Dietary Cholesterol in the Elderly Chinese Population: An Analysis of CNHS 2010–2012
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Dietary Data
2.3. Assessment of Dietary Cholesterol and Protein Intake
2.4. Statistical Analysis
3. Results
3.1. Subject Demographic Characteristics
3.2. Daily Cholesterol Intake Level
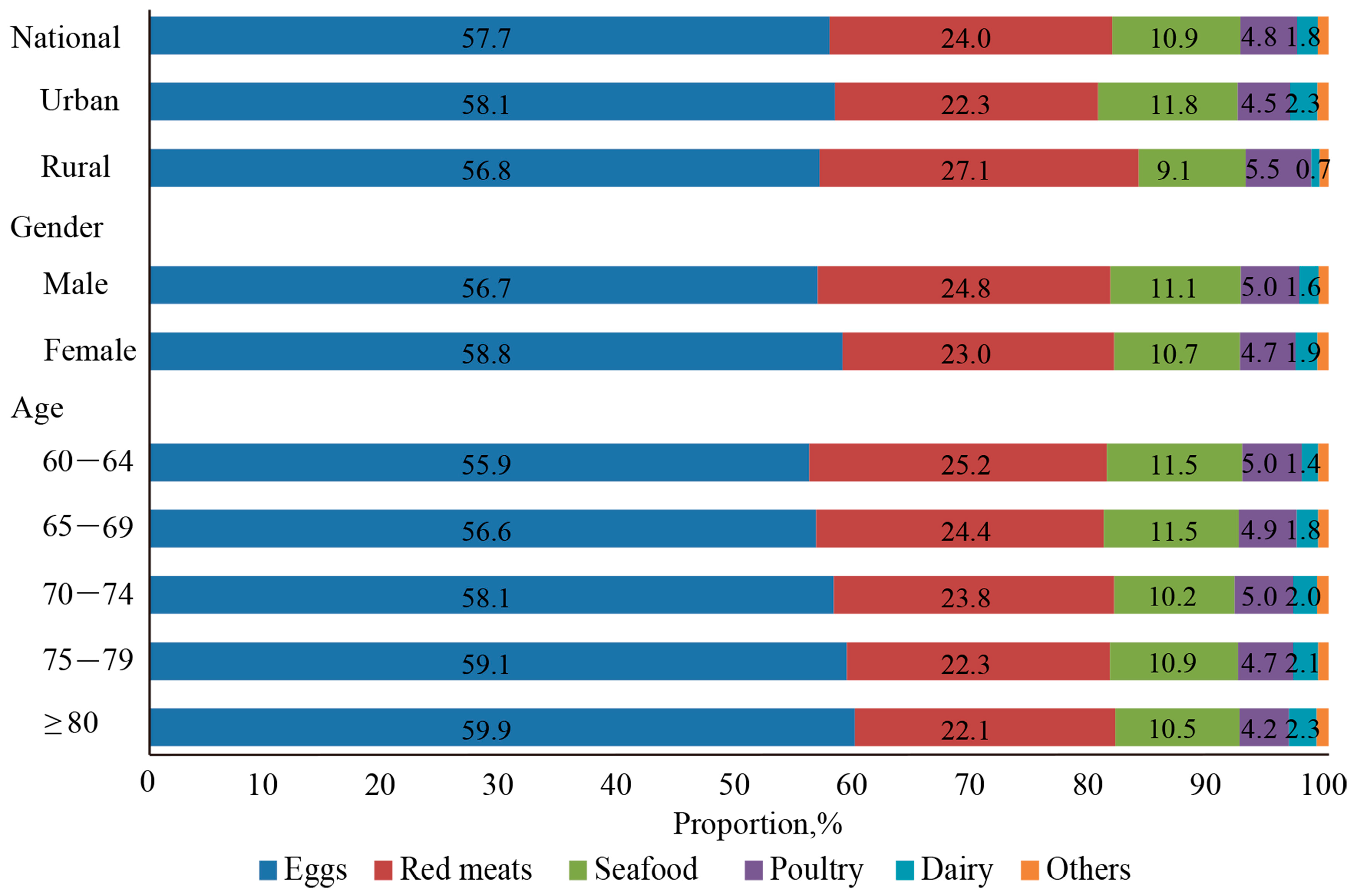
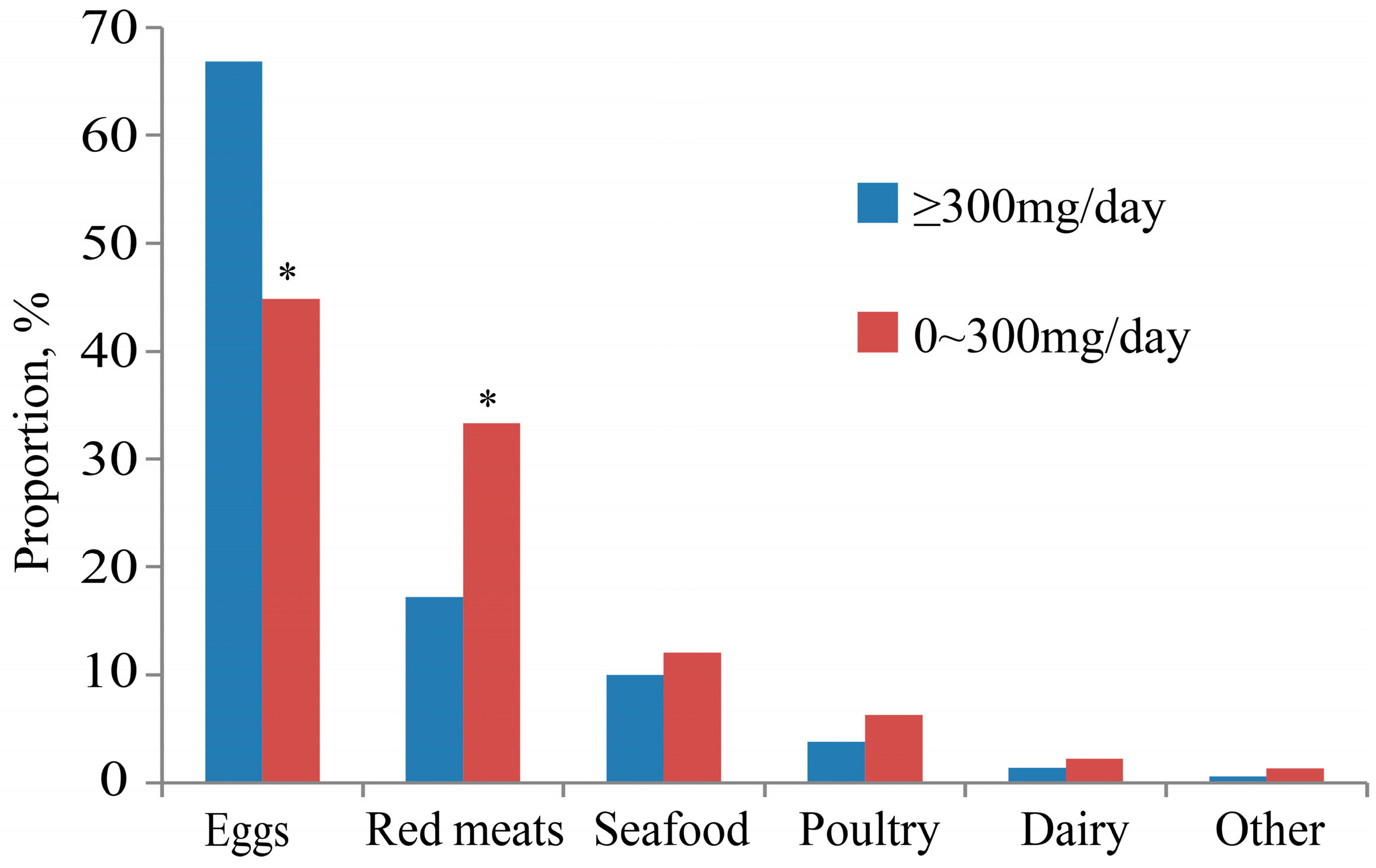
3.3. Food Sources of Dietary Cholesterol
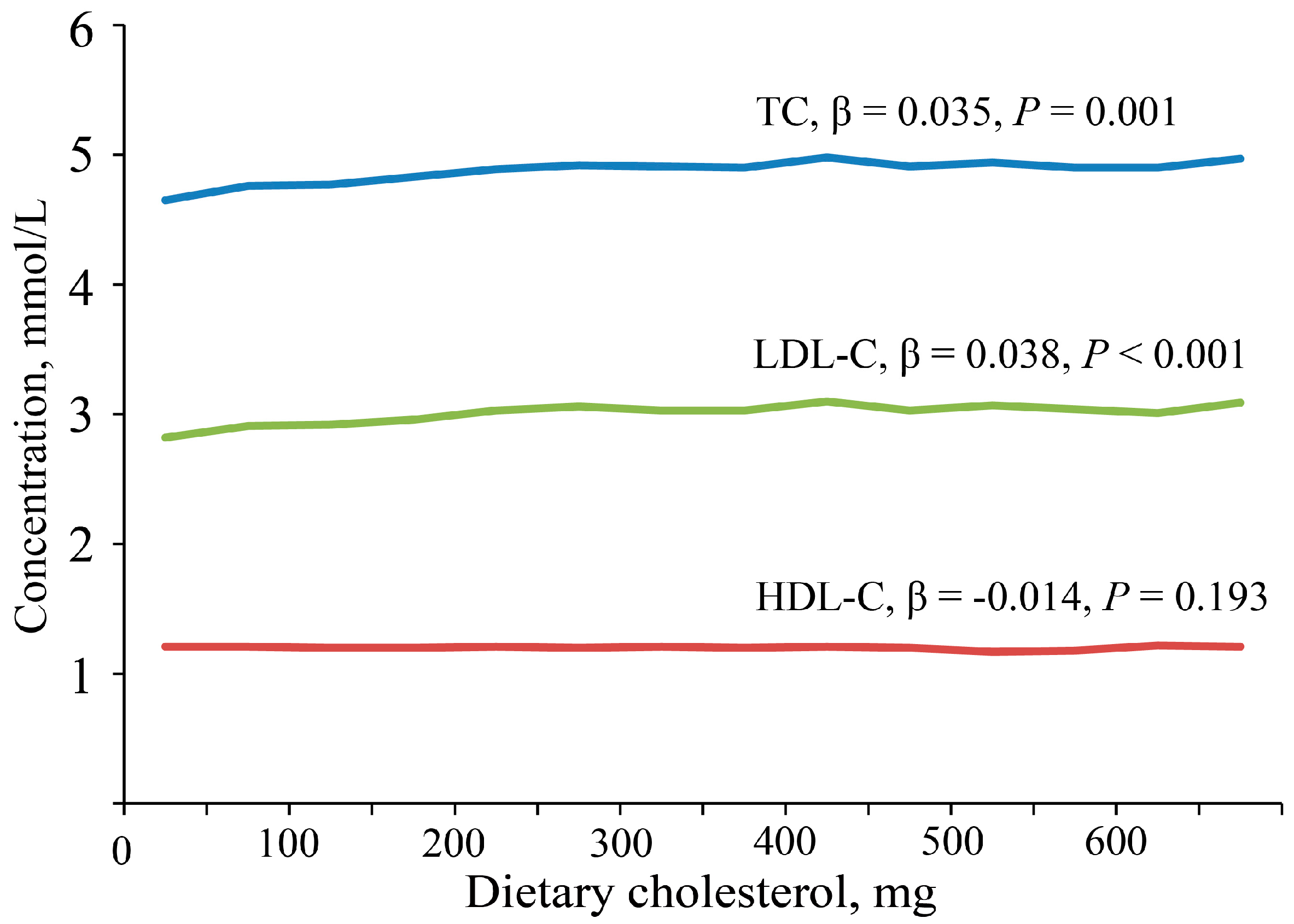
3.4. The Relationship between Dietary Cholesterol and Serum Cholesterol
3.5. The Relationship between Dietary Cholesterol and Protein Intake
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Fang, E.F.; Scheibye-Knudsen, M.; Jahn, H.J.; Li, J.; Ling, L.; Guo, H.; Zhu, X.; Preedy, V.; Lu, H.; Bohr, V.A.; et al. A research agenda for aging in China in the 21st century. Ageing Res. Rev. 2015, 24, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Jia, X.; Su, C.; Wang, Z.; Wang, H.; Jiang, H.; Zhang, B. Evaluation of dietary cholesterol intake in elderly Chinese: A longitudinal study from the China health and nutrition survey. BMJ Open 2016, 6, e011074. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Benjamin, E.J.; MacMahon, S. Prevention and control of cardiovascular disease in the rapidly changing economy of China. Circulation 2016, 133, 2545–2560. [Google Scholar] [CrossRef] [PubMed]
- Wu, F.; Guo, Y.; Kowal, P.; Jiang, Y.; Yu, M.; Li, X.; Zheng, Y.; Xu, J. Prevalence of major chronic conditions among older Chinese adults: The study on global ageing and adult health (SAGE) wave 1. PLoS ONE 2013, 8, e74176. [Google Scholar] [CrossRef] [PubMed]
- Berger, S.; Raman, G.; Vishwanathan, R.; Jacques, P.F.; Johnson, E.J. Dietary cholesterol and cardiovascular disease: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2015, 102, 276–294. [Google Scholar] [CrossRef] [PubMed]
- Silverman, M.G.; Ference, B.A.; Im, K.; Wiviott, S.D.; Giugliano, R.P.; Grundy, S.M.; Braunwald, E.; Sabatine, M.S. Association between lowering LDL-C and cardiovascular risk reduction among different therapeutic interventions: A systematic review and meta-analysis. JAMA 2016, 316, 1289–1297. [Google Scholar] [CrossRef] [PubMed]
- Elmadfa, I.; Meyer, A.L. Animal proteins as important contributors to a healthy human diet. Annu. Rev. Anim. Biosci. 2017, 5, 111–131. [Google Scholar] [CrossRef] [PubMed]
- Paddon-Jones, D.; Campbell, W.W.; Jacques, P.F.; Kritchevsky, S.B.; Moore, L.L.; Rodriguez, N.R.; van Loon, L.J. Protein and healthy aging. Am. J. Clin. Nutr. 2015. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Protein and Amino Acid Requirements in Human Nutrition: Report of a Joint WHO/FAO/UNU Expert Consultation; WHO Press: Geneva, Switzerland, 2007. [Google Scholar]
- Bauer, J.; Biolo, G.; Cederholm, T.; Cesari, M.; Cruz-Jentoft, A.J.; Morley, J.E.; Phillips, S.; Sieber, C.; Stehle, P.; Teta, D.; et al. Evidence-based recommendations for optimal dietary protein intake in older people: A position paper from the prot-age study group. J. Am. Med. Dir. Assoc. 2013, 14, 542–559. [Google Scholar] [CrossRef] [PubMed]
- Deutz, N.E.; Bauer, J.M.; Barazzoni, R.; Biolo, G.; Boirie, Y.; Bosy-Westphal, A.; Cederholm, T.; Cruz-Jentoft, A.; Krznaric, Z.; Nair, K.S.; et al. Protein intake and exercise for optimal muscle function with aging: Recommendations from the espen expert group. Clin. Nutr. 2014, 33, 929–936. [Google Scholar] [CrossRef] [PubMed]
- Rizzoli, R.; Stevenson, J.C.; Bauer, J.M.; van Loon, L.J.; Walrand, S.; Kanis, J.A.; Cooper, C.; Brandi, M.L.; Diez-Perez, A.; Reginster, J.Y.; et al. The role of dietary protein and vitamin D in maintaining musculoskeletal health in postmenopausal women: A consensus statement from the European society for clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Maturitas 2014, 79, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Chinese Nutrition Society. Chinese Dietary Reference Intakes (2013); Science Press: Beijing, China, 2014; pp. 106–108. ISBN 978-7-03-041401-4. [Google Scholar]
- Van Horn, L.; Carson, J.A.; Appel, L.J.; Burke, L.E.; Economos, C.; Karmally, W.; Lancaster, K.; Lichtenstein, A.H.; Johnson, R.K.; Thomas, R.J.; et al. Recommended dietary pattern to achieve adherence to the American Heart Association/American College of Cardiology (AHA/ACC) guidelines: A scientific statement from the American Heart Association. Circulation 2016, 134, e505–e529. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.L.; Wang, Y. Report on Chinese Residents’ Chronic Diseases and Nutrition; Peking University Medical Press: Beijing, China, 2016; ISBN 978-7-5659-1460-7. [Google Scholar]
- Song, P.K.; Li, H.; Man, Q.Q.; Jia, S.S.; Li, L.X.; Zhang, J. Trends in determinants of hypercholesterolemia among Chinese adults between 2002 and 2012: Results from the national nutrition survey. Nutrients 2017, 9, 279. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Fahimi, S.; Lim, S.; Andrews, K.G.; Engell, R.E.; Powles, J.; Ezzati, M.; Mozaffarian, D.; et al. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys. BMJ 2014, 348, g2272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bian, S.; Gao, Y.; Zhang, M.; Wang, X.; Liu, W.; Zhang, D.; Huang, G. Dietary nutrient intake and metabolic syndrome risk in Chinese adults: A case-control study. Nutr. J. 2013, 12, 106. [Google Scholar] [CrossRef] [PubMed]
- Yin, R.; Pan, S.; Chen, H.; Yang, H.; Wu, H.; Chen, Y.; Wu, J.; Huang, F.; Li, M.; Li, M. Diet, alcohol consumption, and serum lipid levels of the middle-aged and elderly in the Guangxi Bai Ku Yao and Han populations. Alcohol 2008, 42, 219–229. [Google Scholar]
- Wu, S.J.; Chang, Y.H.; Wei, I.L.; Kao, M.D.; Lin, Y.C.; Pan, W.H. Intake levels and major food sources of energy and nutrients in the Taiwanese elderly. Asia Pac. J. Clin. Nutr. 2005, 14, 211–220. [Google Scholar] [PubMed]
- Grundy, S.M. Does dietary cholesterol matter? Curr. Atheroscler. Rep. 2016, 18, 68. [Google Scholar] [CrossRef] [PubMed]
- Linseisen, J.; Welch, A.A.; Ocke, M.; Amiano, P.; Agnoli, C.; Ferrari, P.; Sonestedt, E.; Chajes, V.; Bueno-de-Mesquita, H.B.; Kaaks, R.; et al. Dietary fat intake in the European prospective investigation into cancer and nutrition: Results from the 24-h dietary recalls. Eur. J. Clin. Nutr. 2009, 63 (Suppl. 4), S61–S80. [Google Scholar] [CrossRef] [PubMed]
- Lecerf, J.M.; de Lorgeril, M. Dietary cholesterol: From physiology to cardiovascular risk. Br. J. Nutr. 2011, 106, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Rong, Y.; Chen, L.; Zhu, T.; Song, Y.; Yu, M.; Shan, Z.; Sands, A.; Hu, F.B.; Liu, L. Egg consumption and risk of coronary heart disease and stroke: Dose-response meta-analysis of prospective cohort studies. BMJ 2013, 346, e8539. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, F.B.; Stampfer, M.J.; Rimm, E.B.; Manson, J.E.; Ascherio, A.; Colditz, G.A.; Rosner, B.A.; Spiegelman, D.; Speizer, F.E.; Sacks, F.M.; et al. A prospective study of egg consumption and risk of cardiovascular disease in men and women. JAMA 1999, 281, 1387–1394. [Google Scholar] [CrossRef] [PubMed]
- Farvid, M.S.; Malekshah, A.F.; Pourshams, A.; Poustchi, H.; Sepanlou, S.G.; Sharafkhah, M.; Khoshnia, M.; Farvid, M.; Abnet, C.C.; Kamangar, F.; et al. Dietary protein sources and all-cause and cause-specific mortality: The golestan cohort study in Iran. Am. J. Prev. Med. 2017, 52, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Houston, D.K.; Ding, J.; Lee, J.S.; Garcia, M.; Kanaya, A.M.; Tylavsky, F.A.; Newman, A.B.; Visser, M.; Kritchevsky, S.B.; Health, A.B.C.S. Dietary fat and cholesterol and risk of cardiovascular disease in older adults: The Health ABC Study. Nutr. Metab. Cardiovasc. Dis. 2011, 21, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Djousse, L.; Kamineni, A.; Nelson, T.L.; Carnethon, M.; Mozaffarian, D.; Siscovick, D.; Mukamal, K.J. Egg consumption and risk of type 2 diabetes in older adults. Am. J. Clin. Nutr. 2010, 92, 422–427. [Google Scholar] [CrossRef] [PubMed]
- Weggemans, R.M.; Zock, P.L.; Katan, M.B. Dietary cholesterol from eggs increases the ratio of total cholesterol to high-density lipoprotein cholesterol in humans: A meta-analysis. Am. J. Clin. Nutr. 2001, 73, 885–891. [Google Scholar] [PubMed]
- Branch of Non-communicable Chronic Disease Prevention & Control, Chinese Preventive Medicine Association; Branch of Nutrition and Non-communicable Chronic Disease Prevention & Control, Chinese Nutrition Society; Chinese Association of Cardiovascular Health. Scientific statement on the correct understanding of cholesterol. Zhonghua Yu Fang Yi Xue Za Zhi 2016, 50, 936–937. [Google Scholar]
- Zhu, J.R.; Gao, R.L. Guidelines on prevention and treatment of blood lipid abnormality in Chinese adults (2016). Chin. Circ. J. 2016, 31, 17. [Google Scholar]
- Shi, Z.; Yuan, B.; Zhao, D.; Taylor, A.W.; Lin, J.; Watts, G.F. Familial hypercholesterolemia in China: Prevalence and evidence of underdetection and undertreatment in a community population. Int. J. Cardiol. 2014, 174, 834–836. [Google Scholar] [CrossRef] [PubMed]
- Bauer, J.M.; Diekmann, R. Protein and older persons. Clin. Geriatr. Med. 2015, 31, 327–338. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.S.; Lay, S.; Yu, H.N.; Shen, S.R. Dietary guidelines for Chinese residents (2016): Comments and comparisons. J. Zhejiang Univ. Sci. B 2016, 17, 649–656. [Google Scholar] [CrossRef] [PubMed]
| Nation (n = 16,594) | Urban (n = 9095) | Rural (n = 7499) | |
|---|---|---|---|
| Age, year | 69.9 (69.8–70.1) | 70.0 (69.8–70.2) | 69.9 (69.7–70.1) * |
| Male, % | 49.0 (48.2–49.8) | 48.4 (47.4–48.4) | 49.8 (48.6–50.9) |
| BMI, kg/m2 | 23.7 (23.7–23.8) | 24.4 (24.4–24.5) | 23.0 (22.9–23.1) * |
| Energy, kcal | 1826.1 (1816.2–1836.0) | 1728.0 (1715.3–1740.6) | 1928.6 (1913.1–1944.0) * |
| Total protein, g | 54.8 (54.5–55.2) | 56.5 (56.0–57.0) | 53.0 (52.6–53.5) * |
| High-quality protein, g | 21.2 (21.0–21.5) | 26.0 (25.6–26.4) | 16.2 (15.8–16.6) * |
| Protein intake per kilogram BW, g | 0.95 (0.95–0.96) | 0.94 (0.93, 0.95) | 0.97 (0.96, 0.98) * |
| High-quality protein percentage, % | 35.3 (35.0, 35.6) | 43.0 (42.6, 43.4) | 27.2 (26.8, 27.7) * |
| Fat, g | 65.8 (65.2–66.3) | 69.1 (68.3–69.8) | 62.3 (61.5–63.1) * |
| Carbohydrate, g | 255.2 (253.6–256.8) | 221.7 (219.8–223.5) | 290.1 (287.5–292.8) * |
| TC, mmol/L | 4.8 (4.8–4.9) | 4.9 (4.9–5.0) | 4.7 (4.7–4.8) * |
| LDL-C, mmol/L | 3.0 (3.0–3.0) | 3.1 (3.0–3.1) | 2.9 (2.9–2.9) * |
| HDL-C, mmol/L | 1.2 (1.2–1.2) | 1.2 (1.2–1.2) | 1.2 (1.2–1.2) * |
| Dietary Cholesterol | ||||||
|---|---|---|---|---|---|---|
| Nation (n = 16,594) | Urban (n = 9095) | Rural (n = 7499) | ||||
| mg | mg/1000 kcal | mg | mg/1000 kcal | mg | mg/1000 kcal | |
| Total | 217.4 (214.5–220.3) | 125.4 (123.7–127.1) | 264.0 (259.8–268.2) | 158.9 (156.4–161.5) | 168.8 (164.8–172.8) * | 90.3 (88.1–92.6) * |
| Gender | ||||||
| Male | 230.4 (226.1–234.7) | 122.1 (119.8–124.4) | 279.5 (273.4–285.6) | 155.0 (151.6–158.3) | 179.7 (173.8–185.5) | 88.1 (85.2–91.1) |
| Female | 205.0 (201.0–209.1) | 128.6 (126.0–131.2) | 249.3 (243.5–255.0) | 162.7 (158.9–166.5) | 158.2 (152.8–163.7) | 92.5 (89.1–95.9) |
| p-values for difference ‡ | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Age | ||||||
| 60–64 | 226.2 (221.3–231.1) | 121.3 (118.7–124.0) | 275.9 (268.8–283.1) | 156.5 (152.5–160.5) | 174.6 (168.4–180.8) | 84.8 (81.7–88.0) |
| 65–69 | 220.5 (214.7–226.3) | 122.8 (119.6–126.1) | 267.2 (259.0–275.3) | 156.7 (151.9–161.4) | 173.5 (165.6–181.5) | 88.8 (84.7–92.9) |
| 70–74 | 210.5 (203.7–217.2) | 122.3 (118.4–126.2) | 253.0 (244.1–261.8) | 152.6 (147.4–157.9) | 165.6 (155.8–175.5) | 90.3 (84.9–95.7) |
| 75–79 | 207.0 (198.3–215.6) | 129.8 (124.3–135.4) | 253.7 (241.7–265.7) | 165.2 (157.2–173.2) | 156.7 (144.9–168.4) | 91.7 (84.9–98.6) |
| ≥80 | 209.8 (199.2–220.5) | 141.5 (134.4–148.6) | 254.2 (239.1–269.4) | 172.5 (162.6–180.8) | 161.5 (147.4–175.5) | 107.8 (98.3–117.2) |
| p-values for linear trend † | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| BMI | ||||||
| <18.5 | 188.3 (169.0–207.5) | 106.9 (96.5–117.3) | 243.1 (210.0–276.2) | 150.7 (130.7–170.8) | 165.6 (142.5–188.7) | 88.2 (77.1–100.4) |
| 18.5–24 | 211.4 (199.8–223.1) | 119.7 (113.1–126.2) | 264.1 (245.7–282.6) | 157.7 (146.9–168.5) | 168.1 (153.7–182.5) | 88.4 (80.7–96.1) |
| ≥24 | 227.3 (215.3–239.2) | 130.7 (124.0–137.5) | 265.3 (249.5–281.1) | 157.9 (148.4–166.5) | 168.8 (152.8–184.7) | 89.6 (81.1–98.0) |
| p-values for linear trend † | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| 0 mg | 0–300 mg | ≥300 mg | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Total | 1068 | 6.8 (6.6–7.0) | 10,978 | 66.6 (66.2–67.0) | 4548 | 26.6 (26.2–26.9) |
| Region | ||||||
| Urban | 233 | 2.6 (2.5–2.7) | 5621 | 62.0 (61.6–62.4) | 3241 | 35.5 (35.2–35.8) |
| Rural | 835 | 11.2 (11.0–11.4) | 5357 | 71.5 (71.1–71.9) | 1307 | 17.3 (17.1–17.5) |
| p-values for difference † | <0.001 | <0.001 | <0.001 | |||
| Gender | ||||||
| Male | 518 | 6.7 (6.6–6.8) | 5186 | 64.1 (63.7–64.5) | 2431 | 29.2 (28.9–29.5) |
| Female | 550 | 6.9 (6.7–7.1) | 5792 | 69.0 (68.6–69.4) | 2117 | 24.1 (23.8–24.4) |
| p-values for difference † | <0.001 | <0.001 | <0.001 | |||
| Age | ||||||
| 60–64 | 356 | 6.0 (5.9–6.1) | 3935 | 65.8 (65.5–66.1) | 1679 | 28.1 (27.9–28.3) |
| 65–69 | 283 | 6.9 (6.8–7.0) | 2837 | 65.9 (65.6–66.2) | 1207 | 27.2 (27.0–27.4) |
| 70–74 | 214 | 7.3 (7.2–7.4) | 2147 | 67.5 (67.2–67.8) | 856 | 25.2 (25.0–25.4) |
| 75–79 | 139 | 7.9 (7.8–8.0) | 1263 | 67.1 (66.9–67.3) | 498 | 25.0 (24.9–25.4) |
| ≥80 | 76 | 6.7 (6.8–6.9) | 796 | 68.2 (67.9–68.5) | 308 | 25.2 (25.0–25.4) |
| p-values for trend ‡ | <0.001 | <0.001 | <0.001 | |||
| Q1 (n = 4145) | Q2 (n = 4152) | Q3 (n = 4149) | Q4 (n = 4148) | p-Values | |
|---|---|---|---|---|---|
| TC, mmol/L | 4.7 (4.4–4.8) | 4.8 (4.8–4.9) a | 4.9 (4.9–4.9) a,b | 4.9 (4.9–5.0) a,b,c | <0.001 |
| LDL-C, mmol/L | 2.9 (2.9–2.9) | 3.0 (2.9–3.0) a | 3.1 (3.0–3.1) a,b | 3.1 (3.1–3.1) a,b,c | <0.001 |
| HDL-C, mmol/L | 1.2 (1.2–1.2) | 1.2 (1.2–1.2) | 1.2 (1.2–1.2) | 1.2 (1.2–1.2) | 0.633 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pang, S.-J.; Jia, S.-S.; Man, Q.-Q.; Song, S.; Li, Y.-Q.; Song, P.-K.; Zhao, W.-H.; Zhang, J. Dietary Cholesterol in the Elderly Chinese Population: An Analysis of CNHS 2010–2012. Nutrients 2017, 9, 934. https://doi.org/10.3390/nu9090934
Pang S-J, Jia S-S, Man Q-Q, Song S, Li Y-Q, Song P-K, Zhao W-H, Zhang J. Dietary Cholesterol in the Elderly Chinese Population: An Analysis of CNHS 2010–2012. Nutrients. 2017; 9(9):934. https://doi.org/10.3390/nu9090934
Chicago/Turabian StylePang, Shao-Jie, Shan-Shan Jia, Qing-Qing Man, Shuang Song, Yu-Qian Li, Peng-Kun Song, Wen-Hua Zhao, and Jian Zhang. 2017. "Dietary Cholesterol in the Elderly Chinese Population: An Analysis of CNHS 2010–2012" Nutrients 9, no. 9: 934. https://doi.org/10.3390/nu9090934







