Inverse Associations between a Locally Validated Mediterranean Diet Index, Overweight/Obesity, and Metabolic Syndrome in Chilean Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Data Collection, and Subjects
2.2. Dietary, Anthropometric, and Clinical Measurements
2.3. Statistical Analyses
3. Results
3.1. Sample Characteristics
3.2. Diet Quality Evaluation Using Chilean-MDI
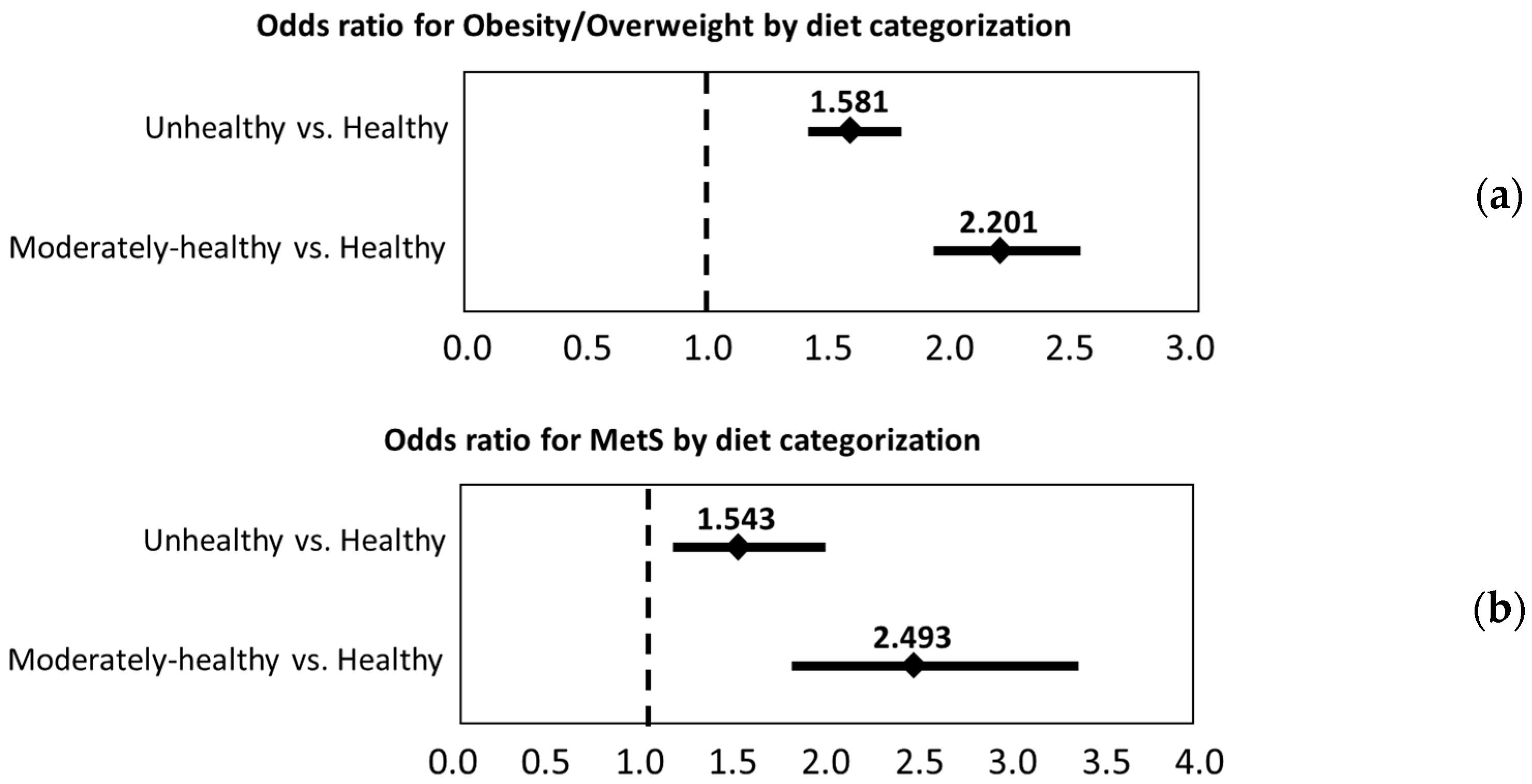
3.3. Associations between Chilean-MDI, BMI, and MetS
3.4. Association between Chilean-MDI Food Groups, BMI, and MetS Components
4. Discussion
Acknowledgments
Author Contributions
Conflicts of Interest
References
- WHO. Global Status Report on Noncommunicable Diseases; World Health Organization (WHO): Geneva, Switzerland, 2014; pp. 1–273. [Google Scholar]
- Grundy, S.M.; Brewer, H.B.; Cleeman, J.I.; Smith, S.C.; Lenfant, C.; Participants, F.T.C. Definition of metabolic syndrome: Report of the national heart, lung, and blood institute/American heart association conference on scientific issues related to definition. Circulation 2004, 109, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Mottillo, S.; Filion, K.B.; Genest, J.; Joseph, L.; Pilote, L.; Poirier, P.; Rinfret, S.; Schiffrin, E.L.; Eisenberg, M.J. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J. Am. Coll. Cardiol. 2010, 56, 1113–1132. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Li, C.; Sattar, N. Metabolic syndrome and incident diabetes: Current state of the evidence. Diabetes Care 2008, 31, 1898–1904. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Muntner, P.; Hamm, L.L.; Jones, D.W.; Batuman, V.; Fonseca, V.; Whelton, P.K.; He, J. The metabolic syndrome and chronic kidney disease in US Adults. Ann. Intern. Med. 2004, 140, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Chiodini, P.; Colao, A.; Lenzi, A.; Giugliano, D. Metabolic syndrome and risk of cancer: A systematic review and meta-analysis. Diabetes Care 2012, 35, 2402–2411. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kahn, R.; Buse, J.; Ferrannini, E.; Stern, M. The metabolic syndrome: Time for a critical appraisal: Joint statement from the American diabetes association and the European association for the study of diabetes. Diabetes Care 2005, 28, 2289–2304. [Google Scholar] [CrossRef] [PubMed]
- Feldeisen, S.E.; Tucker, K.L. Nutritional strategies in the prevention and treatment of metabolic syndrome. Appl. Physiol. Nutr. Metab. 2007, 32, 46–60. [Google Scholar] [CrossRef] [PubMed]
- Swinburn, B.A.; Caterson, I.; Seidell, J.C.; James, W.P. Diet, nutrition and the prevention of excess weight gain and obesity. Public Health Nutr. 2004, 7, 123–146. [Google Scholar] [PubMed]
- Jacques, P.F.; Tucker, K.L. Are dietary patterns useful for understanding the role of diet in chronic disease? Am. J. Clin. Nutr. 2001, 73, 1–2. [Google Scholar] [PubMed]
- Hoffmann, K.; Schulze, M.; Boeing, H.; Altenburg, H. Dietary patterns: Report of an international workshop. Public Health Nutr. 2002, 5, 89–90. [Google Scholar] [CrossRef]
- Schulze, M.B.; Hu, F.B. Dietary patterns and risk of hypertension, type 2 diabetes mellitus, and coronary heart disease. Curr. Atheroscler. Rep. 2002, 4, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Bach, A.; Serra-Majem, L.; Carrasco, J.L.; Roman, B.; Ngo, J.; Bertomeu, I.; Obrador, B. The use of indexes evaluating the adherence to the Mediterranean diet in epidemiological studies: A review. Public Health Nutr. 2006, 9, 132–146. [Google Scholar] [CrossRef] [PubMed]
- Willett, W.C.; Sacks, F.; Trichopoulou, A.; Drescher, G.; Ferro-Luzzi, A.; Helsing, E.; Trichopoulos, D. Mediterranean diet pyramid: A cultural model for healthy eating. Am. J. Clin. Nutr. 1995, 61, 1402S–1406S. [Google Scholar] [PubMed]
- Panagiotakos, D.B.; Chrysohoou, C.; Pitsavos, C.; Stefanadis, C. Association between the prevalence of obesity and adherence to the Mediterranean diet: The attica study. Nutrition 2006, 22, 449–456. [Google Scholar] [CrossRef] [PubMed]
- Schrröder, H. Protective mechanisms of the Mediterranean diet in obesity and type 2 diabetes. J. Nutr. Biochem. 2007, 18, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.; Marrugat, J.; Vila, J.; Covas, M.I.; Elosua, R. Adherence to the traditional Mediterranean diet is inversely associated with body mass index and obesity in a Spanish population. J. Nutr. 2004, 134, 3355–3361. [Google Scholar] [PubMed]
- Kastorini, C.M.; Milionis, H.J.; Esposito, K.; Giugliano, D.; Goudevenos, J.A.; Panagiotakos, D.B. The effect of mediterranean diet on metabolic syndrome and its components: A meta-analysis of 50 studies and 534,906 individuals. J. Am. Coll. Cardiol. 2011, 57, 1299–1313. [Google Scholar] [CrossRef] [PubMed]
- Tortosa, A.; Bes-Rastrollo, M.; Sanchez-Villegas, A.; Basterra-Gortari, F.J.; Nuñez-Cordoba, J.M.; Martinez-Gonzalez, M.A. Mediterranean diet inversely associated with the incidence of metabolic syndrome: The sun prospective cohort. Diabetes Care 2007, 30, 2957–2959. [Google Scholar] [CrossRef] [PubMed]
- Rumawas, M.E.; Meigs, J.B.; Dwyer, J.T.; McKeown, N.M.; Jacques, P.F. Mediterranean-style dietary pattern, reduced risk of metabolic syndrome traits, and incidence in the framingham offspring cohort. Am. J. Clin. Nutr. 2009, 90, 1608–1614. [Google Scholar] [CrossRef] [PubMed]
- Kesse-Guyot, E.; Ahluwalia, N.; Lassale, C.; Hercberg, S.; Fezeu, L.; Lairon, D. Adherence to Mediterranean diet reduces the risk of metabolic syndrome: A 6-year prospective study. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 677–683. [Google Scholar] [CrossRef] [PubMed]
- Babio, N.; Toledo, E.; Estruch, R.; Ros, E.; Martínez-González, M.A.; Castañer, O.; Bulló, M.; Corella, D.; Arós, F.; Gómez-Gracia, E.; et al. Mediterranean diets and metabolic syndrome status in the predimed randomized trial. Can. Med. Assoc. J. 2014, 186, E649–E657. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Marfella, R.; Ciotola, M.; Di Palo, C.; Giugliano, F.; Giugliano, G.; D’Armiento, M.; D’Andrea, F.; Giugliano, D. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA 2004, 292, 1440–1446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richard, C.; Couture, P.; Desroches, S.; Charest, A.; Lamarche, B. Effect of the mediterranean diet with and without weight loss on cardiovascular risk factors in men with the metabolic syndrome. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Mendez, M.A.; Popkin, B.M.; Jakszyn, P.; Berenguer, A.; Tormo, M.J.; Sanchez, M.J.; Quiros, J.R.; Pera, G.; Navarro, C.; Martinez, C.; et al. Adherence to a mediterranean diet is associated with reduced 3-year incidence of obesity. J. Nutr. 2006, 136, 2934–2938. [Google Scholar] [PubMed]
- Departamento de Estadísticas e Información de Salud (DEIS). Indicadores Básicos de Salud, IBS. Chile 2014. Ministerio de Salud, Gobierno de Chile. Available online: http://www.deis.cl/wp-content/uploads/2015/04/IBS-2014.pdf (accessed on 7 August 2016).
- Ministerio de Salud, Gobierno de Chile. Encuesta Nacional de Salud ENS Chile 2009–2010. Ministerio de Salud, Gobierno de Chile. Available online: http://web.minsal.cl/portal/url/item/bcb03d7bc28b64dfe040010165012d23.pdf (accessed on 7 August 2016).
- Ministerio de Salud, Gobierno de Chile. Encuesta Nacional de Consumo Alimentario: Informe Fina. Ministerio de Salud, Gobierno de Chile. Available online: http://web.minsal.cl/sites/default/files/ENCA-INFORME_FINAL.pdf (accessed on 7 August 2016).
- Vio, F.; Albala, C.; Kain, J. Nutrition transition in chile revisited: Mid-term evaluation of obesity goals for the period 2000–2010. Public Health Nutr. 2008, 11, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Crovetto, M.; Uauy, R. Changes in household food and nutrient consumption in metropolitan santiago 1988–97 by income. Rev. Med. Chile 2010, 138, 1091–1108. [Google Scholar] [PubMed]
- Dussaillant, C.; Echeverría, G.; Villarroel, L.; Marín, P.P.; Rigotti, A. Una alimentación poco saludable se asocia a mayor prevalencia de síndrome metabólico en la población adulta chilena: Estudio de corte transversal en la encuesta nacional de salud 2009–2010. Nutr. Hosp. 2015, 32, 2098–2104. [Google Scholar] [PubMed]
- Rozowski, J.; Castillo, O.; Figari, N.; Garcia-Diaz, D.F.; Cruchet, S.; Weisstaub, G.; Perez-Bravo, F.; Gotteland, M. Nutritional status and biochemical markers of deficiency or excess of micronutrients in 4 to 14 year-old chilean children: A critical review. Nutr. Hosp. 2015, 32, 2916–2925. [Google Scholar]
- Urquiaga, I.; Echeverría, G.; Polic, G.; Castillo, O.; Liberona, Y.; Rozowski, J.; Perez, D.; Martinez, C.; Vasquez, L.; Strobel, P.; et al. Mediterranean food and diets, global resource for the control of metabolic syndrome and chronic diseases. World Rev. Nutr. Diet. 2008, 98, 150–173. [Google Scholar] [PubMed]
- Leighton, F.; Urquiaga, I. Chilenos ‘latinomediterráneos’. In Revista Universitaria—Pontificia Universidad Católica de Chile; Revista Universitaria: Santiago, Chile, 2005; pp. 36–40. [Google Scholar]
- Urquiaga, I.; Echeverría, G.; Dussaillant, C.; Rigotti, A. Origen, componentes y posibles mecanismos de acción de la dieta Mediterránea. Rev. Med. Chile 2016, 145, 85–95. [Google Scholar] [CrossRef] [PubMed]
- Leighton, F.; Polic, G.; Strobel, P.; Perez, D.; Martinez, C.; Vasquez, L.; Castillo, O.; Villarroel, L.; Echeverría, G.; Urquiaga, I.; et al. Health impact of mediterranean diets in food at work. Public Health Nutr. 2009, 12, 1635–1643. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Ruiz, A.; Garcia-Villanova, B.; Guerra Hernandez, E.J.; Amiano, P.; Azpiri, M.; Molina-Montes, E. Description of indexes based on the adherence to the Mediterranean dietary pattern: A review. Nutr. Hosp. 2015, 32, 1872–1884. [Google Scholar] [PubMed]
- Echeverria, G.; Urquiaga, I.; Concha, M.J.; Dussaillant, C.; Villarroel, L.; Velasco, N.; Leighton, F.; Rigotti, A. Diseño y aplicación de un índice de alimentación Mediterránea en Chile. Rev. Med. Chile. 2017, 144, 1531–1543. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Gonzalez, M.A.; Garcia-Arellano, A.; Toledo, E.; Salas-Salvado, J.; Buil-Cosiales, P.; Corella, D.; Covas, M.I.; Schroder, H.; Aros, F.; Gomez-Gracia, E.; et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: The predimed trial. PLoS ONE 2012, 7, e43134. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C.; et al. Diagnosis and management of the metabolic syndrome: An American heart association/national heart, lung, and blood institute scientific statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed]
- Team, R.C. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2014. [Google Scholar]
- Rosell, M.S.; Hellenius, M.L.; de Faire, U.H.; Johansson, G.K. Associations between diet and the metabolic syndrome vary with the validity of dietary intake data. Am. J. Clin. Nutr. 2003, 78, 84–90. [Google Scholar] [PubMed]
- Mila-Villarroel, R.; Bach-Faig, A.; Puig, J.; Puchal, A.; Farran, A.; Serra-Majem, L.; Carrasco, J.L. Comparison and evaluation of the reliability of indexes of adherence to the Mediterranean diet. Public Health Nutr. 2011, 14, 2338–2345. [Google Scholar] [CrossRef] [PubMed]
- Fisberg, M.; Kovalskys, I.; Gómez, G.; Rigotti, A.; Cortés, L.Y.; Herrera-Cuenca, M.; Yépez, M.C.; Pareja, R.G.; Guajardo, V.; Zimberg, I.Z.; et al. ELANS Study Group.Latin American Study of Nutrition and Health (ELANS): Rationale and study design. BMC Public Health 2016, 16, 93. [Google Scholar]
- Ferreccio, C.; Roa, J.C.; Bambs, C.; Vives, A.; Corvalán, A.H.; Cortés, S.; Foerster, C.; Acevedo, J.; Huidobro, A.; Passi, A.; et al. Study protocol for the Maule Cohort (MAUCO) of chronic diseases, Chile 2014–2024. BMC Public Health 2016, 16, 122. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Kastorini, C.M.; Panagiotakos, D.B.; Giugliano, D. Mediterranean diet and weight loss: Meta-analysis of randomized controlled trials. Metab. Syndr. Relat. Disord. 2011, 9, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Romaguera, D.; Norat, T.; Vergnaud, A.-C.; Mouw, T.; May, A.M.; Agudo, A.; Buckland, G.; Slimani, N.; Rinaldi, S.; Couto, E.; et al. Mediterranean dietary patterns and prospective weight change in participants of the EPIC-PANACEA project. Am. J. Clin. Nutr. 2010, 92, 912–921. [Google Scholar] [CrossRef] [PubMed]
- Nordmann, A.J.; Suter-Zimmermann, K.; Bucher, H.C.; Shai, I.; Tuttle, K.R.; Estruch, R.; Briel, M. Meta-analysis comparing Mediterranean to low-fat diets for modification of cardiovascular risk factors. Am. J. Med. 2011, 124, 841–851. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Fitó, M.; Chiva-Blanch, G.; Fiol, M.; Gómez-Gracia, E.; Arós, F.; Lapetra, J.; et al. Effect of a high-fat Mediterranean diet on bodyweight and waist circumference: A prespecified secondary outcomes analysis of the predimed randomised controlled trial. Lancet Diabetes Endocrinol. 2016, 4, 666–676. [Google Scholar] [CrossRef]
- Estruch, R. Anti-inflammatory effects of the Mediterranean diet: The experience of the predimed study. Proc. Nutr. Soc. 2010, 69, 333–340. [Google Scholar] [CrossRef] [PubMed]
- García-Fernández, E.; Rico-Cabanas, L.; Rosgaard, N.; Estruch, R.; Bach-Faig, A. Mediterranean diet and cardiodiabesity: A review. Nutrients 2014, 6, 3474–3500. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E.; Salas-Salvadó, J.; Covas, M.-I.; Corella, D.; Arós, F.; Gómez-Gracia, E.; Ruiz-Gutiérrez, V.; Fiol, M.; Lapetra, J.; et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013, 368, 1279–1290. [Google Scholar] [CrossRef] [PubMed]


| Score Item | Score Units | Scoring | |||
|---|---|---|---|---|---|
| 1.0 Point | 0.5 Points | 0 Points | |||
| 1 | Vegetables (excluding potatoes) | Servings per day | ≥3 | 1 to <3 | <1 |
| 2 | Legumes | Servings per week | >2 | 1 to 2 | <1 |
| 3 | Nuts | Servings per week | >2 | 1 to 2 | <1 |
| 4 | Fruits | Servings per day | ≥2 | 1 to <2 | <1 |
| 5 | Whole grain cereals | Servings per day | ≥2 | 1 to <2 | <1 |
| 6 | Lean meat and poultry | Servings per week | 5–8 | 1–4 | <1 or >8 |
| 7 | Fish and seafood | Servings per week | >2 | 1 to 2 | <1 |
| 8 | Fatty and processed meats | Servings per week | <1 | 1 to 2 | >2 |
| 9 | Whole fat dairy products, not fermented | Servings per day | <1 | 1 to <2 | ≥2 |
| 10 | Low fat and fermented dairy products | Servings per day | ≥2 | 1 to <2 | <1 |
| 11 | Olive oil | Teaspoons per day | ≥3 | 1 to <3 | <1 |
| 12 | Other healthy fats: Canola oil (C) and avocado (A) | C: consumption pattern A: units per week | regularly >3 | occasionally 0.5 to 3 | Never <0.5 |
| 13 | Sugar (S) and sugary snacks, juices, and soft drinks (SS) | S: Teaspoons per day SS: Serving per day | <4 non-daily | <4 daily | ≥4 daily |
| 14 | Wine | Glasses per day | 1 to 2 regularly, usually with meals | <1 or >2 regularly, usually with meals | Non-drinker or irregular and usually not with meals |
| Parameters | By Nutritional Status (n = 24,882) | By Metabolic Syndrome Presence (n = 4348) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Under & Normal Weight | Overweight & Obesity | p-Value | Total | Without MS | With MS | p-Value | |||
| Sex | ||||||||||
| Female | 68.5% | 78.5% | 59.9% | <0.001 | 70.6% | 72.2% | 64.4% | <0.001 | ||
| Male | 31.5% | 21.5% | 40.1% | 29.4% | 27.8% | 35.6% | ||||
| Age | ||||||||||
| 19–29 years old | 43.1% | 53.2% | 34.4% | <0.001 | 33.5% | 35.6% | 25.3% | <0.001 | ||
| 30–39 years old | 31.4% | 28.6% | 33.9% | 29.0% | 30.1% | 24.4% | ||||
| 40–49 years old | 14.9% | 11.0% | 18.2% | 17.8% | 17.1% | 20.8% | ||||
| 50–59 years old | 7.1% | 5.0% | 9.0% | 11.5% | 10.2% | 16.7% | ||||
| >60 years old | 3.5% | 2.2% | 4.6% | 8.2% | 7.0% | 12.9% | ||||
| Region of residence | ||||||||||
| Santiago metropolitan region | 57.5% | 59.2% | 56.0% | <0.001 | 58.1% | 58.8% | 55.1% | <0.001 | ||
| All other regions | 42.5% | 40.8% | 44.0% | 41.9% | 41.2% | 44.9% | ||||
| Educational levels | ||||||||||
| ≤12 years of school completed | 17.9% | 16.0% | 19.5% | <0.001 | 14.6% | 13.1% | 20.6% | <0.001 | ||
| >12 years of school completed | 82.1% | 84.0% | 80.5% | 85.4% | 86.9% | 79.4% | ||||
| Smoking status | ||||||||||
| Non-smoker | 62.1% | 64.6% | 60.1% | <0.001 | 70.3% | 70.9% | 67.7% | 0.004 | ||
| Moderate smoker | 28.0% | 27.3% | 28.6% | 21.4% | 21.5% | 21.0% | ||||
| Heavy Smoker | 9.9% | 8.1% | 11.4% | 8.3% | 7.6% | 11.2% | ||||
| Physical activity level | ||||||||||
| Low | 39.4% | 32.8% | 45.0% | <0.001 | 37.8% | 34.6% | 50.6% | <0.001 | ||
| Medium | 36.5% | 38.4% | 34.9% | 38.1% | 38.5% | 36.8% | ||||
| High | 24.1% | 28.8% | 20.1% | 24.1% | 26.9% | 12.6% | ||||
| BMI status | ||||||||||
| Underweight | 1.4% | 3.1% | 0.0% | <0.001 | 0.9% | 1.0% | 0.2% | <0.001 | ||
| Normal weight | 44.7% | 96.9% | 0.0% | 40.8% | 48.2% | 11.1% | ||||
| Overweight | 35.9% | 0.0% | 66.7% | 37.3% | 36.9% | 39.0% | ||||
| Obese | 17.9% | 0.0% | 33.3% | 21.0% | 13.8% | 49.7% | ||||
| Number of MetS components present | ||||||||||
| 0 components | 23.8% | 40.2% | 12.1% | <0.001 | 23.8% | 29.8% | 0.0% | <0.001 | ||
| 1–2 components | 56.2% | 54.4% | 57.5% | 56.2% | 70.2% | 0.0% | ||||
| 3–5 components | 20.0% | 5.5% | 30.4% | 20.0% | 0.0% | 100.0% | ||||
| Chilean-MDI scoring | ||||||||||
| Unhealthy/low adherence to Mediterranean diet (0–4.5 points) | 34.5% | 29.4% | 38.9% | <0.001 | 22.4% | 19.9% | 32.4% | <0.001 | ||
| Moderately healthy/moderate adherence to Mediterranean diet (5–8.5 points) | 57.0% | 60.4% | 54.1% | 61.3% | 62.4% | 56.7% | ||||
| Healthy/high adherence to Mediterranean diet (9–14 points) | 8.5% | 10.1% | 7.1% | 16.3% | 17.6% | 10.9% | ||||
| Food Groups | Intake Categories * | Statistical Model † | Abdominal Obesity | Blood Hypertension | High Blood Glucose | High Triglycerides | Low HDL-Cholesterol | Obesity/Overweight |
|---|---|---|---|---|---|---|---|---|
| Vegetables (excluding potatoes) | <3 portions/day vs. ≥3 portions/day (ref) | Model 1 | 1.38 (1.16–1.65) | 1.31 (1.09–1.56) | 1.26 (1.04–1.53) | 1.26 (1.15–1.37) | ||
| Model 2 | 1.21 (1.00–1.46) | |||||||
| Legumes | <2 portions/week vs. ≥2 portions/week (ref) | Model 1 | 1.51 (1.04–2.18) | 1.51 (1.27–1.80) | ||||
| Model 2 | 1.24 (1.04–1.48) | |||||||
| Nuts | <2 portions/week vs. ≥2 portions/week (ref) | Model 1 | 1.79 (1.45–2.21) | 1.34 (1.10–1.63) | 1.36 (1.10–1.69) | 1.28 (1.04–1.57) | 1.504 (1.36–1.67) | |
| Model 2 | 1.58 (1.27–1.96) | 1.35 (1.21–1.50) | ||||||
| Fruits | <2 portions/day vs. ≥2 portions/day (ref) | Model 1 | 1.30 (1.10–1.54) | 1.22 (1.12–1.32) | ||||
| Model 2 | ||||||||
| Whole grain cereals | <2 portions/day vs. ≥2 portions/day (ref) | Model 1 | 1.26 (1.07–1.49) | 1.18 (1.00–1.39) | 1.16 (1.08–1.25) | |||
| Model 2 | 1.11 (1.03–1.20) | |||||||
| Lean meat and poultry | <4 or>8 portions/week vs. 4–8 portions/week (ref) | Model 1 | ||||||
| Model 2 | 0.76 (0.61–0.93) | |||||||
| Fish and seafood | <1 portion/week vs. ≥1 portion/week (ref) | Model 1 | 1.25 (1.08–1.45) | 1.31 (1.13–1.52) | 1.22 (1.04–1.43) | 1.12 (1.05–1.20) | ||
| Model 2 | 1.12 (1.03–1.40) | |||||||
| Fatty and processed meats | ≥1 portion/week vs. <1 portion/week (ref) | Model 1 | 1.30 (1.12–1.50) | 1.41 (1.20–1.66) | 1.19 (1.02–1.39) | 1.47 (1.37–1.57) | ||
| Model 2 | 1.21 (1.03–1.44) | 1.37 (1.28–1.47) | ||||||
| Whole fat dairy products, not fermented | ≥1 portion/day vs. <1 portion/day (ref) | Model 1 | 1.34 (1.15–1.57) | 1.26 (1.08–1.47) | 1.52 (1.29–1.80) | 1.13 (1.06–1.21) | ||
| Model 2 | 1.296 (1.086–1.546) | |||||||
| Low fat and fermented dairy products | ≤1 portion/day vs. >1 portion/day (ref) | Model 1 | 1.33 (1.15–1.55) | 1.21 (1.05–1.41) | 1.38 (1.18–1.62) | 1.16 (1.09–1.24) | ||
| Model 2 | 1.19 (1.02–1.39) | 1.25 (1.06–1.48) | ||||||
| Olive oil and healthy fats (canola oil and avocado) | ≤3 tea-spoon/day vs. >3 tea-spoon/day (ref) | Model 1 | 1.43 (1.17–1.74) | 1.34 (1.01–1.77) | 1.29 (1.17–1.43) | |||
| Model 2 | 1.30 (1.06–1.59) | 1.12 (1.01–1.24) | ||||||
| Wine | Occasional or excessive vs. regular, moderate consumption (1–2 drinks/day) (ref) | Model 1 | 1.32 (1.17–1.49) | |||||
| Model 2 | 1.33 (1.01–1.76) | 1.27 (1.13–1.43) | ||||||
| Sugar | Excessive consumption vs. moderate consumption (ref) | Model 1 | 1.47 (1.27–1.71) | 1.36 (1.17–1.58) | 1.47 (1.25–1.72) | 1.32 (1.23–1.41) | ||
| Model 2 | 1.28 (1.09–1.50) | 1.24 (1.06–1.46) | 1.23 (1.04–1.47) | 1.15 (1.07–1.24) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Echeverría, G.; McGee, E.E.; Urquiaga, I.; Jiménez, P.; D’Acuña, S.; Villarroel, L.; Velasco, N.; Leighton, F.; Rigotti, A. Inverse Associations between a Locally Validated Mediterranean Diet Index, Overweight/Obesity, and Metabolic Syndrome in Chilean Adults. Nutrients 2017, 9, 862. https://doi.org/10.3390/nu9080862
Echeverría G, McGee EE, Urquiaga I, Jiménez P, D’Acuña S, Villarroel L, Velasco N, Leighton F, Rigotti A. Inverse Associations between a Locally Validated Mediterranean Diet Index, Overweight/Obesity, and Metabolic Syndrome in Chilean Adults. Nutrients. 2017; 9(8):862. https://doi.org/10.3390/nu9080862
Chicago/Turabian StyleEcheverría, Guadalupe, Emma E. McGee, Inés Urquiaga, Paulina Jiménez, Sonia D’Acuña, Luis Villarroel, Nicolás Velasco, Federico Leighton, and Attilio Rigotti. 2017. "Inverse Associations between a Locally Validated Mediterranean Diet Index, Overweight/Obesity, and Metabolic Syndrome in Chilean Adults" Nutrients 9, no. 8: 862. https://doi.org/10.3390/nu9080862





