Preschool and School Meal Policies: An Overview of What We Know about Regulation, Implementation, and Impact on Diet in the UK, Sweden, and Australia
Abstract
:1. Introduction
1.1. Background and Aims
1.2. School Food as a Public Health Nutrition Intervention
1.3. Country Contexts
2. UK National Preschool and Primary Food Policy
2.1. UK Regional Preschool Food Policies
2.2. UK Regional School Food Policies
2.3. UK Reach and Implementation of Preschool and Primary Food Policy
2.4. UK Impact of Policy on Diet Quality
3. Swedish Preschool and Primary Meals Provision
3.1. Swedish Preschool and Primary School Meals Guidelines
3.2. Sweden: Reach, Implementation and Impact of Preschool and Primary School Meals Policy
4. Australian Preschool and Primary School Meals
4.1. Australian Preschool Meal Policies
4.2. Australian Primary and Secondary School Meal Policies
4.3. Australian Reach, Implementation, and Impact of Preschool and School Meals Policies
5. Discussion
5.1. Implications for Policy
5.2. Implications for Practice
5.3. Implications for Research
6. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO. What Is a Health Promoting School? Available online: http://www.who.int/school_youth_health/gshi/hps/en/ (accessed on 12 April 2017).
- McKenna, M.L. Policy options to support healthy eating in schools. Can. J. Public Health 2010, 101, S14–S17. [Google Scholar] [PubMed]
- Mikkelsen, B.E.; Engesveen, K.; Afflerbach, T.; Barnekow, V. The human rights framework, the school and healthier eating among young people: A European perspective. Public Health Nutr. 2016, 19, 15–25. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.; Breda, J. School food research: Building the evidence base for policy. Public Health Nutr. 2013, 16, 958–967. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef] [PubMed]
- Public Health England. National Diet And Nutrition Survey Results from Years 5 and 6 Combined of the Rolling Programme for 2012 and 2013 to 2013 and 2014: Report; Public Health England: London, UK, 2016.
- Barbieri, H.E.; Pearson, M.; Becker, W. Riksmaten—Barn 2003. Livsmedels-och Näringsintag Bland Barn i Sverige [Food and Nutrient Intake of Children in Sweden]; Livsmedelsverket: Uppsala, Sweden, 2006. (In Swedish) [Google Scholar]
- Australian Bureau of Statistics. Australian Health Survey: Nutrition First Results—Food and Nutrients, 2011–2012; Australian Bureau of Statistics: Canberra, Australia, 2014.
- Public Health England. National Diet And Nutrition Survey: Results from Years 1 to 4 (Combined) of the Rolling Programme (2008/2009–2011/12): Executive Summary; Public Health England and Food Standards Agency: London, UK, 2015.
- Nelson, M.; Erens, B.; Bates, B.; Church, S.; Boshier, T. Low Income Diet and Nutrition Survey; The Stationary Office: London, UK, 2007; Volume 3. [Google Scholar]
- Rasmussen, M.; Krolner, R.; Klepp, K.; Lytle, L.A.; Brug, J.; Bere, E.; Due, P. Determinants of fruit and vegetable consumption among children and adolescents: A review of the literature. Part I: Quantitative studies. Int. J. Behav. Nutr. Phys. Act. 2006, 3, 22. [Google Scholar] [CrossRef] [PubMed]
- Mattisson, I. Socioekonomiska Skillnader i Matvanor i Sverige [Socioeconomic Differences in Food Habits in Sweden]; Livsmedelsverket: Uppsala, Sweden, 2016. (In Swedish) [Google Scholar]
- Brambila-Macias, J.; Shankar, B.; Capacci, S.; Mazzocchi, M.; Perez-Cueto, F.J.; Verbeke, W.; Traill, W.B. Policy interventions to promote healthy eating: A review of what works, what does not, and what is promising. Food Nutr. Bull. 2011, 32, 365–375. [Google Scholar] [CrossRef] [PubMed]
- Tilles-Tirkkonen, T.; Pentikainen, S.; Lappi, J.; Karhunen, L.; Poutanen, K.; Mykkanen, H. The quality of school lunch consumed reflects overall eating patterns in 11–16-year-old schoolchildren in Finland. Public Health Nutr. 2011, 14, 2092–2098. [Google Scholar] [CrossRef] [PubMed]
- Raulio, S.; Roos, E.; Prattala, R. School and workplace meals promote healthy food habits. Public Health Nutr. 2010, 13, 987–992. [Google Scholar] [CrossRef] [PubMed]
- Rogers, I.S.; Ness, A.R.; Hebditch, K.; Jones, L.R.; Emmett, P.M. Quality of food eaten in English primary schools: School dinners vs. packed lunches. Eur. J. Clin. Nutr. 2007, 61, 856–864. [Google Scholar] [CrossRef] [PubMed]
- Persson Osowski, C.; Lindroos, A.K.; Enghardt Barbieri, H.; Becker, W. The contribution of school meals to energy and nutrient intake of swedish children in relation to dietary guidelines. Food Nutr. Res. 2015, 59, 27563. [Google Scholar] [CrossRef] [PubMed]
- Syrad, H.; Llewellyn, C.H.; van Jaarsveld, C.H.; Johnson, L.; Jebb, S.A.; Wardle, J. Energy and nutrient intakes of young children in the UK: Findings from the gemini twin cohort. Br. J. Nutr. 2016, 115, 1843–1850. [Google Scholar] [CrossRef] [PubMed]
- Bevans, K.B.; Sanchez, B.; Teneralli, R.; Forrest, C.B. Children’s eating behavior: The importance of nutrition standards for foods in schools. J. Sch. Health 2011, 81, 424–429. [Google Scholar] [CrossRef] [PubMed]
- De Costa, P.; Moller, P.; Frost, M.B.; Olsen, A. Changing children’s eating behaviour—A review of experimental research. Appetite 2017, 113, 327–357. [Google Scholar] [CrossRef] [PubMed]
- Ray, C.; Roos, E.; Brug, J.; Behrendt, I.; Ehrenblad, B.; Yngve, A.; te Velde, S.J. Role of free school lunch in the associations between family-environmental factors and children’s fruit and vegetable intake in four European countries. Public Health Nutr. 2013, 16, 1109–1117. [Google Scholar] [CrossRef] [PubMed]
- Williamson, D.A.; Han, H.; Johnson, W.D.; Martin, C.K.; Newton, R.L., Jr. Modification of the school cafeteria environment can impact childhood nutrition. Results from the wise mind and la health studies. Appetite 2013, 61, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Gubbels, J.S.; Gerards, S.M.; Kremers, S.P. Use of food practices by childcare staff and the association with dietary intake of children at childcare. Nutrients 2015, 7, 2161–2175. [Google Scholar] [CrossRef] [PubMed]
- Mukoma, W.; Flisher, A.J. Evaluations of health promoting schools: A review of nine studies. Health Promot. Int. 2004, 19, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Lister-Sharp, D.; Chapman, S.; Stewart-Brown, S.; Sowden, A. Health promoting schools and health promotion in schools: Two systematic reviews. Health Technol. Assess. 1999, 3, 1–207. [Google Scholar] [PubMed]
- Skolverket [Swedish National Agency for Education]. Curriculum for the Preschool Lpfö 98 Revised 2010; Skolverket: Stockholm, Sweden, 2010. [Google Scholar]
- Department for Education. Statutory Framework for the Early Years Foundation Stage. Setting the Standards for Learning, Development and Care for Children from Birth to Five; Department for Education: London, UK, 2012.
- The Organisation for Economic Co-operation and Development (OCED). Country Statistical Profiles: Key Tables from OECD; The Organisation for Economic Co-operation and Development (OECD): Paris, France, 2017. [Google Scholar]
- Gov.Uk. Help Paying for Childcare. Available online: https://www.gov.uk/help-with-childcare-costs/free-childcare-and-education-for-2-to-4-year-olds (accessed on 22 April 2017).
- Department for Education. Will I Qualify for 30 h Free Childcare? Available online: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/600592/30_h_free_childcare_eligibility.pdf (accessed on 22 April 2017).
- Family and Childcare Trust. Help with My Childcare Costs. Available online: https://www.familyandchildcaretrust.org/help-my-childcare-costs (accessed on 10 July 2017).
- Evans, C.E.; Harper, C.E. A history and review of school meal standards in the UK. J. Hum. Nutr. Diet. 2009, 22, 89–99. [Google Scholar] [CrossRef] [PubMed]
- The Children’s Food Trust. Eat Better Start Better, Voluntary Food and Drink Guidelines for Early Years Settings in England—A Practical Guide; Children’s Food Trust: Sheffield, UK, 2012; p. 80. [Google Scholar]
- Advisory Panel on Food and Nutrition in Early Years. Laying the Table. Recommendations for National Food and Nutrition Guidance for Early Years Settings in England; Main Report; Schools Food Trust: Sheffield, UK, 2010; Volume 1. [Google Scholar]
- NHS Scotland. Setting the Table. Nutritional Guidance and Food Standards for Early Years Childcare Providers in Scotland; NHS Scotland: Edinburgh, UK, 2015.
- Children’s Food Trust. Available online: http://www.childrensfoodtrust.org.uk/childrens-food-trust/parents/your-childs-food-at-school/packed-lunches/packed-lunch-information/ (accessed on 10 July 2017).
- Department for Education. Provision for Children under Five Years of Age in England; Statistical First Release; Department for Education: London, UK, 2013.
- Nicholas, J.; Stevens, L.; Briggs, L.; Wood, L. Pre-School Food Survey; Children’s Food Trust: Sheffield, UK, 2013. [Google Scholar]
- Lucas, P.; Richards, H.; Johnson, L. How common are packed or sack lunches in English early education and care? (Bristol, England). Personal communication, 2017. [Google Scholar]
- FOI Directory. Reference from Freedom of Information Directory. Available online: http://www.foi.directory/updates/foi-reveals-rising-numbers-of-pupils-home-educated/ (accessed on 10 July 2017).
- Wollny, I.; Lord, C.; Tanner, E.; Fry, A.; Tipping, S.; Kitchen, S. School Lunch Take-Up Survey 2013 to 2014 Research Report; Department for Education: London, UK, 2015.
- Chambers, S.; Ford, A.; Boydell, N.; Moore, L.; Stead, M.; Eadie, D. Universal free school meals in Scotland: A process evaluation of implementation and uptake. Eur. J. Public Health 2016, 26, ckw169. [Google Scholar] [CrossRef]
- Parker, M.; Lloyd-Williams, F.; Weston, G.; Macklin, J.; McFadden, K. Nursery nutrition in liverpool: An exploration of practice and nutritional analysis of food provided. Public Health Nutr. 2011, 14, 1867–1875. [Google Scholar] [CrossRef] [PubMed]
- Mucavele, P.; Sharp, L.; Wall, C.; Nicholas, J. Children’s food trust ‘eat better, start better’ programme: Outcomes and recommendations. Perspect. Public Health 2014, 134, 67–69. [Google Scholar] [PubMed]
- Sweitzer, S.J.; Briley, M.E.; Robert-Gray, C. Do sack lunches provided by parents meet the nutritional needs of young children who attend child care? J. Am. Diet. Assoc. 2009, 109, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Romo-Palafox, M.J.; Ranjit, N.; Sweitzer, S.J.; Roberts-Gray, C.; Hoelscher, D.M.; Byrd-Williams, C.E.; Briley, M.E. Dietary quality of preschoolers’ sack lunches as measured by the healthy eating index. J. Acad. Nutr. Diet. 2015, 115, 1779–1788. [Google Scholar] [CrossRef] [PubMed]
- Spence, S.; Delve, J.; Stamp, E.; Matthews, J.N.; White, M.; Adamson, A.J. Did school food and nutrient-based standards in England impact on 11–12Y olds nutrient intake at lunchtime and in total diet? Repeat cross-sectional study. PLoS ONE 2014, 9, e112648. [Google Scholar] [CrossRef] [PubMed]
- Spence, S.; Delve, J.; Stamp, E.; Matthews, J.N.; White, M.; Adamson, A.J. The impact of food and nutrient-based standards on primary school children’s lunch and total dietary intake: A natural experimental evaluation of government policy in England. PLoS ONE 2013, 8, e78298. [Google Scholar] [CrossRef] [PubMed]
- Golley, R.; Pearce, J.; Nelson, M. Children’s lunchtime food choices following the introduction of food-based standards for school meals: Observations from six primary schools in sheffield. Public Health Nutr. 2011, 14, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Adamson, A.; Spence, S.; Reed, L.; Conway, R.; Palmer, A.; Stewart, E.; McBratney, J.; Carter, L.; Beattie, S.; Nelson, M. School food standards in the UK: Implementation and evaluation. Public Health Nutr. 2013, 16, 968–981. [Google Scholar] [CrossRef] [PubMed]
- Moore, L.; Tapper, K. The impact of school fruit tuck shops and school food policies on children’s fruit consumption: A cluster randomised trial of schools in deprived areas. J. Epidemiol. Commun. Health 2008, 62, 926–931. [Google Scholar] [CrossRef] [PubMed]
- Haroun, D.; Harper, C.; Wood, L.; Nelson, M. The impact of the food-based and nutrient-based standards on lunchtime food and drink provision and consumption in primary schools in England. Public Health Nutr. 2011, 14, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, J.; Wood, L.; Harper, C.; Nelson, M. The impact of the food-based and nutrient-based standards on lunchtime food and drink provision and consumption in secondary schools in England. Public Health Nutr. 2013, 16, 1052–1065. [Google Scholar] [CrossRef] [PubMed]
- Pearce, J.; Wood, L.; Stevens, L. Portion weights of food served in english schools: Have they changed following the introduction of nutrient-based standards? J. Hum. Nutr. Diet. 2013, 26, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Belot, M.; James, J. Healthy school meals and educational outcomes. J. Health Econom. 2011, 30, 489–504. [Google Scholar] [CrossRef] [PubMed]
- Department for Education. Available online: www.gov.uk/government/publications/evaluation-of-the-free-school-meals-pilot-impact-report (accessed on 10 July 2017).
- Evans, C.E.; Greenwood, D.C.; Thomas, J.D.; Cade, J.E. A cross-sectional survey of children’s packed lunches in the UK: Food- and nutrient-based results. J. Epidemiol. Commun. Health 2010, 64, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.E.; Mandl, V.; Christian, M.S.; Cade, J.E. Impact of school lunch type on nutritional quality of english children’s diets. Public Health Nutr. 2016, 19, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Harrison, F.; Jennings, A.; Jones, A.; Welch, A.; van Sluijs, E.; Griffin, S.; Cassidy, A. Food and drink consumption at school lunchtime: The impact of lunch type and contribution to overall intake in british 9–10-year-old children. Public Health Nutr. 2013, 16, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Sveriges Riksdag [The Swedish Parliament]. Den nya Skollagen—för Kunskap, Valfrihet och Trygghet [The New School Law—For Knowledge, Choice and Security]; Sveriges Riksdag, Ed.; Sveriges Riksdag: Stockholm, Sweden, 2010. (In Swedish) [Google Scholar]
- Skolverket [Swedish National Agency for Education]. Måluppfyllelse i förskolan [Goal Achievement in Preschool]; Skolverket: Stockholm, Sweden, 2017. (In Swedish) [Google Scholar]
- Persson Osowski, C.; Goranzon, H.; Fjellstrom, C. Teachers’ interaction with children in the school meal situation: The example of pedagogic meals in Sweden. J. Nutr. Educ. Behav. 2013, 45, 420–427. [Google Scholar] [CrossRef] [PubMed]
- Swedish National Food Agency. Good School Meals; Livsmedelsverket: Uppsala, Sweden, 2014. [Google Scholar]
- Livsmedelsverket [Swedish National Food Agency]. Bra måltider i Förskolan [Good Meals in Preschool]; Livsmedelsverket: Uppsala, Sweden, 2016. (In Swedish) [Google Scholar]
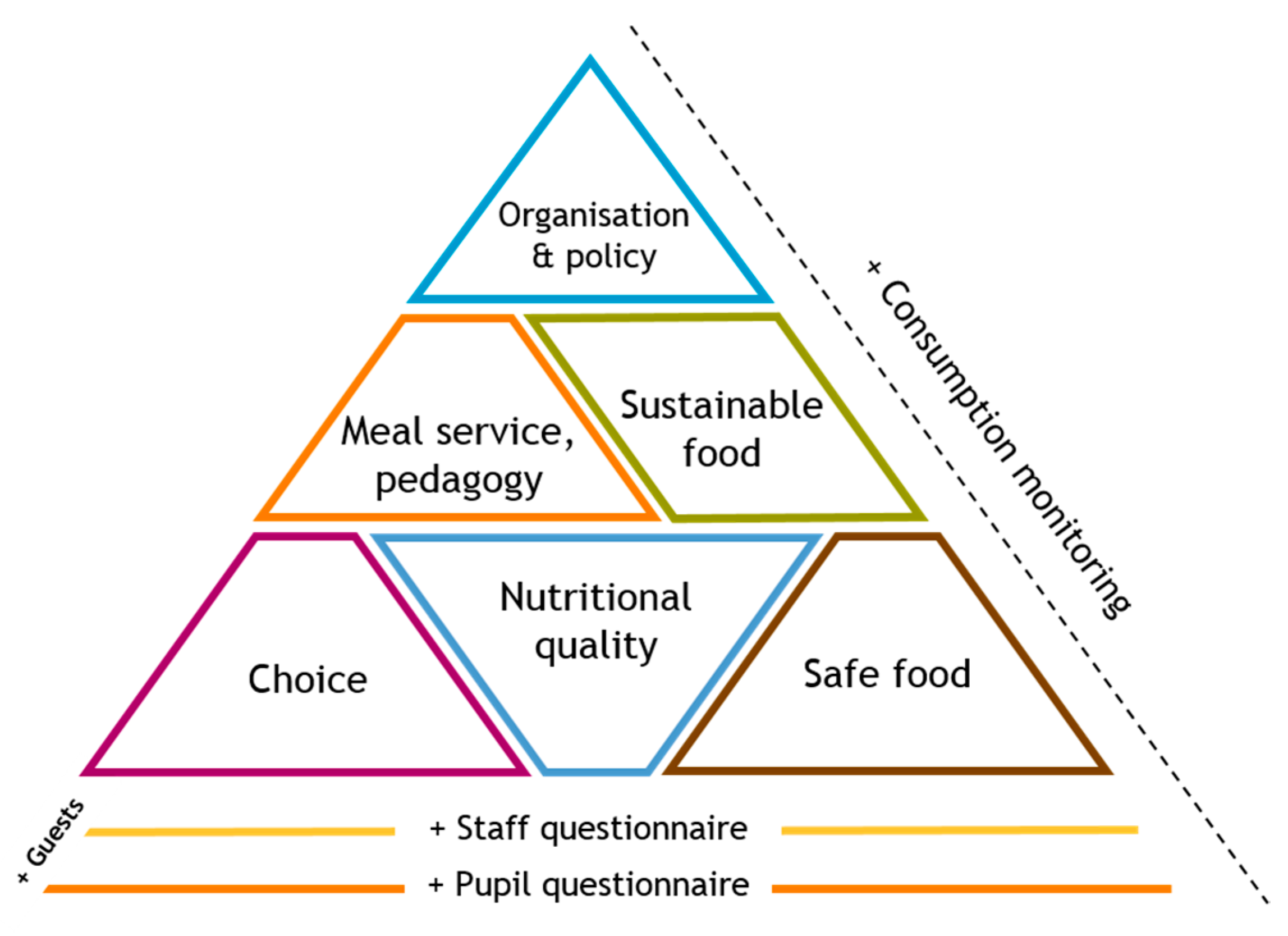
- Patterson, E.; Quetel, A.-K.; Lilja, K.; Simma, M.; Olsson, L.; Schäfer Elinder, L. Design, testing and validation of an innovative web-based instrument to evaluate school meal quality. Public Health Nutr. 2013, 16, 1028–1036. [Google Scholar] [CrossRef] [PubMed]
- SkolmatSverige. What Is Skolmatsverige? Available online: www.skolmatsverige.se/in-english (accessed on 22 June 2017).
- Patterson, E.; Elinder, L.S. Improvements in school meal quality in Sweden after the introduction of new legislation-a 2-year follow-up. Eur. J. Public Health 2015, 25, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Patterson, E.; Regnander, M.; Elinder, L.S. SkolmatSveriges Kartläggning av Skolmåltidens Kvalitet—Läsåret 2014/15 [School Food Sweden’s Survey of School Meal Quality—For the School Year 2014/15]; Centrum för Epidemiologi och Samhällsmedicin, Stockholms Läns Landsting: Stockholm, Sweden, 2015. (In Swedish) [Google Scholar]
- Skolmatens Vänner; Livsmedelsverket. Kartläggning av Sveriges Kommuner Gällande Skolmaten i Grundskolan [Survey of Sweden’s Municpalities Concerning School Food in Primary School]. Available online: https://www.livsmedelsverket.se/globalassets/rapporter/2016/rapport-2016---maltidsverksamheten-i-kommunala-grundskolor.pdf (accessed on 10 July 2017).
- Australian Children’s Education and Care Quality Authority (ACEQUA). The National Quality Framework. Available online: http://www.acecqa.gov.au/national-quality-framework (accessed on 10 July 2017).
- Nutrition Australia Victoria Division. Healthy Eating Advisory Service. Available online: http://heas.health.vic.gov.au/ (accessed on 10 July 2017).
- New South Wales Office of Preventative Health. The Munch & Move Program. Available online: http://www.preventivehealth.net.au/munch--move.html (accessed on 10 July 2017).
- Nutrition Australia ACT Division. Act Nutrition Support Service. Available online: http://www.actnss.org/ (accessed on 10 July 2017).
- Bell, A.C.; Swinburn, B.A. What are the key food groups to target for preventing obesity and improving nutrition in schools? Eur. J. Clin. Nutr. 2004, 58, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Sanigorski, A.M.; Bell, A.C.; Kremer, P.J.; Swinburn, B.A. Lunchbox contents of Australian school children: Room for improvement. Eur. J. Clin. Nutr. 2005, 59, 1310–1316. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. Role of the School Canteen in Contributing to a Health Promoting School. Available online: http://health.gov.au/internet/publications/publishing.nsf/Content/canteen-mgr-tr1~role-school-canteen (accessed on 10 July 2017).
- Lawlis, T.; Knox, M.; Jamieson, M. School canteens: A systematic review of the policy, perceptions and use from an Australian perspective. Nutr. Diet. 2016, 73, 389–398. [Google Scholar] [CrossRef]
- NHMRC. Australian Dietary Guidelines; NHMRC: Canberra, Australia, 2013.
- NSW School Canteen Advisory Committee. Fresh Tastes @ School: NSW Healthy School Canteen Strategy; NSW School Canteen Advisory Committee: Sydney, Australia, 2006. [Google Scholar]
- Department of Education. Healthy Food And Drink Policy; Department of Education: Perth, Australia, 2014.
- Department of Education. Smart Choices: Healthy Food and Drink Supply Strategy for Queensland Schools; Department of Education: Brisbane, Australia, 2016.
- Victorian Government. Healthy Canteen Kit: School Canteens and Other School Food Services Policy; Victorian Government: Melbourne, Australia, 2012.
- Department of Education. Canteen, Nutrition and Healthy Eating; Department of Education: Darwin, Australia, 2013.
- Tasmanian School Canteen Association Inc. School Canteen Handbook: A Whole School Approach to Healthy Eating; Tasmanian School Canteen Association Inc.: Hobart, Australia, 2014. [Google Scholar]
- Department of Health. National Healthy School Canteens: Guidelines for Healthy Foods and Drinks Supplied in School Canteens; Department of Health: Canberra, Australia, 2014.
- Department for Education and Child Development. Right Bite, Easy Guide to Healthy Food and Drink Supply for South Australian Schools and Preschools; Department for Education and Child Development: Adelaide, Australia, 2008.
- Woods, J.; Bressan, A.; Langelaan, C.; Mallon, A.; Palermo, C. Australian school canteens: Menu guideline adherence or avoidance? Health Promot. J. Aust. 2014, 25, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Ardzejewska, K.; Tadros, R.; Baxter, D. A descriptive study on the barriers and facilitators to implementation of the NSW (Australia) healthy school canteen strategy. Health Educ. J. 2012, 72, 136–145. [Google Scholar] [CrossRef]
- De Silva-Sanigorski, A.; Breheny, T.; Jones, L.; Lacy, K.; Kremer, P.; Carpenter, L.; Bolton, K.; Prosser, L.; Gibbs, L.; Waters, E.; et al. Government food service policies and guidelines do not create healthy school canteens. Aust. N. Z. J. Public Health 2011, 35, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Pettigrew, S.; Donovan, R.J.; Jalleh, G.; Pescud, M. Predictors of positive outcomes of a school food provision policy in Australia. Health Promot. Int. 2014, 29, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Hills, A.; Nathan, N.; Robinson, K.; Fox, D.; Wollfenden, L. Improvement in primary school adherence to the NSW healthy school canteen strategy in 2007 and 2010. Health Promot. J. Aust. 2015, 26, 89–92. [Google Scholar] [CrossRef] [PubMed]
- Dick, M.; Lee, A.; Bright, M.; Turner, K.; Edwards, R.; Dawson, J.; Miller, J. Evaluation of implementation of a healthy food and drink supply strategy throughout the whole school environment in queensland state schools, Australia. Eur. J. Clin. Nutr. 2012, 66, 1124–1129. [Google Scholar] [CrossRef] [PubMed]
- Reilly, K.; Nathan, N.; Wolfenden, L.; Wiggers, J.; Sutherland, R.; Wyse, R.; Yoong, S.L. Validity of four measures in assessing school canteen menu compliance with state-based healthy canteen policy. Health Promot. J. Aust. 2016, 27, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Yoong, S.L.; Nathan, N.; Wolfenden, L.; Wiggers, J.; Reilly, K.; Oldmeadow, C.; Wyse, R.; Sutherland, R.; Delaney, T.; Butler, P.; et al. Cafe: A multicomponent audit and feedback intervention to improve implementation of healthy food policy in primary school canteens: A randomised controlled trial. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 126. [Google Scholar] [CrossRef] [PubMed]
- Cole, A.; Vidgen, H.; Cleland, P. Food provision in early childhood education and care services: Exploring how staff determine nutritional adequacy. Nutr. Diet. 2017, 74, 105–110. [Google Scholar] [CrossRef]
- Council on School Health; Committee on Nutrition. Snacks, sweetened beverages, added sugars, and schools. Pediatrics 2015, 135, 575–583. [Google Scholar]
- Perez-Cueto, F.J.; Aschemann-Witzel, J.; Shankar, B.; Brambila-Macias, J.; Bech-Larsen, T.; Mazzocchi, M.; Capacci, S.; Saba, A.; Turrini, A.; Niedzwiedzka, B.; et al. Assessment of evaluations made to healthy eating policies in Europe: A review within the eatwell project. Public Health Nutr. 2012, 15, 1489–1496. [Google Scholar] [CrossRef] [PubMed]
- Ganann, R.; Fitzpatrick-Lewis, D.; Ciliska, D.; Peirson, L.J.; Warren, R.L.; Fieldhouse, P.; Delgado-Noguera, M.F.; Tort, S.; Hams, S.P.; Martinez-Zapata, M.J.; et al. Enhancing nutritional environments through access to fruit and vegetables in schools and homes among children and youth: A systematic review. BMC Res. Notes 2014, 7, 422. [Google Scholar] [CrossRef] [PubMed]
- Treasury, H. The Magenta Book. Guidance for Evaluation; HM Treasury: London, UK, 2011.
- Campaign for Tobacco Free Kids. How Schools Can Help Students Stay Tobacco-Free. Available online: http://www.tobaccofreekids.org/research/factsheets/pdf/0153.pdf (accessed on 27 June 2017).
- Oliver, T.R. The politics of public health policy. Annu. Rev. Public Health 2006, 27, 195–233. [Google Scholar] [CrossRef] [PubMed]
- Centre for Disease Control. Zoning to Encourage Healthy Eating. Available online: https://www.cdc.gov/phlp/winnable/zoning_obesity.html (accessed on 27 June 2017).
- Parliamentary Office for Science and Technology (POST). Barriers to Healthy Food; Parliamentary Office for Science and Technology: London, UK, 2016. [Google Scholar]
- Dudley, D.A.; Cotton, W.G.; Peralta, L.R. Teaching approaches and strategies that promote healthy eating in primary school children: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 28. [Google Scholar] [CrossRef] [PubMed]
- Sansolios, S.; Mikkelsen, B.E. Views of parents, teachers and children on health promotion in kindergarten—First results from formative focus groups and observations. J. Paediatr. Obes. 2011, 6, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.; Murphy, S.; Tapper, K.; Moore, L. From policy to plate: Barriers to implementing healthy eating policies in primary schools in Wales. Health Policy 2010, 94, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Evans, C.E.; Greenwood, D.C.; Thomas, J.D.; Cleghorn, C.L.; Kitchen, M.S.; Cade, J.E. Smart lunch box intervention to improve the food and nutrient content of children’s packed lunches: UK wide cluster randomised controlled trial. J. Epidemiol. Commun. Health 2010, 64, 970–976. [Google Scholar] [CrossRef] [PubMed]
- Sweitzer, S.J.; Briley, M.E.; Roberts-Gray, C.; Hoelscher, D.M.; Staskel, D.M.; Almansour, F.D. How to help parents pack better preschool sack lunches: Advice from parents for educators. J. Nutr. Educ. Behav. 2011, 43, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Sweitzer, S.J.; Ranjit, N.; Calloway, E.E.; Hoelscher, D.M.; Almansor, F.; Briley, M.E.; Roberts-Gray, C.R. Examining how adding a booster to a behavioral nutrition intervention prompts parents to pack more vegetables and whole gains in their preschool children’s sack lunches. Behav. Med. 2016, 42, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.A.; Cates, S.C.; Blitstein, J.L.; Hersey, J.; Gabor, V.; Ball, M.; Kosa, K.; Wilson, H.; Olson, S.; Singh, A. Nutrition-education program improves preschoolers’ at-home diet: A group randomized trial. J. Acad. Nutr. Diet. 2014, 114, 1001–1008. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, J.; Christian, M.S.; Evans, C.E.; Nykjaer, C.; Hancock, N.; Cade, J.E. Evaluation of the impact of school gardening interventions on children’s knowledge of and attitudes towards fruit and vegetables. A cluster randomised controlled trial. Appetite 2015, 91, 405–414. [Google Scholar] [CrossRef] [PubMed]
- De Silva-Sanigorski, A.; Prosser, L.; Carpenter, L.; Honisett, S.; Gibbs, L.; Moodie, M.; Sheppard, L.; Swinburn, B.; Waters, E. Evaluation of the childhood obesity prevention program Kids—‘Go for your life’. BMC Public Health 2010, 10, 288. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.M.; Nathan, N.; Delaney, T.; Yoong, S.L.; Wiggers, J.; Preece, S.; Lubans, N.; Sutherland, R.; Pinfold, J.; Smith, K.; et al. Cafe: A multicomponent audit and feedback intervention to improve implementation of healthy food policy in primary school canteens: Protocol of a randomised controlled trial. BMJ Open 2015, 5, e006969. [Google Scholar] [CrossRef] [PubMed]
- Waling, M.; Olafsdottir, A.S.; Lagstrom, H.; Wergedahl, H.; Jonsson, B.; Olsson, C.; Fossgard, E.; Holthe, A.; Talvia, S.; Gunnarsdottir, I.; et al. School meal provision, health, and cognitive function in a nordic setting—The promeal-study: Description of methodology and the nordic context. Food Nutr. Res. 2016, 60, 30468. [Google Scholar] [CrossRef] [PubMed]

| Food | Standard or Guidance | Level, Country (Jurisdiction) |
|---|---|---|
| Fruit and vegetables | Minimum number portions per day/meal | School and Preschool, UK (England, Scotland) |
| Meat, fish, eggs, and non-dairy protein | ||
| Starchy foods | Recommended number of portions per day | School and Preschool, UK (England, Scotland) |
| Milk and dairy | ||
| Drinks | Fresh water to be freely available | School and Preschool, UK (England, Scotland) |
| Diluted fruit juice or fresh cows’ milks | Preschool, UK (England, Scotland) | |
| Traffic Light: “Green” foods | Minimum of 60% of food and snacks sold should be “Green” | School, Australia (WA *) |
| Should be available every day the canteen is open | School, Australia (NT, SA, Q, V *) | |
| Every-day (Core) foods | Recommended to make up 75% of food and drinks sold | School, Australia (NSW *) |
| “Nutritious” meals | Meals must be “nutritious”. Preschool meals must also be “varied”, and “evenly distributed over the day” | School and Preschool, Sweden |
| “Good meals in preschool” | Suggestions provided for meal components and nutritional content (e.g., serve fatty fish twice within 4 weeks, serve only milk and water to drink, provide a wide selection of salads, include wholegrain versions of products etc.) | School and Preschool, Sweden |
| “Good school meals” |
| Food | Standard or Guidance | Level, Country (Jurisdiction) |
|---|---|---|
| Meat, fish, eggs, and non-dairy protein | Maximum number portions | School, UK (England), Preschool UK (Scotland) |
| Starchy foods | Maximum number of occasions higher fat versions offered (fried starchy foods and cheese as protein) | School, UK (England) |
| Milk and dairy food | ||
| Traffic Light: “Amber” foods | Maximum of 40% of foods and drinks sold should be “Amber” | School, Australia (WA *) |
| “Amber” foods should be limited and sold in smaller serve sizes | School, Australia (NT, SA, Q, V *) | |
| Desserts & Puddings | To be served only once per day with main meal | School and Preschool, UK (England, Scotland) |
| Occasional (non-core) foods | Maximum of 25% of food and drinks sold should be “occasional” and least healthy not sold | School, Australia (NSW *) |
| Foods high in fat, salt, and sugar | Avoided or limited | School and Preschool, UK (England, Scotland) |
| Traffic Light: “Red” foods | “Red” foods prohibited or limited to special occasions (no more than twice per term) | School, Australia (NT, SA, Q, V *) |
| “Red” foods prohibited | School, Australia (NT, SA, Q, V *) | |
| Salt and condiments | Reduced or not salt in cooking, No salt available to add. Condiments avoided or size limited. | School and Preschool, UK (England, Scotland) |
| Should not be available to students | School and Preschool, Sweden | |
| Drinks | All those not specified to be excluded | School and Preschool, UK (England, Scotland) |
| “Amber” drinks should be avoided and sold in smaller serve sizes | School, Australia (NT, SA, Q, V *) | |
| “Red” drinks (sugary) not to be sold and not permitted | School, Australia (all states and territories) | |
| No sweet drinks containing sugar or sweetener | School and Preschool, Sweden | |
| Confectionary | Not permitted | School and Preschool, UK (England, Scotland) |
| Not permitted | School, Australia (all states and territories) | |
| Should not be provided | School and Preschool, Sweden |
| Policy | Country (Jurisdiction) | Level | Reach | Cost to Families | System of Monitoring |
|---|---|---|---|---|---|
| Food Based Standards for Schools in England | UK (England) | School | Mandatory for local government controlled schools and schools that became academies before 2010 and after June 2014. Recommended for remaining academies and private schools. | Free for 4–7 years | Included in the Office of Standards in Education (OFSTED) inspection report on healthy eating. |
| Paid for other years | |||||
| Voluntary Guidance | UK (England) | Preschool | Voluntary | Paid | Not monitored in OFSTED inspections, although the Early Years Foundation Stage (EYFS) requires that provided food must be “healthy balanced and nutritious” (EYFS 2017). |
| Preschool standards | UK (Scotland) | Preschool | Mandatory for all settings registered with the Care Inspectorate. | Paid | Inspected by the Care Inspectorate. EEC must show they provide opportunities for children to learn about diet and health. EEC must show children have access to a well-balanced and healthy diet. For example, through use of a food policy. |
| Traffic light food groups | Australia (Australia Capital Territory) | School | Policy applies to all food services activities within a school setting. Mandatory for government schools. In independent and Catholic schools, it is not mandatory but highly recommended. | Paid | Independent compliance monitoring. Free assessment, resources and training available for canteens. Facilitate government license agreements with school canteens. |
| Australia (Northern Territory) | School | Policy applies to all food services activities within a school setting. Mandatory for government schools | Paid | Independent compliance monitoring, schools responsible for oversight. | |
| Australia (South Australia) | School | Policy applies to all food services activities within a school setting. Mandatory for government schools. Catholic and independent school sectors support implementation of the policy. | Paid | Independent compliance monitoring, schools responsible for oversight. Resources provided to canteens. | |
| Australia (Queensland) | School | Policy applies to all food services activities within a school setting. Mandatory for government schools. | Paid | Independent compliance monitoring, schools responsible for oversight. Training and resources provided to canteens. | |
| Australia (Tasmania) | School | Schools are recommended (not mandatory) to apply to have their canteen accredited. | Paid | Training, resources and monitoring available to canteens. | |
| Australia (Victoria) | School | Policy applies to all food services activities within a school setting. Mandatory for government schools. | Paid | Independent compliance monitoring, schools responsible for oversight. Optional monitoring and assessment of canteens available. Training and resources provided to canteens. | |
| Every-day vs. occasional foods | Australia (New South Wales) | School | Policy applies to all food services activities within a school setting. Mandatory for government schools. Catholic and independent schools are also encouraged to participate. | Paid | Independent compliance monitoring, schools responsible for oversight. Resources provided to canteens. |
| Traffic light and core vs. non-core foods | Australia (Western Australia) | School | Policy applies to all food services activities within a school setting. Mandatory for government schools. Catholic schools have a similar mandatory policy. | Paid | Principals are required to develop and implement a whole school-based policy on the provision of healthy food and drinks and ensure that the school canteen/food service menu complies with the requirements of the policy. |
| Nutritious preschool meals | Sweden | Preschool | Legislation. Mandatory for all (whether local authority or privately run). | Free or subsidized * | Monitoring of provision and cost is not required. Monitoring of nutritional quality falls to the management (i.e., the local authority or owner). |
| Nutritious school meals | Sweden | School | Legislation. Mandatory for all (whether local authority or privately run). | Free | Monitoring of provision and cost is not required. Monitoring of nutritional quality falls under the School Inspectorate, but is delagated to the school management (i.e., the local authority or owner). |
| “Good meals in preschool”, “Good school meals” | Sweden | Preschool, School | Guidelines. Voluntary for all. | Free or subsidized * | Not applicable, but for schools, compliance with several of the guidelines can be demonstrated using “School Food Sweden” tool. |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucas, P.J.; Patterson, E.; Sacks, G.; Billich, N.; Evans, C.E.L. Preschool and School Meal Policies: An Overview of What We Know about Regulation, Implementation, and Impact on Diet in the UK, Sweden, and Australia. Nutrients 2017, 9, 736. https://doi.org/10.3390/nu9070736
Lucas PJ, Patterson E, Sacks G, Billich N, Evans CEL. Preschool and School Meal Policies: An Overview of What We Know about Regulation, Implementation, and Impact on Diet in the UK, Sweden, and Australia. Nutrients. 2017; 9(7):736. https://doi.org/10.3390/nu9070736
Chicago/Turabian StyleLucas, Patricia Jane, Emma Patterson, Gary Sacks, Natassja Billich, and Charlotte Elizabeth Louise Evans. 2017. "Preschool and School Meal Policies: An Overview of What We Know about Regulation, Implementation, and Impact on Diet in the UK, Sweden, and Australia" Nutrients 9, no. 7: 736. https://doi.org/10.3390/nu9070736





