Cardiovascular Effects of Calcium Supplements
Abstract
:1. Introduction
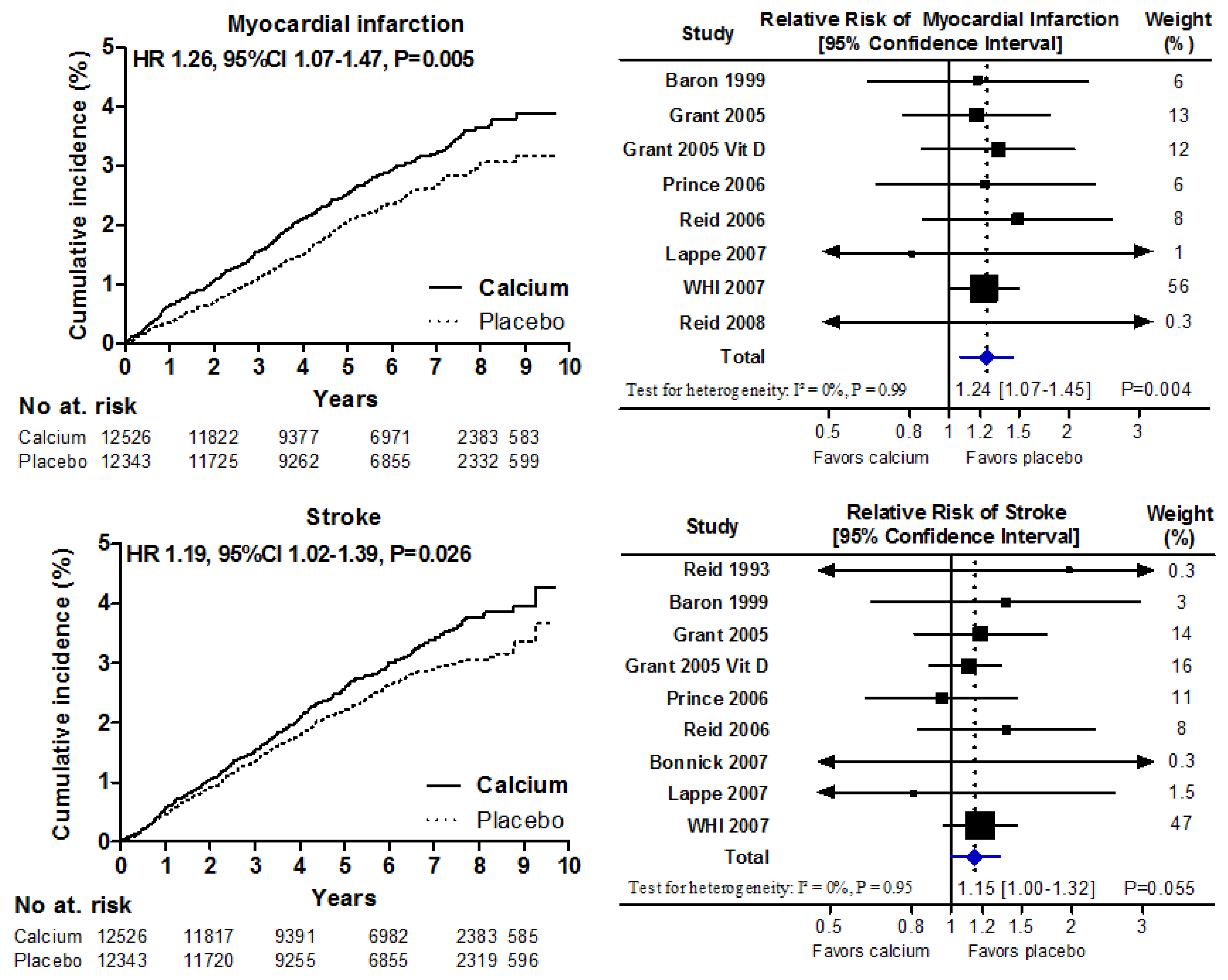
2. Clinical Trials & Meta-Analyses
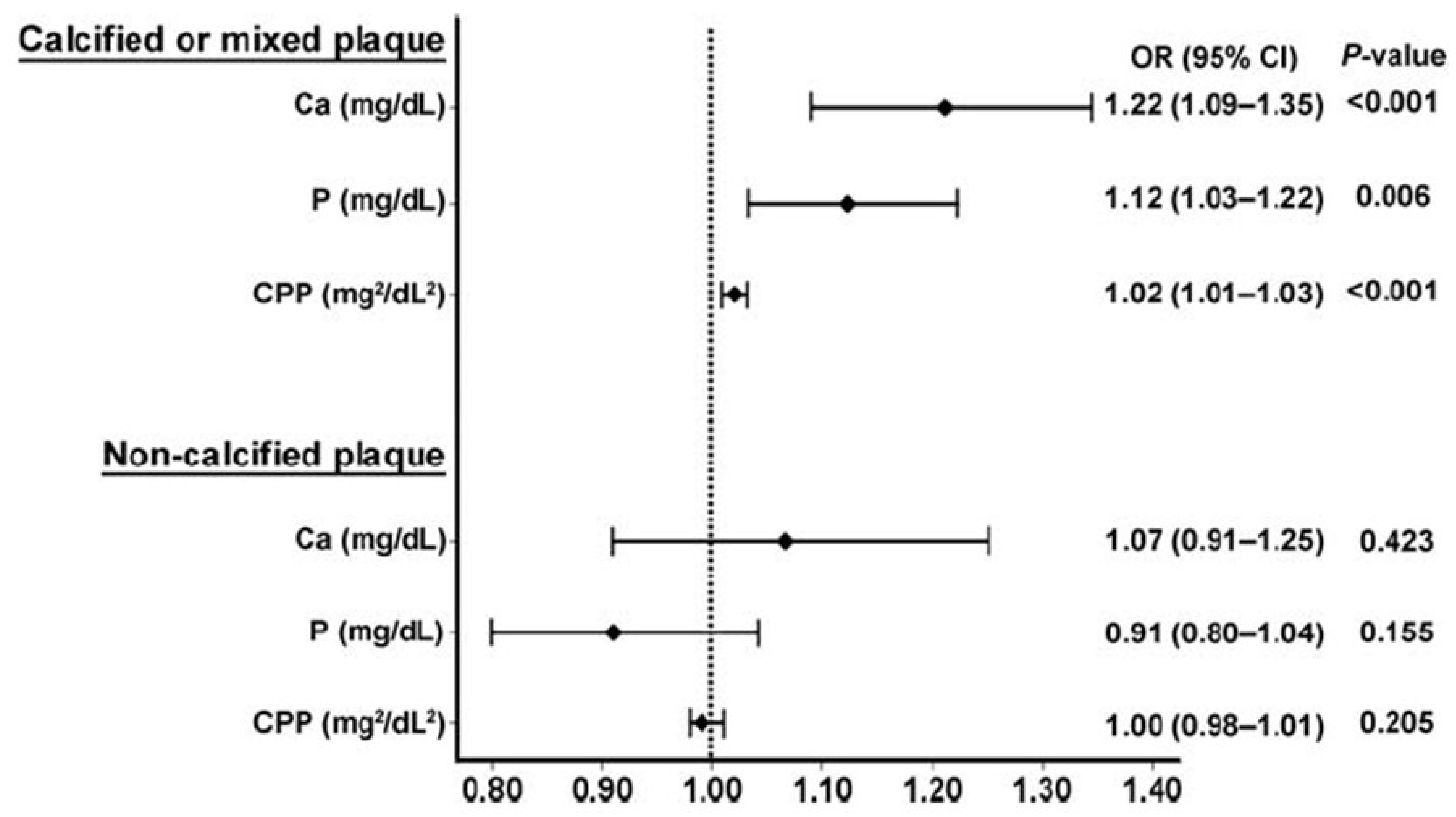
3. Mechanisms
4. Conclusions
Acknowledgments
Conflict of Interest
References
- Bischoff-Ferrari, H.A.; Dawson-Hughes, B.; Baron, J.A.; Burckhardt, P.; Li, R.; Spiegelman, D.; Specker, B.; Orav, J.E.; Wong, J.B.; Staehelin, H.B.; et al. Calcium intake and hip fracture risk in men and women: A meta-analysis of prospective cohort studies and randomized controlled trials. Am. J. Clin. Nutr. 2007, 86, 1780–1790. [Google Scholar]
- Bischoff-Ferrari, H.A.; Kiel, D.P.; Dawson-Hughes, B.; Orav, J.E.; Li, R.F.; Spiegelman, D.; Dietrich, T.; Willett, W.C. Dietary calcium and serum 25-hydroxyvitamin d status in relation to bmd among us adults. J. Bone Miner. Res. 2009, 24, 935–942. [Google Scholar]
- Reid, I.R.; Mason, B.; Horne, A.; Ames, R.; Reid, H.E.; Bava, U.; Bolland, M.J.; Gamble, G.D. Randomized controlled trial of calcium in healthy older women. Am. J. Med. 2006, 119, 777–785. [Google Scholar]
- Reid, I.R.; Bolland, M.J.; Grey, A. Effect of calcium supplementation on hip fractures. Osteoporos. Int. 2008, 19, 1119–1123. [Google Scholar]
- Tang, B.M.P.; Eslick, G.D.; Nowson, C.; Smith, C.; Bensoussan, A. Use of calcium or calcium in combination with vitamin d supplementation to prevent fractures and bone loss in people aged 50 years and older: A meta-analysis. Lancet 2007, 370, 657–666. [Google Scholar] [CrossRef]
- Reid, I.R.; Horne, A.; Mason, B.; Ames, R.; Bava, U.; Gamble, G.D. Effects of calcium supplementation on body weight and blood pressure in normal older women: A randomized controlled trial. J. Clin. Endocrinol. Metab. 2005, 90, 3824–3829. [Google Scholar] [CrossRef]
- Reid, I.R.; Mason, B.; Horne, A.; Clearwater, J.; Bava, U.; Orr-Walker, B.; Wu, F.; Evans, M.C.; Gamble, G.D. Effects of calcium supplementation on serum lipids in normal older women—A randomized controlled trial. Am. J. Med. 2002, 112, 343–347. [Google Scholar] [CrossRef]
- Bolland, M.J.; Barber, P.A.; Doughty, R.N.; Mason, B.; Horne, A.; Ames, R.; Gamble, G.D.; Grey, A.; Reid, I.R. Vascular events in healthy older women receiving calcium supplementation: Randomised controlled trial. BMJ 2008, 336, 262–266. [Google Scholar] [CrossRef]
- Bolland, M.J.; Avenell, A.; Baron, J.A.; Grey, A.; MacLennan, G.S.; Gamble, G.D.; Reid, I.R. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: Meta-analysis. BMJ 2010, 341, C3691. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.; Manson, J.E.; Song, Y.Q.; Sesso, H.D. Systematic review: Vitamin d and calcium supplementation in prevention of cardiovascular events. Ann. Intern. Med. 2010, 152, 315–323. [Google Scholar] [CrossRef]
- Hsia, J.; Heiss, G.; Ren, H.; Allison, M.; Dolan, N.C.; Greenland, P.; Heckbert, S.R.; Johnson, K.C.; Manson, J.E.; Sidney, S.; et al. Calcium/vitamin D supplementation and cardiovascular events. Circulation 2007, 115, 846–854. [Google Scholar] [CrossRef]
- Bolland, M.J.; Grey, A.; Avenell, A.; Gamble, G.D.; Reid, I.R. Calcium/vitamin D supplements and cardiovascular events: A re-analysis of the women’s health initiative limited-access dataset, and meta-analysis of calcium with or without vitamin D. BMJ 2011, 342, d2040. [Google Scholar] [CrossRef] [Green Version]
- Lappe, J.M.; Travers-Gustafson, D.; Davies, K.M.; Recker, R.R.; Heaney, R.P. Vitamin d and calcium supplementation reduces cancer risk: Results of a randomized trial. Am. J. Clin. Nutr. 2007, 85, 1586–1591. [Google Scholar]
- Grant, A.M.; Avenell, A.; Campbell, M.K.; McDonald, A.M.; MacLennan, G.S.; McPherson, G.C.; Anderson, F.H.; Cooper, C.; Francis, R.M.; Donaldson, C.; et al. Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (randomised evaluation of calcium or vitamin D, record): A randomised placebo-controlled trial. Lancet 2005, 365, 1621–1628. [Google Scholar] [CrossRef]
- Sambrook, P.N.; Cameron, I.D.; Chen, J.S.; Cumming, R.G.; Durvasula, S.; Herrmann, M.; Kok, C.; Lord, S.R.; Macara, M.; March, L.M.; et al. Does increased sunlight exposure work as a strategy to improve vitamin D status in the elderly: A cluster randomised controlled trial. Osteoporos. Int. 2012, 23, 615–624. [Google Scholar] [CrossRef]
- Reid, I.R.; Bolland, M.J.; Sambrook, P.N.; Grey, A. Calcium supplementation: Balancing the cardiovascular risks. Maturitas 2011, 69, 289–295. [Google Scholar] [CrossRef]
- Pentti, K.; Tuppurainen, M.T.; Honkanen, R.; Sandini, L.; Kroger, H.; Alhava, E.; Saarikoski, S. Use of calcium supplements and the risk of coronary heart disease in 52–62-year-old women: The kuopio osteoporosis risk factor and prevention study. Maturitas 2009, 63, 73–78. [Google Scholar]
- Li, K.; Kaaks, R.; Linseisen, J.; Rohrmann, S. Associations of dietary calcium intake and calcium supplementation with myocardial infarction and stroke risk and overall cardiovascular mortality in the heidelberg cohort of the european prospective investigation into cancer and nutrition study (epic-heidelberg). Heart 2012, 98, 920–925. [Google Scholar]
- Reynolds, J.L.; Joannides, A.J.; Skepper, J.N.; Mcnair, R.; Schurgers, L.J.; Proudfoot, D.; Jahnen-Dechent, W.; Weissberg, P.L.; Shanahan, C.M. Human vascular smooth muscle cells undergo vesicle-mediated calcification in response to changes in extracellular calcium and phosphate concentrations: A potential mechanism for accelerated vascular calcification in esrd. J. Am. Soc. Nephrol. 2004, 15, 2857–2867. [Google Scholar] [CrossRef]
- Marz, W.; Seelhorst, U.; Wellnitz, B.; Tiran, B.; Obermayer-Pietsch, B.; Renner, W.; Boehm, B.O.; Ritz, E.; Hoffmann, M.M. Alanine to serine polymorphism at position 986 of the calcium-sensing receptor associated with coronary heart disease, myocardial infarction, all-cause, and cardiovascular mortality. J. Clin. Endocrinol. Metab. 2007, 92, 2363–2369. [Google Scholar]
- Rubin, M.R.; Rundek, T.; McMahon, D.J.; Lee, H.-S.; Sacco, R.L.; Silverberg, S.J. Carotid artery plaque thickness is associated with increased serum calcium levels: The northern manhattan study. Atherosclerosis 2007, 194, 426–432. [Google Scholar] [CrossRef]
- Bolland, M.J.; Wang, T.K.M.; van Pelt, N.C.; Horne, A.M.; Mason, B.H.; Ames, R.W.; Grey, A.B.; Ruygrok, P.N.; Gamble, G.D.; Reid, I.R. Abdominal aortic calcification on vertebral morphometry images predicts incident myocardial infarction. J. Bone Miner. Res. 2010, 25, 505–512. [Google Scholar]
- Shin, S.; Kim, K.-J.; Chang, H.-J.; Cho, I.; Kim, Y.J.; Choi, B.-W.; Rhee, Y.; Lim, S.-K.; Yang, W.-I.; Shim, C.-Y.; et al. Impact of serum calcium and phosphate on coronary atherosclerosis detected by cardiac computed tomography. Eur. Heart J. 2012, 33, 2873–2881. [Google Scholar]
- Slinin, Y.; Blackwell, T.; Ishani, A.; Cummings, S.R.; Ensrud, K.E. Serum calcium, phosphorus and cardiovascular events in post-menopausal women. Int. J. Cardiol. 2011, 149, 335–340. [Google Scholar] [CrossRef]
- Lind, L.; Skarfors, E.; Berglund, L.; Lithell, H.; Ljunghall, S. Serum calcium: A new, independent, prospective risk factor for myocardial infarction in middle-aged men followed for 18 years. J. Clin. Epidemiol. 1997, 50, 967–973. [Google Scholar] [CrossRef]
- Leifsson, B.G.; Ahren, B. Serum calcium and survival in a large health screening program. J. Clin. Endocrinol. Metab. 1996, 81, 2149–2153. [Google Scholar] [CrossRef]
- Larsson, T.E.; Olauson, H.; Hagstrom, E.; Ingelsson, E.; Arnlov, J.; Lind, L.; Sundstrom, J. Conjoint effects of serum calcium and phosphate on risk of total, cardiovascular, and noncardiovascular mortality in the community. Arterioscler. Thromb. Vasc. Biol. 2010, 30, 333–339. [Google Scholar]
- Karp, H.J.; Ketola, M.E.; Lamberg-Allardt, C.J.E. Acute effects of calcium carbonate, calcium citrate and potassium citrate on markers of calcium and bone metabolism in young women. Br. J. Nutr. 2009, 102, 1341–1347. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Reid, I.R. Cardiovascular Effects of Calcium Supplements. Nutrients 2013, 5, 2522-2529. https://doi.org/10.3390/nu5072522
Reid IR. Cardiovascular Effects of Calcium Supplements. Nutrients. 2013; 5(7):2522-2529. https://doi.org/10.3390/nu5072522
Chicago/Turabian StyleReid, Ian R. 2013. "Cardiovascular Effects of Calcium Supplements" Nutrients 5, no. 7: 2522-2529. https://doi.org/10.3390/nu5072522



