Egg Consumption and Risk of Metabolic Syndrome in Korean Adults: Results from the Health Examinees Study
Abstract
:1. Introduction
2. Subjects and Methods
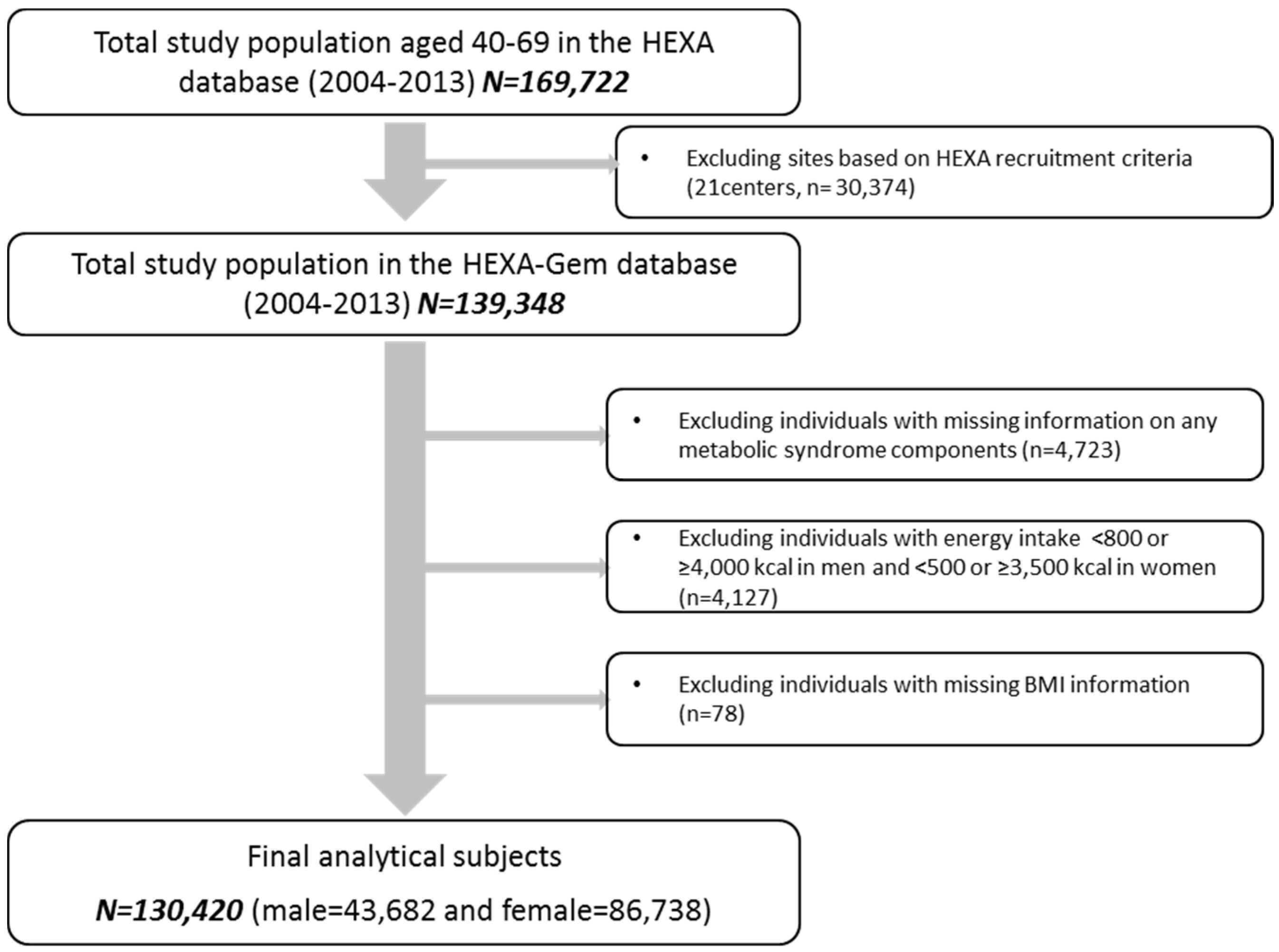
2.1. Study Population
2.2. Assessment of Egg Consumption
2.3. Metabolic Syndrome Diagnosis
2.4. Covariates
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- O’Neill, S.; O’Driscoll, L. Metabolic syndrome: A closer look at the growing epidemic and its associated pathologies. Obes. Rev. 2015, 16, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kaur, J. A comprehensive review on metabolic syndrome. Cardiol. Res. Pract. 2014, 2014, 943162. [Google Scholar] [CrossRef] [PubMed]
- Elder, S.J.; Lichtenstein, A.H.; Pittas, A.G.; Roberts, S.B.; Fuss, P.J.; Greenberg, A.S.; McCrory, M.A.; Bouchard, T.J., Jr.; Saltzman, E.; Neale, M.C. Genetic and environmental influences on factors associated with cardiovascular disease and the metabolic syndrome. J. Lipid Res. 2009, 50, 1917–1926. [Google Scholar] [CrossRef] [PubMed]
- Djousse, L.; Gaziano, J.M.; Buring, J.E.; Lee, I.M. Egg consumption and risk of type 2 diabetes in men and women. Diabetes Care 2009, 32, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.M.; Yuan, B.J.; Zhang, C.L.; Zhou, M.H.; Holmboe-Ottesen, G. Egg consumption and the risk of diabetes in adults, Jiangsu, China. Nutrition 2011, 27, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Andersen, C.J. Bioactive egg components and inflammation. Nutrients 2015, 7, 7889–7913. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, J.K.; Mursu, J.; Tuomainen, T.P.; Virtanen, H.E.K.; Voutilainen, S. Egg consumption and risk of incident type 2 diabetes in men: The Kuopio Ischaemic heart disease risk factor study. Am. J. Clin. Nutr. 2015, 101, 1088–1096. [Google Scholar] [CrossRef] [PubMed]
- Kurotani, K.; Nanri, A.; Goto, A.; Mizoue, T.; Noda, M.; Oba, S.; Sawada, N.; Tsugane, S. Japan Public Health Center-Based Prospective Study Group. Cholesterol and egg intakes and the risk of type 2 diabetes: The Japan public health center-based prospective study. Br. J. Nutr. 2014, 112, 1636–1643. [Google Scholar] [CrossRef] [PubMed]
- Zazpe, I.; Beunza, J.J.; Bes-Rastrollo, M.; Basterra-Gortari, F.J.; Mari-Sanchis, A.; Martinez-Gonzalez, M.A.; Investigators, S.P. Egg consumption and risk of type 2 diabetes in a mediterranean cohort; the sun project. Nutr. Hosp. 2013, 28, 105–111. [Google Scholar] [PubMed]
- Zazpe, I.; Beunza, J.J.; Bes-Rastrollo, M.; Warnberg, J.; de la Fuente-Arrillaga, C.; Benito, S.; Vazquez, Z.; Martinez-Gonzalez, M.A.; Investigators, S.P. Egg consumption and risk of cardiovascular disease in the sun project. Eur. J. Clin. Nutr. 2011, 65, 676–682. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.H.; Zhou, C.H.; Zhou, X.L.; Li, L.H. Egg consumption and risk of cardiovascular diseases and diabetes: A meta-analysis. Atherosclerosis 2013, 229, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.Y.; Xun, P.C.; Nakamura, Y.; He, K. Egg consumption in relation to risk of cardiovascular disease and diabetes: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2013, 98, 146–159. [Google Scholar] [CrossRef] [PubMed]
- Blesso, C.N.; Andersen, C.J.; Barona, J.; Volek, J.S.; Fernandez, M.L. Whole egg consumption improves lipoprotein profiles and insulin sensitivity to a greater extent than yolk-free egg substitute in individuals with metabolic syndrome. Metabolism 2013, 62, 400–410. [Google Scholar] [CrossRef] [PubMed]
- Pearce, K.L.; Clifton, P.M.; Noakes, M. Egg consumption as part of an energy-restricted high-protein diet improves blood lipid and blood glucose profiles in individuals with type 2 diabetes. Br. J. Nutr. 2011, 105, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Health Examinees Study Group. The Health Examinees (HEXA) study: Rationale, study design and baseline characteristics. Asian Pac. J. Cancer Prev. 2015, 16, 1591–1597. [Google Scholar]
- Kim, Y.; Han, B.G.; The KoGES Group. Cohort profile: The Korean genome and epidemiology study (KoGES) consortium. Int. J. Epidemiol. 2016, 46, e20. [Google Scholar] [CrossRef] [PubMed]
- National Rural Nutrition Institute. National Rural Nutrition Institute Food Composition Tables, 2012. Korean Standard Food Composition Table. Available online: http://koreanfood.rda.go.kr/eng/fctFoodSrchEng/engMain (accessed on 14 April 2017).
- Ahn, Y.; Kwon, E.; Shim, J.E.; Park, M.K.; Joo, Y.; Kimm, K.; Park, C.; Kim, D.H. Validation and reproducibility of food frequency questionnaire for Korean genome epidemiologic study. Eur. J. Clin. Nutr. 2007, 61, 1435–1441. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Becker, D.; Clark, L.T.; Cooper, R.S.; Denke, M.A.; Howard, W.J.; Hunninghake, D.B.; Illingworth, R.; Luepker, R.V.; McBride, P.; et al. Third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) final report. Circulation 2002, 106, 3143–3421. [Google Scholar]
- Djousse, L.; Petrone, A.B.; Hickson, D.A.; Talegawkar, S.A.; Dubbert, P.M.; Taylor, H.; Tucker, K.L. Egg consumption and risk of type 2 diabetes among African Americans: The Jackson heart study. Clin. Nutr. 2016, 35, 679–684. [Google Scholar] [CrossRef] [PubMed]
- Diez-Espino, J.; Basterra-Gortari, F.J.; Salas-Salvado, J.; Buil-Cosiales, P.; Corella, D.; Schroder, H.; Estruch, R.; Ros, E.; Gomez-Gracia, E.; Aros, F.; et al. Egg consumption and cardiovascular disease according to diabetic status: The predimed study. Clin. Nutr. 2016, 36, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Tamez, M.; Virtanen, J.K.; Lajous, M. Egg consumption and risk of incident type 2 diabetes: A dose-response meta-analysis of prospective cohort studies. Br. J. Nutr. 2016, 115, 2212–2218. [Google Scholar] [CrossRef] [PubMed]
- Woo, H.W.; Choi, B.Y.; Kim, M.K. Cross-sectional and longitudinal associations between egg consumption and metabolic syndrome in adults ≥40 years old: The Yangpyeong cohort of the Korean genome and epidemiology study (KoGES_Yangpyeong). PLoS ONE 2016, 11, e0147729. [Google Scholar] [CrossRef] [PubMed]
- Blesso, C.N.; Andersen, C.J.; Bolling, B.W.; Fernandez, M.L. Egg intake improves carotenoid status by increasing plasma HDL cholesterol in adults with metabolic syndrome. Food Funct. 2013, 4, 213–221. [Google Scholar] [CrossRef] [PubMed]
- McNamara, D.J. The impact of egg limitations on coronary heart disease risk: Do the numbers add up? J. Am. Coll. Nutr. 2000, 19, 540s–548s. [Google Scholar] [CrossRef] [PubMed]
- Miettinen, T.A.; Gylling, H. Cholesterol absorption efficiency and sterol metabolism in obesity. Atherosclerosis 2000, 153, 241–248. [Google Scholar] [CrossRef]
- Naviglio, D.; Gallo, M.; Le Grottaglie, L.; Scala, C.; Ferrara, L.; Santini, A. Determination of cholesterol in Italian chicken eggs. Food Chem. 2012, 132, 701–708. [Google Scholar] [CrossRef]
- Lichtenstein, A.H.; Schwab, U.S. Relationship of dietary fat to glucose metabolism. Atherosclerosis 2000, 150, 227–243. [Google Scholar] [CrossRef]
- Blesso, C.N. Egg phospholipids and cardiovascular health. Nutrients 2015, 7, 2731–2747. [Google Scholar] [CrossRef] [PubMed]
- Mutungi, G.; Ratliff, J.; Puglisi, M.; Torres-Gonzalez, M.; Vaishnav, U.; Leite, J.O.; Quann, E.; Volek, J.S.; Fernandez, M.L. Dietary cholesterol from eggs increases plasma HDL cholesterol in overweight men consuming a carbohydrate-restricted diet. J. Nutr. 2008, 138, 272–276. [Google Scholar] [PubMed]
- Flood, A.; Rastogi, T.; Wirfalt, E.; Mitrou, P.N.; Reedy, J.; Subar, A.F.; Kipnis, V.; Mouw, T.; Hollenbeck, A.R.; Leitzmann, M.; et al. Dietary patterns as identified by factor analysis and colorectal cancer among middle-aged Americans. Am. J. Clin. Nutr. 2008, 88, 176–184. [Google Scholar] [PubMed]
- Kautzky-Willer, A.; Harreiter, J.; Pacini, G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr. Rev. 2016, 37, 278–316. [Google Scholar] [CrossRef] [PubMed]
- Cade, J.; Thompson, R.; Burley, V.; Warm, D. Development, validation and utilisation of food-frequency questionnaires—A review. Public Health Nutr. 2002, 5, 567–587. [Google Scholar] [CrossRef] [PubMed]
| Egg Consumption (Egg/Week) | p-Value * | |||||
|---|---|---|---|---|---|---|
| <1 | 1 | 2–4 | 5–6 | ≥7 | ||
| Men (n = 43,682) | 19,939 | 13,798 | 6476 | 1334 | 2135 | |
| Age (years) † | 54.5 ± 8.1 | 53.0 ± 8.4 | 52.1 ± 8.5 | 51.9 ± 8.4 | 54.0 ± 8.8 | <0.0001 |
| BMI (kg/m2) | 24.4 ± 2.7 | 24.4 ± 2.8 | 24.5 ± 2.8 | 24.6 ± 2.8 | 24.4 ± 2.9 | 0.0290 |
| College or above, n (%) | 6469 (32.9) | 5287 (38.8) | 2671 (41.7) | 596 (45.1) | 964 (45.7) | <0.0001 |
| Current smokers, n (%) | 5783 (29.1) | 4498 (32.7) | 2277 (35.3) | 478 (35.9) | 672 (31.6) | <0.0001 |
| Current drinkers, n (%) | 14,143 (71.1) | 10,192 (74.0) | 4876 (75.4) | 1008 (75.8) | 1538 (72.4) | <0.0001 |
| Regular exercisers, n (%) | 11,296 (43.2) | 7774 (43.6) | 3761 (41.8) | 758 (43.1) | 1322 (37.9) | <0.0001 |
| Dietary Intake ‡ | ||||||
| Energy (kcal) | 1717.8 ± 435.6 | 1879.1 ± 445.6 | 2010.4 ± 479.2 | 2110.2 ± 515.4 | 2101.0 ± 506.8 | <0.0001 |
| Carbohydrate (g) ‡ | 312.1 ± 75.0 | 330 ± 76.8 | 342.5 ± 81.0 | 352.5 ± 86.5 | 346.6 ± 84.6 | <0.0001 |
| Protein (g) ‡ | 55.4 ± 20.1 | 63.9 ± 20.1 | 71.7 ± 22.2 | 77.2 ± 24.1 | 79.1 ± 25.3 | <0.0001 |
| Fat (g) ‡ | 24.9 ± 13.8 | 31.5 ± 14.1 | 37.1 ± 16.0 | 41.3 ± 17.3 | 42.4 ± 17.8 | <0.0001 |
| % Energy from carbohydrate | 74.2 ± 6.9 | 71.4 ± 6.3 | 69.2 ± 6.6 | 67.8 ± 6.7 | 66.8 ± 7.0 | <0.0001 |
| % Energy from protein | 12.9 ± 2.4 | 13.7 ± 2.2 | 14.3 ± 2.3 | 14.7 ± 2.3 | 15.1 ± 2.5 | <0.0001 |
| % Energy from fat | 12.8 ± 5.0 | 15.0 ± 4.6 | 16.5 ± 4.8 | 17.5 ± 4.9 | 18.0 ± 5.0 | <0.0001 |
| Cholesterol (mg) ‡ | 108.5 ± 71.0 | 171.5 ± 70.1 | 250.3 ± 80.4 | 331.6 ± 84.1 | 420.9 ± 138.1 | <0.0001 |
| Fruit (g) | 128.4 + 107.5 | 131.3 + 85.1 | 139.5 + 91.1 | 135.3 + 87.0 | 144.7 + 105.4 | <0.0001 |
| Vegetables (g) | 142.7 + 147.6 | 148.0 + 126.1 | 146.8 + 128.4 | 145.0 + 123.5 | 158.7 + 136.6 | <0.0001 |
| Meat (g) | 38.4 + 33.1 | 43.3 + 31.5 | 45.1 + 33.6 | 45.7 + 33.9 | 42.0 + 34.6 | <0.0001 |
| Women (n = 86,738) | 41,639 | 25,771 | 12,409 | 2592 | 4327 | |
| Age (years) | 53.5 ± 7.6 | 51.6 ± 7.7 | 50.6 ± 7.8 | 50.3 ± 7.8 | 51.5 ± 7.8 | <0.0001 |
| BMI (kg/m2) | 23.8 ± 2.9 | 23.5 ± 2.9 | 23.4 ± 3.0 | 23.5 ± 3.1 | 23.3 ± 3.0 | <0.0001 |
| College or above, n (%) | 5922 (14.2) | 5704 (22.1) | 3246 (26.2) | 707 (27.3) | 1261 (29.1) | <0.0001 |
| Current smokers, n (%) | 896 (2.2) | 518 (2) | 285 (2.3) | 79 (3.0) | 93 (2.1) | 0.0113 |
| Current drinkers, n (%) | 11,752 (28.2) | 8383 (32.5) | 4066 (32.8) | 908 (35.0) | 1328 (30.7) | <0.0001 |
| Regular exercisers, n (%) | 20,873 (50.1) | 13,121 (50.9) | 6520 (52.5) | 1329 (51.3) | 2432 (56.2) | <0.0001 |
| Dietary Intake | ||||||
| Energy (kcal) | 1560.1 ± 457.3 | 1720.6 ± 462.2 | 1859.2 ± 497.9 | 1946.3 ± 531.5 | 1993.2 ± 541.8 | <0.0001 |
| Carbohydrate (g) ‡ | 287.5 ± 82.6 | 306.1 ± 82.5 | 320.9 ± 86.9 | 328.3 ± 90.8 | 331.5 ± 91.9 | <0.0001 |
| Protein (g) ‡ | 50.6 ± 20.0 | 58.7 ± 19.7 | 66.5 ± 21.8 | 71.8 ± 23.8 | 76.0 ± 25.8 | <0.0001 |
| Fat (g) ‡ | 21.3 ± 12.9 | 27.5 ± 13.3 | 33.1 ± 15.0 | 37.1 ± 16.3 | 39.6 ± 17.1 | <0.0001 |
| % Energy from carbohydrate | 74.9 ± 7.2 | 71.9 ± 6.6 | 69.7 ± 6.7 | 68.0 ± 6.7 | 67.0 ± 6.9 | <0.0001 |
| % Energy from protein | 13.0 ± 2.6 | 13.7 ± 2.3 | 14.4 ± 2.4 | 14.8 ± 2.4 | 15.3 ± 2.6 | <0.0001 |
| % Energy from fat | 12.1 ± 5.1 | 14.3 ± 4.8 | 15.9 ± 4.9 | 17.1 ± 4.9 | 17.8 ± 4.9 | <0.0001 |
| Cholesterol (mg) ‡ | 101.5 ± 72.0 | 163.9 ± 68.8 | 244.2 ± 78.5 | 325.2 ± 84.0 | 415.7 ± 143.4 | <0.0001 |
| Fruit (g) | 151.9 + 121.3 | 152.7 + 102.8 | 161.5 + 105.6 | 165.1 + 108.9 | 177.1 + 123.4 | <0.0001 |
| Vegetables (g) | 203.9 + 191.4 | 208.0 + 167 | 207.4 + 162.7 | 200.4 + 162.0 | 221.3 + 173.0 | <0.0001 |
| Meat (g) | 28.3 + 29.1 | 33.9 + 28.4 | 35.5 + 29.4 | 36.0 + 29.1 | 31.5 + 27.3 | <0.0001 |
| Egg Consumption (Egg/Week) | p-Trend † | |||||
|---|---|---|---|---|---|---|
| <1 | 1 | 2–4 | 5–6 | ≥7 | ||
| Men (n = 43,682) | 19,939 | 13,798 | 6476 | 1334 | 2135 | |
| MetS ‡ | 5825 (29.2) § | 3981 (28.9) | 1912 (29.5) | 388 (29.1) | 595 (27.9) | |
| Ref. (Reference) | 0.97 (0.92–1.02) | 1.00 (0.93–1.07) | 0.96 (0.84–1.10) | 0.94 (0.84–1.05) | 0.3806 | |
| WC ≥90 cm | 5698 (28.6) | 4068 (29.5) | 2010 (31.0) | 377 (28.3) | 615 (28.8) | |
| Ref. | 0.98 (0.93–1.03) | 1.04 (0.97–1.11) | 0.89 (0.79–1.01) | 0.90 (0.82–1.00) | 0.1327 | |
| Serum TG ≥150 mg/dL | 7708 (38.7) | 5446 (39.5) | 2646 (40.9) | 540 (40.5) | 807 (37.8) | |
| Ref. | 0.98 (0.94–1.03) | 1.01 (0.95–1.08) | 0.97 (0.86–1.10) | 0.94 (0.85–1.04) | 0.4771 | |
| Serum HDL-C ≤40 mg/dL | 4783 (24.0) | 3135 (22.7) | 1413 (21.8) | 274 (20.5) | 464 (21.7) | |
| Ref. | 0.94 (0.89–1.00) | 0.90 (0.84–0.97) | 0.82 (0.72–0.95) | 0.89 (0.80–1.00) | 0.0004 | |
| BP ≥130/85 mmHg | 10,656 (53.4) | 7171 (52.0) | 3377 (52.2) | 665 (49.9) | 1118 (52.4) | |
| Ref. | 0.98 (0.93–1.02) | 1.00 (0.94–1.06) | 0.91 (0.81–1.02) | 0.98 (0.89–1.07) | 0.2943 | |
| Fasting glucose ≥100 mg/dL | 7088 (35.6) | 4679 (33.9) | 2211 (34.1) | 449 (33.7) | 722 (33.8) | |
| Ref. | 0.97 (0.92–1.02) | 1.00 (0.94–1.07) | 0.97 (0.86–1.10) | 0.99 (0.90–1.10) | 0.7800 | |
| Women (n = 86,738) | 41,639 | 25,771 | 12,409 | 2592 | 4327 | |
| MetS | 11,683 (28.1) | 5836 (22.6) | 2495 (20.1) | 504 (19.4) | 820 (19.0) | |
| Ref. | 0.90 (0.86–0.94) | 0.83 (0.78–0.87) | 0.80 (0.71–0.89) | 0.77 (0.70–0.84) | <0.0001 | |
| WC ≥80 cm | 18,627 (44.7) | 10,137 (39.3) | 4720 (38.0) | 988 (38.1) | 1533 (35.4) | |
| Ref. | 0.91 (0.87–0.94) | 0.91 (0.87–0.95) | 0.93 (0.85–1.01) | 0.80 (0.75–0.86) | <0.0001 | |
| Serum TG ≥150 mg/dL | 10,589 (25.4) | 5540 (21.5) | 2425 (19.5) | 519 (20.0) | 822 (19.0) | |
| Ref. | 0.90 (0.86–0.93) | 0.83 (0.79–0.88) | 0.86 (0.77–0.95) | 0.78 (0.72–0.85) | <0.0001 | |
| Serum HDL-C ≤50 mg/dL | 16,020 (38.5) | 8895 (34.5) | 3981 (32.1) | 788 (30.4) | 1332 (30.8) | |
| Ref. | 0.94 (0.91–0.97) | 0.87 (0.83–0.91) | 0.82 (0.75–0.89) | 0.82 (0.77–0.88) | <0.0001 | |
| BP ≥130/85 mmHg | 16,806 (40.4) | 9197 (35.7) | 4132 (33.3) | 785 (30.3) | 1368 (31.6) | |
| Ref. | 0.98 (0.94–1.01) | 0.95 (0.91–0.99) | 0.83 (0.76–0.91) | 0.86 (0.80–0.92) | <0.0001 | |
| Fasting glucose ≥100 mg/dL | 8868 (21.3) | 4819 (18.7) | 2121 (17.1) | 425 (16.4) | 739 (17.1) | |
| Ref. | 0.98 (0.94–1.02) | 0.94 (0.89–0.99) | 0.90 (0.81–1.01) | 0.94 (0.83–0.99) | 0.0015 | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, S.; Lee, H.-W.; Kim, C.E.; Lim, J.; Lee, J.-k.; Lee, S.-A.; Kang, D. Egg Consumption and Risk of Metabolic Syndrome in Korean Adults: Results from the Health Examinees Study. Nutrients 2017, 9, 687. https://doi.org/10.3390/nu9070687
Shin S, Lee H-W, Kim CE, Lim J, Lee J-k, Lee S-A, Kang D. Egg Consumption and Risk of Metabolic Syndrome in Korean Adults: Results from the Health Examinees Study. Nutrients. 2017; 9(7):687. https://doi.org/10.3390/nu9070687
Chicago/Turabian StyleShin, Sangah, Hwi-Won Lee, Claire E. Kim, Jiyeon Lim, Jong-koo Lee, Sang-Ah Lee, and Daehee Kang. 2017. "Egg Consumption and Risk of Metabolic Syndrome in Korean Adults: Results from the Health Examinees Study" Nutrients 9, no. 7: 687. https://doi.org/10.3390/nu9070687






