Maternal Vitamin D Status and Adverse Birth Outcomes in Children from Rural Western Kenya
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Study Participants
2.3. Anthropometric Measurements
2.4. Blood Sample Collection, Processing, and Preservation
2.5. Standard of Care
2.6. Assessment of Pregnancy Outcomes
2.7. Statistical Analysis
3. Results
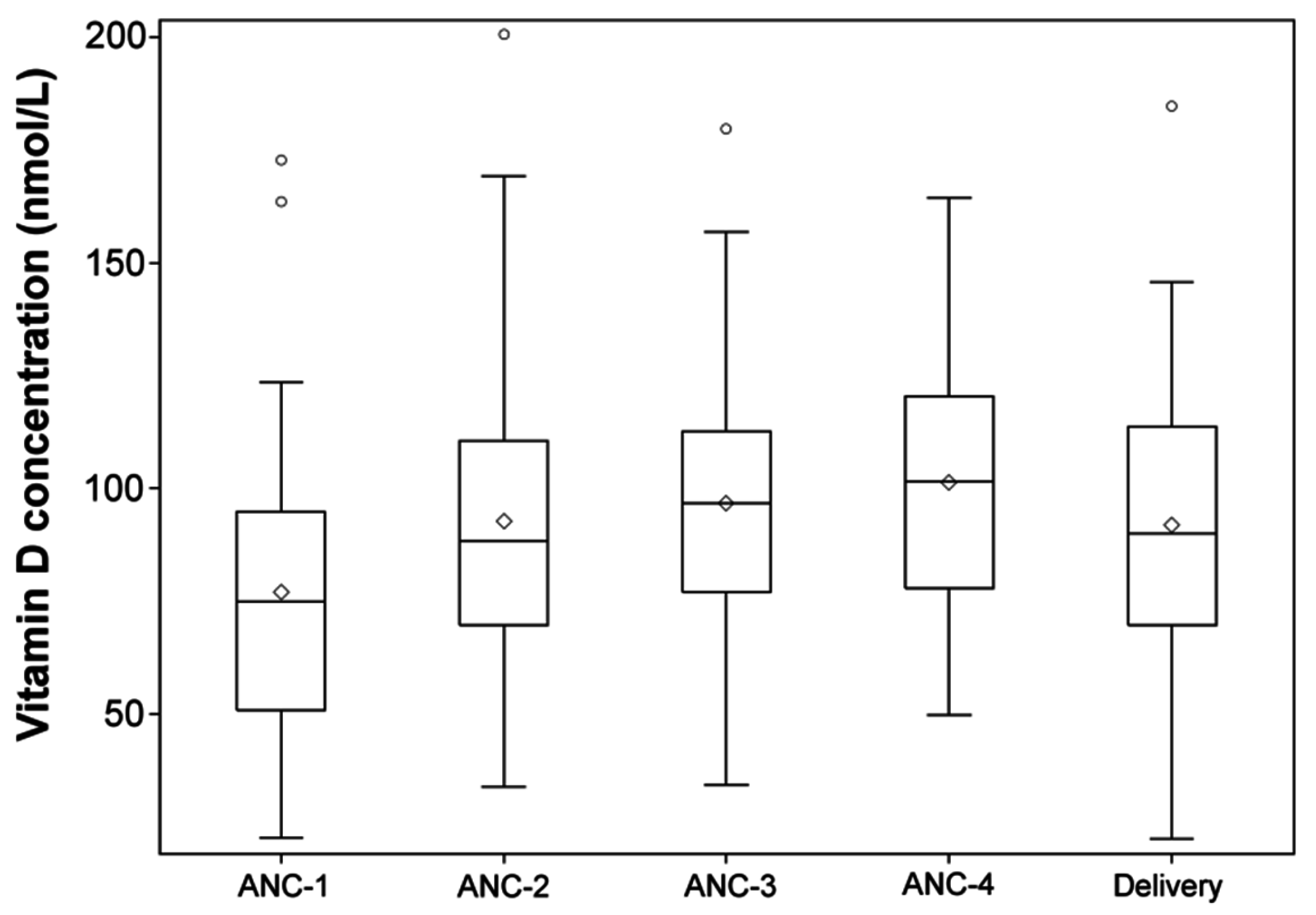
3.1. Varying Maternal and Infant’s Plasma 25(OH)D Concentrations
3.2. Newborns’ Anthropometric Measurements
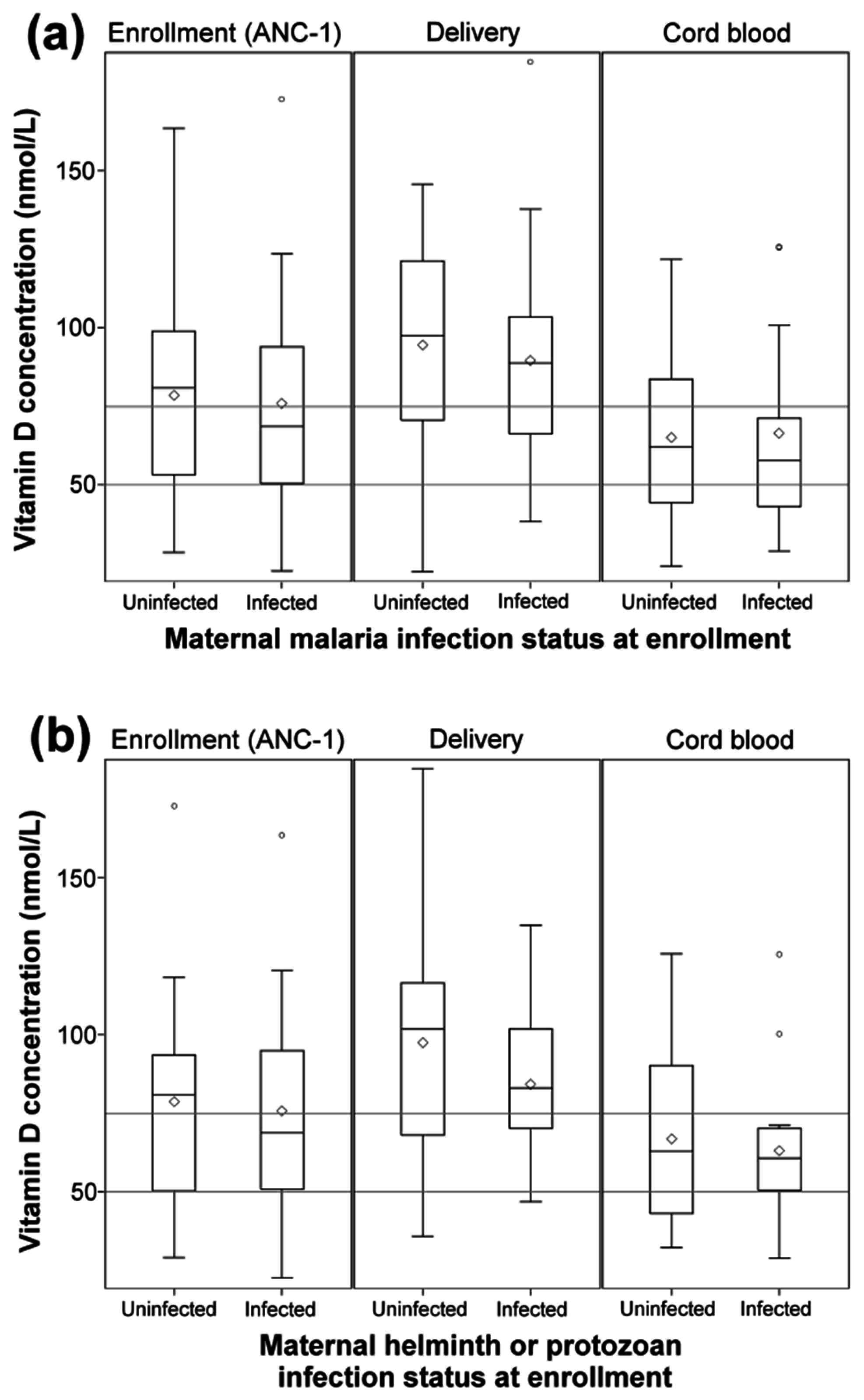
3.3. Protozoa and Helminth Infection Status of Mothers Is Not Associated with Plasma 25(OH)D Levels in Mothers or Their Infants
3.4. Deficient Maternal Plasma 25(OH)D Levels Are Associated with Adverse Pregnancy Outcomes
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Roth, D.E. Vitamin D supplementation during pregnancy: Safety considerations in the design and interpretation of clinical trials. J. Perinatol. 2011, 31, 449–459. [Google Scholar] [CrossRef] [PubMed]
- De-Regil, L.M.; Palacios, C.; Lombardo, L.K.; Peña-Rosas, J.P. Vitamin D supplementation for women during pregnancy. In Cochrane Database of Systematic Reviews; John Wiley & Sons, Ltd.: Chichester, UK, 2016. [Google Scholar]
- Harvey, N.C.; Holroyd, C.; Ntani, G.; Javaid, K.; Cooper, P.; Moon, R.; Cole, Z.; Tinati, T.; Godfrey, K.; Dennison, E.; et al. Vitamin D supplementation in pregnancy: A systematic review. Health Technol. Assess. Winch. Engl. 2014, 18, 1–190. [Google Scholar] [CrossRef] [PubMed]
- Wacker, M.; Holick, M.F. Vitamin D—Effects on Skeletal and Extraskeletal Health and the Need for Supplementation. Nutrients 2013, 5, 111–148. [Google Scholar] [CrossRef] [PubMed]
- Hossein-Nezhad, A.; Holick, M.F. Vitamin D for Health: A Global Perspective. Mayo Clin. Proc. 2013, 88, 720–755. [Google Scholar] [CrossRef] [PubMed]
- Khazai, N.; Judd, S.E.; Tangpricha, V. Calcium and Vitamin D: Skeletal and extraskeletal health. Curr. Rheumatol. Rep. 2008, 10, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Gennari, C. Calcium and vitamin D nutrition and bone disease of the elderly. Public Health Nutr. 2001, 4, 547–559. [Google Scholar] [CrossRef] [PubMed]
- Bendik, I.; Friedel, A.; Roos, F.F.; Weber, P.; Eggersdorfer, M. Vitamin D: A critical and essential micronutrient for human health. Front. Physiol. 2014, 5, 248. [Google Scholar] [CrossRef] [PubMed]
- Jacquemyn, Y.; Ajaji, M.; Karepouan, N. Vitamin D levels in maternal serum and umbilical cord blood in a multi-ethnic population in Antwerp, Belgium. Facts Views Vis. ObGyn 2013, 5, 3–5. [Google Scholar] [PubMed]
- Mahadevan, S.; Kumaravel, V.; Bharath, R. Calcium and bone disorders in pregnancy. Indian J. Endocrinol. Metab. 2012, 16, 358–363. [Google Scholar] [CrossRef] [PubMed]
- Olmos-Ortiz, A.; Avila, E.; Durand-Carbajal, M.; Díaz, L. Regulation of Calcitriol Biosynthesis and Activity: Focus on Gestational Vitamin D Deficiency and Adverse Pregnancy Outcomes. Nutrients 2015, 7, 443–480. [Google Scholar] [CrossRef] [PubMed]
- Barrett, H.; McElduff, A. Vitamin D and pregnancy: An old problem revisited. Best Pract. Res. Clin. Endocrinol. Metab. 2010, 24, 527–539. [Google Scholar] [CrossRef] [PubMed]
- Bodnar, L.M.; Rouse, D.J.; Momirova, V.; Peaceman, A.M.; Sciscione, A.; Spong, C.Y.; Varner, M.W.; Malone, F.D.; Iams, J.D.; Mercer, B.M.; et al. Maternal 25-Hydroxyvitamin D and Preterm Birth in Twin Gestations. Obstet. Gynecol. 2013, 122, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Bodnar, L.M.; Catov, J.M.; Zmuda, J.M.; Cooper, M.E.; Parrott, M.S.; Roberts, J.M.; Marazita, M.L.; Simhan, H.N. Maternal Serum 25-Hydroxyvitamin D Concentrations Are Associated with Small-for-Gestational Age Births in White Women. J. Nutr. 2010, 140, 999–1006. [Google Scholar] [CrossRef] [PubMed]
- Bodnar, L.M.; Klebanoff, M.A.; Gernand, A.D.; Platt, R.W.; Parks, W.T.; Catov, J.M.; Simhan, H.N. Maternal Vitamin D Status and Spontaneous Preterm Birth by Placental Histology in the US Collaborative Perinatal Project. Am. J. Epidemiol. 2014, 179, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Bodnar, L.M.; Simhan, H.N. Vitamin D may be a link to black-white disparities in adverse birth outcomes. Obstet. Gynecol. Surv. 2010, 65, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Halicioglu, O.; Aksit, S.; Koc, F.; Akman, S.A.; Albudak, E.; Yaprak, I.; Coker, I.; Colak, A.; Ozturk, C.; Gulec, E.S. Vitamin D deficiency in pregnant women and their neonates in spring time in western Turkey. Paediatr. Perinat. Epidemiol. 2012, 26, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Smith, J.R.; Philipp, B.L.; Chen, T.C.; Mathieu, J.; Holick, M.F. Vitamin D Deficiency in a Healthy Group of Mothers and Newborn Infants. Clin. Pediatr. (Phila.) 2007, 46, 42–44. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Spiegelman, D.; Aboud, S.; Giovannucci, E.L.; Msamanga, G.I.; Hertzmark, E.; Mugusi, F.M.; Hunter, D.J.; Fawzi, W.W. Lipid-soluble vitamins A, D, and E in HIV-infected pregnant women in Tanzania. Eur. J. Clin. Nutr. 2010, 64, 808–817. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Setsuo Maeda, S.; Luporini Saraiva, G.; Sizue Kunii, I.; Fukusima Hayashi, L.; Seabra Cendoroglo, M.; Ramos, L.R.; Lazaretti-Castro, M. Factors affecting vitamin D status in different populations in the city of São Paulo, Brazil: The São PAulo vitamin D Evaluation Study (SPADES). BMC Endocr. Disord. 2013, 13. [Google Scholar] [CrossRef]
- Martineau, A.R.; Nhamoyebonde, S.; Oni, T.; Rangaka, M.X.; Marais, S.; Bangani, N.; Tsekela, R.; Bashe, L.; de Azevedo, V.; Caldwell, J.; et al. Reciprocal seasonal variation in vitamin D status and tuberculosis notifications in Cape Town, South Africa. Proc. Natl. Acad. Sci. USA 2011, 108, 19013–19017. [Google Scholar] [CrossRef] [PubMed]
- Coussens, A.K.; Naude, C.E.; Goliath, R.; Chaplin, G.; Wilkinson, R.J.; Jablonski, N.G. High-dose vitamin D3 reduces deficiency caused by low UVB exposure and limits HIV-1 replication in urban Southern Africans. Proc. Natl. Acad. Sci. USA 2015, 112, 8052–8057. [Google Scholar] [CrossRef] [PubMed]
- Finkelstein, J.L.; Mehta, S.; Duggan, C.P.; Spiegelman, D.; Aboud, S.; Kupka, R.; Msamanga, G.I.; Fawzi, W.W. Predictors of anaemia and iron deficiency in HIV-infected pregnant women in Tanzania: A potential role for vitamin D and parasitic infections. Public Health Nutr. 2012, 15, 928–937. [Google Scholar] [CrossRef] [PubMed]
- Moormann, A.M.; Chelimo, K.; Sumba, O.P.; Lutzke, M.L.; Ploutz-Snyder, R.; Newton, D.; Kazura, J.; Rochford, R. Exposure to Holoendemic Malaria Results in Elevated Epstein-Barr Virus Loads in Children. J. Infect. Dis. 2005, 191, 1233–1238. [Google Scholar] [CrossRef] [PubMed]
- Daud, I.I.; Ogolla, S.; Amolo, A.S.; Namuyenga, E.; Simbiri, K.; Bukusi, E.A.; Ploutz-Snyder, R.; Sumba, P.O.; Dent, A.; Rochford, R.; et al. Plasmodium falciparum Infection is Associated with Epstein–Barr Virus Reactivation in Pregnant Women Living in Malaria Holoendemic Area of Western Kenya. Matern. Child Health J. 2015, 19, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Butler, M.G.; Menitove, J.E. Umbilical cord blood banking: An update. J. Assist. Reprod. Genet. 2011, 28, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Vitamin D External Quality Assessment Scheme (DEQAS). Available online: http://www.deqas.org (accessed on 23 November 2016).
- World Health Organization. Guideline: Vitamin D Supplementation in Pregnant Women; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- World Health Organization. An Evaluation of Infant Growth. Available online: http://www.who.int/childgrowth/publications/evaluation_bul/en/ (accessed on 15 June 2016).
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, Treatment, and Prevention of Vitamin D Deficiency: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- Zou, G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. Am. J. Epidemiol. 2004, 159, 702–706. [Google Scholar] [CrossRef] [PubMed]
- Spiegelman, D.; Hertzmark, E. Easy SAS Calculations for Risk or Prevalence Ratios and Differences. Am. J. Epidemiol. 2005, 162, 199–200. [Google Scholar] [CrossRef] [PubMed]
- Rothman, K.; Greenland, S. Modern Epidemiology, 2nd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 1998. [Google Scholar]
- Karras, S.N.; Anagnostis, P.; Annweiler, C.; Naughton, D.P.; Petroczi, A.; Bili, E.; Harizopoulou, V.; Tarlatzis, B.C.; Persinaki, A.; Papadopoulou, F.; et al. Maternal vitamin D status during pregnancy: The Mediterranean reality. Eur. J. Clin. Nutr. 2014, 68, 864–869. [Google Scholar] [CrossRef] [PubMed]
- Cadario, F.; Savastio, S.; Pozzi, E.; Capelli, A.; Dondi, E.; Gatto, M.; Zaffaroni, M.; Bona, G. Vitamin D status in cord blood and newborns: Ethnic differences. Ital. J. Pediatr. 2013, 39. [Google Scholar] [CrossRef] [PubMed]
- Wagner, C.L.; Baggerly, C.; McDonnell, S.; Baggerly, K.A.; French, C.B.; Baggerly, L.; Hamilton, S.A.; Hollis, B.W. Post-hoc analysis of vitamin D status and reduced risk of preterm birth in two vitamin D pregnancy cohorts compared with South Carolina March of Dimes 2009–2011 rates. J. Steroid Biochem. Mol. Biol. 2016, 155, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Marya, R.K.; Rathee, S.; Dua, V.; Sangwan, K. Effect of vitamin D supplementation during pregnancy on foetal growth. Indian J. Med. Res. 1988, 88, 488–492. [Google Scholar] [PubMed]
- Xiao, J.-P.; Zang, J.; Pei, J.-J.; Xu, F.; Zhu, Y.; Liao, X.-P. Low Maternal Vitamin D Status during the Second Trimester of Pregnancy: A Cross-Sectional Study in Wuxi, China. PLoS ONE 2015, 10, e0117748. [Google Scholar] [CrossRef] [PubMed]
- Shiue, I. Low vitamin D levels in adults with longer time to fall asleep: US NHANES, 2005–2006. Int. J. Cardiol. 2013, 168, 5074–5075. [Google Scholar] [CrossRef] [PubMed]
- Gozdzik, A.; Barta, J.; Wu, H.; Wagner, D.; Cole, D.E.; Vieth, R.; Whiting, S.; Parra, E.J. Low wintertime vitamin D levels in a sample of healthy young adults of diverse ancestry living in the Toronto area: Associations with vitamin D intake and skin pigmentation. BMC Public Health 2008, 8, 336. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Rodriguez, L.; Lopez-Hoyos, M.; Garcia-Unzueta, M.; Amado, J.A.; Cacho, P.M.; Martinez-Taboada, V.M. Age and low levels of circulating vitamin D are associated with impaired innate immune function. J. Leukoc. Biol. 2012, 91, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Samuel, L.; Borrell, L.N. The effect of body mass index on optimal vitamin D status in U.S. adults: The National Health and Nutrition Examination Survey 2001–2006. Ann. Epidemiol. 2013, 23, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Luk, J.; Torrealday, S.; Perry, G.N.; Pal, L. Relevance of vitamin D in reproduction. Hum. Reprod. 2012, 27, 3015–3027. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.S.; Choi, M.Y.; Longtine, M.S.; Nelson, D.M. Vitamin D effects on pregnancy and the placenta. Placenta 2010, 31, 1027–1034. [Google Scholar] [CrossRef] [PubMed]
- Kennel, K.A.; Drake, M.T.; Hurley, D.L. Vitamin D Deficiency in Adults: When to Test and How to Treat. Mayo Clin. Proc. 2010, 85, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Brannon, P.M.; Picciano, M.F. Vitamin D in Pregnancy and Lactation in Humans. Annu. Rev. Nutr. 2011, 31, 89–115. [Google Scholar] [CrossRef] [PubMed]
- Ettyang, G.A.; van Marken Lichtenbelt, W.D.; Oloo, A.; Saris, W.H.M. Serum Retinol, Iron Status and Body Composition of Lactating Women in Nandi, Kenya. Ann. Nutr. Metab. 2003, 47, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Wagner, C.L.; McNeil, R.B.; Johnson, D.D.; Hulsey, T.C.; Ebeling, M.; Robinson, C.; Hamilton, S.A.; Hollis, B.W. Health characteristics and outcomes of two randomized vitamin D supplementation trials during pregnancy: A combined analysis. J. Steroid Biochem. Mol. Biol. 2013, 136, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Litonjua, A.A.; Carey, V.J.; Laranjo, N.; Harshfield, B.J.; McElrath, T.F.; O’Connor, G.T.; Sandel, M.; Iverson, R.E., Jr.; Lee-Paritz, A.; Strunk, R.C.; et al. Effect of prenatal supplementation with vitamin D on asthma or recurrent wheezing in offspring by age 3 years: The vdaart randomized clinical trial. JAMA 2016, 315, 362–370. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean ± SD or % (n) |
|---|---|
| Maternal characteristics at enrollment ANC-1 (N = 63) | |
| Maternal age, years | 22.5 ± 6.6 |
| Gestational age, weeks | 19.9 ± 5.7 |
| Body mass index, kg/m | 22.9 ± 2.9 |
| Anemia (Hb < 11.0 g/dL) | 47.5% (28) |
| Severe anemia (Hb < 8.5 g/dL) | 6.8% (4) |
| Maternal malaria infection (by qPCR) | 38.7% (24) |
| Maternal pathogenic protozoan 1 or helminth infection 2 | 45.2% (19) |
| Plasma 25(OH)D, nmol/L | 77.0 ± 31.5 |
| Plasma 25(OH)D, deficient (<50 nmol/L) | 20.6% (13) |
| Plasma 25(OH)D, insufficient (<75 nmol/L) | 50.8% (32) |
| Maternal characteristics throughout gestation | |
| ANC-2 Visit (N = 38) | |
| Gestational age, weeks | 23.6 ± 5.7 |
| Plasma 25(OH)D, nmol/L | 92.7 ± 32.3 |
| ANC-3 Visit (N = 39) | |
| Gestational age, weeks | 27.2 ± 6.2 |
| Plasma 25(OH)D, nmol/L | 96.6 ± 29.5 |
| ANC-4 Visit (N = 35) | |
| Gestational age, weeks | 30.4 ± 5.7 |
| Plasma 25(OH)D, nmol/L | 101.3 ± 28.1 |
| Plasma 25(OH)D in venous blood at delivery, nmol/L | 91.9 ± 32.6 |
| Newborn characteristics (N = 54) | |
| Female | 42.6% (23) |
| Gestational age at birth, weeks | 39.2 ± 2.8 |
| Preterm (<37 weeks of gestation) | 18.4% (9) |
| Birth weight, kg | 3.3 ± 0.4 |
| Length, cm | 49.0 ± 2.7 |
| Head circumference, cm | 35.4 ± 1.5 |
| Plasma 25(OH)D in cord blood, nmol/L | 64.9 ± 26.4 |
| Plasma 25(OH)D, deficient (<50 nmol/L) | 30.2% (13) |
| Plasma 25(OH)D, insufficient (<75 nmol/L) | 74.4% (32) |
| Outcome | Mean Difference (SE) 2 | p |
|---|---|---|
| Gestational age at birth, weeks | 0.01 (0.01) | 0.41 |
| Birth weight, grams | 3.0 (1.6) | 0.06 |
| Weight-for-age z-score (WAZ) | 0.01 (0.00) | 0.035 * |
| Length-for-age z-score (LAZ) | 0.00 (0.01) | 0.70 |
| Weight-for-length z-score (WLZ) | 0.02 (0.01) | 0.02 * |
| BMI z-score | 0.01 (0.01) | 0.14 |
| Maternal Plasma 25(OH)D Level 1 | Bivariate Analysis | Multivariate Analysis 2 | ||||
|---|---|---|---|---|---|---|
| Low (<50 nmol/L) | Adequate (≥50 nmol/L) | |||||
| Outcome | n/N (%) | n/N (%) | RR (95% CI) | p 3 | RR (95% CI) | p 3 |
| Preterm birth (<37 weeks) | 4/10 (40.0) | 5/39 (12.8) | 3.12 (1.02, 9.53) | 0.06 | 5.36 (1.13, 25.33) | 0.03 * |
| Stunted (LAZ < −2) | 4/10 (40.0) | 4/43 (9.3) | 4.30 (1.29, 14.32) | 0.03 * | 4.39 (1.04, 18.55) | 0.04 * |
| Wasted (WLZ < −2) | 1/8 (12.5) | 5/42 (11.9) | 1.05 (0.14, 7.83) | 0.96 | 1.12 (0.12, 10.36) | 0.92 |
| BMI z-score (<−2) | 1/10 (10.0) | 2/43 (4.7) | 2.15 (0.22, 21.44) | 0.54 | 1.76 (0.15, 19.97) | 0.65 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toko, E.N.; Sumba, O.P.; Daud, I.I.; Ogolla, S.; Majiwa, M.; Krisher, J.T.; Ouma, C.; Dent, A.E.; Rochford, R.; Mehta, S. Maternal Vitamin D Status and Adverse Birth Outcomes in Children from Rural Western Kenya. Nutrients 2016, 8, 794. https://doi.org/10.3390/nu8120794
Toko EN, Sumba OP, Daud II, Ogolla S, Majiwa M, Krisher JT, Ouma C, Dent AE, Rochford R, Mehta S. Maternal Vitamin D Status and Adverse Birth Outcomes in Children from Rural Western Kenya. Nutrients. 2016; 8(12):794. https://doi.org/10.3390/nu8120794
Chicago/Turabian StyleToko, Eunice N., Odada P. Sumba, Ibrahim I. Daud, Sidney Ogolla, Maxwel Majiwa, Jesse T. Krisher, Collins Ouma, Arlene E. Dent, Rosemary Rochford, and Saurabh Mehta. 2016. "Maternal Vitamin D Status and Adverse Birth Outcomes in Children from Rural Western Kenya" Nutrients 8, no. 12: 794. https://doi.org/10.3390/nu8120794





