Hypocholesterolemic Effects of Probiotic Mixture on Diet-Induced Hypercholesterolemic Rats
Abstract
:1. Introduction
2. Materials and Methods
2.1. Bacteria and Culture
2.2. Animals and Study Design
2.3. Measurement of Serum Lipids and Alanine Transaminase (ALT) and Aspartate Transaminase (AST)
2.4. Liver Histological Analysis
2.5. Measurement of Hepatic TC and TG
2.6. Western Blot Analysis
2.7. Statistical Analysis
3. Results
3.1. Effects of Probiotics Mixture on Hypercholesterolemic Rats
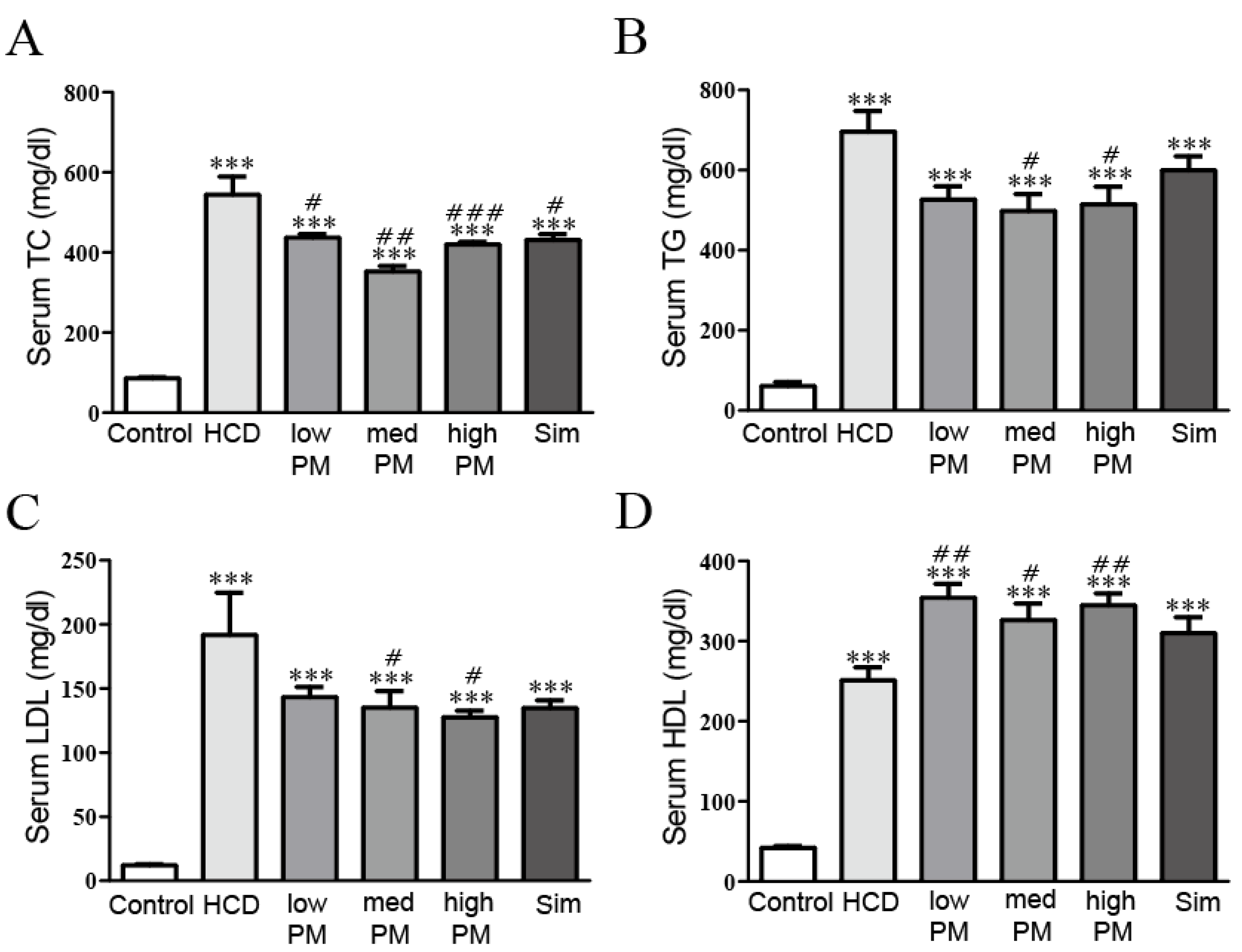
3.2. Effects of Probiotics Mixture on Serum Lipid Levels in Hypercholesterolemic Rats
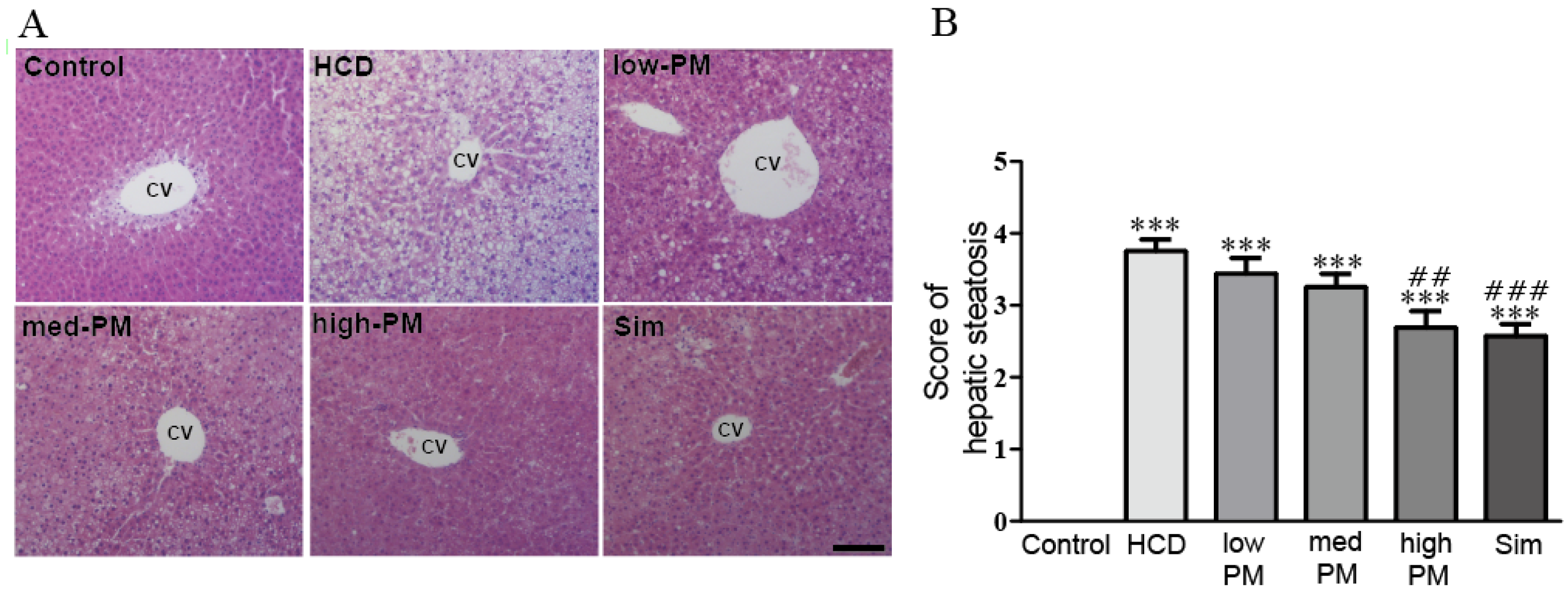
3.3. Effects of Probiotics Mixture on Hepatic Steatosis in Hypercholesterolemic Rats
3.4. Effects of Probiotics Mixture on Hepatic ALT, AST, TC, and TG in Hypercholesterolemic Rats
3.5. Effects of Probiotics Mixture on Expressions of Hepatic Cholesterol Homeostasis-Related Proteins in Hypercholesterolemic Rats
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Gielen, S.; Landmesser, U. The year in cardiology 2013: Cardiovascular disease prevention. Eur. Heart J. 2014, 35, 307–312. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Cardiovascular Disease; Fact. Sheet n°317; WHO: Geneva, Swizerland, 2009. [Google Scholar]
- Davis, C.E.; Rifkind, B.M.; Brenner, H.; Gordon, D.J. A single cholesterol measurement underestimates the risk of coronary heart disease. An empirical example from the Lipid Research Clinics Mortality Follow-up Study. JAMA 1990, 264, 3044–3046. [Google Scholar] [CrossRef] [PubMed]
- Tunstall-Pedoe, H.; Vanuzzo, D.; Hobbs, M.; Mahonen, M.; Cepaitis, Z.; Kuulasmaa, K.; Keil, U. Estimation of contribution of changes in coronary care to improving survival, event rates, and coronary heart disease mortality across the WHO MONICA Project populations. Lancet 2000, 355, 688–700. [Google Scholar] [CrossRef]
- Dai, F.J.; Hsu, W.H.; Huang, J.J.; Wu, S.C. Effect of pigeon pea (Cajanus cajan L.) on high-fat diet-induced hypercholesterolemia in hamsters. Food Chem. Toxicol. 2013, 53, 384–391. [Google Scholar] [CrossRef] [PubMed]
- Browning, J.D.; Horton, J.D. Molecular mediators of hepatic steatosis and liver injury. J. Clin. Investig. 2004, 114, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Matteoni, C.A.; Younossi, Z.M.; Gramlich, T.; Boparai, N.; Liu, Y.C.; McCullough, A.J. Nonalcoholic fatty liver disease: A spectrum of clinical and pathological severity. Gastroenterology 1999, 116, 1413–1419. [Google Scholar] [CrossRef]
- Marchesini, G.; Brizi, M.; Bianchi, G.; Tomassetti, S.; Bugianesi, E.; Lenzi, M.; McCullough, A.J.; Natale, S.; Forlani, G.; Melchionda, N. Nonalcoholic fatty liver disease: A feature of the metabolic syndrome. Diabetes 2001, 50, 1844–1850. [Google Scholar] [CrossRef] [PubMed]
- Younossi, Z.M.; Gramlich, T.; Liu, Y.C.; Matteoni, C.; Petrelli, M.; Goldblum, J.; Rybicki, L.; McCullough, A.J. Nonalcoholic fatty liver disease: Assessment of variability in pathologic interpretations. Mod. Pathol. 1998, 11, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Bugianesi, E.; Leone, N.; Vanni, E.; Marchesini, G.; Brunello, F.; Carucci, P.; Musso, A.; De Paolis, P.; Capussotti, L.; Salizzoni, M.; et al. Expanding the natural history of nonalcoholic steatohepatitis: From cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology 2002, 123, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Neuschwander-Tetri, B.A.; Caldwell, S.H. Nonalcoholic steatohepatitis: Summary of an AASLD single topic conference. Hepatology 2003, 37, 1202–1219. [Google Scholar] [CrossRef] [PubMed]
- Food and Agriculture Organization (FAO)/World Health Organization (WHO). Evaluation of Health and Nutritional Properties of Powder Milk and Live Lactic Acid Bacteria; Food and Agriculture Organization of the United Nations and World Health Organization Expert Consultation Report; FAO/WHO: Rome, Italy, 2001. [Google Scholar]
- Holzapfel, W.H.; Schillinger, U. Introduction to pre- and probiotics. Food Res. Int. 2002, 35, 109–116. [Google Scholar] [CrossRef]
- Yeo, S.K.; Liong, M.T. Angiotensin I-converting enzyme inhibitory activity and bioconversion of isoflavones by probiotics in soymilk supplemented with prebiotics. Int. J. Food Sci. Nutr. 2010, 61, 161–181. [Google Scholar] [CrossRef] [PubMed]
- Hirayama, K.; Rafter, J. The role of probiotic bacteria in cancer prevention. Microbes Infect. 2000, 2, 681–686. [Google Scholar] [CrossRef]
- Weston, S.; Halbert, A.; Richmond, P.; Prescott, S.L. Effects of probiotics on atopic dermatitis: A randomised controlled trial. Arch. Dis. Child. 2005, 90, 892–897. [Google Scholar] [CrossRef]
- Baharav, E.; Mor, F.; Halpern, M.; Weinberger, A. Lactobacillus GG bacteria ameliorate arthritis in lewis rats. J. Nutr. 2004, 134, 1964–1969. [Google Scholar] [PubMed]
- Kumar, M.; Rakesh, S.; Nagpal, R.; Hemalatha, R.; Ramakrishna, A.; Sudarshan, V.; Ramagoni, R.; Shujauddin, M.; Verma, V.; Kumar, A.; et al. Probiotic Lactobacillus rhamnosus GG and Aloe vera gel improve lipid profiles in hypercholesterolemic rats. Nutrition 2013, 29, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.W.; Gilliland, S.E. Effect of fermented milk (yogurt) containing Lactobacillus acidophilus L1 on serum cholesterol in hypercholesterolemic humans. J. Am. Coll. Nutr. 1999, 18, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.Z.; Kondo, S.; Takahashi, N.; Miyaji, K.; Oshida, K.; Hiramatsu, A.; Iwatsuki, K.; Kokubo, S.; Hosono, A. Effects of milk products fermented by Bifidobacterium longum on blood lipids in rats and healthy adult male volunteers. J. Dairy Sci. 2003, 86, 2452–2461. [Google Scholar] [CrossRef]
- Paigen, B.; Morrow, A.; Brandon, C.; Mitchell, D.; Holmes, P. Variation in susceptibility to atherosclerosis among inbred strains of mice. Atherosclerosis 1985, 57, 65–73. [Google Scholar] [CrossRef]
- Kleiner, D.E.; Brunt, E.M.; Van Natta, M.; Behling, C.; Contos, M.J.; Cummings, O.W.; Ferrell, L.D.; Liu, Y.C.; Torbenson, M.S.; Unalp-Arida, A.; et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005, 41, 1313–1321. [Google Scholar] [CrossRef] [PubMed]
- Brunt, E.M.; Kleiner, D.E.; Wilson, L.A.; Belt, P.; Neuschwander-Tetri, B.A.; Network, N.C.R. Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: Distinct clinicopathologic meanings. Hepatology 2011, 53, 810–820. [Google Scholar] [CrossRef] [PubMed]
- Artham, S.M.; Lavie, C.J.; Milani, R.V.; Ventura, H.O. The obesity paradox: Impact of obesity on the prevalence and prognosis of cardiovascular diseases. Postgrad. Med. 2008, 120, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Bellentani, S.; Saccoccio, G.; Masutti, F.; Croce, L.S.; Brandi, G.; Sasso, F.; Cristanini, G.; Tiribelli, C. Prevalence of and risk factors for hepatic steatosis in northern Italy. Ann. Intern. Med. 2000, 132, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, C.J.; Murphy, M.B.; Buckley, B.M. Statins do more than just lower cholesterol. Lancet 1996, 348, 1079–1082. [Google Scholar] [CrossRef]
- Bellosta, S.; Paoletti, R.; Corsini, A. Safety of statins: Focus on clinical pharmacokinetics and drug interactions. Circulation 2004, 109, III50–III57. [Google Scholar] [CrossRef] [PubMed]
- El-Shafie, H.A.; Yahia, N.I.; Ali, H.A.; Khalil, F.A.; El-Kady, E.M.; Moustafa, Y.A. Hypocholesterolemic action of Lactobacillus plantarum NRRL-B-4524 and lactobacillus paracasei in mice with hypercholesterolemia induced by diet. Aust. J. Basic Appl. Sci. 2009, 3, 218–228. [Google Scholar]
- Chen, D.; Yang, Z.; Chen, X.; Huang, Y.; Yin, B.; Guo, F.; Zhao, H.; Zhao, T.; Qu, H.; Huang, J.; et al. The effect of Lactobacillus rhamnosus hsryfm 1301 on the intestinal microbiota of a hyperlipidemic rat model. BMC Complement. Altern. Med. 2014, 14, 386. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.Y.; Chen, J.H.; Chang, J.H.; Lin, H.C.; Lin, C.Y.; Peng, C.C. Multiple strains probiotics appear to be the most effective probiotics in the prevention of necrotizing enterocolitis and mortality: An updated meta-analysis. PLoS ONE 2017, 12, e0171579. [Google Scholar] [CrossRef] [PubMed]
- Al-Muzafar, H.M.; Amin, K.A. Probiotic mixture improves fatty liver disease by virtue of its action on lipid profiles, leptin, and inflammatory biomarkers. BMC Complement. Altern. Med. 2017, 17, 43. [Google Scholar] [CrossRef] [PubMed]
- Pereira, D.I.; Gibson, G.R. Effects of consumption of probiotics and prebiotics on serum lipid levels in humans. Crit. Rev. Biochem. Mol. Biol. 2002, 37, 259–281. [Google Scholar] [CrossRef] [PubMed]
- Shimomura, I.; Bashmakov, Y.; Horton, J.D. Increased levels of nuclear SREBP-1c associated with fatty livers in two mouse models of diabetes mellitus. J. Biol. Chem. 1999, 274, 30028–30032. [Google Scholar] [CrossRef] [PubMed]
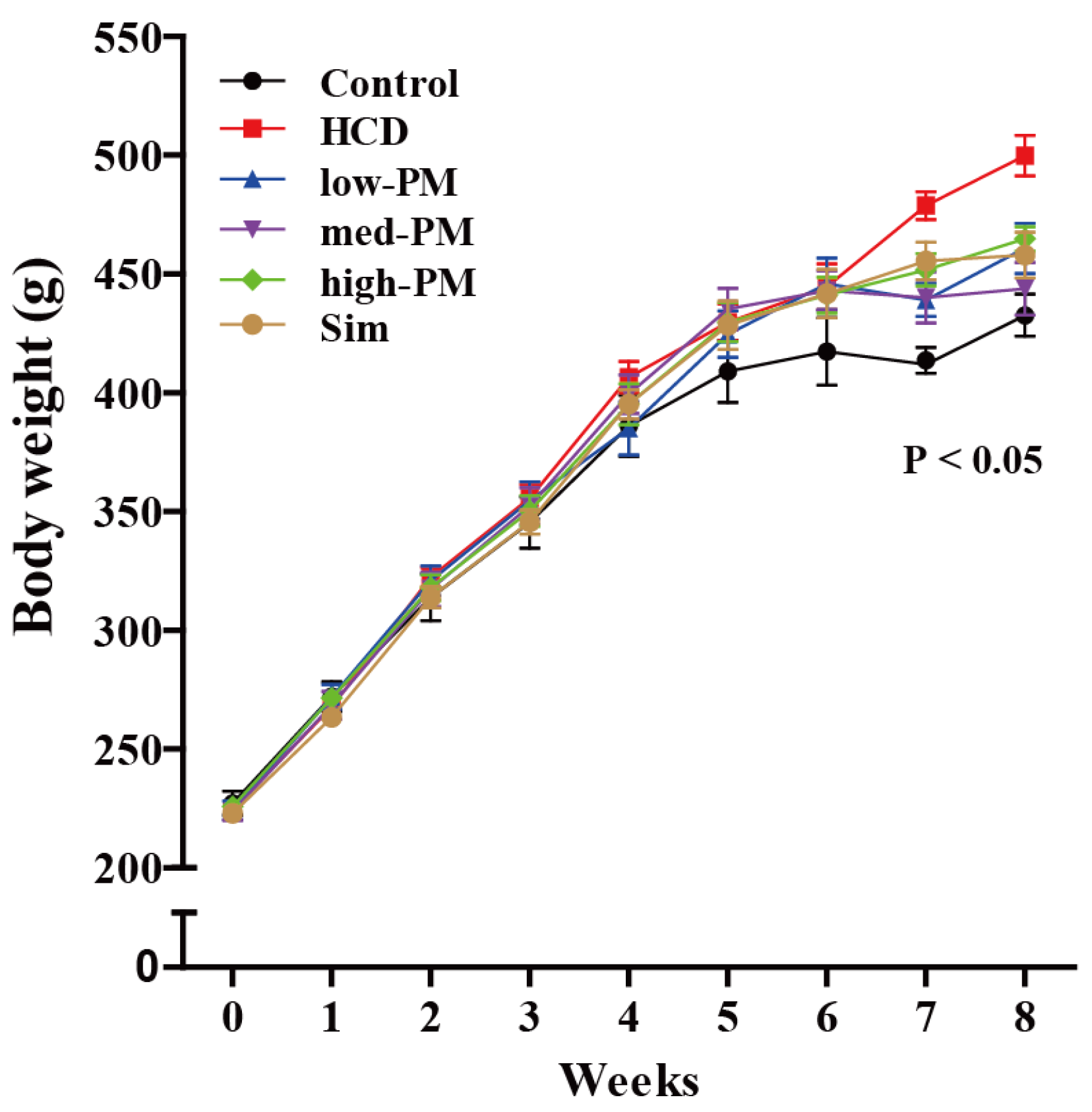

| Parameter | Control | HCD | Low-PM | Med-PM | High-PM | Simvastatin |
|---|---|---|---|---|---|---|
| Initial BW (g) | 227.2 ± 5.1 | 224.8 ± 2.6 | 224.3 ± 3.6 | 223.8 ± 3.6 | 226.0 ± 2.3 | 223.1 ± 2.2 |
| Final BW (g) | 432.7 ± 8.8 | 499.8 ± 8.5 # | 460.8 ± 10.5 * | 443.8 ± 11.0 * | 464.8 ± 5.1 * | 458.0 ± 9.6 * |
| Food intake (g/day) | 19.0 ± 0.5 | 18.37 ± 0.3 | 19.2 ± 0.6 | 19.1 ± 0.3 | 19.0 ± 0.5 | 18.9 ± 0.5 |
| Water intake (g/day) | 33.4 ± 1.5 | 28.0 ± 0.8 | 30.0 ± 1.7 | 31.2 ± 1.0 | 30.5 ± 0.7 | 27.5 ± 0.4 |
| Parameter | Control | HCD | Low-PM | Med-PM | High-PM | Sim |
|---|---|---|---|---|---|---|
| ALT (IU/L) | 72.3 ± 4.8 | 117.7 ± 18.5 ## | 75.8 ± 17.9 * | 69.7 ± 14.7 ** | 93.2 ± 10.7 * | 82.3 ± 14.4 * |
| AST (IU/L) | 136.0 ± 12.9 | 171.3 ± 18.1 # | 122.2 ± 13.9 ** | 103.2 ± 9.4 ** | 135.2 ± 11.9 * | 118.4 ± 12.7 * |
| TG (mg/dL) | 43.8 ± 4.3 | 140.3 ± 54.9 ## | 128.6 ± 32.4 * | 116.9 ± 34.5 * | 89.54 ± 14.5 ** | 92.58 ± 16.6 * |
| TC (mg/dL) | 41.6 ± 11.4 | 152.4 ± 27.1 ## | 143.3 ± 32.2 * | 136.5 ± 61.4 * | 134.9 ± 46.8 * | 127.0 ± 52.1 * |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.-J.; Park, S.H.; Sin, H.-S.; Jang, S.-H.; Lee, S.-W.; Kim, S.-Y.; Kwon, B.; Yu, K.-Y.; Kim, S.Y.; Yang, D.K. Hypocholesterolemic Effects of Probiotic Mixture on Diet-Induced Hypercholesterolemic Rats. Nutrients 2017, 9, 293. https://doi.org/10.3390/nu9030293
Kim S-J, Park SH, Sin H-S, Jang S-H, Lee S-W, Kim S-Y, Kwon B, Yu K-Y, Kim SY, Yang DK. Hypocholesterolemic Effects of Probiotic Mixture on Diet-Induced Hypercholesterolemic Rats. Nutrients. 2017; 9(3):293. https://doi.org/10.3390/nu9030293
Chicago/Turabian StyleKim, Shang-Jin, Sang Hoon Park, Hong-Sig Sin, Seung-Hwan Jang, Sang-Wang Lee, Seon-Young Kim, Bora Kwon, Kang-Yeol Yu, Su Young Kim, and Dong Kwon Yang. 2017. "Hypocholesterolemic Effects of Probiotic Mixture on Diet-Induced Hypercholesterolemic Rats" Nutrients 9, no. 3: 293. https://doi.org/10.3390/nu9030293





