Contribution of Dietary Supplements to Nutritional Adequacy in Race/Ethnic Population Subgroups in the United States
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Micronutrient Intake from Foods
2.3. Micronutrient Intake from Supplements
2.4. Statistics
2.5. Trial Registration
3. Results
3.1. Dietary Supplement Usage
3.2. Effect of Supplement Use on Usual Intake of Nutrients
3.3. Effect of Supplement Use on Prevalence of Inadequacy
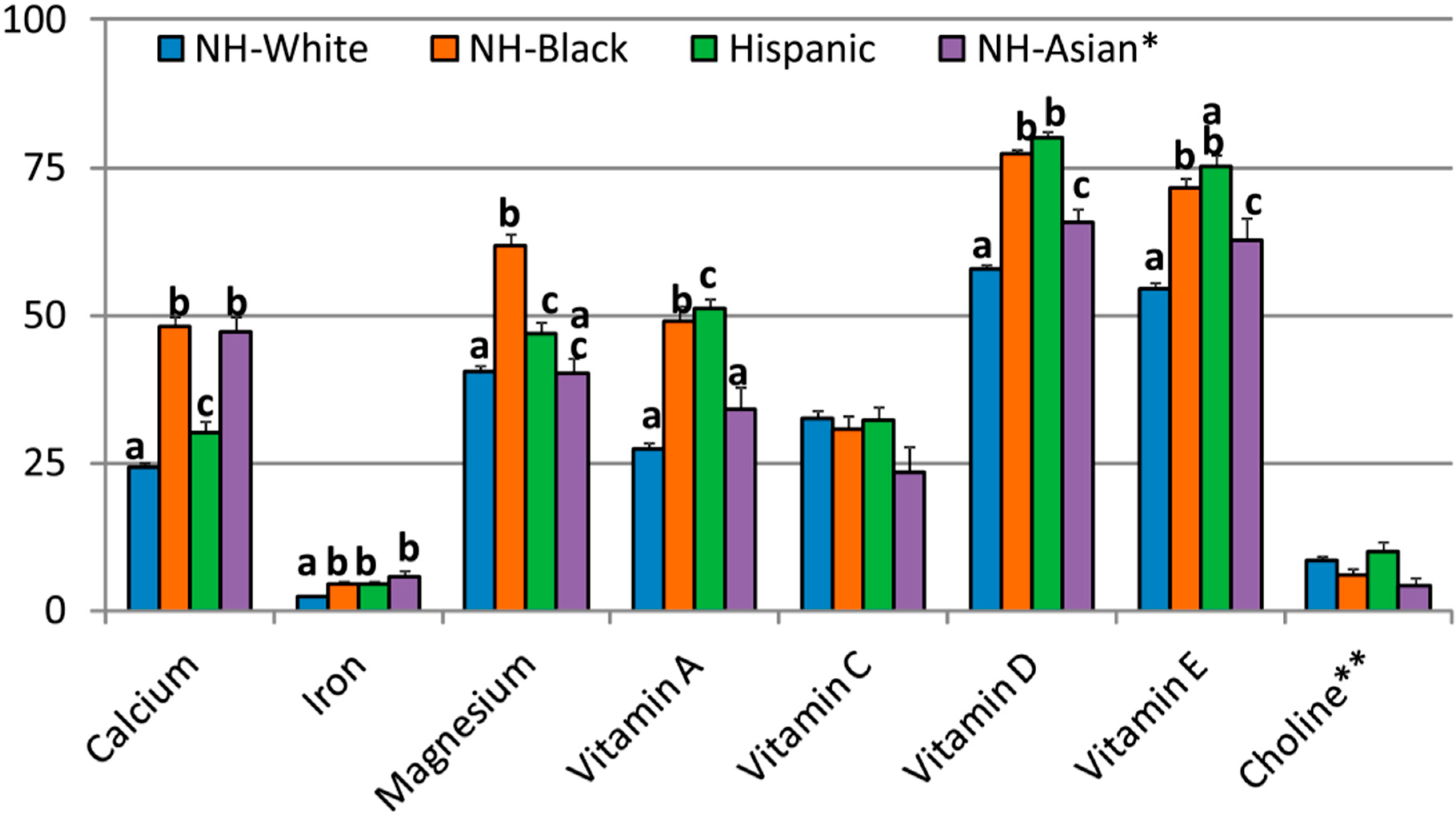
3.4. Comparison of Prevalence of Inadequacy by Race/Ethnicity
3.5. Effect of Supplement Use on Prevalence of Intakes above the UL
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- U.S. Department of Health and Human Services; U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. 8th Edition. December 2015. Available online: http://health.gov/dietaryguidelines/2015/guidelines/ (accessed on 15 March 2017).
- Otten, J.J.; Pitzi Hellwig, J.; Meyers, L.D. (Eds.) Dietary Reference Intakes, the Essential Guide to Nutrient Requirements; National Academy Press: Washington, DC, USA, 2006. [Google Scholar]
- Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D; National Academy Press: Washington, DC, USA, 2011. [Google Scholar]
- Fulgoni, V.L., III; Keast, D.R.; Bailey, R.L.; Dwyer, J. Foods, fortificants and supplements: Where do Americans get their nutrients? J. Nutr. 2011, 141, 1847–1854. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Gahche, J.J.; Miller, P.E.; Thomas, P.R.; Dwyer, J.T. Why US adults use dietary supplements. JAMA Intern. Med. 2013, 173, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, A.; MacKay, D.; Wong, A. Consumer attitudes about the role of multivitamins and other dietary supplements: Report of a survey. Nutr. J. 2015, 14, 66. [Google Scholar] [CrossRef] [PubMed]
- Briefel, R.R.; Johnson, C.L. Secular trends in dietary intake in the United States. Annu. Rev. Nutr. 2004, 24, 401–431. [Google Scholar] [CrossRef] [PubMed]
- Gahche, J.J.; Bailey, R.L.; Potischman, N.; Dwyer, J.T. Dietary supplement use was very high among older adults in the United States in 2011–2014. J. Nutr. 2017. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Gahche, J.J.; Lentino, C.V.; Dwyer, J.T.; Engel, J.S.; Thomas, P.R.; Betz, J.M.; Sempos, C.T.; Picciano, M.F. Dietary supplement use in the United States, 2003–2006. J. Nutr. 2011, 141, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Wallace, T.C.; McBurney, M.; Fulgoni, V.L. Multivitamin/mineral supplement contribution to micronutrient intakes in the United States, 2007–2010. J. Am. Coll. Nutr. 2014, 33, 94–102. [Google Scholar] [CrossRef] [PubMed]
- Kantor, E.D.; Rehm, C.D.; Du, M.; White, E.; Giovannucci, E.L. Trends in dietary supplement use among US adults from 1999–2012. JAMA 2016, 316, 1464–1474. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Murphy, S.P.; Wilkens, L.R.; Shen, L.; Hankin, J.H.; Monroe, K.R.; Henderson, B.; Kolonel, L.N. Adherence to the Food Guide Pyramid recommendations among African Americans and Latinos: Results from the Multiethnic Cohort. J. Am. Diet. Assoc. 2004, 104, 1873–1877. [Google Scholar] [CrossRef] [PubMed]
- Nicklas, T.A.; Jahns, L.; Bogle, M.L.; Chester, D.N.; Giovanni, M.; Klurfeld, D.M.; Laugero, K.; Liu, Y.; Lopez, S.; Tucker, K.L. Barriers and facilitators for consumer adherence to the dietary guidelines for Americans: The HEALTH study. J. Acad. Nutr. Diet. 2013, 113, 1317–1331. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, S.I.; Dodd, K.W.; Reedy, J.; Krebs-Smith, S.M. Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. J. Acad. Nutr. Diet. 2012, 112, 624–635. [Google Scholar] [CrossRef] [PubMed]
- Gordon-Larsen, P.; Popkin, B. Understanding socioeconomic and racial/ethnic status disparities in diet, exercise, and weight: Underlying contextual factors and pathways. J. Am. Diet. Assoc. 2011, 111, 1816–1819. [Google Scholar] [CrossRef] [PubMed]
- Batis, C.; Hernandez-Barrera, L.; Barquera, S.; Rivera, J.A.; Popkin, B.M. Food acculturation drives dietary differences among Mexicans, Mexican Americans, and Non-Hispanic Whites. J. Nutr. 2011, 141, 1898–1906. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, C.E.; Nicklas, T.A.; Keast, D.R.; Fulgoni, V.L. Ethnic disparities among food sources of energy and nutrients of public health concern and nutrients to limit in adults in the United States: NHANES 2003–2006. Food Nutr. Res. 2014, 58, 15784. [Google Scholar] [CrossRef] [PubMed]
- Newby, P.K.; Noel, S.E.; Grant, R.; Judd, S.; Shikany, J.M.; Ard, J. Race and region are associated with nutrient intakes among black and white men in the United States. J. Nutr. 2011, 141, 296–303. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.K.; Graubard, B.I.; Kumanyika, S.K. Trends in black–white differentials in dietary intakes of US adults, 1971–2002. Am. J. Prev. Med. 2007, 32, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Bowman, S.A. Socioeconomic characteristics, dietary and lifestyle patterns, and health and weight status of older adults in NHANES, 1999–2002: A comparison of Caucasians and African Americans. J. Nutr. Elder. 2009, 28, 30–46. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Siega-Riz, A.M.; Haines, P.S. A comparison of dietary trends among racial and socioeconomic groups in the United States. N. Engl. J. Med. 1996, 335, 716–720. [Google Scholar] [CrossRef] [PubMed]
- Norris, J.; Harnack, L.; Carmichael, S.; Pouane, T.; Wakimoto, P.; Block, G. US trends in nutrient intake: The 1987 and 1992 National Health Interview Surveys. Am. J. Public Health 1997, 87, 740–746. [Google Scholar] [CrossRef] [PubMed]
- CDC, National Center for Health Statistics. Second National Report on Biochemical Indicators of Diet and Nutrition in the U.S. Population. 2012. Available online: http://www.cdc.gov/nutritionreport/pdf/nutrition_book_complete508_final.pdf (accessed on 10 November 2016).
- Radimer, K.; Bindewald, B.; Hughes, J.; Ervin, B.; Swanson, C.; Picciano, M.F. Dietary supplement use by US adults: Data from the National Health and Nutrition Examination Survey, 1999–2000. Am. J. Epidemiol. 2004, 160, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Gahche, J.; Bailey, R.; Burt, V.; Hughes, J.; Yetley, E.; Dwyer, J.; Picciano, M.F.; McDowell, M.; Sempos, C. Dietary Supplement Use among U.S. Adults Has Increased since NHANES III (1988–1994); NCHS Data Brief, No. 61; National Center for Health Statistics: Hyattsville, MD, USA, 2011.
- Murphy, S.P.; Wilkens, L.R.; Monroe, K.R.; Steffen, A.D.; Yonemori, K.M.; Morimoto, Y.; Albright, C.L. Dietary Supplement Use Within a Multiethnic Population as Measured by a Unique Inventory Method. J. Am. Diet. Assoc. 2011, 111, 1065–1072. [Google Scholar] [CrossRef] [PubMed]
- Rock, C.L. Multivitamin-multimineral supplements: Who uses them? Am. J. Clin. Nutr. 2007, 85, 277S–279S. [Google Scholar] [PubMed]
- Burnett-Hartman, A.N.; Fitzpatrick, A.L.; Gao, K.; Jackson, S.A.; Schreiner, P.J. Supplement use contributes to meeting recommended dietary intakes for calcium, magnesium, and vitamin C in four ethnicities of middle-aged and older Americans: The Multi-Ethnic Study of Atherosclerosis. J. Am. Diet. Assoc. 2009, 109, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Blumberg, J.B.; Frei, B.; Fulgoni, V.L.; Weaver, C.M.; Zeisel, S.H. Impact of frequency of multi-vitamin/multi-mineral supplement intake on nutritional adequacy and nutrient status in US adults. Nutrients 2017, 9, 849. [Google Scholar] [CrossRef] [PubMed]
- CDC, National Center for Health Statistics. About the National Health and Nutrition Examination Survey. Available online: http://www.cdc.gov/nchs/nhanes/about nhanes.htm (accessed on 5 October 2016).
- Ahuja, J.K.A.; Montville, J.B.; Omolewa-Tomobi, G.; Heendeniya, K.Y.; Martin, C.L.; Steinfeldt, L.C.; Anand, J.; Adler, M.E.; LaComb, R.P.; Moshfegh, A.J. USDA Food and Nutrient Database for Dietary Studies; USDA/ARS/FSRG: Beltsville, MD, USA, 2012. [Google Scholar]
- U.S. Department of Agriculture; Agricultural Research Service. USDA Food and Nutrient Database for Dietary Studies 2011–2012. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fndds-download-databases/ (accessed on 10 January 2017).
- US Department of Agriculture National Agriculture Library: National Nutrient Database for Standard Reference. Available online: http://ndb.nal.usda.gov/ (accessed on 5 October 2016).
- CDC, National Center for Health Statistics. Questionnaires, Datasets and Related Documentation, NHANES [Internet]. Hyattsville (MD). Available online: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm (accessed on 5 October 2016).
- Tooze, J.A.; Kipnis, V.; Buckman, D.W.; Carroll, R.J.; Freedman, L.S.; Guenther, P.M.; Krebs-Smith, S.M.; Subar, A.F.; Dodd, K.W. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: The NCI method. Stat. Med. 2010, 29, 2857–2868. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Medicine, Food and Nutrition Board. Dietary Reference Intakes: Applications in Dietary Assessment; National Academies Press: Washington, DC, USA, 2000. [Google Scholar]
- Ames, B.N. Low micronutrient intake may accelerate the degenerative diseases of aging through allocation of scarce micronutrients by triage. Proc. Natl. Acad. Sci. USA 2006, 103, 17589–17594. [Google Scholar] [CrossRef] [PubMed]
- Fairfield, K.M.; Fletcher, R.H. Vitamins for chronic disease prevention in adults: Scientific review. JAMA 2002, 287, 3116–3126. [Google Scholar] [CrossRef] [PubMed]
- He, F.J.; MacGregor, G.A. Beneficial effects of potassium on human health. Physiol. Plant. 2008, 133, 725–735. [Google Scholar] [CrossRef] [PubMed]
- Resmini, G.; Tarantino, U.; Iolascon, G. Vitamin D: Role and opportunity to prescribe. Aging Clin. Exp. Res. 2013, 25, S125–S127. [Google Scholar] [CrossRef] [PubMed]
- Uusi-Rasi, K.; Karkkainen, M.U.; Lamberg-Allardt, C.J. Calcium intake in health maintenance a systematic review. Food Nutr. Res. 2013, 57. [Google Scholar] [CrossRef] [PubMed]
- Vuksan, V.; Jenkins, A.L.; Jenkins, D.J.; Rogovik, A.L.; Sievenpiper, J.L.; Jovanovski, E. Using cereal to increase dietary fiber intake to the recommended level and the effect of fiber on bowel function in healthy persons consuming North American diets. Am. J. Clin. Nutr. 2008, 88, 1256–1262. [Google Scholar] [PubMed]
| Nutrients | NH-White (n = 4649) | NH-Black (n = 2358) | Hispanic (n = 2625) | NH-Asian ** (n = 615) | ||||
|---|---|---|---|---|---|---|---|---|
| Food Only | Food + Supplement | Food Only | Food + Supplement | Food Only | Food + Supplement | Food Only | Food + Supplement | |
| Calcium (mg) | 1057 ± 10 | 1244 ± 11 * | 847 ± 13 | 935 ± 15 * | 990 ± 17 | 1073 ± 19 * | 788 ± 17 | 942 ± 22 * |
| Copper (mg) | 1.35 ± 0.01 | 1.70 ± 0.02 * | 1.20 ± 0.02 | 1.40 ± 0.02 * | 1.27 ± 0.02 | 1.46 ± 0.03 * | 1.44 ± 0.02 | 1.69 ± 0.05 * |
| Iron (mg) | 15.8 ± 0.2 | 19.2 ± 0.2 * | 14.1 ± 0.2 | 16.9 ± 0.3 * | 15.8 ± 0.3 | 17.6 ± 0.3 * | 14.4 ± 0.4 | 17.0 ± 0.5 * |
| Magnesium (mg) | 319 ± 3 | 351 ± 4 * | 271 ± 5 | 286 ± 5 | 312 ± 4 | 327 ± 5 | 323 ± 6 | 344 ± 7 |
| Phosphorus (mg) | 1455 ± 10 | 1466 ± 11 | 1264 ± 17 | 1267 ± 17 | 1459 ± 20 | 1463 ± 20 | 1278 ± 24 | 1280 ± 23 |
| Selenium (µg) | 113 ± 1 | 132 ± 1 * | 111 ± 2 | 122 ± 2 * | 119 ± 2 | 147 ± 18 | 122 ± 3 | 137 ± 4 * |
| Zinc (mg) | 12.1 ± 0.1 | 16.8 ± 0.3 * | 10.8 ± 0.3 | 13.2 ± 0.3 * | 11.7 ± 0.2 | 13.8 ± 0.2 * | 10.4 ± 0.2 | 13.8 ± 0.5 * |
| Vitamin A (µg RE) | 697 ± 18 | 1078 ± 26 * | 542 ± 20 | 745 ± 22 * | 541 ± 11 | 726 ± 16 * | 614 ± 24 | 902 ± 47 * |
| Thiamin (mg) | 1.70 ± 0.10 | 6.41 ± 0.52 * | 1.48 ± 0.02 | 3.04 ± 0.22 * | 1.65 ± 0.02 | 3.44 ± 0.26 * | 1.56 ± 0.04 | 4.80 ± 0.73 * |
| Riboflavin (mg) | 2.31 ± 0.02 | 5.39 ± 0.39 * | 1.74 ± 0.03 | 3.07 ± 0.17 * | 2.02 ± 0.03 | 3.57 ± 0.22 * | 1.80 ± 0.05 | 4.00 ± 0.55 * |
| Niacin (mg) | 26.4 ± 0.2 | 38.1 ± 1.0 * | 24.9 ± 0.3 | 29.8 ± 0.6 * | 26.7 ± 0.4 | 31.0 ± 0.6 * | 24.7 ± 0.8 | 33.1 ± 2.3 * |
| Folate DFE (µg) | 574 ± 7 | 813 ± 8 * | 475 ± 9 | 612 ± 11 * | 564 ± 9 | 684 ± 12 * | 561 ± 15 | 745 ± 25 * |
| Vitamin B6 (mg) | 2.18 ± 0.02 | 6.04 ± 0.26 * | 1.94 ± 0.03 | 3.89 ± 0.2 * | 2.22 ± 0.04 | 4.15 ± 0.25 * | 2.10 ± 0.06 | 4.50 ± 0.59 * |
| Vitamin B12 (µg) | 5.60 ± 0.11 | 56.8 ± 4.0 * | 4.76 ± 0.12 | 38.5 ± 6.0 * | 4.92 ± 0.12 | 38.6 ± 6.8 * | 4.62 ± 0.20 | 62.0 ± 9.7 * |
| Vitamin C (mg) | 82.8 ± 2.3 | 177 ± 7 * | 92.0 ± 2.3 | 139 ± 7 * | 93.6 ± 2.9 | 132 ± 4 * | 94.2 ± 4.5 | 178 ± 12 * |
| Vitamin D (µg) | 5.11 ± 0.08 | 16.2 ± 0.9 * | 3.97 ± 0.12 | 9.28 ± 0.36 * | 4.68 ± 0.09 | 8.50 ± 0.34 * | 4.71 ± 0.32 | 15.0 ± 1.0 * |
| Vitamin E (mg) | 8.84 ± 0.11 | 29.7 ± 1.4 * | 7.79 ± 0.19 | 17.4 ± 0.9 * | 7.64 ± 0.19 | 17.5 ± 1.4 * | 8.50 ± 0.28 | 19.6 ± 1.4 * |
| Vitamin K (µg) | 112 ± 3 | 119 ± 3 | 99.4 ± 3.6 | 104 ± 4 | 82.1 ± 3.1 | 87.0 ± 2.7 | 149 ± 10 | 157 ± 10 |
| Choline (mg) | 340 ± 3 | 341 ± 3 | 326 ± 4.2 | 326 ± 4 | 348 ± 6 | 350 ± 6 | 329 ± 8 | 330 ± 7 |
| Nutrients | NH-White (n = 4649) | NH-Black (n = 2358) | Hispanic (n = 2625) | NH-Asian ** (n = 615) | ||||
|---|---|---|---|---|---|---|---|---|
| Food Only | Food + Supplement | Food Only | Food + Supplement | Food Only | Food + Supplement | Food Only | Food + Supplement | |
| Nutrients with EAR, percentage below EAR | ||||||||
| Calcium | 35.9 ± 1.0 1 | 24.2 ± 0.7 * | 56.3 ± 1.4 | 48.2 ± 1.4 * | 36.4 ± 2.1 | 30.1 ± 2.0 | 61.4 ± 2.5 | 47.0 ± 2.6 * |
| Copper | 4.5 ± 0.6 | 3.6 ± 0.4 | 6.7 ± 1.3 | 5.7 ± 1.1 | 5.6 ± 1.4 | 4.9 ± 1.3 | 2.4 ± 0.9 | 2.0 ± 0.7 |
| Iron | 3.1 ± 0.2 | 2.3 ± 0.2 | 5.5 ± 0.5 | 4.6 ± 0.4 | 5.2 ± 0.5 | 4.5 ± 0.5 | 7.0 ± 1.3 | 5.6 ± 1.1 |
| Magnesium | 48.5 ± 1.3 | 40.3 ± 1.2 * | 67.2 ± 2.2 | 61.7 ± 1.9 | 51.3 ± 2.0 | 46.7 ± 2.1 | 46.1 ± 2.4 | 40.1 ± 2.5 |
| Phosphorus | <1 | <1 | <1 | <1 | <1 | <1 | 1.2 ± 0.5 | 1.3 ± 0.5 |
| Selenium | <1 | <1 | <1 | <1 | <1 | <1 | <1 | <1 |
| Zinc | 11.9 ± 1.3 | 8.2 ± 1.0 | 22.1 ± 2.5 | 17.9 ± 2.0 | 15.4 ± 2.0 | 13.0 ± 2.0 | 20.6 ± 1.8 | 15.8 ± 1.7 |
| Vitamin A | 37.7 ± 2.0 | 27.2 ± 1.3 * | 59.7 ± 3.0 | 49.0 ± 2.5 * | 59.0 ± 2.0 | 51.0 ± 1.8 * | 45.3 ± 5.6 | 33.9 ± 4.0 |
| Thiamin | 4.1 ± 0.6 | 2.6 ± 0.4 | 10.1 ± 1.2 | 8.1 ± 1.0 | 7.7 ± 1.5 | 6.3 ± 1.3 | 5.8 ± 1.4 | 4.1 ± 1.2 |
| Riboflavin | 1.3 ± 0.2 | <1 | 6.8 ± 1.3 | 5.6 ± 1.1 | 4.4 ± 1.1 | 3.9 ± 0.9 | 9.0 ± 1.4 | 6.8 ± 1.3 |
| Niacin | <1 | <1 | 1.4 ± 0.5 | 1.2 ± 0.4 | 1.6 ± 0.5 | 1.3 ± 0.5 | 1.1 ± 0.7 | <1 |
| Folate DFE | 9.1 ± 1.0 | 5.9 ± 0.6 * | 19.0 ± 1.6 | 14.9 ± 1.3 | 9.0 ± 1.4 | 7.8 ± 1.3 | 8.5 ± 1.6 | 6.1 ± 1.3 |
| Vitamin B6 | 9.2 ± 0.7 | 5.9 ± 0.5 * | 11.2 ± 1.7 | 8.8 ± 1.3 | 7.7 ± 1.7 | 6.2 ± 1.4 | 7.90 ± 2.23 | 5.4 ± 1.6 |
| Vitamin B12 | 3.2 ± 0.6 | 1.9 ± 1.4 | 3.4 ± 1.5 | 2.5 ± 1.1 | 4.9 ± 0.9 | 3.9 ± 0.8 | 3.9 ± 2.8 | 2.6 ± 1.7 |
| Vitamin C | 46.9 ± 1.6 | 32.6 ± 1.4 * | 37.4 ± 2.8 | 30.7 ± 2.2 | 38.4 ± 2.5 | 32.3 ± 2.2 | 30.1 ± 6.2 | 23.5 ± 4.2 |
| Vitamin D | 93.2 ± 0.6 | 57.9 ± 0.8 * | 98.5 ± 0.7 | 77.2 ± 1.0 * | 96.9 ± 0.6 | 80.1 ± 0.9 * | 95.1 ± 1.7 | 65.7 ± 2.4 * |
| Vitamin E | 82.6 ± 0.9 | 54.6 ± 0.8 * | 90.3 ± 1.8 | 71.5 ± 1.8 * | 91.2 ± 1.7 | 75.3 ± 1.8 * | 85.8 ± 3.3 | 62.6 ± 3.8 * |
| Nutrients with AI, percentage above AI | ||||||||
| Vitamin K | 44.6 ± 1.5 | 50.0 ± 1.5 | 38.2 ± 2.5 | 41.5 ± 2.3 | 24.0 ± 2.6 | 27.8 ± 2.3 | 69.0 ± 5.7 | 71.9 ± 5.1 |
| Choline | 8.2 ± 0.8 | 8.5 ± 0.8 | 5.9 ± 1.1 | 6.0 ± 1.1 | 9.5 ± 1.5 | 9.9 ± 1.8 | 4.2 ± 1.4 | 4.2 ± 1.5 |
| Nutrients | NH-White (n = 4649) | NH-Black (n = 2358) | Hispanic (n = 2625) | NH-Asian * (n = 615) |
|---|---|---|---|---|
| Nutrients with EAR, percentage below EAR | ||||
| Calcium | 24.2 ± 0.7 1 a | 48.2 ± 1.4 b | 30.1 ± 2.0 c | 47.0 ± 2.6 b |
| Copper | 3.6 ± 0.4 ab | 5.73 ± 1.12 a | 4.92 ± 1.28 ab | 1.95 ± 0.71 b |
| Iron | 2.3 ± 0.18 a | 4.59 ± 0.44 b | 4.47 ± 0.47 b | 5.63 ± 1.11 b |
| Magnesium | 40.3 ± 1.2 a | 61.7 ± 1.9 b | 46.7 ± 2.1 c | 40.1 ± 2.5 ac |
| Phosphorus | <1 | <1 | <1 | 1.3 ± 0.5 |
| Selenium | <1 | <1 | <1 | <1 |
| Zinc | 8.2 ± 1.0 a | 17.9 ± 2.0 b | 13.0 ± 2.0 ab | 15.8 ± 1.7 b |
| Vitamin A | 27.2 ± 1.3 a | 49.0 ± 2.5 b | 51.0 ± 1.8 c | 33.9 ± 4.0 a |
| Thiamin | 2.6 ± 0.4 a | 8.1 ± 1.0 b | 6.3 ± 1.3b c | 4.1 ± 1.2 ac |
| Riboflavin | <1a | 5.61 ± 1.13 b | 3.85 ± 0.85 b | 6.79 ± 1.28 b |
| Niacin | <1 | 1.2 ± 0.4 | 1.3 ± 0.5 | <1 |
| Folate DFE | 5.9 ± 0.6 a | 14.9 ± 1.3 b | 7.8 ± 1.3 a | 6.1 ± 1.3 a |
| Vitamin B6 | 5.9 ± 0.5 | 8.8 ± 1.3 | 6.2 ± 1.4 | 5.4 ± 1.6 |
| Vitamin B12 | 1.9 ± 1.4 | 2.5 ± 1.1 | 3.9 ± 0.8 | 2.6 ± 1.7 |
| Vitamin C | 32.6 ± 1.4 | 30.7 ± 2.2 | 32.3 ± 2.2 | 23.5 ± 4.2 |
| Vitamin D | 57.9 ± 0.8 a | 77.2 ± 1.0 b | 80.1 ± 0.9 b | 65.7 ± 2.4 c |
| Vitamin E | 54.6 ± 0.8 a | 71.5 ± 1.8 b | 75.3 ± 1.8 c | 62.6 ± 3.8 ab |
| Nutrients with AI, percentage above AI | ||||
| Vitamin K | 50.0 ± 1.5 a | 41.5 ± 2.3 b | 27.8 ± 2.3 c | 71.9 ± 5.1 d |
| Choline | 8.5 ± 0.8 | 6.0 ± 1.1 | 9.9 ± 1.8 | 4.9 ± 1.5 |
| Nutrients | NH-White (n = 4649) | NH-Black (n = 2358) | Hispanic (n = 2625) | NH-Asian ** (n = 615) | ||||
|---|---|---|---|---|---|---|---|---|
| Food Only | Food + Supplement | Food Only | Food + Supplement | Food Only | Food + Supplement | Food Only | Food + Supplement | |
| Calcium | <1 | 4.8 ± 0.3 *,1 | <1 | 1.0 ± 0.3 | <1 | 1.1 ± 0.2 * | <1 | <1 |
| Copper | <1 | <1 | <1 | <1 | <1 | <1 | <1 | <1 |
| Iron | <1 | 1.9 ± 0.2 * | <1 | 1.9 ± 0.3 * | <1 | 1.1 ± 0.2 * | <1 | 1.2 ± 0.5 |
| Phosphorus | <1 | <1 | <1 | <1 | <1 | <1 | <1 | <1 |
| Selenium | <1 | <1 | <1 | <1 | <1 | <1 | <1 | <1 |
| Zinc | <1 | 2.5 ± 0.3 * | <1 | <1 | <1 | <1 | <1 | 1.5 ± 0.6 |
| Vitamin A | <1 | <1 | <1 | <1 | <1 | <1 | <1 | <1 |
| Niacin | ND | ND | ND | ND | ND | ND | ND | ND |
| Folate DFE | <1 | 2.1 ± 0.2 * | <1 | <1 | <1 | 1.3 ± 0.3 * | <1 | <1 |
| Vitamin B6 | <1 | 1.1 ± 0.2 * | <1 | <1 | <1 | <1 | <1 | <1 |
| Vitamin C | <1 | <1 | <1 | <1 | <1 | <1 | <1 | <1 |
| Vitamin D | <1 | 1.5 ± 0.2 * | <1 | <1 | <1 | <1 | <1 | 2.2 ± 0.7 * |
| Vitamin E | <1 | <1 | <1 | <1 | <1 | <1 | <1 | <1 |
| Choline | <1 | <1 | <1 | <1 | <1 | <1 | <1 | <1 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blumberg, J.B.; Frei, B.; Fulgoni III, V.L.; Weaver, C.M.; Zeisel, S.H. Contribution of Dietary Supplements to Nutritional Adequacy in Race/Ethnic Population Subgroups in the United States. Nutrients 2017, 9, 1295. https://doi.org/10.3390/nu9121295
Blumberg JB, Frei B, Fulgoni III VL, Weaver CM, Zeisel SH. Contribution of Dietary Supplements to Nutritional Adequacy in Race/Ethnic Population Subgroups in the United States. Nutrients. 2017; 9(12):1295. https://doi.org/10.3390/nu9121295
Chicago/Turabian StyleBlumberg, Jeffrey B., Balz Frei, Victor L. Fulgoni III, Connie M. Weaver, and Steven H. Zeisel. 2017. "Contribution of Dietary Supplements to Nutritional Adequacy in Race/Ethnic Population Subgroups in the United States" Nutrients 9, no. 12: 1295. https://doi.org/10.3390/nu9121295






