1. Introduction
In recent years, dietary patterns have shifted towards a diet that is high in saturated fats, cholesterol, and sugar, but low in unsaturated fats and fiber, and these have been regarded as an important contributor to the increasing prevalence of chronic diseases, including obesity, cardiovascular diseases, and cancers [
1,
2,
3,
4,
5]. A growing number of studies have shown that the shift in dietary patterns has contributed to a large disease burden [
3,
6]. China has been undergoing a dramatic transition in disease and dietary patterns, accompanied by rapid economic growth, lifestyle changes, and population aging [
7,
8].
Most previous studies have focused on dietary pattern shifts in the Chinese urban population of all age groups [
4,
5,
9,
10,
11,
12,
13], but have ignored the rural residents. In China, a higher proportion of rural residents are below the average poverty levels, and are also more likely to fall victim to over-nutrition or under-nutrition than urban residents [
9]. Mortality in the rural population is also substantially higher than that in the urban population [
9]. In addition, China’s population is ageing rapidly. There are currently 618 million rural residents, making up almost half of China’s total population. Therefore, more attention should be paid to the nutrition transition in rural communities. Although there have been some reports on the lifestyles and status of chronic diseases in rural people in China, few studies have focused on the trends in nutrient intakes. Moreover, evaluations on food consumption trends could help social agencies to gain some insight into the implementation and monitoring of health and nutrition policies, as well as evaluations on how public health information is perceived and actualized by the population [
14]. The present study aimed to examine the secular trends in dietary energy and macronutrient intake among rural Chinese groups between 1991 and 2011, using data from the China Health and Nutrition Survey (CHNS).
3. Results
Table 1 presents the characteristics of the rural adult population aged 18–60 years in the CHNS, by survey year. The sample size was 4926 in 1991, 5212 in 1993, 5441 in 1997, 6036 in 2000, 5318 in 2004, 5112 in 2006, 5134 in 2009, and 4560 in 2011. The mean age ranged from 36.2 to 43.7 years, and there were statistically significant differences across the survey periods (
p < 0.01). There were no significant differences in the distribution of sex across the survey years. However, we observed significant temporal trends in family income and urbanicity across the survey years (
p < 0.01), which indicated that rapid economic growth and dramatic urbanicity have occurred in the past 20 years in China.
As shown in
Table 2, energy intakes among the Chinese rural population steadily declined over time across all age (18–39 and 40–60 years), sex, region, urbanicity, and income groups (
p < 0.0001). The average daily energy intake decreased from 2512.7 kcal in 1991, to 2192.0 kcal in 2011. It is worth noting that the decline in energy intakes of rural adults in the younger age group (355.9 kcal/day), was larger than that in the older group (282.8 kcal/day). Moreover, the largest decline in energy intake, of 391.8 kcal/day, was found in low-income groups. This decline was larger than that in the medium- (306.2 kcal/day) or high-income groups (286.6 kcal/day).
Likewise, as seen in
Table 3, the daily carbohydrate intake steadily dropped across the survey years in each age group, sex, region, urbanicity, and different income group (
p < 0.0001). The daily carbohydrate intake dropped from 394.8 g in 1991, to 319.4 g in 2011. The decline in carbohydrate intake in rural women was higher than that in rural men. Furthermore, the decline in carbohydrate intake in the rural population from the low-income group was higher than that in medium- and high-income groups.
Table 4 shows that the daily fat intake in the Chinese rural population increased from 65.8 to 76.9 g (
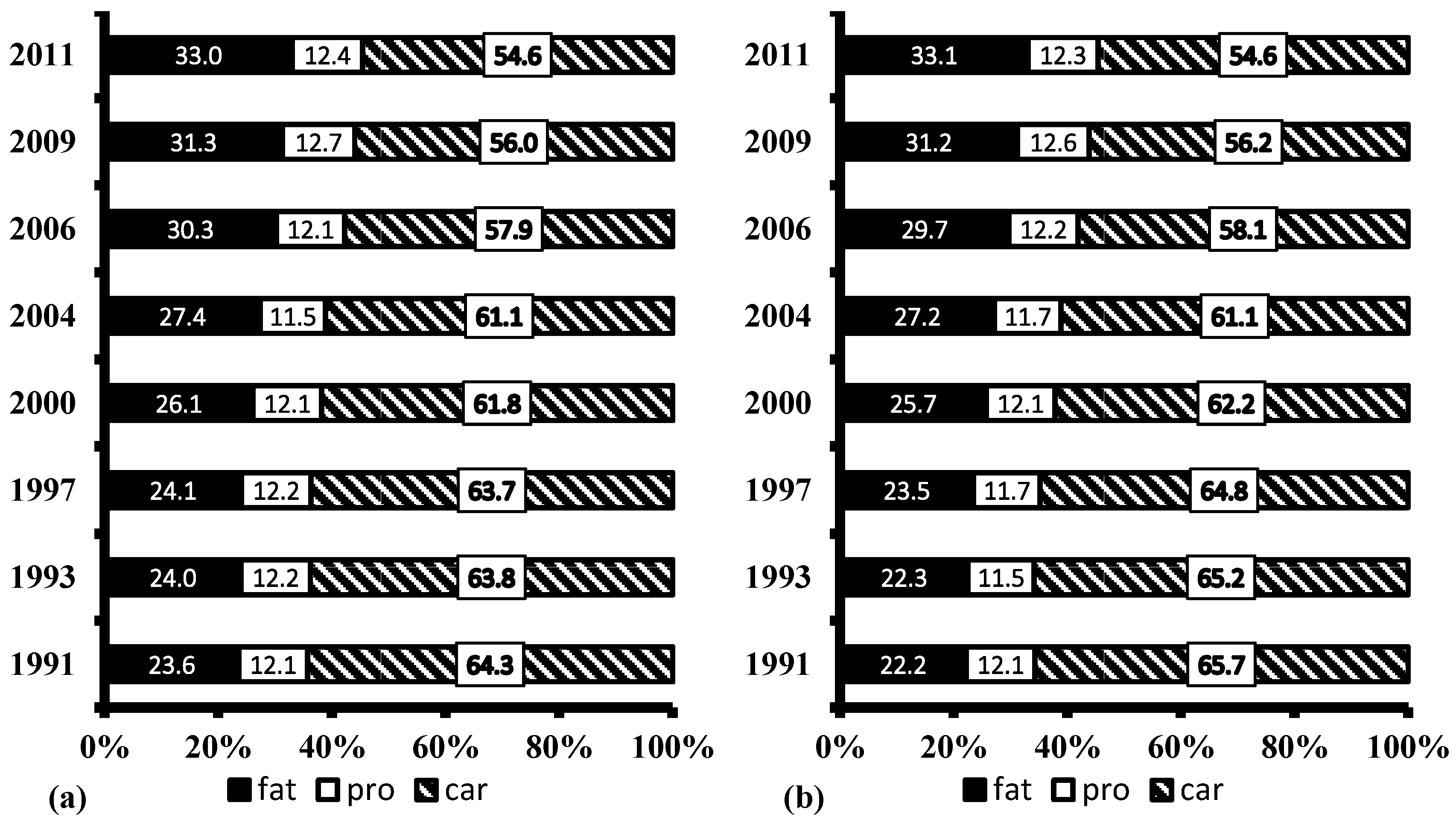
p < 0.0001), from 1991 to 2011. Meanwhile, the energy intake of rural residents substantially decreased. As a result, the proportion of energy from fat increased, while the proportion of energy from carbohydrate decreased, from 1991 to 2011, in both males and females (
Figure 1). The proportion of the rural population consuming a diet with more than 30% of energy from fat increased from 24.6% in 1991, to 58.3% in 2011 (
Table 5). Furthermore, the increase in the proportion of the rural population who consumed more than 30% of energy from fat was greater in the low-income group than in high-income group, while the increase was larger in the high-urbanicity group than in the low-urbanicity group.
Table 6 presents the daily protein intake among the Chinese rural population from 1991 to 2011, which steadily declined from 75.3 g to 64.4 g during this period (
p < 0.0001). We observed that the daily protein intake steadily dropped across the survey years in each age group, sex, region, urbanicity, and different income groups (
p < 0.0001).
4. Discussion
Previous studies have evaluated the nutritional status and nutrition transition in different countries [
24,
25,
26,
27,
28], but no previous studies have assessed the dietary energy and macronutrient intakes in Chinese rural people across three levels of urbanicity, in three regions of China. The present study shows that dietary energy intake has dramatically decreased between 1991 and 2011, while the dominant dietary pattern has shifted from one high in carbohydrate, to one high in fat. The proportion of rural people consuming a high fat diet more than tripled from 1991 to 2011. Findings from the present study indicate that Chinese rural people have been undergoing a rapid nutrition transition in the past two decades, supported by economic growth and rapid modernisation. It is especially noted that the largest transitions in dietary patterns took place in rural people from low-income households. Our results suggest that the disease burdens brought about by the nutrition transition may shift toward low-income rural people in China in the future.
Our findings indicated that the total energy intake in Chinese rural populations significantly declined during the past two decades. The observed trend is consistent with that observed in an urban population from 2394.6 kcal in 1992, to 2053.0 kcal in 2012 [
29,
30]. However, the decline in energy intake in Chinese urban people during the same period was much larger than that in rural people between the 1990s and 2010s. These findings are also in agreement with a previous study, which showed a steady decrease in the total energy intake for Indian rural women, from 2014.0 kcal in 1997 to 1780.0 kcal in 2011, in parallel with economic development [
31]. Given the rapid increase in the prevalence of overweight and obese Chinese people, a potential explanation for this decline in the total energy intake is a decrease in the total energy expenditure. In our previous study, it was illustrated that both occupational and domestic activity decreased, and sedentary hours increased in the Chinese population during the past two decades [
32]. There are also other reasons for such a decline, such as an increased underestimation of dietary intake [
33], and it would be important to distinguish the outcomes of these factors in future research.
A notable change in the total fat intake and the proportion of energy from fat has occurred in Chinese rural adults during the last two decades. In both genders, the total fat intake increased from 1991 to 2011, by 18.4% in men and by 15.6% in women. Similar trends have been found in the urban population enrolled in the China National Nutrition and Health Survey (CHNNS) between 1992 and 2012 [
29,
30]. Most previous studies have reported a positive link between the increased total fat intake in adults worldwide, and economic growth and nutrition transitions in the past several decades [
24,
25,
26]. Contrary to our results, the total fat intake in Indian rural women decreased from a very low fat consumption of 25.2 g in 1997, to 25.1 g in 2011 [
31]. It is worth noting that an increase in the consumption of total fat was also observed in South Korea [
28], but South Koreans maintained a low- fat, traditional diet, because of the nationwide campaign advocating healthy eating habits. Hence, if reasonable measures are taken, a traditional diet can be maintained, despite rapid economic growth.
As a main source of dietary energy, carbohydrate plays a critical role in the Chinese traditional diet. A continuous decrease in carbohydrate intake was observed, which is in agreement with a previous study that confirmed a decline of carbohydrate consumption in Chinese urban adults from 348.7 g in 1992, to 261.1 g in 2012 [
29,
30]. The decrease in carbohydrate can partly be explained by the drop in energy expenditure, as Chinese lifestyles have become more sedentary [
32]. The drop in the carbohydrate intake in Chinese rural adults was similar to that found in adults in some developing Asian countries, but was inconsistent with adults in Morocco and Chile [
24,
25], where the consumption of carbohydrate increased, resulting in an increase in the total energy intake over the past four decades.
A dramatic decline was observed regarding the consumption of total protein in rural adults’ diets, a result also recorded elsewhere [
31]. Our results are supported by the official data [
29], which showed a decrease in protein intake of 3% in 2002 relative to 1982, and also by a previous study, which showed a slow decrease in protein intake in women between 1997 and 2011 [
31]. The reasons for the decline in protein intake are difficult to identify and can only be speculated. For instance, a potential explanation may be due to significantly reduced plant food. Future efforts are needed to explore the other impossible reasons.
The Chinese Dietary Guideline (CDG) of 2016 suggested that, for Chinese adults, the total energy derived from carbohydrate, fat, and protein, was 55%–65%, below 30%, and 10%–15%, respectively [
34]. The present study indicates that the total energy intakes derived from carbohydrate, protein, and fat in males (54.6%, 12.4%, and 33.0%, respectively) were very similar to those (54.6%, 12.3%, and 33.1%, respectively) in females in 2011. The proportion of total energy from protein and carbohydrate is in line with the CDG recommendation, but the proportion of total energy from fat exceeded the recommendation. Moreover, the proportion of rural adults consuming a diet with more than 30% of total energy from fat more than tripled from 1991 to 2011 (nearly 60%). Excessive fat intake may lead to the development of NCD and chronic conditions such as hypertension [
35], overweight and obesity [
36,
37], and type 2 diabetes [
38]. Accordingly, the Chinese government need to take immediate actions to implement effective interventions which promote a healthy diet, considering a rapid acceleration of nutrition and epidemiological transition with an increased burden of NCDs [
39]. These measures are especially needed in China’s southern rural regions, where approximately two-thirds of the Chinese rural people had relative fat intakes higher than those recommended by CDG.
Relative to many parts of the developing world, as the biggest developing country, a double burden of undernutrition and overnutrition have been observed in the Chinese population [
40]. About 50% of China’s population resides in rural China. Experiencing a faster change of dietary pattern, the nutrition status in the rural population is gradually shifting from undernutrtion to overnutrition. The excess of the total energy intake and macronutrients is known to have a negative impact on a population’s health and can lead to an increased risk of NCD [
36]. Apart from the influence of rapid nutrition transition, the rural populations are also at a higher risk of NCDs because of low health literacy, compared to the urban population [
41,
42]. Currently, some food programs have been pursued by the Chinese government, which target the rural population and aim to improve their dietary quality and promote the development of better eating habits. These programs could have great effects on controlling and preventing the rapid increase of NCDs.
The present study has many strengths, including its large sample size with a wide age range, which was carried out by staff trained in the study’s methodology and the simultaneous standardization of different parameters, by the same scientists. The use of the individual, consecutive three-day recall method could improve the accuracy of dietary recalls and hence, the analysis and results [
43]. Moreover, mixed-effect modeling could reduce bias and increase the accuracy of estimates.
Several limitations warrant cautious interpretations of our findings. First, dietary data were collected using three consecutive 24-h dietary recalls, which might have relatively limited corrections for within-subject variations, compared to non-consecutive 24-h recalls. However, the average intake over three days can offer a relatively valid estimate of nutrient intakes, as shown in an earlier study using the CHNS [
44]. Secondly, individuals may report their food consumption inaccurately because of various reasons such as memory, knowledge, and the interview situation [
31]. Furthermore, it is possible that the obese participants might have under-reported their true habitual food intake, compared with non-obese participants [
45]. In addition, the CHNS does not present national data and the vast, western areas of China were not included in the present study.