Comparison of Dietary Intakes of 7-Year-Old Children Enrolled in Observational Birth Cohort Studies on the Isle of Man and in South-West England
Abstract
:1. Introduction
2. Methods
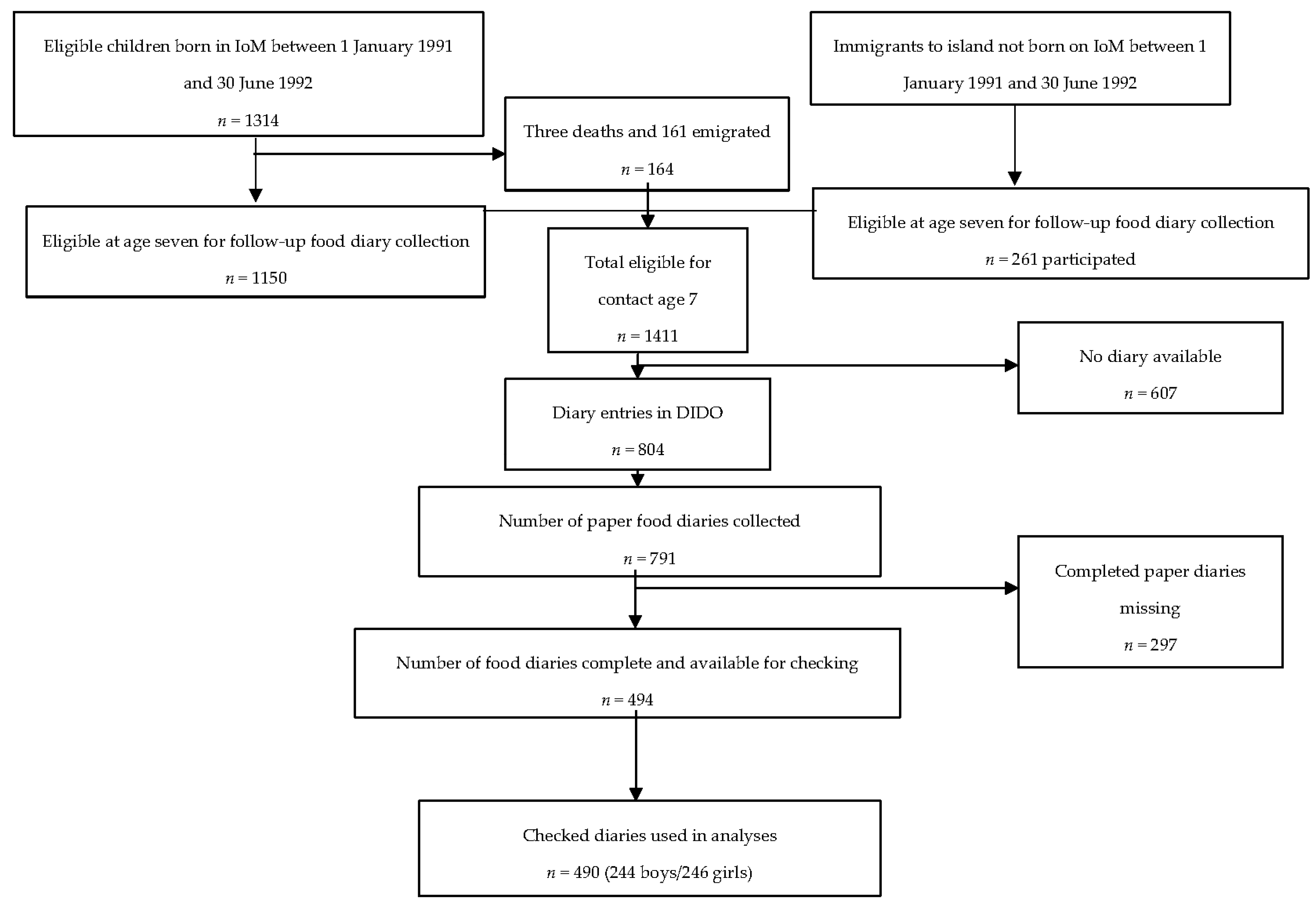
2.1. Birth Cohort Studies: Isle of Man and ALSPAC
2.2. Demographic Data Collection
2.3. Dietary Data Collection: IoM and ALSPAC
2.4. Data Processing: IoM and ALSPAC
2.5. Statistical Analyses
3. Results
4. Discussion
4.1 Strengths and Limitations
5. Conclusions
Supplementary Materials
Acknowledgments
Ethics Approval
Financial Support
Author Contributions
Conflicts of Interest
References
- Gregory, J.; Lowe, S. National Diet and Nutrition Survey: Young People Aged 4 to 18 Years; TSO: London, UK, 2000. [Google Scholar]
- Irish Universities Nutrition Alliance. National Children’s Food Survey. Available online: http://www.iuna.net/?p=27 (accessed on 1 September 2016).
- Economic Affairs Division; Isle of Man Government Treasury. Isle of Man Census Report 2001 Volume 1. Available online: https://www.gov.im/media/207870/2001censusreportvolume1.pdf (accessed on 7 July 2017).
- Economic Affairs; Cabinet Office. Isle of Man Earnings Survey 2015. Available online: https://www.gov.im/media/1350687/2016-01-29-earnings-survey-2015.pdf (accessed on 1 September 2016).
- Economic Affairs. Fuel Poverty in the Isle of Man. Available online: https://www.gov.im/media/1350750/2016-03-10-study-into-fuel-poverty-on-the-isle-of-man-with-minsiters-foreward.pdf (accessed on 1 September 2016).
- Goodfellow, S.A.; Northstone, K. Childhood overweight and obesity in the UK—A comparison of two environmentally distinct populations of 7-year-old children. Int. J. Pediatr. Obes. 2008, 3, 117–119. [Google Scholar] [CrossRef] [PubMed]
- Glynn, L.; Emmett, P.; Rogers, I. Food and nutrient intakes of a population sample of 7-year-old children in the south-west of England in 1999/2000—What difference does gender make? J. Hum. Nutr. Diet. 2005, 18, 7–19. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Report on Health and Social Subjects 41. In Dietary Reference Values for Food Energy and Nutrients for the United Kingdom; TSO: London, UK, 1991. [Google Scholar]
- Scientific Advisory Committee on Nutrition. Dietary Reference Values for Energy; TSO: London, UK, 2011.
- Goodfellow, S.A.; Rolfe, E.M.; Golding, J. Cohort profile: The Isle of Man birth cohort study. Int. J. Epidemiol. 2012, 42, 1246–1252. [Google Scholar] [CrossRef] [PubMed]
- ELSPAC in the Isle of Man (2017). Available online: http://www.bristol.ac.uk/social-community-medicine/projects/isleofmanstudy/ (accessed on 7 July 2017).
- Boyd, A.; Golding, J.; Macleod, J.; Lawlor, D.A.; Fraser, A.; Henderson, J.; Molloy, L.; Ness, A.; Ring, S.; Davey Smith, G. Cohort profile: The ‘Children of the 90s’—The index offspring of the Avon Longitudinal Study of Parents and Children. Int. J. Epidemiol. 2013, 42, 111–127. [Google Scholar] [CrossRef] [PubMed]
- Avon Longitudinal Study of Parents and Children. Accessing the Resource (2017). Available online: http://www.bristol.ac.uk/alspac/researchers/access/ (accessed on 7 July 2017).
- Avon Longitudinal Study of Parents and Children. Questionnaires (2017). Available online: http://www.bristol.ac.uk/alspac/researchers/our-data/questionnaires/ (accessed on 7 July 2017).
- Price, G.M.; Paul, A.A.; Key, F.B.; Harter, A.C.; Cole, T.J.; Day, K.C.; Wadsworth, M.E.J. Measurement of diet in a large national survey: Comparison of computerized and manual coding of records in household measures. J. Hum. Nutr. Diet. 1995, 8, 417–428. [Google Scholar] [CrossRef]
- Holland, B.; McCance, R.A.; Widdowson, E.M. McCance and Widdowson’s the Composition of Foods; Holland, B., Ed.; Royal Society of Chemistry: Cambridge, UK, 1991. [Google Scholar]
- Emmett, P.; Rogers, I.; Symes, C.; Team, A.S. Food and nutrient intakes of a population sample of 3-year-old children in the south west of England in 1996. Public Health Nutr. 2002, 5, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Torun, B. Energy requirements of children and adolescents. Public Health Nutr. 2005, 8, 968–993. [Google Scholar] [CrossRef] [PubMed]
- Black, A.E.; Cole, T.J. Within- and between-subject variation in energy expenditure measured by the doubly-labelled water technique: Implications for validating reported dietary energy intake. Eur. J. Clin. Nutr. 2000, 54, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Rennie, K.L.; Coward, A.; Jebb, S.A. Estimating under-reporting of energy intake in dietary surveys using an individualised method. Br. J. Nutr. 2007, 97, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- Scientific Advisory Committee on Nutrition. Carbohydrates and Health; TSO: Norwich, UK, 2015.
- Sandvik, C.; De Bourdeaudhuij, I.; Due, P.; Brug, J.; Wind, M.; Bere, E.; Perez-Rodrigo, C.; Wolf, A.; Elmadfa, I.; Thorsdottir, I.; et al. Personal, social and environmental factors regarding fruit and vegetable intake among schoolchildren in nine European countries. Ann. Nutr. Metab. 2005, 49, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Bjelland, M.; Brantsaeter, A.L.; Haugen, M.; Meltzer, H.M.; Nystad, W.; Andersen, L.F. Changes and tracking of fruit, vegetables and sugar-sweetened beverages intake from 18 months to 7 years in the Norwegian Mother and Child cohort study. BMC Public Health 2013, 13, 793. [Google Scholar] [CrossRef] [PubMed]
- Lorson, B.A.; Melgar-Quinonez, H.R.; Taylor, C.A. Correlates of fruit and vegetable intakes in US children. J. Am. Diet. Assoc. 2009, 109, 474–478. [Google Scholar] [CrossRef] [PubMed]
- Poppitt, S.D. Beverage consumption: Are alcoholic and sugary drinks tipping the balance towards overweight and obesity? Nutrients 2015, 7, 6700–6718. [Google Scholar] [CrossRef] [PubMed]
- Rugg-Gunn, A.J.; Fletcher, E.S.; Matthews, J.N.; Hackett, A.F.; Moynihan, P.J.; Kelly, S.; Adams, J.; Mathers, J.C.; Adamson, A. Changes in consumption of sugars by English adolescents over 20 years. Public Health Nutr. 2007, 10, 354–363. [Google Scholar] [CrossRef] [PubMed]
- Jones, L.R.; Steer, C.D.; Rogers, I.S.; Emmett, P.M. Influences on child fruit and vegetable intake: Sociodemographic, parental and child factors in a longitudinal cohort study. Public Health Nutr. 2010, 13, 1122–1130. [Google Scholar] [CrossRef] [PubMed]
- Prynne, C.J.; Paul, A.A.; Price, G.M.; Day, K.C.; Hilder, W.S.; Wadsworth, M.E. Food and nutrient intake of a national sample of 4-year-old children in 1950: Comparison with the 1990s. Public Health Nutr. 1999, 2, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Bingham, S.A.; Gill, C.; Welch, A.; Day, K.; Cassidy, A.; Khaw, K.T.; Sneyd, M.J.; Key, T.J.; Roe, L.; Day, N.E. Comparison of dietary assessment methods in nutritional epidemiology: Weighed records v. 24 h recalls, food-frequency questionnaires and estimated-diet records. Br. J. Nutr. 1994, 72, 619–643. [Google Scholar] [CrossRef] [PubMed]
- Burrows, T.L.; Martin, R.J.; Collins, C.E. A systematic review of the validity of dietary assessment methods in children when compared with the method of doubly labeled water. J. Am. Diet. Assoc. 2010, 110, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- Emmett, P.M.; Jones, L.R. Diet, growth, and obesity development throughout childhood in the Avon Longitudinal Study of Parents and Children. Nutr. Rev. 2015, 73, 175–206. [Google Scholar] [CrossRef] [PubMed]
- Ambrosini, G.L.; Johns, D.J.; Northstone, K.; Emmett, P.M.; Jebb, S.A. Free sugars and total fat are important characteristics of a dietary pattern associated with adiposity across childhood and adolescence. J. Nutr. 2016, 146, 778–784. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | IoM a | ALSPAC | P for IoM Included vs. ALSPAC Included | ||
|---|---|---|---|---|---|
| With a Checked Food Record (n = 490) | Without a Checked Food Record (n = 921) | P value for IoM Included vs. IoM Excluded | With a Checked Food Record (n = 7087) | ||
| Sex, n (%) | |||||
| Male | 244 (49.8%) | 466 (52.5%) | 0.340 | 3593 (50.7%) | 0.699 |
| Female | 246 (50.2%) | 422 (47.5%) | 3494 (49.3%) | ||
| Birth weight (g) | 3453 ± 525 (n = 421) | 3410 ± 559 (n = 886) | 0.179 | 3445.6 ± 533.7 (n = 6633) | 0.438 |
| Gestation length (weeks) | 39.8 ± 1.7 (n = 421) | 39.9 ± 1.7 (n = 886) | 0.386 | 39.5 ± 1.8 (n = 6710) | <0.001 |
| Maternal characteristics | |||||
| Parity | 0.228 | ||||
| 0 | 188 (50.4%) | 288 (46.5%) | 2985 (46.4%) | 0.131 | |
| ≥1 | 185 (49.6%) | 332 (53.5%) | 3450 (53.6%) | ||
| Marital status | |||||
| Never married | 58 (15.2%) | 166 (26.1%) | <0.001 | 848 (12.9%) | 0.317 |
| Widowed/Divorced/Separated | 20 (5.2%) | 41 (6.4%) | 295 (4.0%) | ||
| Married | 304 (79.6%) | 430 (67.5%) | 5432 (8.3%) | ||
| Age (years) | |||||
| <20 | 20 (5.2%) | 53 (8.2%) | 0.007 | 487 (6.9%) | 0.013 |
| 20–24 | 71 (18.4%) | 170 (26.4%) | 893 (12.6%) | ||
| 25–29 | 145 (37.6%) | 213 (33%) | 2648 (37.4%) | ||
| 30–34 | 108 (28.0%) | 148 (22.9%) | 2218 (31.3%) | ||
| ≥35 | 42 (10.9%) | 61 (9.5%) | 841 (11.9%) | ||
| BMI (kg/m2) | 23.1 ± 3.7 (n = 367) | 23.0 ± 3.77 (n = 611) | 0.792 | 22.9 ± 3.7 (n = 6094) | 0.364 |
| Ethnicity b | |||||
| White | 373 (96.9%) | 625 (97.2%) | 0.770 | 6371 (98.3%) | 0.035 |
| Other | 12 (3.1%) | 18 (2.8%) | 108 (1.7%) | ||
| IoM | ALSPAC | |||
|---|---|---|---|---|
| Boys | Girls | Boys | Girls | |
| n | 244 | 246 | 3593 | 3494 |
| Energy (MJ) | 7.70 (7.53, 7.88) * | 7.26 (7.09, 7.43)††† | 7.44 (7.39, 7.48) | 6.88 (6.84, 6.92) |
| % from protein | 14.0 (13.7, 14.3) *** | 13.6 (13.3, 13.9) † | 13.3 (13.2, 13.4) | 13.3 (13.2, 13.4) |
| % from fat | 33.9 (33.3, 34.4) | 34.3 (33.8, 34.9) | 35.3 (35.2, 35.5) *** | 35.6 (35.5, 35.7) ††† |
| % from saturated fat | 14.1 (13.7, 14.4) | 14.0 (13.6, 14.3) | 14.2 (14.1, 14.3) | 14.3 (14.2, 14.3) |
| % from carbohydrate | 55.0 (54.3, 55.6) *** | 54.9 (54.3, 55.6)††† | 51.4 (51.3, 51.6) | 51.2 (51.0, 51.3) |
| % from free sugars | 18.2 (17.4, 19.0) | 19.0 (18.4, 19.8)††† | 17.5 (17.3, 17.7) | 17.4 (17.2, 17.6) |
| Protein (g) | 64 (62, 66) *** | 59 (57, 58) ††† | 58 (57, 58) | 53 (53, 54) |
| Fat (g) | 70 (67, 72) | 66 (64, 69) | 71 (71, 72) | 66 (66, 67) |
| Carbohydrate (g) | 253 (246, 259) *** | 238 (232, 244) ††† | 239 (237, 240) | 220 (218, 221) |
| Free sugars (g) | 84 (80, 88) | 83 (79, 87) ††† | 82 (81, 83) | 75 (74, 76) |
| Fibre (g NSP) | 11.1 (10.6, 11.5) | 10.2 (9.8, 10.5) | 10.8 (10.7, 10.9) | 10.0 (9.9, 10.1) |
| Retinol equivalents (µg) | 615 (578, 652) | 603 (570, 636) | 687 (673, 700) ** | 670 (651, 689) |
| Thiamin (mg) | 1.5 (1.4, 1.5) | 1.3 (1.2, 1.4) | 1.5 (1.5, 1.66) | 1.4 (1.35, 1.41) |
| Riboflavin (mg) | 1.8 (1.7, 1.8) | 1.5 (1.4, 1.5) | 1.7 (1.73, 1.77) | 1.5 (1.53, 1.57) |
| Niacin equivalents (mg) | 31 (30, 32) *** | 28 (27, 29) ††† | 27 (27.2, 27.6) | 25 (24.9, 25.3) |
| Vitamin B6 (mg) | 2.0 (2.0, 2.1) *** | 1.9 (1.8, 1.9) ††† | 1.8 (1.81, 1.86) | 1.7 (1.67, 1.70) |
| Vitamin B12 (µg) | 4.1 (3.8, 4.3) | 3.7 (3.5, 3.9) | 3.9 (3.82, 3.94) | 3.6 (3.50, 3.64) |
| Folate (µg) | 209 (201, 218) | 190 (184, 197) | 205 (203, 207) | 190 (188, 192) |
| Vitamin C (mg) | 92.0 (83.1, 100.3) ** | 98.0 (90.3, 105.7) ††† | 80.6 (78.7, 82.5) | 80.0 (78.2, 81.9) |
| Vitamin D (µg) | 2.4 (2.2, 2.6) | 2.3 (2.2, 2.4) | 2.5 (2.4, 2.5) | 2.3 (2.26, 2.33) |
| Calcium (mg) | 891(855, 927) *** | 787 (757, 818) † | 824 (814, 833) | 751 (742, 760) |
| Iron (mg) | 9.3 (9.0, 9.6) *** | 8.3 (8.1, 8.6) †† | 8.7 (8.7, 8.8) | 7.9 (7.9, 8.0) |
| Zinc (mg) | 7.1 (6.9, 7.4) *** | 6.2 (6.0, 6.4) ††† | 6.4 (6.3, 6.4) | 5.8 (5.7, 5.8) |
| Selenium (µg) | 64 (62, 67) *** | 60 (57, 62) ††† | 55 (54, 55) | 50 (49, 50) |
| Iodine (µg) | 158 (149, 168) | 136 (129, 142) | 156 (153, 158) | 139 (137, 141) |
| UK Reference Intake Age 7–10 Years a | % Children Below RNI | % Children Below LRNI | ||||
|---|---|---|---|---|---|---|
| RNI | LRNI | IoM | ALSPAC | IoM | ALSPAC | |
| Energy (kJ) | ||||||
| Boys | 6900 b | - | 28.3 | 35.7 | - | - |
| Girls | 6400 b | - | 23.2 | 36.7 | - | - |
| Fibre (g NSP) | 15.3 c | - | 92.5 | 92.3 | - | - |
| Retinol equivalents (µg) | 500 | 250 | 38.1 | 34.9 | 4.5 | 4.4 |
| Thiamin (mg/4.2 MJ) | 0.4 | 0.2 | 0.4 | 0.8 | 0.0 | 0.1 |
| Riboflavin (mg) | 1.0 | 0.5 | 8.9 | 11.9 | 0.2 | 0.6 |
| Niacin equivalents (mg/4.2 MJ) | 6.6 | 4.4 | 8.1 | 16.9 | 0.2 | 1.5 |
| Vitamin B6 (µg/g protein) | 15 | 11 | 0.0 | 0.5 | 0.0 | 0.1 |
| Vitamin B12 (µg) | 1.0 | 0.6 | 0.6 | 1.7 | 0.0 | 0.5 |
| Folate (mg) | 150 | 75 | 21.1 | 23.7 | 0.4 | 0.7 |
| Vitamin C (mg) | 30 | 8 | 11.1 | 16.2 | 0.0 | 0.5 |
| Calcium (mg) | 550 | 325 | 11.5 | 19.5 | 0.8 | 1.6 |
| Iron (mg) | 8.7 | 4.7 | 52.0 | 62.1 | 1.0 | 2.0 |
| Zinc (mg) | 7 | 4 | 63.0 | 74.4 | 4.3 | 8.3 |
| Selenium (mg) | 30 | 16 | 2.6 | 6.9 | 0.4 | 0.4 |
| Iodine (mg) | 110 | 55 | 30.0 | 34.1 | 1.8 | 2.9 |
| Food Groups | Mean Weight (g per Day) and Consumers (%) | |||
|---|---|---|---|---|
| IoM | ALSPAC | |||
| Boys n = 244 | Girls n = 246 | Boys n = 3593 | Girls n = 3494 | |
| Total bread | 93 (98) *** | 91 (98) ††† | 74 (97) | 68 (97) |
| White bread | 78 (95) *** | 76 (94) ††† | 59 (90) | 54 (89) |
| Brown bread | 5 (10) ** | 3 (11) | 2 (8) | 2 (9) |
| Wholemeal bread | 7 (14) | 4 (12 ) | 9 (20) | 7 (20) |
| High-fibre white bread | 2 (6) | 3 (8) | 1 (3) | 1 (2) |
| Other bread | 1 (5) * | 4 (13) | 3 (11) | 3 (12) |
| Total cereals | 35 (95) | 23 (86) | 35 (90) | 28 (85) †† |
| High-fibre breakfast cereal | 17 (62) | 10 (48) | 18 (55) | 14 (48) † |
| Other breakfast cereal | 17 (70) | 13 (61) | 17 (61) | 14 (59) |
| Biscuits | 20 (84) | 19 (81) | 22 (83) | 19 (82) |
| Cakes, buns, fruit pies | 21 (58) | 23 (65) | 29 (70) *** | 28 (70) †† |
| Puddings, ice cream | 40 (68) | 42 (76) | 45 (70) | 44 (73) |
| Total milk | 344 (97) *** | 258 (94) | 282 (96) | 236 (94) |
| Full-fat milk | 219 (70) *** | 155 (66) ††† | 145 (55) | 114 (51) |
| Semi-skimmed milk | 97 (41) | 88 (42) | 128 (54) ** | 113 (54) †† |
| Skimmed milk | 20 (10) *** | 10 (7) † | 5 (5) | 5 (5) |
| Cheese | 11 (57) | 13 (65) | 11 (54) | 12 (58) |
| Yoghurt, fromage frais | 39 (56) | 34 (57) | 38 (55) | 35 (55) |
| Eggs/egg dishes | 9 (29) | 8 (27) | 8 (26) | 8 (29) |
| Total spreads (includes butter) | 9 (87) | 8 (89) | 12 (91) | 11 (91) |
| Butter | 2 (23) | 2 (23) | 3 (21) | 2 (23) |
| Full fat spreads | 5 (56) | 5 (62) | 8 (71) | 7 (70) |
| Low fat spreads | 2 (21) | 1 (19) | 1 (9) | 1 (10) |
| Total meat | 106 (98) *** | 98 (100) ††† | 82 (96) | 76 (95) |
| Pork | 7 (17) * | 5 (14) | 5 (17) | 5 (17) |
| Beef | 21 (43) *** | 19 (40) ††† | 13 (31) | 13 (31) |
| Chicken, turkey dishes | 23 (58) *** | 22 (55) ††† | 17 (50) | 16 (50) |
| Lamb | 10 (17) *** | 8 (16) †† | 5 (16) | 5 (14) |
| Bacon, ham | 10 (55) * | 10 (52) †† | 8 (46) | 7 (45) |
| Sausages | 11 (43) | 11 (44) †† | 10 (40) | 8 (35) |
| Burgers/ kebabs | 4 (15) | 2 (13) | 4 (15) | 3 (12) |
| Pies | 7 (14) | 6 (15) | 5 (15) | 5 (16) |
| Coated chicken, turkey | 11 (38) | 11 (38) | 10 (30) | 10 (32) |
| Other meat products | 2 (12) | 3 (13) | 3 (15) | 2 (14) |
| Total fish | 12 (35) | 14 (43) | 14 (40) | 15 (44) |
| Oily fish | 3 (13) | 5 (20) | 3 (13) | 4 (18) |
| Coated white fish | 7 (22) | 7 (24) | 8 (27) | 8 (26) |
| Other fish | 2 (5) | 3 (7) | 2 (6) | 2 (7) |
| Total vegetables | 45 (83) | 50 (87) | 42 (87) | 54 (89) |
| Salad/raw vegetables | 5 (24) | 6 (31) | 6 (31) | 8 (38) |
| Carrots, cooked | 11 (53) | 10 (52) | 11 (52) | 10 (51) |
| Green leafy vegetables | 8 (36) | 9 (36) | 10 (42) | 10 (45) |
| Peas | 7 (43) | 7 (44) † | 6 (35) | 6 (35) |
| Green and runner beans | 1 (9) | 1 (9) | 1 (10) | 2 (12) |
| Tomatoes, tinned/cooked raw | 3 (14) | 6 (24) | 5 (20) | 6 (26) |
| Other cooked vegetables | 9 (43) | 8 (42) | 9 (40) | 9 (41) |
| Baked beans | 19 (38) | 16 (35) | 19 (41) | 15 (36) |
| Potatoes, fried, roast, chips | 50 (85) | 47 (81) | 50 (82) | 47 (81) |
| Other potatoes | 41 (70) *** | 36 (69) †† | 30 (57) | 30 (57) |
| Total fruit | 79 (76) | 82 (81) | 79 (76) | 83(82) |
| Citrus fruit | 11 (21) | 8 (22) | 9 (19) | 12 (24) |
| Apples and pears | 33 (48) | 35 (57) | 31 (50) | 30 (52) |
| Bananas | 19 (39) | 17 (37) | 18 (33) | 16 (32) |
| Other fresh fruit | 15 (30) | 19 (43) | 18 (36) | 22 (43) |
| Canned fruit | 2 (5) | 2 (7) | 2 (6) | 3 (8) |
| Savoury snacks, crisps | 17 (79) | 17 (83) | 18 (82) | 17 (83) |
| Chocolate, confectionery | 13 (64) | 13 (68) | 17 (73) *** | 15 (72) |
| Sugar, confectionery | 5 (40) | 6 (51) | 11 (53) *** | 12 (57) ††† |
| Sugar, preserves, sweet spreads | 7 (68) | 6 (67) | 9 (70) ** | 8 (68) †† |
| Fruit juice | 117 (61) * | 135 (66) ††† | 89 (49) | 89 (51) |
| Soft drinks, sugar-sweetened | 224 (81) *** | 217 (87) ††† | 129 (53) | 112 (50) |
| Soft drinks, diet or low calorie | 141 (59) | 117 (54) | 337 (81) *** | 311 (82) ††† |
| Foods | IoM | ALSPAC | ||
|---|---|---|---|---|
| Boys n = 244 | Girls n = 246 | Boys n = 3593 | Girls n = 3494 | |
| Milk | 11.2 (10.3, 12.0) *** | 9.1 (8.3, 9.9) ††† | 9.2 (9.0, 9.4) | 8.2 (8.0, 8.5) |
| Bread | 12.4 (11.5, 13.2) *** | 12.8 (12.1, 13.6) ††† | 10.1 (9.9, 10.3) | 10.0 (9.8, 10.2) |
| Total meat | 12.3 (11.5, 13.0) *** | 11.9 (11.1, 12.6) ††† | 10.2 (10.0, 10.4) | 10.1 (9.9, 10.3) |
| Beef, pork, lamb, poultry | 5.7 (5.1, 6.3) *** | 5.4 (4.8, 6.0) ††† | 4.1 (4.0, 4.2) | 4.2 (4.1, 4.4) |
| Processed meat | 6.5 (5.9, 7.2) | 6.4 (5.8, 7.0) | 6.1 (5.9, 6.3) | 5.9 (5.7, 6.1) |
| Potatoes (all) | 7.4 (6.8, 8.0) | 7.4 (6.8, 8.0) | 7.1 (7.0, 7.3) | 7.4 (7.3, 7.6) |
| Fried, roast and chips | 5.2 (4.6, 5.7) | 5.3 (4.8, 6.0) | 5.5 (5.3, 5.7) | 5.6 (5.5, 5.8) |
| Other | 2.3 (1.9, 2.6) *** | 2.1 (1.8, 2.4) † | 1.6 (1.5, 1.7) | 1.8 (1.7, 1.9) |
| Sweet foods (all) | 18.5 (17.5, 19.5) | 20.2 (19.1, 21.3) | 24.0 (23.7, 24.3) *** | 24.1 (23.8, 24.4) ††† |
| Confectionery | 5.4 (4.8, 5.9) | 5.9 (5.3, 6.4) | 7.9 (7.7, 8.0) *** | 7.8 (7.6, 8.0) ††† |
| Buns, cakes and pastries | 4.3 (3.7, 4.9) | 4.9 (4.3, 5.6) | 5.9 (5.7, 6.1) *** | 6.2 (6.0, 6.4) † |
| Puddings including ice-cream | 3.5 (3.0, 4.0) | 4.1 (3.6, 4.6) | 4.2 (4.1, 4.4) * | 4.5 (4.3, 4.6) |
| Sweet biscuits | 5.4 (4.8, 5.9) | 5.2 (4.7, 5.8) | 6.0 (5.8, 6.2) | 5.6 (5.5, 5.8) |
| Fruit juice | 2.5 (2.1, 2.9) * | 3.1 (2.6, 3.5) ††† | 1.9 (1.8, 2.0) | 2.0 (1.9, 2.1) |
| Soft drinks with sugar | 3.9 (3.4, 4.4) *** | 4.0 (3.5, 4.5) ††† | 2.3 (2.1, 2.4) | 2.1 (2.0, 2.2) |
| Diet soft drinks | 0.2 (0.1, 0.3) | 0.3 (0.2, 0.4) | 0.3 (0.2, 0.3) | 0.3 (0.2, 0.3) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tweney, E.M.; Emmett, P.M.; Golding, J.; Goodfellow, S.; Taylor, C.M. Comparison of Dietary Intakes of 7-Year-Old Children Enrolled in Observational Birth Cohort Studies on the Isle of Man and in South-West England. Nutrients 2017, 9, 724. https://doi.org/10.3390/nu9070724
Tweney EM, Emmett PM, Golding J, Goodfellow S, Taylor CM. Comparison of Dietary Intakes of 7-Year-Old Children Enrolled in Observational Birth Cohort Studies on the Isle of Man and in South-West England. Nutrients. 2017; 9(7):724. https://doi.org/10.3390/nu9070724
Chicago/Turabian StyleTweney, Ellen M., Pauline M. Emmett, Jean Golding, Stephanie Goodfellow, and Caroline M. Taylor. 2017. "Comparison of Dietary Intakes of 7-Year-Old Children Enrolled in Observational Birth Cohort Studies on the Isle of Man and in South-West England" Nutrients 9, no. 7: 724. https://doi.org/10.3390/nu9070724





