Risk of Deficiency in Multiple Concurrent Micronutrients in Children and Adults in the United States
Abstract
:1. Introduction
2. Materials and Methods
2.1. Description of Dataset
2.2. Criteria for Determining Biochemical Vitamin and Mineral Status, Biochemical Deficiency Score and Dietary Inadequacy Score
2.3. Selection of Full Spectrum Multivitamin-Multimineral Supplements
2.4. Statistical Methods
3. Results
3.1. Individual Biochemical Deficiencies and Insufficient Intakes of Vitamins and Minerals
3.2. Overall Inadequate Biochemical Status According to Demographic Characteristics
3.3. Biochemical Deficiencies across Age and Gender Categories
3.4. Risk of Vitamin Deficiency or Anemia by Dietary Supplement Use Categories and Age/Gender Groups
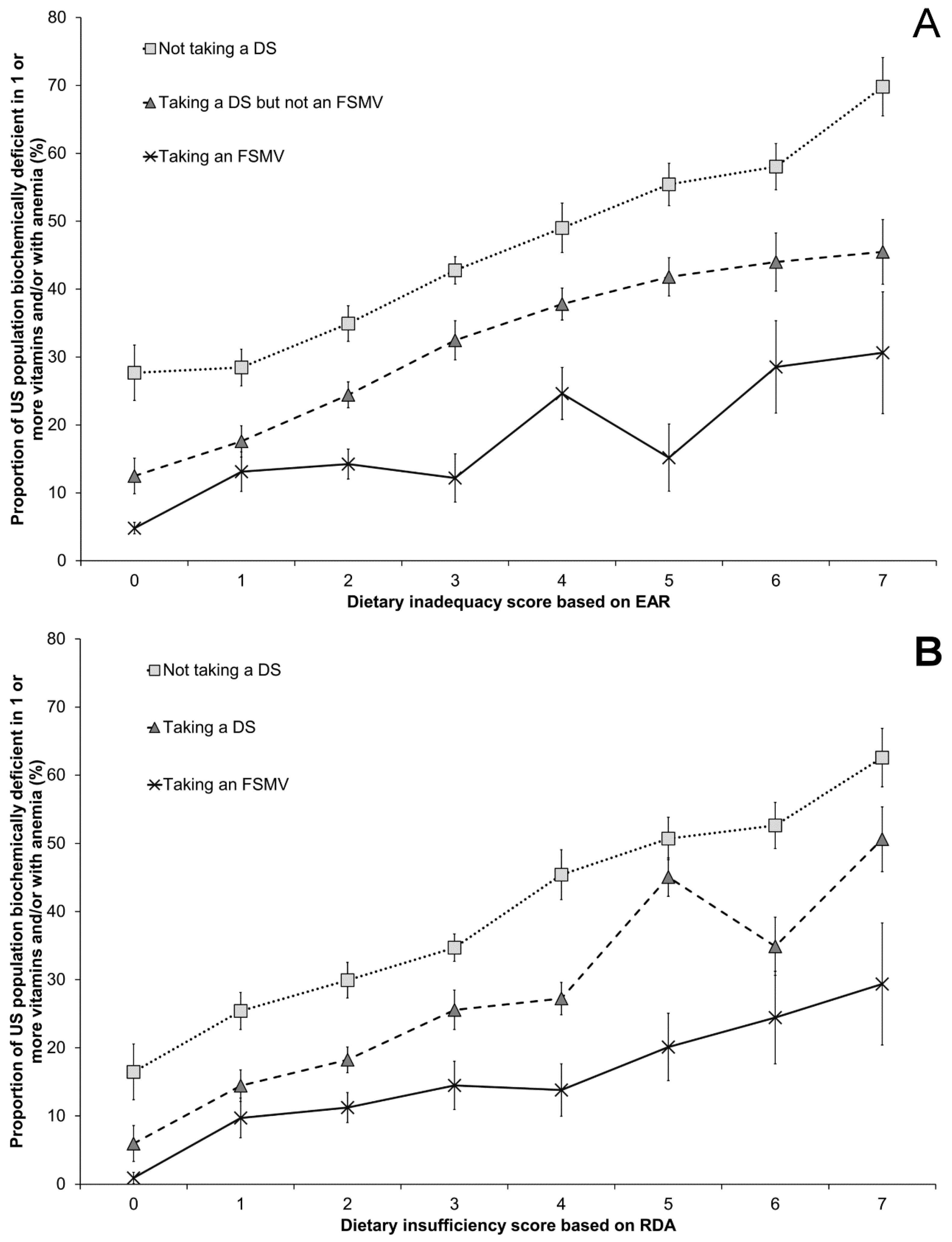
3.5. Risk of Vitamin Deficiency According to Dietary Sufficiency Score and Dietary Supplement Use
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- McGuire, S. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. Washington, DC: US Departments of Agriculture and Health and Human Services, 2015. Adv. Nutr. 2016, 7, 202–204. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, C.M.; Sternberg, M.R.; Schleicher, R.L.; Haynes, B.M.; Rybak, M.E.; Pirkle, J.L. The CDC’s Second National Report on Biochemical Indicators of Diet and Nutrition in the U.S. Population is a valuable tool for researchers and policy makers. J. Nutr. 2013, 143, 938S–947S. [Google Scholar] [CrossRef] [PubMed]
- Tanumihardjo, S. Biomarkers of vitamin A status: What do they mean. In Report: Priorities in the Assessment of Vitamin A and Iron Status in Populations, Proceedings of the Priorities in the Assessment of Vitamin A and Iron Status in Populations, Panama City, Panama, 15–19 September 2010; World Health Organisation: Geneva, Switzerland, 2012; Available online: http://www.who.int/nutrition/publications/micronutrients/background_paper2_report_assessment_vitAandIron_status.pdf (accessed on 22 June 2017).
- Schleicher, R.L.; Carroll, M.D.; Ford, E.S.; Lacher, D.A. Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003–2004 National Health and Nutrition Examination Survey (NHANES). Am. J. Clin. Nutr. 2009, 90, 1252–1263. [Google Scholar] [CrossRef] [PubMed]
- Otten, J.J.; Hellwig, J.P.; Meyers, L.D. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements; The National Academies Press: Washington, DC, USA, 2006. [Google Scholar]
- Wacker, M.; Holick, M.F. Vitamin D—Effects on skeletal and extraskeletal health and the need for supplementation. Nutrients 2013, 5, 111–148. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline; National Academies Press (US): Washington, DC, USA, 1998. [Google Scholar]
- Lane, D.J.; Richardson, D.R. The active role of vitamin C in mammalian iron metabolism: Much more than just enhanced iron absorption! Free Radic. Biol. Med. 2014, 75, 69–83. [Google Scholar] [CrossRef] [PubMed]
- Kelsay, J.L. A compendium of nutritional status studies and dietary evaluation studies conducted in the United States, 1957–1967. J. Nutr. 1969, 99 (Suppl. 1), 119–166. [Google Scholar]
- Yetley, E.; Johnson, C. Nutritional applications of the Health and Nutrition Examination Surveys (HANES). Annu. Rev. Nutr. 1987, 7, 441–463. [Google Scholar] [CrossRef] [PubMed]
- Karakis, I.; Pase, M.P.; Beiser, A.; Booth, S.L.; Jacques, P.F.; Rogers, G.; DeCarli, C.; Vasan, R.S.; Wang, T.J.; Himali, J.J.; et al. Association of Serum Vitamin D with the Risk of Incident Dementia and Subclinical Indices of Brain Aging: The Framingham Heart Study. J. Alzheimers Dis. 2016, 51, 451–461. [Google Scholar] [CrossRef] [PubMed]
- Kolonel, L.N.; Henderson, B.E.; Hankin, J.H.; Nomura, A.M.; Wilkens, L.R.; Pike, M.C.; Stram, D.O.; Monroe, K.R.; Earle, M.E.; Nagamine, F.S. A multiethnic cohort in Hawaii and Los Angeles: Baseline characteristics. Am. J. Epidemiol. 2000, 151, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Bertone-Johnson, E.R.; Powers, S.I.; Spangler, L.; Larson, J.; Michael, Y.L.; Millen, A.E.; Bueche, M.N.; Salmoirago-Blotcher, E.; Wassertheil-Smoller, S.; Brunner, R.L.; et al. Vitamin D supplementation and depression in the women's health initiative calcium and vitamin D trial. Am. J. Epidemiol. 2012, 176, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Ma, J.; Manson, J.E.; Buring, J.E.; Gaziano, J.M.; Sesso, H.D. A prospective study of plasma vitamin D metabolites, vitamin D receptor gene polymorphisms, and risk of hypertension in men. Eur. J. Nutr. 2013, 52, 1771–1779. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Second National Report on Biochemical Indicators of Diet and Nutrition in the U.S. Population; National Center for Environmental Health: Atlanta, GA, USA, April 2012. Available online: http://www.cdc.gov/nutritionreport/pdf/Nutrition_Book_complete508_final.pdf (accessed on 22 June 2017).
- Haynes, B.M.; Pfeiffer, C.M.; Sternberg, M.R.; Schleicher, R.L. Selected physiologic variables are weakly to moderately associated with 29 biomarkers of diet and nutrition, NHANES 2003–2006. J. Nutr. 2013, 143, 1001S–1010S. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, C.M.; Sternberg, M.R.; Caldwell, K.L.; Pan, Y. Race-ethnicity is related to biomarkers of iron and iodine status after adjusting for sociodemographic and lifestyle variables in NHANES 2003–2006. J. Nutr. 2013, 143, 977S–985S. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, C.M.; Sternberg, M.R.; Schleicher, R.L.; Rybak, M.E. Dietary supplement use and smoking are important correlates of biomarkers of water-soluble vitamin status after adjusting for sociodemographic and lifestyle variables in a representative sample of U.S. adults. J. Nutr. 2013, 143, 957S–965S. [Google Scholar] [CrossRef] [PubMed]
- Schleicher, R.L.; Sternberg, M.R.; Pfeiffer, C.M. Race-ethnicity is a strong correlate of circulating fat-soluble nutrient concentrations in a representative sample of the U.S. population. J. Nutr. 2013, 143, 966S–976S. [Google Scholar] [CrossRef] [PubMed]
- Sternberg, M.R.; Schleicher, R.L.; Pfeiffer, C.M. Regression modeling plan for 29 biochemical indicators of diet and nutrition measured in NHANES 2003–2006. J. Nutr. 2013, 143, 948S–956S. [Google Scholar] [CrossRef] [PubMed]
- Anderson, V.P.; Jack, S.; Monchy, D.; Hem, N.; Hok, P.; Bailey, K.B.; Gibson, R.S. Co-existing micronutrient deficiencies among stunted Cambodian infants and toddlers. Asia Pac. J. Clin. Nutr. 2008, 17, 72–79. [Google Scholar] [PubMed]
- Hashizume, M.; Chiba, M.; Shinohara, A.; Iwabuchi, S.; Sasaki, S.; Shimoda, T.; Kunii, O.; Caypil, W.; Dauletbaev, D.; Alnazarova, A. Anaemia, iron deficiency and vitamin A status among school-aged children in rural Kazakhstan. Public Health Nutr. 2005, 8, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.S.; Sampaio, P.; Muniz, P.T.; Cardoso, M.A. Multiple micronutrients in powder delivered through primary health care reduce iron and vitamin A deficiencies in young Amazonian children. Public Health Nutr. 2016, 19, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Van Nhien, N.; Khan, N.C.; Ninh, N.X.; Van Huan, P.; Hop le, T.; Lam, N.T.; Ota, F.; Yabutani, T.; Hoa, V.Q.; Motonaka, J.; et al. Micronutrient deficiencies and anemia among preschool children in rural Vietnam. Asia Pac. J. Clin. Nutr. 2008, 17, 48–55. [Google Scholar] [PubMed]
- Bailey, R.L.; Gahche, J.J.; Miller, P.E.; Thomas, P.R.; Dwyer, J.T. Why US adults use dietary supplements. JAMA Intern. Med. 2013, 173, 355–361. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Gahche, J.J.; Thomas, P.R.; Dwyer, J.T. Why US children use dietary supplements. Pediatr. Res. 2013, 74, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Rock, C.L. Multivitamin-multimineral supplements: Who uses them? Am. J. Clin. Nutr. 2007, 85, 277S–279S. [Google Scholar] [PubMed]
- Bailey, R.L.; Fulgoni, V.L., 3rd; Keast, D.R.; Dwyer, J.T. Examination of vitamin intakes among US adults by dietary supplement use. J. Acad. Nutr. Diet. 2012, 112, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Fulgoni, V.L., 3rd; Keast, D.R.; Bailey, R.L.; Dwyer, J. Foods, fortificants, and supplements: Where do Americans get their nutrients? J. Nutr. 2011, 141, 1847–1854. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Murphy, S.P.; Martin, C.L.; Kolonel, L.N. Nutrient intake from multivitamin/mineral supplements is similar among users from five ethnic groups: The Multiethnic Cohort Study. J. Am. Diet. Assoc. 2008, 108, 529–533. [Google Scholar] [CrossRef] [PubMed]
- Stang, J.; Story, M.T.; Harnack, L.; Neumark-Sztainer, D. Relationships between vitamin and mineral supplement use, dietary intake, and dietary adequacy among adolescents. J. Am. Diet. Assoc. 2000, 100, 905–910. [Google Scholar] [CrossRef]
- Dickinson, A.; MacKay, D. Health habits and other characteristics of dietary supplement users: A review. Nutr. J. 2014, 13, 14. [Google Scholar] [CrossRef] [PubMed]
- Stewart, P.A.; Hyman, S.L.; Schmidt, B.L.; Macklin, E.A.; Reynolds, A.; Johnson, C.R.; James, S.J.; Manning-Courtney, P. Dietary Supplementation in Children with Autism Spectrum Disorders: Common, Insufficient, and Excessive. J. Acad. Nutr. Diet. 2015, 115, 1237–1248. [Google Scholar] [CrossRef] [PubMed]
- The Age-Related Eye Disease Study (AREDS): Design implications. AREDS report no. 1. Control Clin. Trials 1999, 20, 573–600.
- Chew, E.Y.; Clemons, T.; SanGiovanni, J.P.; Danis, R.; Domalpally, A.; McBee, W.; Sperduto, R.; Ferris, F.L. The Age-Related Eye Disease Study 2 (AREDS2): Study design and baseline characteristics (AREDS2 report number 1). Ophthalmology 2012, 119, 2282–2289. [Google Scholar] [CrossRef] [PubMed]
- Gaziano, J.M.; Sesso, H.D.; Christen, W.G.; Bubes, V.; Smith, J.P.; MacFadyen, J.; Schvartz, M.; Manson, J.E.; Glynn, R.J.; Buring, J.E. Multivitamins in the prevention of cancer in men: The Physicians' Health Study II randomized controlled trial. JAMA 2012, 308, 1871–1880. [Google Scholar] [CrossRef] [PubMed]
- Zipf, G.; Chiappa, M.; Porter, K.S.; Ostchega, Y.; Lewis, B.G.; Dostal, J. National health and nutrition examination survey: Plan and operations, 1999–2010. Vital Health Stat. 1 2013, 1–37. [Google Scholar]
- National Center for Health Statistics. About the National Health and Nutrition Examination Survey. Available online: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm (accessed on 21 April 2015).
- Centers for Disease Control and Prevention. 2005–2006 Data Documentation, Codebook, and Frequencies. Vitamin B6 (VIT_B6_D). Analytic notes. Available online: http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/VIT_B6_D.htm#Analytic_Notes (accessed on 10 February 2016).
- World Health Organization. Iron Deficiency Anaemia. Assessment, Prevention, and Control. A Guide for Programme Managers; WHO/NHD/01.3; WHO: Geneva, Switzerland, 2001; Available online: http://whqlibdoc.who.int/hq/2001/WHO_NHD_01.3.pdf (accessed on 22 June 2017).
- Short, M.W.; Domagalski, J.E. Iron deficiency anemia: Evaluation and management. Am. Fam. Physician 2013, 87, 98–104. [Google Scholar] [PubMed]
- Dallal, G.E. Identifying Similar Groups. Available online: http://www.jerrydallal.com/lhsp/similar_prog.htm (accessed on 29 January 2016).
- Johnson, C.; Paulose-Ram, R.; Ogden, C.; Carroll, M.; Kruszon-Moran, D.; Dohrmann, S.; Curtin, L. National Health and Nutrition Examination Survey: Analytic guidelines, 1999–2010. Vital Health Stat. 2013, 161, 1–24. [Google Scholar]
- Bailey, R.L.; Carmel, R.; Green, R.; Pfeiffer, C.M.; Cogswell, M.E.; Osterloh, J.D.; Sempos, C.T.; Yetley, E.A. Monitoring of vitamin B-12 nutritional status in the United States by using plasma methylmalonic acid and serum vitamin B-12. Am. J. Clin. Nutr. 2011, 94, 552–561. [Google Scholar] [CrossRef] [PubMed]
- Branum, A.M.; Bailey, R.; Singer, B.J. Dietary supplement use and folate status during pregnancy in the United States. J. Nutr. 2013, 143, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Kant, A.K.; Graubard, B.I. Race-ethnic, family income, and education differentials in nutritional and lipid biomarkers in US children and adolescents: NHANES 2003–2006. Am. J. Clin. Nutr. 2012, 96, 601–612. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, C.M.; Hughes, J.P.; Lacher, D.A.; Bailey, R.L.; Berry, R.J.; Zhang, M.; Yetley, E.A.; Rader, J.I.; Sempos, C.T.; Johnson, C.L. Estimation of trends in serum and RBC folate in the U.S. population from pre–to postfortification using assay-adjusted data from the NHANES 1988–2010. J. Nutr. 2012, 142, 886–893. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Cogswell, M.E.; Hamner, H.C.; Carriquiry, A.; Bailey, L.B.; Pfeiffer, C.M.; Berry, R.J. Folic acid source, usual intake, and folate and vitamin B-12 status in US adults: National Health and Nutrition Examination Survey (NHANES) 2003–2006. Am. J. Clin. Nutr. 2010, 91, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.S.; Picciano, M.F.; Jacques, P.F.; Selhub, J. Plasma pyridoxal 5'-phosphate in the US population: The National Health and Nutrition Examination Survey, 2003–2004. Am. J. Clin. Nutr. 2008, 87, 1446–1454. [Google Scholar] [PubMed]
- Cogswell, M.E.; Looker, A.C.; Pfeiffer, C.M.; Cook, J.D.; Lacher, D.A.; Beard, J.L.; Lynch, S.R.; Grummer-Strawn, L.M. Assessment of iron deficiency in US preschool children and nonpregnant females of childbearing age: National Health and Nutrition Examination Survey 2003–2006. Am. J. Clin. Nutr. 2009, 89, 1334–1342. [Google Scholar] [CrossRef] [PubMed]
- Hanson, C.; Lyden, E.; Abresch, C.; Anderson-Berry, A. Serum Retinol Concentrations, Race, and Socioeconomic Status in of Women of Childbearing Age in the United States. Nutrients 2016, 8, 508. [Google Scholar] [CrossRef] [PubMed]
- Rai, D.; Bird, J.K.; McBurney, M.I.; Chapman-Novakofski, K.M. Nutritional status as assessed by nutrient intakes and biomarkers among women of childbearing age—Is the burden of nutrient inadequacies growing in America? Public Health Nutr. 2014, 18, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Bodnar, L.M.; Simhan, H.N.; Powers, R.W.; Frank, M.P.; Cooperstein, E.; Roberts, J.M. High prevalence of vitamin D insufficiency in black and white pregnant women residing in the northern United States and their neonates. J. Nutr. 2007, 137, 447–452. [Google Scholar] [PubMed]
- Mathews, F.; Youngman, L.; Neil, A. Maternal circulating nutrient concentrations in pregnancy: Implications for birth and placental weights of term infants. Am. J. Clin. Nutr. 2004, 79, 103–110. [Google Scholar] [PubMed]
- Gibbs, B.G.; Forste, R. Socioeconomic status, infant feeding practices and early childhood obesity. Pediatr. Obes. 2014, 9, 135–146. [Google Scholar] [CrossRef] [PubMed]
- O’Neil, C.E.; Nicklas, T.A.; Keast, D.R.; Fulgoni, V.L. Ethnic disparities among food sources of energy and nutrients of public health concern and nutrients to limit in adults in the United States: NHANES 2003–2006. Food Nutr. Res. 2014, 58, 15784. [Google Scholar] [CrossRef] [PubMed]
- Kirkpatrick, S.I.; Dodd, K.W.; Reedy, J.; Krebs-Smith, S.M. Income and race/ethnicity are associated with adherence to food-based dietary guidance among US adults and children. J. Acad. Nutr. Diet. 2012, 112, 624.e6–635.e6. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, A.; Monsivais, P.; Cook, A.J.; Drewnowski, A. Positive attitude toward healthy eating predicts higher diet quality at all cost levels of supermarkets. J. Acad. Nutr. Diet. 2014, 114, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Valdes, S.T.; Tostes, M.D.; Anunciacao, P.C.; da Silva, B.P.; Sant’Ana, H.M. Association between Vitamin Deficiency and Metabolic Disorders Related to Obesity. Crit. Rev. Food Sci. Nutr. 2016, 57, 3332–3343. [Google Scholar] [CrossRef] [PubMed]
- Harris, E.; Macpherson, H.; Pipingas, A. Improved blood biomarkers but no cognitive effects from 16 weeks of multivitamin supplementation in healthy older adults. Nutrients 2015, 7, 3796–3812. [Google Scholar] [CrossRef] [PubMed]
- Kofoed, C.L.; Christensen, J.; Dragsted, L.O.; Tjonneland, A.; Roswall, N. Determinants of dietary supplement use—Healthy individuals use dietary supplements. Br. J. Nutr. 2015, 113, 1993–2000. [Google Scholar] [CrossRef] [PubMed]
- Murphy, S.P.; White, K.K.; Park, S.Y.; Sharma, S. Multivitamin-multimineral supplements' effect on total nutrient intake. Am. J. Clin. Nutr. 2007, 85, 280S–284S. [Google Scholar] [PubMed]
- Sebastian, R.S.; Cleveland, L.E.; Goldman, J.D.; Moshfegh, A.J. Older adults who use vitamin/mineral supplements differ from nonusers in nutrient intake adequacy and dietary attitudes. J. Am. Diet. Assoc. 2007, 107, 1322–1332. [Google Scholar] [CrossRef] [PubMed]
- Lacher, D.A.; Hughes, J.P.; Carroll, M.D. Estimate of biological variation of laboratory analytes based on the third national health and nutrition examination survey. Clin. Chem. 2005, 51, 450–452. [Google Scholar] [CrossRef] [PubMed]
- Ong, K.L.; Allison, M.A.; Cheung, B.M.; Wu, B.J.; Barter, P.J.; Rye, K.A. Trends in C-reactive protein levels in US adults from 1999 to 2010. Am. J. Epidemiol. 2013, 177, 1430–1442. [Google Scholar] [CrossRef] [PubMed]
- Dhurandhar, N.V.; Schoeller, D.; Brown, A.W.; Heymsfield, S.B.; Thomas, D.; Sorensen, T.I.A.; Speakman, J.R.; Jeansonne, M.; Allison, D.B.; Energy Balance Measurement Working Group. Energy balance measurement: When something is not better than nothing. Int. J. Obes. (Lond.) 2015, 39, 1109–1113. [Google Scholar] [CrossRef] [PubMed]
- Powers, H.J.; Hill, M.H.; Mushtaq, S.; Dainty, J.R.; Majsak-Newman, G.; Williams, E.A. Correcting a marginal riboflavin deficiency improves hematologic status in young women in the United Kingdom (RIBOFEM). Am. J. Clin. Nutr. 2011, 93, 1274–1284. [Google Scholar] [CrossRef] [PubMed]
- Davison, K.M.; Kaplan, B.J. Vitamin and mineral intakes in adults with mood disorders: Comparisons to nutrition standards and associations with sociodemographic and clinical variables. J. Am. Coll. Nutr. 2011, 30, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Gibson, R.S.; Heath, A.L.; Limbaga, M.L.; Prosser, N.; Skeaff, C.M. Are changes in food consumption patterns associated with lower biochemical zinc status among women from Dunedin, New Zealand? Br. J. Nutr. 2001, 86, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Bertinato, J.; Wu Xiao, C.; Ratnayake, W.M.; Fernandez, L.; Lavergne, C.; Wood, C.; Swist, E. Lower serum magnesium concentration is associated with diabetes, insulin resistance, and obesity in South Asian and white Canadian women but not men. Food Nutr. Res. 2015, 59, 25974. [Google Scholar] [CrossRef] [PubMed]
- Mensink, G.B.; Fletcher, R.; Gurinovic, M.; Huybrechts, I.; Lafay, L.; Serra-Majem, L.; Szponar, L.; Tetens, I.; Verkaik-Kloosterman, J.; Baka, A.; et al. Mapping low intake of micronutrients across Europe. Br. J. Nutr. 2013, 110, 755–773. [Google Scholar] [CrossRef] [PubMed]
- ter Borg, S.; Verlaan, S.; Hemsworth, J.; Mijnarends, D.M.; Schols, J.M.; Luiking, Y.C.; de Groot, L.C. Micronutrient intakes and potential inadequacies of community-dwelling older adults: A systematic review. Br. J. Nutr. 2015, 113, 1195–1206. [Google Scholar] [CrossRef] [PubMed]
- Lamers, Y.; O'Rourke, B.; Gilbert, L.R.; Keeling, C.; Matthews, D.E.; Stacpoole, P.W.; Gregory, J.F., 3rd. Vitamin B-6 restriction tends to reduce the red blood cell glutathione synthesis rate without affecting red blood cell or plasma glutathione concentrations in healthy men and women. Am. J. Clin. Nutr. 2009, 90, 336–343. [Google Scholar] [CrossRef] [PubMed]
- Melanson, K.J.; Angelopoulos, T.J.; Nguyen, V.T.; Martini, M.; Zukley, L.; Lowndes, J.; Dube, T.J.; Fiutem, J.J.; Yount, B.W.; Rippe, J.M. Consumption of whole-grain cereals during weight loss: Effects on dietary quality, dietary fiber, magnesium, vitamin B-6, and obesity. J. Am. Diet. Assoc. 2006, 106, 1380–1388. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Rodriguez, E.; Lopez-Sobaler, A.M.; Navarro, A.R.; Bermejo, L.M.; Ortega, R.M.; Andres, P. Vitamin B6 status improves in overweight/obese women following a hypocaloric diet rich in breakfast cereals, and may help in maintaining fat-free mass. Int. J. Obes. (Lond.) 2008, 32, 1552–1558. [Google Scholar] [CrossRef] [PubMed]
- Baker, A.H.; Wardle, J. Sex differences in fruit and vegetable intake in older adults. Appetite 2003, 40, 269–275. [Google Scholar] [CrossRef]
- Naughton, P.; McCarthy, S.N.; McCarthy, M.B. The creation of a healthy eating motivation score and its association with food choice and physical activity in a cross sectional sample of Irish adults. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 74. [Google Scholar] [CrossRef] [PubMed]
- O’Hara, B.J.; Phongsavan, P.; Venugopal, K.; Bauman, A.E. Characteristics of participants in Australia’s Get Healthy telephone-based lifestyle information and coaching service: Reaching disadvantaged communities and those most at need. Health Educ. Res. 2011, 26, 1097–1106. [Google Scholar] [CrossRef] [PubMed]
- Polidori, M.C.; Carrillo, J.C.; Verde, P.E.; Sies, H.; Siegrist, J.; Stahl, W. Plasma micronutrient status is improved after a 3-month dietary intervention with 5 daily portions of fruits and vegetables: Implications for optimal antioxidant levels. Nutr. J. 2009, 8, 10. [Google Scholar] [CrossRef] [PubMed]
- Taksler, G.B.; Cutler, D.M.; Giovannucci, E.; Keating, N.L. Vitamin D deficiency in minority populations. Public Health Nutr. 2015, 18, 379–391. [Google Scholar] [CrossRef] [PubMed]
- Ethgen, O.; Hiligsmann, M.; Burlet, N.; Reginster, J.Y. Public health impact and cost-effectiveness of dairy products supplemented with vitamin D in prevention of osteoporotic fractures. Arch. Public Health 2015, 73, 48. [Google Scholar] [CrossRef] [PubMed]
- Fuleihan Gel, H.; Bouillon, R.; Clarke, B.; Chakhtoura, M.; Cooper, C.; McClung, M.; Singh, R.J. Serum 25-Hydroxyvitamin D Levels: Variability, Knowledge Gaps, and the Concept of a Desirable Range. J. Bone Miner. Res. 2015, 30, 1119–1133. [Google Scholar] [CrossRef] [PubMed]
| Nutritional Biomarker | Deficiency Risk Criteria | Proportion Biochemically Deficient 2003–2004 | Proportion Biochemically Deficient 2005–2006 | Proportion Biochemically Deficient 2003–2006 | |||
|---|---|---|---|---|---|---|---|
| % | SE | % | SE | % | SE | ||
| Vitamin A | Serum retinol <20 µg/dL [15] | 0.28 | 0.65 | 0.25 | 0.84 | 0.26 | 0.05 |
| Vitamin B6 | PLP <20 nmol/L [15] | 20 * | 1.4 | 11 * | 0.76 | 16 | 0.87 |
| Vitamin B12 | Serum vitamin B12 <200 pg/mL or MMA >0.271 µmol/L [15] | 7.5 * | 0.70 | 2.6 * | 0.30 | 5.0 | 0.44 |
| Folate | Red blood cell folate <95 ng/mL or serum folate <2 ng/mL [15] | 0.37 | 0.10 | 0.18 | 0.40 | 0.27 | 0.05 |
| Vitamin C | Serum ascorbic acid <0.2 mg/dL [15] | 7.5 | 0.99 | 4.9 | 0.59 | 6.2 | 0.59 |
| Vitamin D | 25-hydroxyvitamin D <12 ng/mL [15] | 7.9 | 1.2 | 9.8 | 1.2 | 8.9 | 0.83 |
| Vitamin E | Alpha-tocopherol <500 µg/dL [15] | 0.75 | 0.15 | 0.66 | 0.09 | 0.70 | 0.08 |
| Anemia | Hemoglobin <13 g/dL (men ≥15 years) or <12 (women ≥15 years, adolescents 12–14 years) or <11 g/dL (pregnant women) or <11.5 g/dL (children >12); and mean cell volume <95 fL [40,41] | 3.9 | 0.41 | 4.6 | 0.37 | 4.3 | 0.28 |
| Characteristic | N | Deficient in 1 * | Deficient in 2 * | Deficient in 3–5 * | Not Deficient | ||||
|---|---|---|---|---|---|---|---|---|---|
| % | SE | % | SE | % | SE | % | SE | ||
| All participants | 13,225 | 23 | 0.78 | 6.3 | 0.49 | 1.7 | 0.18 | 69 | 1.2 |
| Cycle | |||||||||
| 2003–2004 | 6600 | 27 | 0.82 a | 7.2 | 0.64 | 1.9 | 0.29 | 63 | 1.4 a |
| 2005–2006 | 6625 | 19 | 1.1 b | 5.5 | 0.68 | 1.5 | 0.19 | 75 | 1.7 b |
| Sex | |||||||||
| Male | 6506 | 19 a | 1.1 | 4.6 a | 0.39 | 1.1 | 0.20 | 75 a | 1.4 |
| Female | 6719 | 26 b | 0.75 | 8.0 b | 0.64 | 2.3 | 0.29 | 64 b | 1.3 |
| Ethnicity † | |||||||||
| Mexican American | 3195 | 24 a | 1.4 | 5.4 a | 0.61 | 1.2 a | 0.30 | 69 a | 2.1 |
| Non-Hispanic White | 5647 | 20 a | 1.1 | 5.4 a | 0.46 | 1.3 a | 0.19 | 73 a | 1.4 |
| Non-Hispanic Black | 3432 | 36 b | 1.2 | 14 b | 0.81 | 5.1 b | 0.37 | 45 b | 1.7 |
| PIR (%) | |||||||||
| Low PIR, ≤1.85 | 5804 | 27 a | 0.92 | 9.8 a | 0.77 | 2.8 a | 0.27 | 60 a | 1.4 |
| Medium PIR, >1.85 and ≤3.5 | 3224 | 24 a | 0.91 | 6.1 a | 0.80 | 1.8 ab | 0.26 | 68 b | 1.3 |
| High PIR, >3.5 | 3570 | 18 b | 0.93 | 3.8 b | 0.43 | 0.82 b | 0.17 | 77 c | 1.1 |
| Education ‡ | |||||||||
| Less than high school | 2433 | 27 a | 1.1 | 11 a | 0.84 | 2.9 | 0.43 | 59 a | 1.6 |
| High school graduate | 2105 | 26 ab | 1.2 | 8.0 ab | 0.91 | 2.2 | 0.44 | 64 a | 1.5 |
| Some college/college graduate | 4043 | 21 b | 1.0 | 5.0 b | 0.47 | 1.5 | 0.23 | 72 b | 1.3 |
| BMI § | |||||||||
| Underweight | 280 | 23 ab | 2.6 | 10 | 2.4 | 8.4 | 1.7 | 58 ac | 4.1 |
| Normal weight | 2473 | 23 ab | 1.2 | 5.7 | 0.64 | 1.5 ab | 0.25 | 70 ab | 1.6 |
| Overweight | 2949 | 21 a | 0.90 | 5.4 | 0.51 | 0.98 a | 0.19 | 73 b | 1.1 |
| Obese | 2891 | 27 b | 1.3 | 9.4 | 0.88 | 2.8 b | 0.33 | 61 c | 1.8 |
| Pregnancy status | | |||||||||
| Positive | 574 | 33 | 3.2 | 14 | 2.7 | 4.9 | 1.3 | 48 | 4.8 |
| Negative | 4520 | 27 | 0.88 | 7.5 | 0.72 | 2.1 | 0.34 | 63 | 1.3 |
| Breastfeeding status ¶ | |||||||||
| Breastfeeding a child | 100 | 21 | 6.4 ** | 9.2 | 3.3 ** | 3.5 | 3.3 ** | 66 | 8.5 |
| Not breastfeeding | 269 | 35 | 4.7 | 15 | 3.2 | 3.9 | 1.6 ** | 47 | 4.9 |
| Age, Gender and Life Stage Category | N | Deficient in 1 * | Deficient in 2 * | Deficient in 3–5 * | Not deficient | ||||
|---|---|---|---|---|---|---|---|---|---|
| % | SE | % | SE | % | SE | % | SE | ||
| 9–13 years, male & female | 1734 | 15 b | 1.4 | 1.5 ab | 0.36 | 0.06 a**‡ | 0.04 | 83 ab | 1.6 |
| 14–18 years, male | 1242 | 18 b | 1.7 | 2.2 a | 0.65 | 0.13 ab**‡ | 0.08 | 80 a | 1.9 |
| 14–18 years, female | 1107 | 26 ab | 1.9 | 5.3 abc | 0.89 | 0.98 abcd | 0.23 | 68 bcd | 2.2 |
| 19–50 years, male | 2442 | 20 b | 1.3 | 3.9 ab | 0.36 | 0.70 abc | 0.23 | 76 ab | 1.5 |
| 19–50 years, female | 2150 | 30 a | 1.0 | 8.5 cd | 0.89 | 2.5 d | 0.43 | 59 d | 1.6 |
| 51–70 years, male & female | 2347 | 21 b | 1.2 | 7.4 bcd | 0.90 | 2.0 cd | 0.27 | 70 abc | 1.7 |
| 71+ years, male & female | 1540 | 23 b | 1.0 | 9.5 cd | 0.93 | 3.4 d | 0.48 | 64 cd | 1.7 |
| Pregnant or breastfeeding | 683 | 30 ab | 3.3 | 13 d | 2.2 | 4.6 d | 1.5 | 53 d | 4.3 |
| Age, Gender, and Life Stage Category | Serum Retinol <20 µg/dL | PLP <20 nmol/L | Vitamin B12 <200 pg/mL or MMA >0.271 µmol/L | Serum Folate <2 ng/mL or RBC Folate <95 ng/mL | Vitamin C <0.2 mg/dL | Vitamin D <12 ng/mL | Vitamin E <500 µg/dL | Anemia and MCV <95 fL |
|---|---|---|---|---|---|---|---|---|
| 9–13 years, male & female | 0.41 (0.083, 1.2) *‡ | 9.4 (5.8, 12.9) | 1.3 (0.30, 3.5) *‡ | 0.21 (0.011, 1.0) *‡ | 1.1 (0.33, 2.6) *‡ | 4.0 (2.2, 5.8) | 1.4 (0.3, 2.5) | 1.3 (0.5, 2.2) |
| 14–18 years, male | 0.034 (0, 0.53) *‡ | 5.6 (2.7, 8.4) | 2.6 (0.6, 4.5) | 0.20 (0.015, 0.85) *‡ | 3.2 (0.5, 5.8) | 7.1 (3.9, 10.3) | 3.7 (1.0, 6.3) | 0.28 (0.034, 0.97) *‡ |
| 14–18 years, female | 0.062 (0, 0.64) *‡ | 16 (11.2, 21.6) | 2.2 (0.5, 4.0) | 0.33 (0.047, 1.1) *‡ | 3.6 (0.7, 6.5) | 10.6 (5.6, 15.6) | 1.3 (0.1, 2.5) * | 4.5 (2.2, 6.8) |
| 19–50 years, male | 0.20 (0.04, 0.61) *‡ | 8.1 (5.5, 10.6) | 3.0 (1.9, 4.1) | 0.25 (0.062, 0.67) *‡ | 8.7 (5.4, 11.9) | 8.0 (5.2, 10.8) | 0.5 (0.1, 1.0) * | 0.9 (0.4, 1.5) |
| 19–50 years, female | 0.28 (0.04, 0.92) *‡ | 25 (20.3, 29.0) | 3.9 (2.4, 5.4) | 0.35 (0.074, 0.99) *‡ | 6.9 (4.3, 9.5) | 12 (8.3, 15.3) | 0.5 (0.1, 0.8) | 6.6 (4.9, 8.3) |
| 51–70 years, male & female | 0.19 (0.018, 0.75) *‡ | 16 (12.6, 19.7) | 6.9 (3.7, 10.1) | 0.32 (0.076, 0.85) *‡ | 6.6 (4.0, 9.2) | 8.4 (5.3, 11.5) | 0.4 (0.1, 0.6) | 4.0 (2.7, 5.3) |
| 71+ years, male & female | 0.27 (0.025, 1.0) *‡ | 15 (11.4, 18.8) | 15 (10.5, 18.7) | 0.10 (0.0020, 0.57) *‡ | 4.3 (2.3, 6.3) | 9.1 (6.7, 11.5) | 0.28 (0.047, 0.88) *‡ | 8.9 (6.2, 11.6) |
| Pregnant or breastfeeding | 1.7 (0.12, 7.0) *‡ | 35 (25.4, 44.8) | 4.5 (2.6, 6.3) | 0.21 (0, 1.8) *‡ | 0.46 (0.047, 1.7) *‡ | 7.3 (2.0, 12.7) | 2.0 (0.12, 8.5) *‡ | 18 (9.9, 25.3) |
| Not Taking a DS | Taking a DS but Not an FSMV | Taking an FSMV | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % DS Use * | % Deficient † | SE | N | % DS Use * | % Deficient † | SE | N | % DS Use * | % Deficient † | SE | |
| Entire Dataset | 7281 | 44 | 40 a | 1.3 | 4312 | 40 | 28 b | 1.5 | 1615 | 16 | 14 c | 0.9 |
| Age, gender and life stage category | ||||||||||||
| 9–13 years, male & female | 1321 | 68 | 20 | 1.7 | 260 | 20 | 10 | 2.5 | 150 | 12 | 18 | 4.5 |
| 14–18 years, male | 1007 | 75 | 23 | 2.1 | 182 | 20 | 14 | 3.9 | 52 | 4.8 | 12 | 6.0 |
| 14–18 years, female | 861 | 69 | 37 a | 2.8 | 194 | 25 | 25 ab | 3.7 | 50 | 6.2 | 13 b | 6.2 |
| 19–50 years, male | 1469 | 52 | 33 a | 1.8 | 740 | 36 | 17 b | 2.1 | 232 | 12 | 7.9 b | 1.7 |
| 19–50 years, female | 1138 | 43 | 54 a | 2.0 | 828 | 47 | 35 b | 2.0 | 182 | 10 | 19 b | 2.9 |
| 51–70 years, male & female | 869 | 30 | 47 a | 3.1 | 957 | 44 | 29 b | 2.0 | 515 | 26 | 13 c | 1.5 |
| 71+ years, male & female | 459 | 25 | 58 a | 3.5 | 731 | 49 | 34 b | 2.2 | 348 | 26 | 17 c | 2.5 |
| Pregnant or breastfeeding | 157 | 26 | 55 | 7.3 | 420 | 63 | 46 | 4.5 | 86 | 11 | 34 | 7.4 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bird, J.K.; Murphy, R.A.; Ciappio, E.D.; McBurney, M.I. Risk of Deficiency in Multiple Concurrent Micronutrients in Children and Adults in the United States. Nutrients 2017, 9, 655. https://doi.org/10.3390/nu9070655
Bird JK, Murphy RA, Ciappio ED, McBurney MI. Risk of Deficiency in Multiple Concurrent Micronutrients in Children and Adults in the United States. Nutrients. 2017; 9(7):655. https://doi.org/10.3390/nu9070655
Chicago/Turabian StyleBird, Julia K., Rachel A. Murphy, Eric D. Ciappio, and Michael I. McBurney. 2017. "Risk of Deficiency in Multiple Concurrent Micronutrients in Children and Adults in the United States" Nutrients 9, no. 7: 655. https://doi.org/10.3390/nu9070655






