke 2004, 35, 2014–2019. [Google Scholar]
- Northstone, K.; Emmett, P.; Rogers, I. Dietary patterns in pregnancy and associations with socio-demographic and lifestyle factors. Eur. J. Clin. Nutr. 2008, 62, 471–479. [Google Scholar]
- Northstone, K.; Emmett, P.M.; Rogers, I. Dietary patterns in pregnancy and associations with nutrient intakes. Br. J. Nutr. 2008, 99, 406–415. [Google Scholar]
- Knudsen, V.K.; Orozova-Bekkevold, I.M.; Mikkelsen, T.B.; Wolff, S.; Olsen, S.F. Major dietary patterns in pregnancy and fetal growth. Eur. J. Clin. Nutr. 2008, 62, 463–470. [Google Scholar]
- Elder, G.H., Jr. The life course as developmental theory. Child Dev. 1998, 69, 1–12. [Google Scholar]
- Bourre, J.M. Effects of nutrients (in food) on the structure and function of the nervous system: Update on dietary requirements for brain. Part 1: Micronutrients. J. Nutr. Health Aging 2006, 10, 377–385. [Google Scholar]
- Block, G.; Coyle, L.M.; Hartman, A.M.; Scoppa, S.M. Revision of dietary analysis software for the Health Habits and History Questionnaire. Am. J. Epidemiol. 1994, 139, 1190–1196. [Google Scholar]
- Mares-Perlman, J.A.; Klein, B.E.; Klein, R.; Ritter, L.L.; Fisher, M.R.; Freudenheim, J.L. A diet history questionnaire ranks nutrient intakes in middle-aged and older men and women similarly to multiple food records. J. Nutr. 1993, 123, 489–501. [Google Scholar]
- Johnson, B.A.; Herring, A.H.; Ibrahim, J.G.; Siega-Riz, A.M. Structured measurement error in nutritional epidemiology: Applications in the Pregnancy, Infection, and Nutrition (PIN) Study. J. Am. Stat. Assoc. 2007, 102, 856–866. [Google Scholar]
- Subar, A.F.; Thompson, F.E.; Kipnis, V.; Midthune, D.; Hurwitz, P.; McNutt, S.; McIntosh, A.; Rosenfeld, S. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: The Eating at America’s Table Study. Am. J. Epidemiol. 2001, 154, 1089–1099. [Google Scholar]
- Block, G.; Hartman, A.M.; Dresser, C.M.; Carroll, M.D.; Gannon, J.; Gardner, L. A data-based approach to diet questionnaire design and testing. Am. J. Epidemiol. 1986, 124, 453–469. [Google Scholar]
- Willet, W. Nutritional Epidemiology, 2nd ed; Oxford University Press: New York, NY, USA, 1998. [Google Scholar]
- IOM, Weight Gain During Pregnancy: Reexamining the Guidelines; The National Academies Press: Washington, DC, USA, 2009.
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240–1243. [Google Scholar]
- Cole, T.J.; Flegal, K.M.; Nicholls, D.; Jackson, A.A. Body mass index cut offs to define thinness in children and adolescents: International survey. BMJ. 2007, 335. [CrossRef]
- Satia, J.A. Dietary acculturation and the nutrition transition: An overview. Appl. Physiol. Nutr. Metab. 2010, 35, 219–223. [Google Scholar]
- Bourre, J.M. Effects of nutrients (in food) on the structure and function of the nervous system: Update on dietary requirements for brain. Part 2: Macronutrients. J. Nutr. Health Aging 2006, 10, 386–399. [Google Scholar]
- Bovell-Benjamin, A.C.; Dawkin, N.; Pace, R.D.; Shikany, J.M. Use of focus groups to understand African-Americans’ dietary practices: Implications for modifying a food frequency questionnaire. Prev. Med. 2009, 48, 549–554. [Google Scholar]
- Smith, S.L.; Quandt, S.A.; Arcury, T.A.; Wetmore, L.K.; Bell, R.A.; Vitolins, M.Z. Aging and eating in the rural, southern United States: Beliefs about salt and its effect on health. Soc. Sci. Med. 2006, 62, 189–198. [Google Scholar]
- Tucker, K.L.; Maras, J.; Champagne, C.; Connell, C.; Goolsby, S.; Weber, J.; Zaghloul, S.; Carithers, T.; Bogle, M.L. A regional food-frequency questionnaire for the US Mississippi Delta. Public Health Nutr. 2005, 8, 87–96. [Google Scholar]
- Jefferson, W.K.; Zunker, C.; Feucht, J.C.; Fitzpatrick, S.L.; Greene, L.F.; Shewchuk, R.M.; Baskin, M.L.; Walton, N.W.; Phillips, B.; Ard, J.D. Use of the Nominal Group Technique (NGT) to understand the perceptions of the healthiness of foods associated with African Americans. Eval. Program Plann. 2010, 33, 343–348. [Google Scholar]
- Popkin, B.M. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. Am. J. Clin. Nutr. 2006, 84, 289–298. [Google Scholar]
- Smith, A.D.; Emmett, P.M.; Newby, P.K.; Northstone, K. A comparison of dietary patterns derived by cluster and principal components analysis in a UK cohort of children. Eur. J. Clin. Nutr. 2011, 65, 1102–1109. [Google Scholar]
- Sotres-Alvarez, D.; Herring, A.H.; Siega-Riz, A.M. Latent class analysis is useful to classify pregnant women into dietary patterns. J. Nutr. 2010, 140, 2253–2259. [Google Scholar]
- Tseng, M.; DeVellis, R.F.; Maurer, K.R.; Khare, M.; Kohlmeier, L.; Everhart, J.E.; Sandler, R.S. Food intake patterns and gallbladder disease in Mexican Americans. Public Health Nutr. 2000, 3, 233–243. [Google Scholar]
- Tucker, K.L. Dietary patterns, approaches, and multicultural perspective. Appl. Physiol. Nutr. Metab. 2010, 35, 211–218. [Google Scholar]
- Bailey, R.L.; Mitchell, D.C.; Miller, C.; Smiciklas-Wright, H. Assessing the effect of underreporting energy intake on dietary patterns and weight status. J. Am. Diet. Assoc. 2007, 107, 64–71. [Google Scholar]
- Millen, A.E.; Tooze, J.A.; Subar, A.F.; Kahle, L.L.; Schatzkin, A.; Krebs-Smith, S.M. Differences between food group reports of low-energy reporters and non-low-energy reporters on a food frequency questionnaire. J. Am. Diet. Assoc. 2009, 109, 1194–1203. [Google Scholar]
Supplementary Files
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Völgyi, E.; Carroll, K.N.; Hare, M.E.; Ringwald-Smith, K.; Piyathilake, C.; Yoo, W.; Tylavsky, F.A. Dietary Patterns in Pregnancy and Effects on Nutrient Intake in the Mid-South: The Conditions Affecting Neurocognitive Development and Learning in Early Childhood (CANDLE) Study. Nutrients 2013, 5, 1511-1530. https://doi.org/10.3390/nu5051511
Völgyi E, Carroll KN, Hare ME, Ringwald-Smith K, Piyathilake C, Yoo W, Tylavsky FA. Dietary Patterns in Pregnancy and Effects on Nutrient Intake in the Mid-South: The Conditions Affecting Neurocognitive Development and Learning in Early Childhood (CANDLE) Study. Nutrients. 2013; 5(5):1511-1530. https://doi.org/10.3390/nu5051511
Chicago/Turabian StyleVölgyi, Eszter, Kecia N. Carroll, Marion E. Hare, Karen Ringwald-Smith, Chandrika Piyathilake, Wonsuk Yoo, and Frances A. Tylavsky. 2013. "Dietary Patterns in Pregnancy and Effects on Nutrient Intake in the Mid-South: The Conditions Affecting Neurocognitive Development and Learning in Early Childhood (CANDLE) Study" Nutrients 5, no. 5: 1511-1530. https://doi.org/10.3390/nu5051511




