Self-Esteem and Academic Difficulties in Preadolescents and Adolescents Healed from Paediatric Leukaemia
Abstract
:1. Introduction
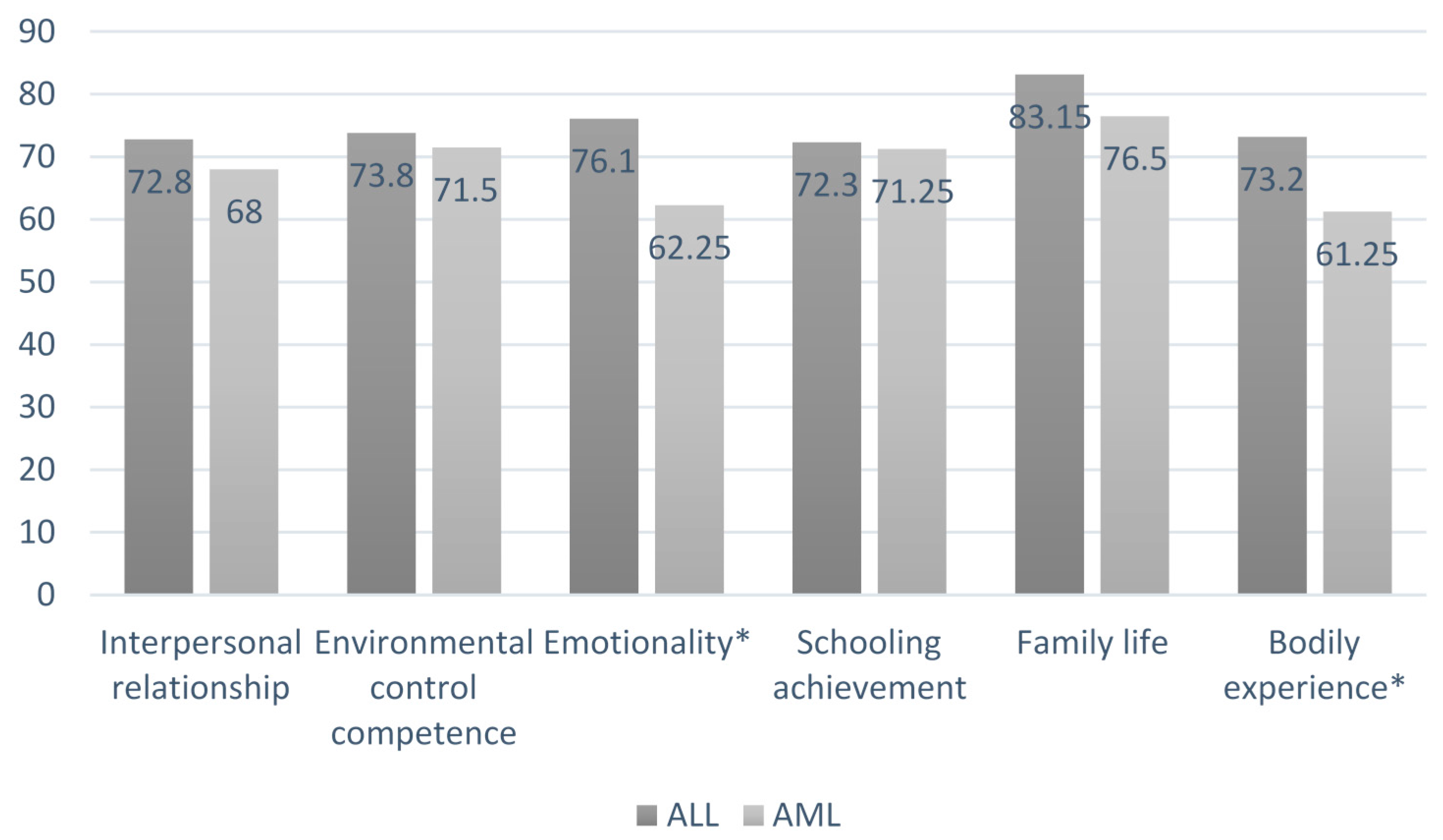
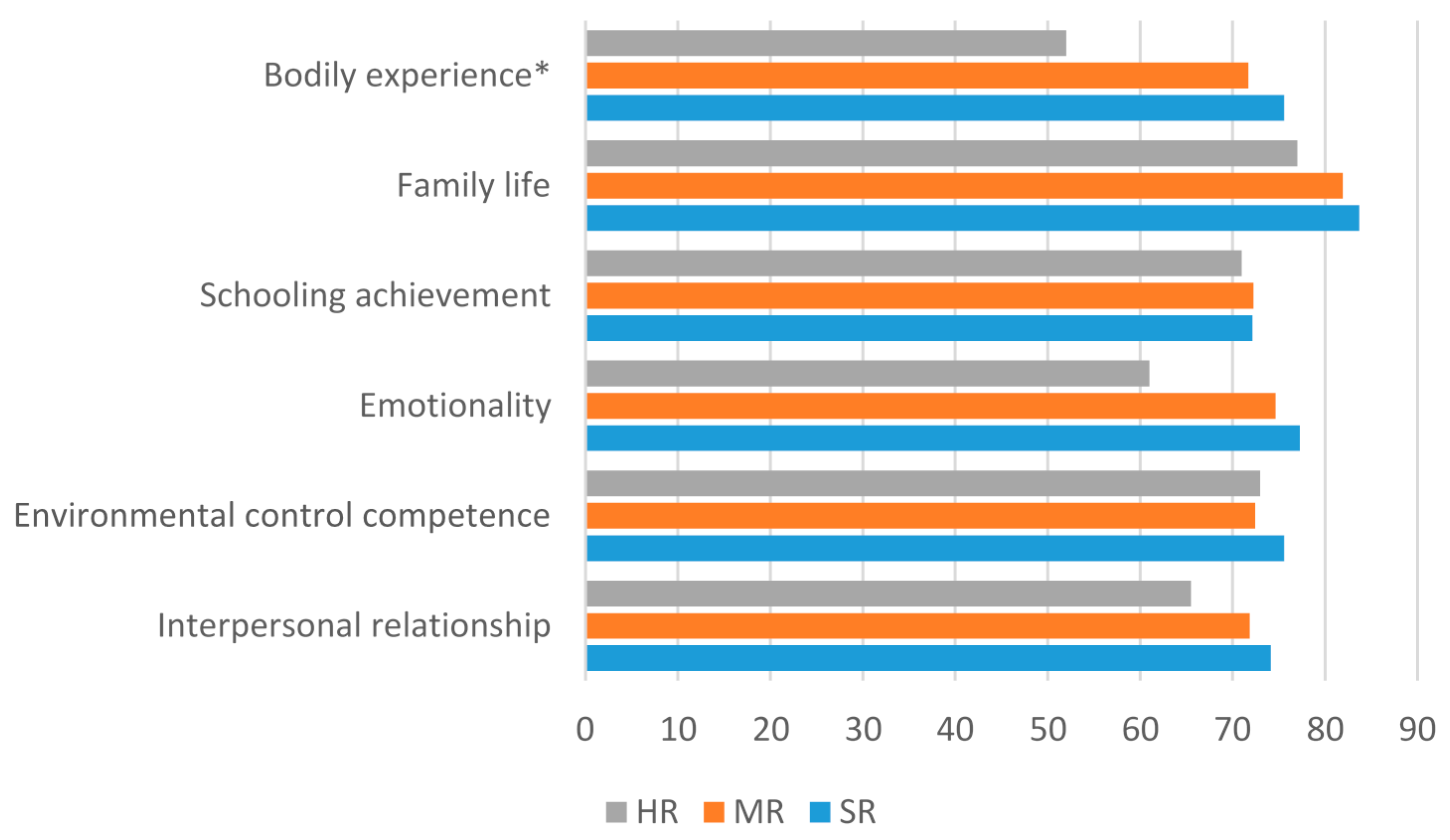
- We presumed that ex-patients with more aggressive therapy, including CRT (Acute Myeloid Leukaemia AML and ALL-HR), would report lower self-esteem scores, as suggested in the study of Hill et al. [35].
- We expected that females would report more self-esteem problems, according to the findings of a study on adolescents during cancer treatments [41].
2. Results
2.1. Self-Esteem Scoring in Preadolescents and Adolescents
2.2. Schooling Situation and Difficulties Reported by Parents
2.3. Associations between Self-Esteem Scoring and Socio-Demographic Variables
2.4. Associations between Self-Esteem Scoring and Illness Variables
3. Discussion
4. Materials and Methods
4.1. Participants
4.2. Procedure
4.3. Instruments
4.3.1. Multidimensional Self-Esteem Test
4.3.2. Socio Economic Status Questionnaire
4.3.3. Schooling Situation
4.4. Statistical Analysis
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Fusco, M.; Trama, A.; Buzzoni, C.; AIRTUM working group. Numeri come notizie. Epidemiol Prev. 2014, 38, 62. (In Italian) [Google Scholar] [PubMed]
- Kanellopoulos, A.; Hamre, H.M.; Dahl, A.A.; Fosså, S.D.; Ruud, E. Factors associated with poor quality of life in survivors of childhood acute lymphoblastic leukemia and lymphoma. Pediatr. Blood Cancer 2013, 60, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Zeltzer, L.K.; Recklitis, C.; Buchbinder, D.; Zebrack, B.; Casillas, J.; Tsao, J.C.; Krull, K. Psychological Status in Childhood Cancer Survivors: A Report From the Childhood Cancer Survivor Study. J. Clin. Oncol. 2009, 27, 2396–2404. [Google Scholar] [CrossRef] [PubMed]
- Gordijn, M.S.; Van Litsenburg, R.R.; Gemke, R.J.; Huisman, J.; Bierings, M.B.; Hoogerbrugge, P.M.; Kaspers, G.J. Sleep, fatigue, depression, and quality of life in survivors of childhood acute lymphoblastic leukemia. Pediatr. Blood Cancer 2013, 60, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Harila, M.J.; Salo, J.; Lanning, M.; Vilkkumaa, I.; Harila-Saari, A.H. High health-related quality of life among long-term survivors of childhood acute lymphoblastic leukemia. Pediatr. Blood Cancer 2010, 55, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Tremolada, M.; Bonichini, S.; Basso, G.; Pillon, M. Perceived social support and health related quality of life in AYA cancer survivors of childhood and controls. Psycho Oncol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Langer, T.; Martus, P.; Ottensmeier, H.; Hertzberg, H.; Beck, J.D.; Meier, W. CNS late-effects after ALL therapy in childhood. Part III: Neuropsychological performance in long-term survivors of childhood ALL: Impairments of concentration, attention, and memory. Med. Pediatr. Oncol. 2002, 38, 320–328. [Google Scholar] [CrossRef] [PubMed]
- Green, D.M.; Whitton, J.A.; Stovall, M.; Mertens, A.C.; Donaldson, S.S.; Ruymann, F.B.; Robison, L.L. Pregnancy outcome of female survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Am. J. Obs. Gynecol. 2002, 187, 1070–1080. [Google Scholar] [CrossRef] [PubMed]
- Kadan-Lottick, N.S.; Dinu, I.; Wasilewski-Masker, K.; Kaste, S.; Meacham, L.R.; Mahajan, A.; Sklar, C.A. Osteonecrosis in Adult Survivors of Childhood Cancer: A Report from the Childhood Cancer Survivor Study. J. Clin. Oncol. 2008, 26, 3038–3045. [Google Scholar] [CrossRef] [PubMed]
- Neglia, J.P.; Friedman, D.L.; Yasui, Y.; Mertens, A.C.; Hammond, S.; Stovall, M.; Robison, L.L. Second malignant neoplasms in five-year survivors of childhood cancer: Childhood cancer survivor study. J. Natl. Cancer Inst. 2001, 93, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Pang, J.W.Y.; Friedman, D.L.; Whitton, J.A.; Stovall, M.; Mertens, A.C.; Robison, L.L.; Weiss, N.S. Employment status among adult survivors in the Childhood Cancer Survivor Study. Pediatr. Blood Cancer 2008, 50, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Langeveld, N.E.; Stam, H.; Groothenhuis, M.A.; Last, B.E. Quality of life in young adult survivors of childhood cancer. Support Care Cancer 2002, 10, 579–600. [Google Scholar] [CrossRef] [PubMed]
- Alderfer, M.A.; Navsaria, N.; Kazak, A.E. Family Functioning and Posttraumatic Stress Disorder in Adolescent Survivors of Childhood Cancer. J. Fam. Psychol. 2009, 23, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Stuber, M.L.; Meeske, K.A.; Krull, K.R.; Leisenring, W.; Zeltzer, L. Prevalence and predictors of Posttraumatic Stress Disorder in adult survivors of childhood cancer: A report from the Childhood Cancer Survivor Study. Pediatrics 2010, 125, 1124–1134. [Google Scholar] [CrossRef] [PubMed]
- Madan-Swain, A.; Brown, R.T.; Foster, M.A.; Vega, R.; Byars, K.; Rodenberger, W.; Lambert, R. Identity in adolescent survivors of childhood cancer. J. Pediatr. Psychol. 2000, 25, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Van Dijk, E.M.; Van Dulmen-den Broeder, E.; Kaspers, G.J.L.; Van Dam, E.W.C.M.; Braam, K.I.; Huisman, J. Psychosexual functioning of childhood cancer survivors. Psycho-Oncology 2007, 17, 506–511. [Google Scholar] [CrossRef] [PubMed]
- Piers, E.V. Revised Manual for the Piers-Harris Children’s Self Concept Scale; Western Psychological Services: Los Angeles, CA, USA, 1984; ISBN-13 978-9991322698; ISBN-10 9991322698. [Google Scholar]
- Bracken, B.A. MSCS Multidimensional Self-Concept Scale; PRO-Ed: Austin, TX, USA, 1992; Italian version Mazzeo, R.; TMA Test di Valutazione dell’Autostima. Erickson: Trento, Italy, 2003. [Google Scholar]
- Evan, E.E.; Zeltzer, L.K. Psychosocial dimensions of cancer in adolescents and young adults. Cancer 2006, 107, 1663–1671. [Google Scholar] [CrossRef] [PubMed]
- Evans, S.E.; Radford, M. Current lifestyle of young adults treated for cancer in childhood. Arch. Dis. Child. 1995, 72, 423–426. [Google Scholar] [CrossRef] [PubMed]
- Buizer, A.I.; De Sonneville, L.M.; Van den Heuvel-Eibrink, M.M.; Veerman, A.J. Behavioral and educational limitations after chemotherapy for childhood acute lymphoblastic leukemia or Wilms tumor. Cancer 2006, 106, 2067–2075. [Google Scholar] [CrossRef] [PubMed]
- Nathan, P.C.; Patel, S.K.; Dilley, K.; Goldsby, R.; Harvey, J.; Jacobsen, C.; Okcu, M.F. Guidelines for identification of, advocacy for, and intervention in neurocognitive problems in survivors of childhood cancer: A report from the Children’s Oncology Group. Arch. Pediatr. Adolesc. Med. 2007, 161, 798–806. [Google Scholar] [CrossRef] [PubMed]
- Peterson, C.C.; Drotar, D. Family impact of neurodevelopmental late effects in survivors of pediatric cancer: Review of research, clinical evidence, and future directions. Clin. Child Psychol. Psychiatry 2006, 11, 349–366. [Google Scholar] [CrossRef] [PubMed]
- .Haupt, R.; Fears, T.R.; Robison, L.L.; Mills, J.L.; Nicholson, H.S.; Zeltzer, L.K.; Byrne, J. Educational attainment in long-term survivors of childhood acute lymphoblastic leukemia. JAMA 1994, 272, 1427–1432. [Google Scholar] [CrossRef] [PubMed]
- Hays, D.M.; Dolgin, M.; Steele, L.L.; Patenaude, A.F.; Hewett, K.D.; Ruymann, F.; Siegel, S.E. Educational achievement, employment and workplace experience of adult survivors of childhood cancer. Int. J. Pediatr. Hematol. Oncol. 1997, 4, 327–337. [Google Scholar]
- Mackie, E.; Hill, J.; Kondryn, H.; McNally, R. Adult psychosocial outcomes in long-term survivors of acute lymphoblastic leukaemia and Wilms’ tumour: A controlled study. Lancet 2000, 355, 1310–1314. [Google Scholar] [CrossRef]
- Reddick, W.E.; Shan, Z.Y.; Glass, J.O.; Helton, S.; Xiong, X.; Wu, S.; Pui, C.H. Smaller White-Matter Volumes Are Associated with Larger Deficits in Attention and Learning among Long-Term Survivors of Acute Lymphoblastic Leukemia. Cancer 2006, 106, 941–949. [Google Scholar] [CrossRef] [PubMed]
- Reddick, W.E.; Taghipour, D.J.; Glass, J.O.; Ashford, J.; Xiong, X.; Wu, S.; Conklin, H.M. Prognostic factors that increase the risk for reduced white matter volumes and deficits in attention and learning for survivors of childhood cancers. Pediatr. Blood Cancer 2014, 61, 1074–1079. [Google Scholar] [CrossRef] [PubMed]
- Van der Plas, E.; Schachar, R.J.; Hitzler, J.; Crosbie, J.; Guger, S.L.; Spiegler, B.J.; Nieman, B.J. Brain structure, working memory and response inhibition in childhood leukemia survivors. Brain Behav. 2017, 7, e00621. [Google Scholar] [CrossRef] [PubMed]
- Kunin-Batson, A.S.; Lu, X.; Balsamo, L.; Graber, K.; Devidas, M.; Hunger, S.P.; Kadan-Lottick, N.S. Prevalence and predictors of anxiety and depression after completion of chemotherapy for childhood acute lymphoblastic leukemia: A prospective longitudinal study. Cancer 2016, 122, 1608–1617. [Google Scholar] [CrossRef] [PubMed]
- Jacola, L.M.; Krull, K.M.; Pui, C.H.; Pei, D.; Cheng, C.; Reddick, W.E.; Conklin, H.M. Longitudinal Assessment of Neurocognitive Outcomes in Survivors of Childhood Acute Lymphoblastic Leukemia Treated on a Contemporary Chemotherapy Protocol. J. Clin. Oncol. 2016, 34, 1239–1247. [Google Scholar] [CrossRef] [PubMed]
- Challinor, J.; Miaskowski, C.; Moore, I.; Slaughter, R.; Franck, L. Review of research studies that evaluated the impact of treatment for childhood cancers on neurocognition and behavioral and social competence: Nursing implications. J. Soc. Pediatr. Nurs. 2000, 5, 57–74. [Google Scholar] [CrossRef] [PubMed]
- Seitzman, R.L.; Glover, D.A.; Meadows, A.T.; Mills, J.L.; Nicholson, H.S.; Robison, L.L.; Zeltzer, L.K. Self-concept in adult survivors of childhood acute lymphoblastic leukemia: A cooperative Children’s Cancer Group and National Institutes of Health study. Pediatr. Blood Cancer 2004, 42, 230–240. [Google Scholar] [CrossRef] [PubMed]
- Speechley, K.N.; Barrera, M.; Shaw, A.K.; Morrison, H.I.; Maunsell, E. Health-related quality of life among child and adolescent survivors of childhood cancer. J. Clin. Oncol. 2006, 24, 2536–2543. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.M.; Kornblith, A.B.; Hones, D.; Fereman, A.; Holland, J.F.; Glicksman, A.S.; Kung, F. A Comparative Study of the Long Term Psychosocial Functioning of Childhood Acute Lymphoblastic Leukemia Survivors Treated by Intrathecal Methotrexate with or without Cranial Radiation. Cancer 1998, 82, 208–218. [Google Scholar] [CrossRef]
- Erikson, E.H. Childhood and Society; Norton: New York, NY, USA, 1950; ISBN 039331068X. [Google Scholar]
- Freud, A. Opere; Bollati Boringhieri: Torino, Italy, 1985; Volume 3, pp. 1965–1975, EAN: 9788833901145. [Google Scholar]
- Kohut, H. The Analysis of the Self; International Universities Press: New York, NY, USA, 1971; ISBN-13 978-0226450124; ISBN-10 0226450120. [Google Scholar]
- Abell, S.C.; Richards, M.H. The relationship between body shape satisfaction and selfesteem: An investigation of gender and class differences. J. Youth Adolesc. 1996, 25, 691–704. [Google Scholar] [CrossRef]
- Pendley, J.S.; Dahlquist, L.M.; Dreyer, Z. Body image and psychosocial adjustment in adolescent cancer survivors. J. Pediatr. Psychol. 1997, 22, 29–43. [Google Scholar] [CrossRef] [PubMed]
- Mertens, A.C.; Brand, S.; Ness, K.K.; Li, Z. Health and well-being in adolescent survivors of early childhood cancer: A report from the Childhood Cancer Survivor Study. Psycho-Oncology 2014, 23, 266–275. [Google Scholar] [CrossRef] [PubMed]
- Maslow, A. Motivation and Personality; Harper: New York, NY, USA, 1954; ISBN-13: 978-0060419875; ISBN-10: 0060419873. [Google Scholar]
- Tremolada, M.; Bonichini, S.; Taverna, L.; Pillon, M.; Basso, G. I pazienti pediatrici che ritornano a scuola dopo aver terminato le terapie per leucemia raccontano la loro vita quotidiana e la loro esperienza di malattia. Paediatric patients cured for leukemia back to school: Analysis of narratives about daily life and illness experience. Psicol. Clin. Dello Svilupp. (In Italian).
- Taverna, L.; Tremolada, M.; Bonichini, S.; Basso, G.; Pillon, M. Adaptive functioning of Preschooler Children with Leukemia Post 1 Year of Therapies Compared with Sane Peers. Br. J. Educ. Soc. Behav. Sci. 2016, 18, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Shavelson, R.J.; Hubner, J.J.; Stanton, G.C. Self-concept: Validation of construct interpretations. Rev. Educ. Res. 1976, 46, 407–441. [Google Scholar] [CrossRef]
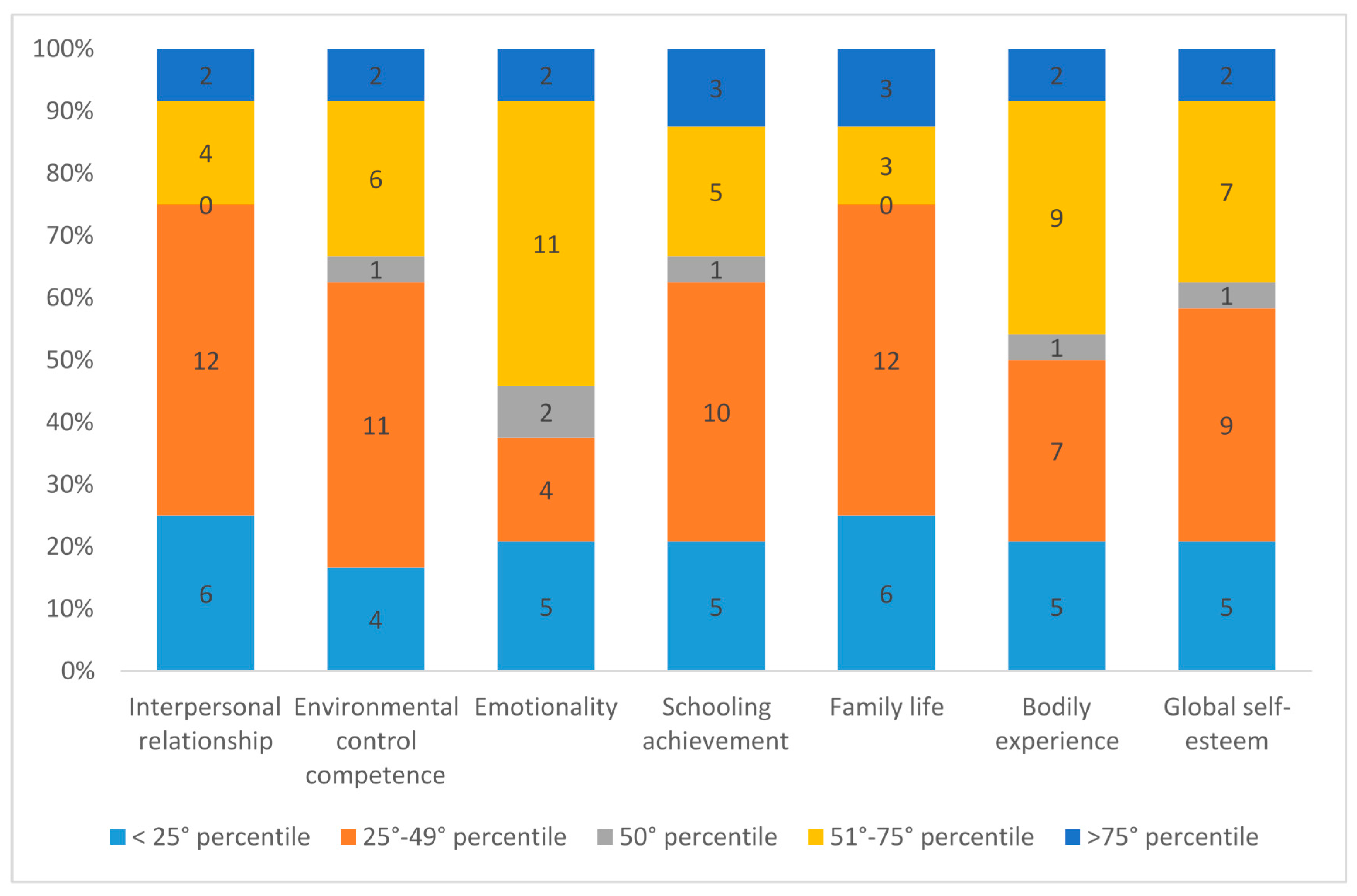
| Percentile Ranks | N | M | SD | Minimum | Maximum |
|---|---|---|---|---|---|
| Interpersonal relationship | 25 | 38.83 | 20.28 | 5 | 83 |
| Environmental control competence | 25 | 44.25 | 22.77 | 5 | 88 |
| Emotionality | 25 | 50.37 | 24.84 | 8 | 93 |
| Schooling achievement | 25 | 43.96 | 23.70 | 11 | 94 |
| Family life | 25 | 40.92 | 22.58 | 8 | 96 |
| Bodily experience | 25 | 45.17 | 22.83 | 4 | 87 |
| Global self-esteem | 25 | 42.71 | 22.09 | 11 | 91 |
| Interpersonal Relationship | Environmental Control Competence | Emotionality | Schooling Achievement | Family Life | |
|---|---|---|---|---|---|
| Environmental control competence | r = 0.33 | ||||
| p = 0.10 | |||||
| Emotionality | r = 0.622 ** | r = 0.66 ** | |||
| p = 0.001 | p = 0.001 | ||||
| Schooling achievement | r = 0.28 | r = 0.41 * | r = 0.41 * | ||
| p = 0.16 | p = 0.04 | p = 0.04 | |||
| Family life | r = 0.50 * | r = 0.12 | r = 0.51 ** | r = 0.37 | |
| p = 0.01 | p = 0.55 | p = 0.009 | p = 0.07 | ||
| Bodily experience | r = 0.50 * | r = 0.53** | r = 0.62 ** | r = 0.53 ** | r = 0.39 |
| p = 0.01 | p = 0.006 | p = 0.001 | p = 0.006 | p = 0.053 |
| Yes | No | ||||
|---|---|---|---|---|---|
| During his school career did he/she encounter any difficulties? | n = 11 | n =13 | |||
| During his school career did he/she repeat year/s? | n = 1 | n = 23 | |||
| During therapies did he/she participate in school activities at hospital? | n = 15 | n = 9 | |||
| Program agreed with the teachers of the school and equal to their peers: 28.6% | Program different from their peers: 21.4% | Program not agreed with the teachers of the school: 50% | |||
| During therapies did he/she had participated in school activities at home? | n = 16 | n = 8 | |||
| Program agreed with the teachers of the school and equal to their peers: 75% | Program different from their peers: 25% | ||||
| How long has the child started to go to school after the diagnosis communication? | 6 months: n = 5 | ||||
| 12 months: n = 10 | |||||
| 18 months: n = 5 | |||||
| 24 months: n = 2 | |||||
| more than 24 months: n = 2 | |||||
| Number of absences in the last scholastic year | No absence: n = 1 | ||||
| Only for important visits: n = 1 | |||||
| 4–10 h: n = 3 | |||||
| 2–4 days: n = 6 | |||||
| 5–7 days: n = 4 | |||||
| 9–10 days: n = 4 | |||||
| 20 days: n = 1 | |||||
| 60 days: n = 1 | |||||
| No response: n = 3 | |||||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tremolada, M.; Taverna, L.; Bonichini, S.; Basso, G.; Pillon, M. Self-Esteem and Academic Difficulties in Preadolescents and Adolescents Healed from Paediatric Leukaemia. Cancers 2017, 9, 55. https://doi.org/10.3390/cancers9060055
Tremolada M, Taverna L, Bonichini S, Basso G, Pillon M. Self-Esteem and Academic Difficulties in Preadolescents and Adolescents Healed from Paediatric Leukaemia. Cancers. 2017; 9(6):55. https://doi.org/10.3390/cancers9060055
Chicago/Turabian StyleTremolada, Marta, Livia Taverna, Sabrina Bonichini, Giuseppe Basso, and Marta Pillon. 2017. "Self-Esteem and Academic Difficulties in Preadolescents and Adolescents Healed from Paediatric Leukaemia" Cancers 9, no. 6: 55. https://doi.org/10.3390/cancers9060055





