Disruption of the Putative Vascular Leak Peptide Sequence in the Stabilized Ricin Vaccine Candidate RTA1-33/44-198
Abstract
:Abbreviations
| BALF | bronchoalveolar lavage fluid |
| CD | circular dichroism |
| DTNB | 5,5'-dithiobis(2-nitrobenzoic acid) |
| i.m. | intramuscular |
| i.p. | intraperitoneal |
| MES | 2-(N-morpholino)ethanesulfonic acid |
| PBS | phosphate buffered saline |
| PEG | polyethylene glycol |
| RIP | ribosome inactivating protein |
| rmsd | root-mean-square deviation |
| RiVax | ricin A-chain variant containing the V76M and Y80A mutations |
| RTA | ricin toxin A-chain |
| RTA1-33/44-198 | ricin toxin A-chain containing residues 1–198 and a deletion of residues 34–43, also known as RVEc |
| RTB | ricin toxin B-chain |
| SDS-PAGE | sodium dodecyl sulfate polyacrylamide gel electrophoresis |
| Tm | melting temperature |
| TTD | time to death |
| TTDD | time to disease score drop |
| TTWG | time to body weight gain |
| VLP | vascular leak peptide |
| VLS | vascular leak syndrome |
1. Introduction
2. Results
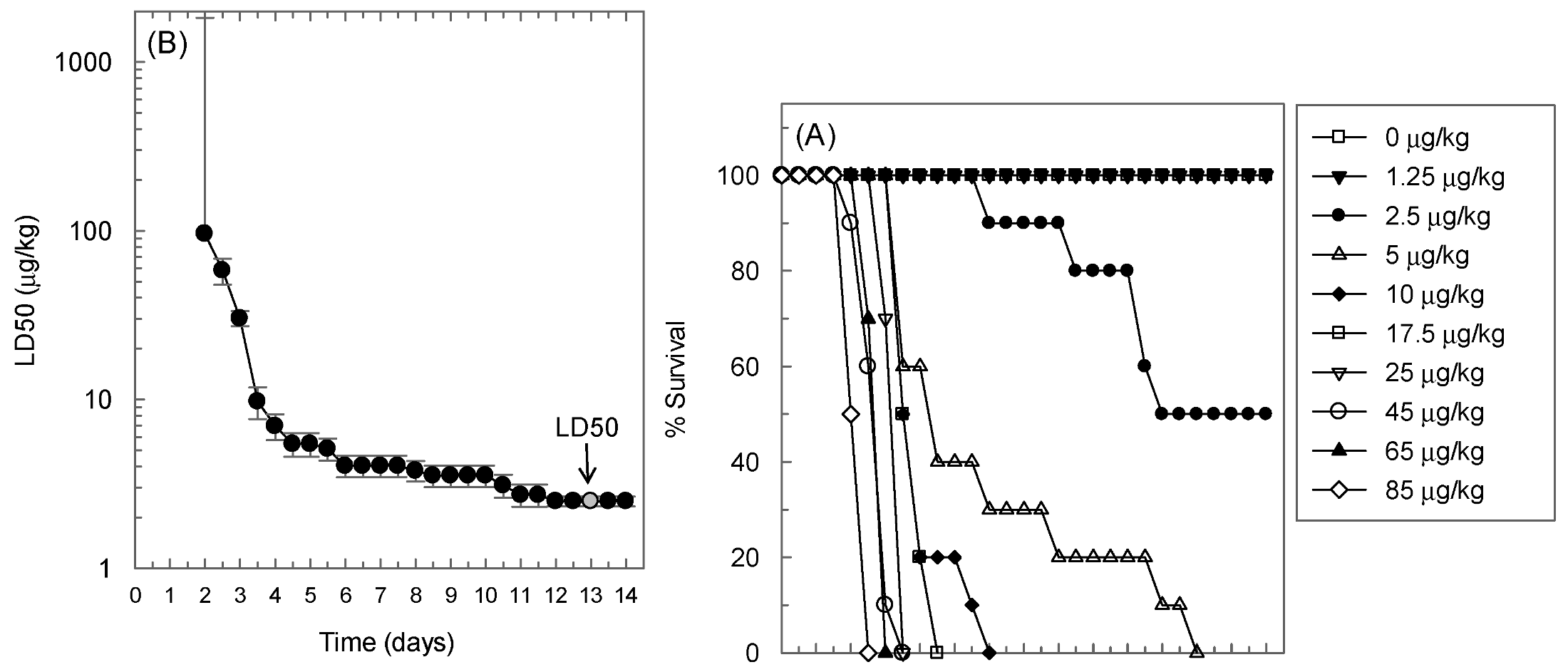
2.1. Determination of the LD50 of Ricin in BALB/c Mice in the Intranasal Challenge Model
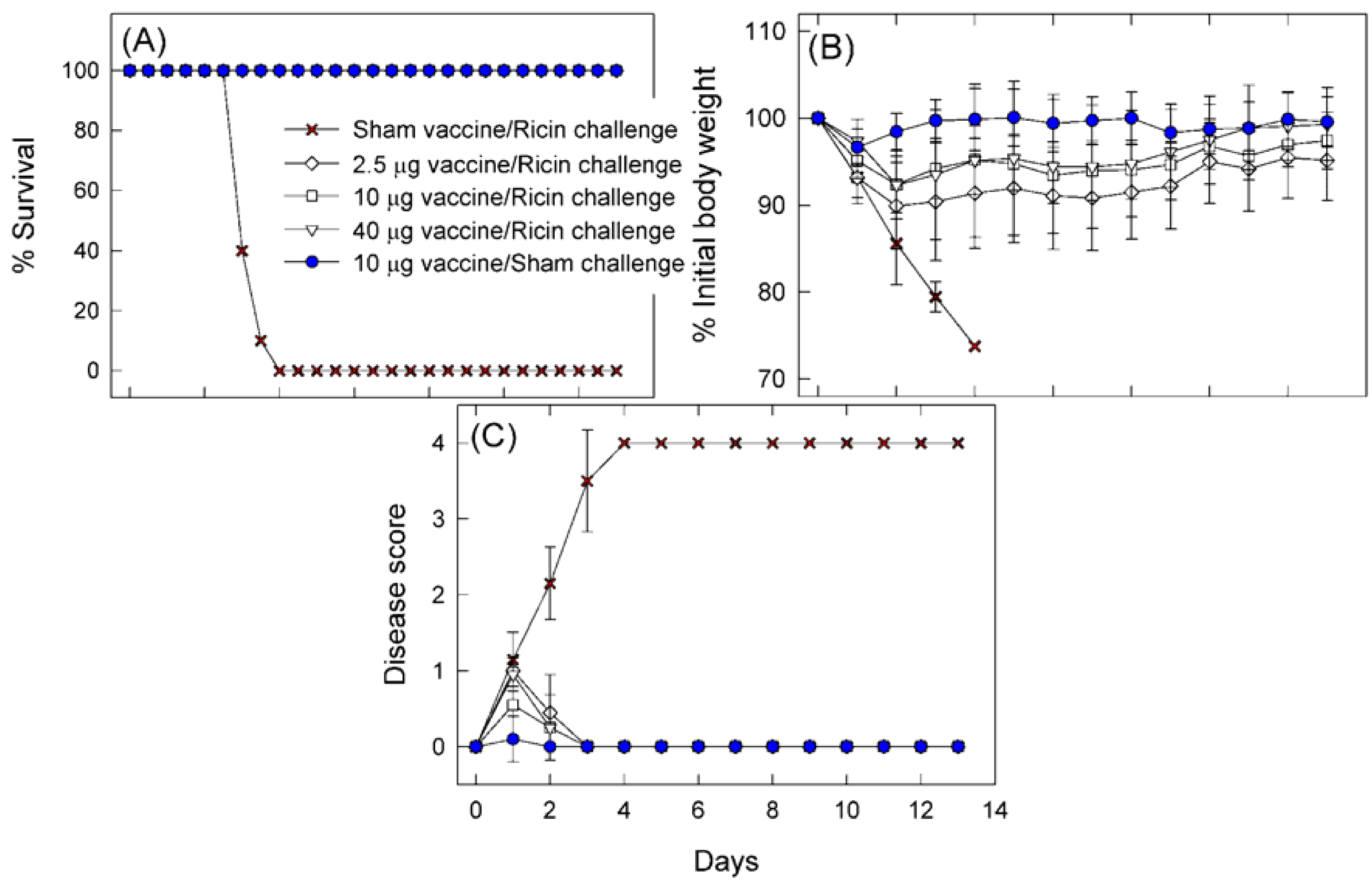
2.2. Protective Immunity Obtained with RTA1-33/44-198

| Post-challenge time point | Vaccine dose (μg/mouse) | Significant deviation of group mean values from the values of the 10 μg vaccine dose group b | |||
|---|---|---|---|---|---|
| BALF protein concentration (μg/mL) | Blood glucose concentration (mg%) | % Initial body weight (g) | Disease scores (points) | ||
| Day 1 | 2.5 | NT | NT | Down by 1.8 (p = 0.032) | Up by 0.4 (p < 0.001) |
| 40 | NT | NT | Up by 2.3 (p = 0.003) | Up by 0.4 (p = 0.004) | |
| Day 2 | 2.5 | - | - | - | - |
| 40 | Down by 253 (p = 0.043) | Up by 61 (p = 0.001) | - | - | |
| Day 3–12 | 2.5 | NT | NT | - | - |
| 40 | NT | NT | - | - | |
| Day 13 | 2.5 | - | - | - | - |
| 40 | - | Up by 45 (p = 0.001) | - | - | |
2.3. Intranasal Challenge with Immunogen in Place of Ricin
| Endpoint a | Time point b | PBS challenge c | RTA1-33/44-198 challenge in immune naïve mice d | RTA1-33/44-198 challenge in immune mice e | Significance of naïve/immune difference (p) | ||
|---|---|---|---|---|---|---|---|
| Mean ± S.D. | Mean ± S.D. | Significance of difference from PBS challenge (p) | Mean ± S.D. | Significance of difference from PBS challenge (p) | |||
| BALF protein (μg/mL) | Day 2 | 154 ± 10 | 178 ± 37 | 0.212 | 274 ± 66 | <0.001 | <0.001 |
| Day 13 | 139 ± 19 | 106 ± 14 | <0.001 | 193 ± 39 | 0.005 | <0.001 | |
| Blood glucose (mg%) | Day 2 | 184 ± 20 | 190 ± 20 | 0.573 | 228 ± 13 | <0.001 | <0.001 |
| Day 13 | 178 ± 14 | 194 ± 14 | 0.026 | 218 ± 25 | <0.001 | 0.023 | |
| % initial weight | Day 1 | 96.7 ± 2.1 | 97.2 ± 1.8 | 0.399 | 94.6 ± 3.0 | 0.016 | 0.002 |
| Day 2 | 98.4 ± 2.2 | 100.1 ± 2.6 | 0.038 | 98.7 ± 3.0 | 0.746 | 0.137 | |
| Day 13 | 99.6 ± 3.0 | 105.1 ± 3.0 | <0.001 | 102.9 ± 2.6 | 0.017 | 0.088 | |
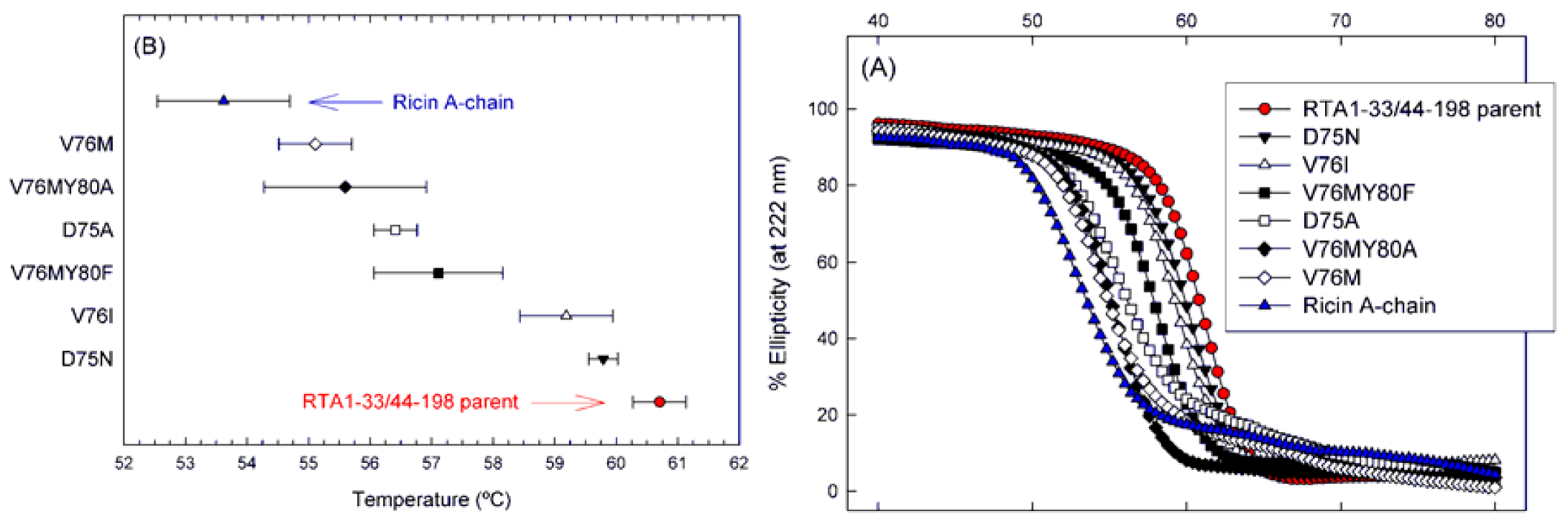
2.4. Vascular Leak Peptide Mutant Derivatives of RTA1-33/44-198 and Their Thermal Stabilities
| Ricin vaccine immunogen | Immunogen | Sequencing 1 | Solubility/Purity 2 | Number of free Cys 3 | Apparent Tm | Disruption of VLP? |
|---|---|---|---|---|---|---|
| Purification Method No. 1 | ||||||
| RTA | - | Yes | S+/>95% | - | 53.5 ± 0.74 | No |
| RTA1-33/44-198 | - | Yes | S+/>95% | - | 61.0 ± 0.23 | No |
| RTA1-33/44-198 | D75N | Yes | S+/>95% | - | 60.0 ± 0.05 | Yes |
| RTA1-33/44-198 | V76I | Yes | S+/>95% | - | 59.8 ± 0.17 | Yes |
| RTA1-33/44-198 | D75A | Yes | S+/>95% | - | 56.6 ± 0.10 | Yes |
| RTA1-33/44-198 | V76M | Yes | S+/>95% | - | 55.4 ± 0.42 | Yes |
| Purification Method No. 2 | ||||||
| RTA1-33/44-198 | - | Yes | S+/>95% | 0.97 ± 0.03 | 57.9 ± 0.03 | No |
| Substitutions that Increase Apparent Tm | ||||||
| RTA1-33/44-198 | R48C/T77C | Yes | S+/>95% | 1.00 ± 0.08 | 62.9 ± 0.22 | No |
| RTA1-33/44-198 | V49C/E99C | Yes | S+/>95% | 0.96 ± 0.05 | 62.9 ± 0.21 | No |
| RTA1-33/44-198 | R48C/T77C/D75N | Yes | S+/>95% | 1.04 ± 0.02 | 63.2 ± 0.26 | Yes |
| RTA1-33/44-198 | V49C/E99C/V76I | Yes | S+/>95% | 0.99 ± 0.03 | 62.6 ± 0.21 | Yes |
| RTA1-33/44-198 | V49C/E99C/D75N | Yes | S+/>95% | 1.10 ± 0.06 | 62.2 ± 0.13 | Yes |
| RTA1-33/44-198 | R48C/T77C/V76I | Yes | S+/>95% | 1.89 ± 0.03 | 59.3 ± 0.60 | Yes |
2.5. Protective Immunity Obtained with the VLP Mutants of RTA1-33/44-198
| Post-challenge time point | Vaccine b | Significant alteration of group mean values from the group mean values of the animals immunized with RTA1-33/44-198 c | ||
|---|---|---|---|---|
| BALF protein concentration (μg/mL) | Blood glucose concentration (mg%) | % Initial body weight (g) | ||
| Day 1 | D75A | NT | NT | - |
| D75N | NT | NT | - | |
| V76I | NT | NT | - | |
| V76M | NT | NT | - | |
| V76M/Y80A | NT | NT | - | |
| V76M/Y80F | NT | NT | - | |
| Day 2 | D75A | Up by 541 (p = 0.001) | - | Down by 4.7 (p = 0.001) |
| D75N | - | - | - | |
| V76I | - | Up by 61 (p = 0.002) | - | |
| V76M | - | Up by 45 (p = 0.012) | - | |
| V76M/Y80A | - | - | - | |
| V76M/Y80F | - | Up by 37 (p = 0.036) | - | |
| Day 13 | D75A | Down by 93 (p < 0.001) | - | - |
| D75N | - | - | - | |
| V76I | - | - | - | |
| V76M | - | - | - | |
| V76M/Y80A | - | - | - | |
| V76M/Y80F | - | - | - | |
2.6. Effects of the D75N and V76I Mutations on the Thermal Stability of RTA1-33/44-198 R48C/T77C and RTA1-33/44-198 V49C/E99C

2.7. Effect of the D75N Mutation on the Structure of RTA1-33/44-198 R48C/T77C
| RTA1-33/44-198 R48C/T77C/D65N (PDB 4IMV) | |
|---|---|
| Space group | I222 |
| Unit Cell Dimensions (Å) | a = 51.6, b = 72.3, c = 94.7 |
| Unit Cell Angles (°) | α = 90, β = 90, γ = 90 |
| Wavelength (Å) | 1.54 |
| Resolution Range (Å) a | 57.5–2.25 (2.31–2.25) |
| Unique Reflections | 8640 (860) |
| Rint | 0.073 (0.285) |
| I/σI | 13.0 (3.6) |
| Completeness | 99.1 (91.6) |
| Redundancy | 6.9 (3.8) |
| Refinement Statistics | |
| Resolution (Å) | 47.35–2.25 |
| No. of reflections | 8233 |
| Rfactor b | 0.216 |
| Rfree c | 0.242(5%) |
| Number of Atoms | |
| Protein | 1318 |
| Solvent | 79 |
| Other | 4 |
| Average B-factors (Å2) | |
| Protein | 22.2 |
| Solvent | 29 |
| R.m.s.d. from ideal geometry | |
| Bond lengths (Å) | 0.015 |
| Bond angles (degrees) | 1.37 |
| Ramachandran plot | |
| Most favored regions (%) | 95.70% |
| Additional allowed regions (%) | 4.30% |
| Generously allowed regions (%) | 0.00% |
| Disallowed regions (%) | 0.00% |
 ; c Rfree for test set and size of test set as % total reflections in parentheses.
; c Rfree for test set and size of test set as % total reflections in parentheses.
3. Discussion
4. Materials and Methods
4.1. Chemicals, Reagent Kits
4.2. Mutagenesis and Protein Purifications
4.3. Circular Dichroism
4.4. Mice and Vaccinations
4.5. Intranasal Ricin Challenge
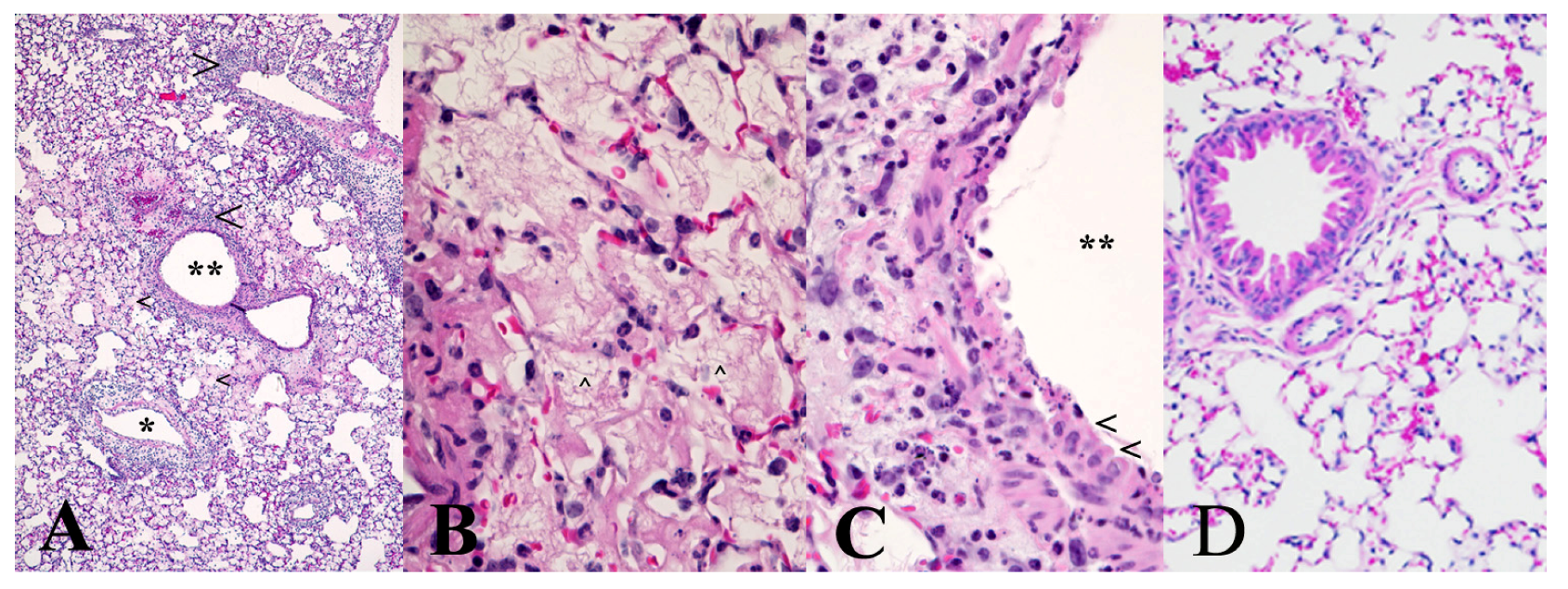
4.6. Survival, Body Weight and Disease Sign Observations, Blood Glucose and Bronchoalveolar Lavage Fluid Protein Concentration Determinations, Lung Histopathology
4.7. Statistical Analysis
4.8. Crystallization of RTA1-33/44-198 R48C/T77C/D75N Disulfide Variant
Acknowledgements
Supplementary Files
References
- Audi, J.; Belson, M.; Patel, M.; Schier, J.; Osterloh, J. Ricin poisoning: A comprehensive review. JAMA 2005, 294, 2342–2351. [Google Scholar] [CrossRef]
- Griffiths, G.D.; Phillips, G.J.; Holley, J. Inhalation toxicology of ricin preparations: Animal models, prophylactic and therapeutic approaches to protection. Inhal. Toxicol. 2007, 19, 873–887. [Google Scholar] [CrossRef]
- Spivak, L.; Hendrickson, R.G. Ricin. Crit. Care Clin. 2005, 21, 815–824. [Google Scholar] [CrossRef]
- Marsden, C.J.; Smith, D.C.; Roberts, L.M.; Lord, J.M. Ricin: Current understanding and prospects for an antiricin vaccine. Expert Rev. Vaccines 2005, 4, 229–237. [Google Scholar] [CrossRef]
- Smallshaw, J.E.; Firan, A.; Fulmer, J.R.; Ruback, S.L.; Ghetie, V.; Vitetta, E.S. A novel recombinant vaccine which protects mice against ricin intoxication. Vaccine 2002, 20, 3422–3427. [Google Scholar] [CrossRef]
- Smallshaw, J.E.; Richardson, J.A.; Pincus, S.; Schindler, J.; Vitetta, E.S. Preclinical toxicity and efficacy testing of RiVax, a recombinant protein vaccine against ricin. Vaccine 2005, 23, 4775–4784. [Google Scholar] [CrossRef]
- Smallshaw, J.E.; Richardson, J.A.; Vitetta, E.S. RiVax, a recombinant ricin subunit vaccine, protects mice against ricin delivered by gavage or aerosol. Vaccine 2007, 25, 7459–7469. [Google Scholar] [CrossRef]
- Vitetta, E.S.; Smallshaw, J.E.; Schindler, J. A pilot phase IB clinical trial of an alhydrogel-adsorbed recombinant ricin vaccine (RiVax). Clin. Vaccine Immunol. 2012, 103, 2268–2273. [Google Scholar]
- Baluna, R.; Rizo, J.; Gordon, B.E.; Ghetie, V.; Vitetta, E.S. Evidence for a structural motif in toxins and interleukin-2 that may be responsible for binding to endothelial cells and initiating vascular leak syndrome. Proc. Natl. Acad. Sci. USA 1999, 96, 3957–3962. [Google Scholar] [CrossRef]
- Vitetta, E.S.; Smallshaw, J.E.; Coleman, E.; Jafri, H.; Foster, C.; Munford, R.; Schindler, J. A pilot clinical trial of a recombinant ricin vaccine in normal humans. Proc. Natl. Acad. Sci. USA 2006, 103, 2268–2273. [Google Scholar]
- Vitetta, E.S. Immunotoxins and vascular leak syndrome. Cancer J. 2000, 6, S218–S224. [Google Scholar]
- Reisler, R.B.; Smith, L.A. The need for continued development of ricin countermeasures. Adv. Prev. Med. 2012, 2012, 149737–149740. [Google Scholar]
- Olson, M.A.; Carra, J.H.; Roxas-Duncan, V.; Wannemacher, R.W.; Smith, L.A.; Millard, C.B. Finding a new vaccine in the ricin protein fold. Protein Eng. Des. Sel. 2004, 17, 391–397. [Google Scholar] [CrossRef]
- McHugh, C.A.; Tammariello, R.F.; Millard, C.B.; Carra, J.H. Improved stability of a protein vaccine through elimination of a partially unfolded state. Protein Sci. 2004, 13, 2736–2743. [Google Scholar]
- Compton, J.R.; Legler, P.M.; Clingan, B.V.; Olson, M.A.; Millard, C.B. Introduction of a disulfide bond leads to stabilization and crystallization of a ricin immunogen. Proteins 2011, 79, 1048–1060. [Google Scholar] [CrossRef]
- Matyas, G.R.; Alving, C.R. Protective prophylactic immunity against intranasal ricin challenge induced by liposomal ricin A subunit. Vaccine Res. 1996, 5, 163–172. [Google Scholar]
- Pratt, T.S.; Pincus, S.H.; Hale, M.L.; Moreira, A.L.; Roy, C.J.; Tchou-Wong, K.M. Oropharyngeal aspiration of ricin as a lung challenge model for evaluation of the therapeutic index of antibodies against ricin A-chain for post-exposure treatment. Exp. Lung Res. 2007, 33, 459–481. [Google Scholar] [CrossRef]
- Roy, C.J.; Hale, M.; Hartings, J.M.; Pitt, L.; Duniho, S. Impact of inhalation exposure modality and particle size on the respiratory deposition of ricin in BALB/c mice. Inhal. Toxicol. 2003, 15, 619–638. [Google Scholar]
- Pincus, S.H.; Eng, L.; Cooke, C.L.; Maddaloni, M. Identification of hypoglycemia in mice as a surrogate marker of ricin toxicosis. Comp. Med. 2002, 52, 530–533. [Google Scholar]
- Niesen, F.H.; Berglund, H.; Vedadi, M. The use of differential scanning fluorimetry to detect ligand interactions that promote protein stability. Nat. Protoc. 2007, 2, 2212–2221. [Google Scholar] [CrossRef]
- Castelletti, D.; Fracasso, G.; Righetti, S.; Tridente, G.; Schnell, R.; Engert, A.; Colombatti, M. A dominant linear B-cell epitope of ricin A-chain is the target of a neutralizing antibody response in Hodgkin’s lymphoma patients treated with an anti-CD25 immunotoxin. Clin. Exp. Immunol. 2004, 136, 365–372. [Google Scholar] [CrossRef]
- Vogel, P.; Rivera, V.R.; Pitt, M.L.; Poli, M.A. Comparison of the pulmonary distribution and efficacy of antibodies given to mice by intratracheal instillation or aerosol inhalation. Lab Anim. Sci. 1996, 46, 516–523. [Google Scholar]
- Griffiths, G.D.; Phillips, G.J.; Bailey, S.C. Comparison of the quality of protection elicited by toxoid and peptide liposomal vaccine formulations against ricin as assessed by markers of inflammation. Vaccine 1999, 17, 2562–2568. [Google Scholar] [CrossRef]
- Balint, G.A. Ultrastructural study of liver cell damage induced by ricin. Exp. Toxicol. Pathol. 2000, 52, 413–417. [Google Scholar] [CrossRef]
- Olsnes, S. Ricin and ricinus agglutinin, toxic lectins from castor bean. Methods Enzymol. 1978, 50, 330–335. [Google Scholar] [CrossRef]
- Navaza, J. Implementation of molecular replacement in AMoRe. Acta Crystallogr. D 2001, 57, 1367–1372. [Google Scholar] [CrossRef]
- Brunger, A.T.; Adams, P.D.; Clore, G.M.; DeLano, W.L.; Gros, P.; Grosse-Kunstleve, R.W.; Jiang, J.S.; Kuszewski, J.; Nilges, M.; Pannu, N.S.; et al. Crystallography & NMR system: A new software suite for macromolecular structure determination. Acta Crystallogr. D 1998, 54, 905–921. [Google Scholar] [CrossRef]
- Potterton, E.; McNicholas, S.; Krissinel, E.; Cowtan, K.; Noble, M. The CCP4 molecular-graphics project. Acta Crystallogr. D 2002, 58, 1955–1957. [Google Scholar] [CrossRef]
- Emsley, P.; Cowtan, K. Coot: Model-building tools for molecular graphics. Acta Crystallogr. D 2004, 60, 2126–2132. [Google Scholar] [CrossRef]
- Ho, M.-C.; Sturm, M.B.; Almo, S.C.; Schramm, V.L. Transition state analogues in structures of ricin and saporin ribosome-inactivating proteins. Proc. Natl. Acad. Sci. USA 2009, 106, 20276–20281. [Google Scholar] [CrossRef]
- Olson, M.A.; Cuff, L. Free energy determinants of binding the rRNA substrate and small ligands to ricin A-Chain. Biophys. J. 1999, 76, 28–39. [Google Scholar] [CrossRef]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Janosi, L.; Compton, J.R.; Legler, P.M.; Steele, K.E.; Davis, J.M.; Matyas, G.R.; Millard, C.B. Disruption of the Putative Vascular Leak Peptide Sequence in the Stabilized Ricin Vaccine Candidate RTA1-33/44-198. Toxins 2013, 5, 224-248. https://doi.org/10.3390/toxins5020224
Janosi L, Compton JR, Legler PM, Steele KE, Davis JM, Matyas GR, Millard CB. Disruption of the Putative Vascular Leak Peptide Sequence in the Stabilized Ricin Vaccine Candidate RTA1-33/44-198. Toxins. 2013; 5(2):224-248. https://doi.org/10.3390/toxins5020224
Chicago/Turabian StyleJanosi, Laszlo, Jaimee R. Compton, Patricia M. Legler, Keith E. Steele, Jon M. Davis, Gary R. Matyas, and Charles B. Millard. 2013. "Disruption of the Putative Vascular Leak Peptide Sequence in the Stabilized Ricin Vaccine Candidate RTA1-33/44-198" Toxins 5, no. 2: 224-248. https://doi.org/10.3390/toxins5020224




