Breastmilk Production in the First 4 Weeks after Birth of Term Infants
Abstract
:1. Introduction
2. Materials and Methods
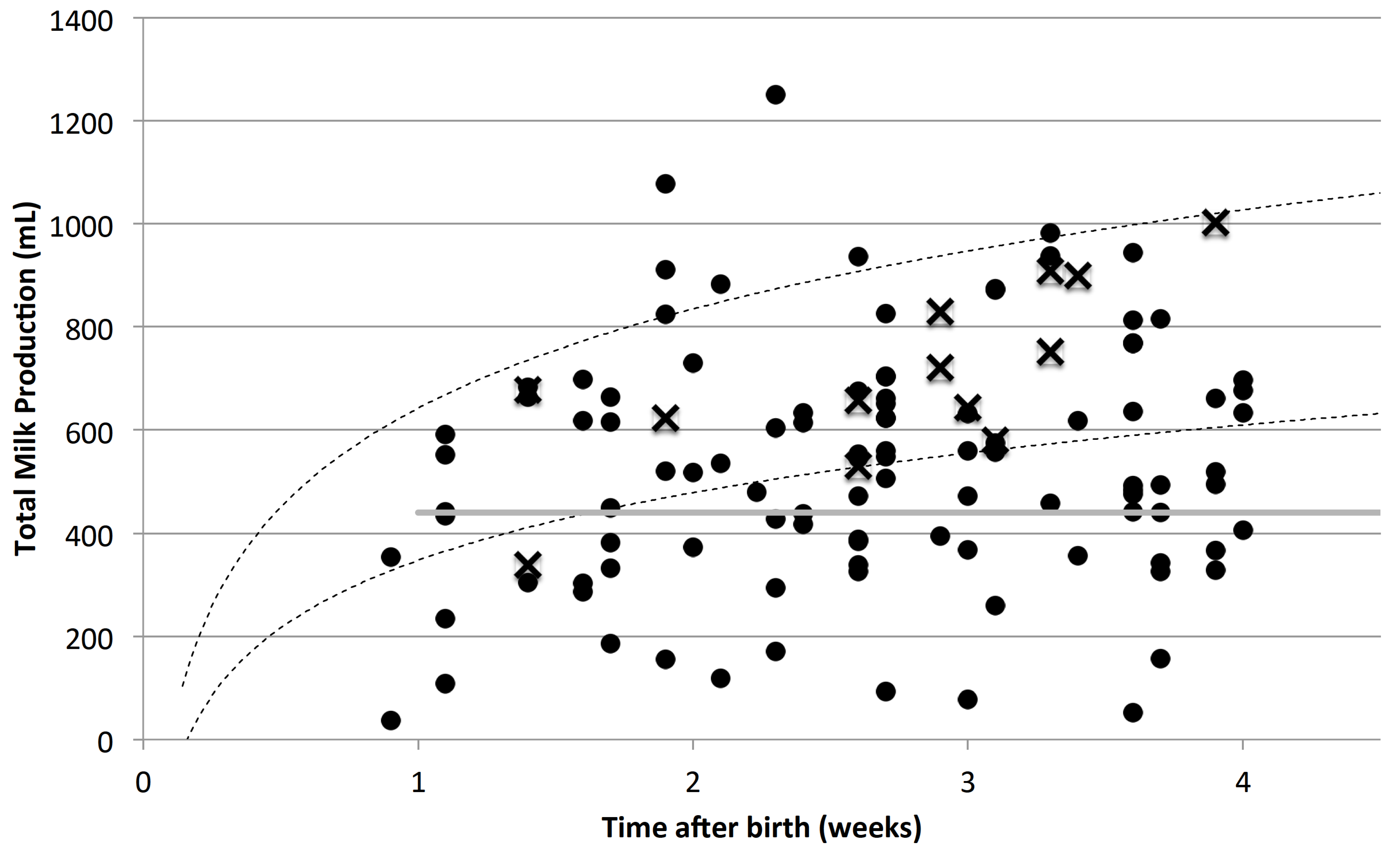
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Allen, J.; Hector, D. Benefits of breastfeeding. N. S. W. Public Health Bull. 2005, 16, 42–46. [Google Scholar] [PubMed]
- Hill, P.D.; Aldag, J.C. Milk volume on day 4 and income predictive of lactation adequacy at 6 weeks of mothers of nonnursing preterm infants. J. Perinat. Neonatal Nurs. 2005, 19, 273–282. [Google Scholar] [CrossRef] [PubMed]
- Hill, P.D.; Aldag, J.C.; Chatterton, R.T.; Zinaman, M. Comparison of milk output between mothers of preterm and term infants: The first 6 weeks after birth. J. Hum. Lact. 2005, 21, 22–30. [Google Scholar] [CrossRef] [PubMed]
- DiGirolamo, A.M.; Grummer-Strawn, L.M.; Fein, S.B. Effect of maternity-care practices on breastfeeding. Pediatrics 2008, 122, S43–S49. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.R.; Anderson, G.C. Randomized controlled trial of very early mother-infant skin-to-skin contact and breastfeeding status. J. Midwifery Womens Health 2007, 52, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.R.; Anderson, G.C.; Bergman, N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst. Rev. 2012. [Google Scholar] [CrossRef] [Green Version]
- Yamauchi, Y.; Yamanouchi, I. Breast-feeding frequency during the first 24 h after birth in full-term neonates. Pediatrics 1990, 86, 171–175. [Google Scholar] [PubMed]
- Kent, J.C.; Mitoulas, L.; Cox, D.B.; Owens, R.A.; Hartmann, P.E. Breast volume and milk production during extended lactation in women. Exp. Physiol. 1999, 84, 435–447. [Google Scholar] [CrossRef] [PubMed]
- Casey, C.E.; Hambidge, K.M.; Neville, M.C. Studies in human lactation: Zinc, copper, manganese and chromium in human milk in the first month of lactation. Am. J. Clin. Nutr. 1985, 41, 1193–1200. [Google Scholar] [PubMed]
- Casey, C.E.; Neifert, M.R.; Seacat, J.M.; Neville, M.C. Nutrient intake by breast-fed infants during the first five days after birth. Am. J. Dis. Child. 1986, 140, 933–936. [Google Scholar] [CrossRef] [PubMed]
- Neville, M.C.; Keller, R.; Seacat, J.; Lutes, V.; Neifert, M.; Casey, C.; Allen, J.; Archer, P. Studies in human lactation: Milk volumes in lactating women during the onset of lactation and full lactation. Am. J. Clin. Nutr. 1988, 48, 1375–1386. [Google Scholar] [PubMed]
- Saint, L.; Smith, M.; Hartmann, P.E. The yield and nutrient content of colostrum and milk of women from giving birth to 1 month post-partum. Br. J. Nutr. 1984, 52, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Evans, K.C.; Evans, R.G.; Royal, R.; Esterman, A.J.; James, S.L. Effect of caesarean section on breast milk transfer to the normal term newborn over the first week of life. Arch. Dis. Child. Fetal Neonatal Ed. 2003, 88, F380–F382. [Google Scholar] [CrossRef] [PubMed]
- Arthur, P.G.; Smith, M.; Hartmann, P.E. Milk lactose, citrate, and glucose as markers of lactogenesis in normal and diabetic women. J. Pediatr. Gastroenterol. Nutr. 1989, 9, 488–496. [Google Scholar] [CrossRef] [PubMed]
- Roderuck, C.; Williams, H.H.; Macy, I.G. Metabolism of women during the reproductive cycle; the utilization of thiamine during lactation. J. Nutr. 1946, 32, 249–265. [Google Scholar] [PubMed]
- Ertem, I.O.; Votto, N.; Leventhal, J.M. The timing and predictors of the early termination of breastfeeding. Pediatrics 2001, 107, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Righard, L. Are breastfeeding problems related to incorrect breastfeeding technique and the use of pacifiers and bottles? Birth 1998, 25, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Segura-Millan, S.; Dewey, K.G.; Perez-Escamilla, R. Factors associated with perceived insufficient milk in a low-income urban population in Mexico. J. Nutr. 1994, 124, 202–212. [Google Scholar] [PubMed]
- Kent, J.C.; Hepworth, A.R.; Langton, D.B.; Hartmann, P.E. Impact of measuring milk production by test weighing on breastfeeding confidence in mothers of term infants. Breastfeed Med. 2015, 10, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Labbok, M.; Krasovec, K. Toward consistency in breastfeeding definitions. Stud. Fam. Plan. 1990, 21, 226–230. [Google Scholar] [CrossRef]
- Prime, D.K.; Garbin, C.P.; Hartmann, P.E.; Kent, J.C. Simultaneous breast expression in breastfeeding women is more efficacious than sequential breast expression. Breastfeed Med. 2012, 7, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Arthur, P.G.; Hartmann, P.E.; Smith, M. Measurement of the milk intake of breast-fed infants. J. Pediatr. Gastroenterol. Nutr. 1987, 6, 758–763. [Google Scholar] [CrossRef] [PubMed]
- R Development Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2011. [Google Scholar]
- Pinheiro, J.; Bates, C.J.; DebRoy, S.; Sarkar, D.; R Development Core Team. Nlme: Linear and Nonlinear Mixed Effects Models, R package version 3.1-102; R Foundation for Statistical Computing: Vienna, Austria, 2011. [Google Scholar]
- Dollberg, S.; Lahav, S.; Mimouni, F.B. A comparison of intakes of breast-fed and bottle-fed infants during the first two days of life. J. Am. Coll. Nutr. 2001, 20, 209–211. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, M.J.; Severo, M.; Santos, A.C. A new approach to estimating weight change and its reference intervals during the first 96 h of life. Acta Paediatr. 2015, 104, 1028–1034. [Google Scholar] [CrossRef] [PubMed]
| Perceived Breastfeeding Problems | p Value | ||
|---|---|---|---|
| No | Yes | ||
| n | 13 | 103 | |
| Birth weight (g) | 3498 (293) | 3450 (3206, 3739) | 0.051 |
| Gestational age at delivery (weeks+days) | 39+2 (1+3) | 39+6 (38+7, 40+3) | 0.025 |
| Feed frequency (breasts) | 12 (3) | 12 (4) | 0.50 |
| Average feed duration (min) | 17 (5) | 15 (13, 21) | 0.052 |
| Average feed amount (mL) | 63 (27) | 30 (20, 45) | <0.001 |
| Total breastfeeding transfer (mL·day−1) | 693 (174) | 399 (211) | <0.001 |
| Total breastmilk expressed (mL·day−1) | 160 (n = 1) | 168 (78, 272) (n = 68) | |
| Supplementary infant formula (mL·day−1) | 0 | 135 (80, 272) (n = 72) | |
| Total infant milk intake (mL·day−1) | 699 (168) | 567 (164) | 0.007 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kent, J.C.; Gardner, H.; Geddes, D.T. Breastmilk Production in the First 4 Weeks after Birth of Term Infants. Nutrients 2016, 8, 756. https://doi.org/10.3390/nu8120756
Kent JC, Gardner H, Geddes DT. Breastmilk Production in the First 4 Weeks after Birth of Term Infants. Nutrients. 2016; 8(12):756. https://doi.org/10.3390/nu8120756
Chicago/Turabian StyleKent, Jacqueline C., Hazel Gardner, and Donna T. Geddes. 2016. "Breastmilk Production in the First 4 Weeks after Birth of Term Infants" Nutrients 8, no. 12: 756. https://doi.org/10.3390/nu8120756




