Vascular Cell Co-Culture on Silk Fibroin Matrix
Abstract
:1. Introduction
2. Materials and Methods
2.1. Preparation of SF Solution
2.2. Preparation of Regenerated SF Films and SFTSs
2.3. Cell Culture
2.4. DNA Extraction and DNA Content Determination
2.5. Immunofluorescence Analysis
2.6. SEM Analysis
2.7. RT-PCR
2.8. DNA Agarose Gel Electrophoresis
2.9. Statistical Analysis
3. Results and Discussion
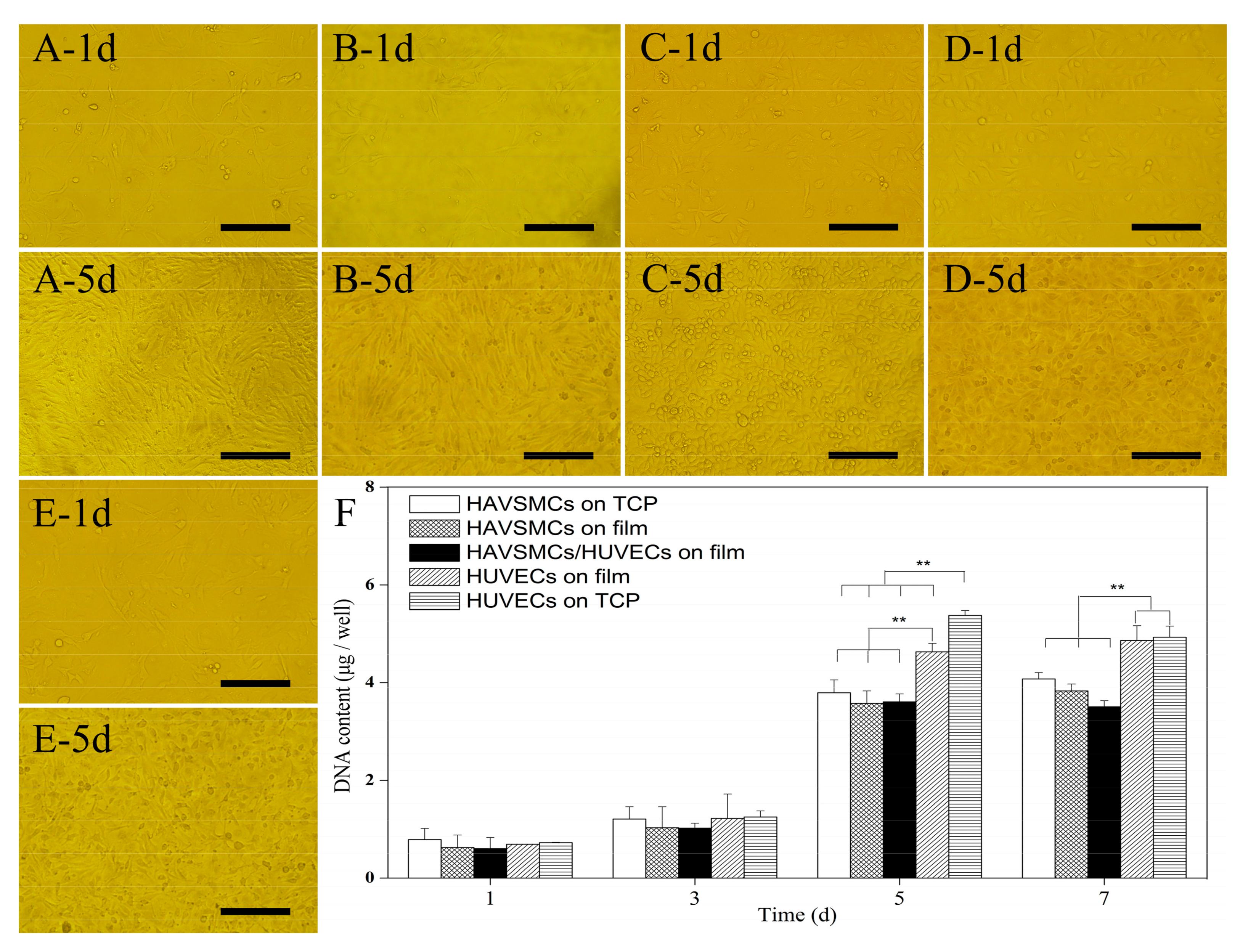
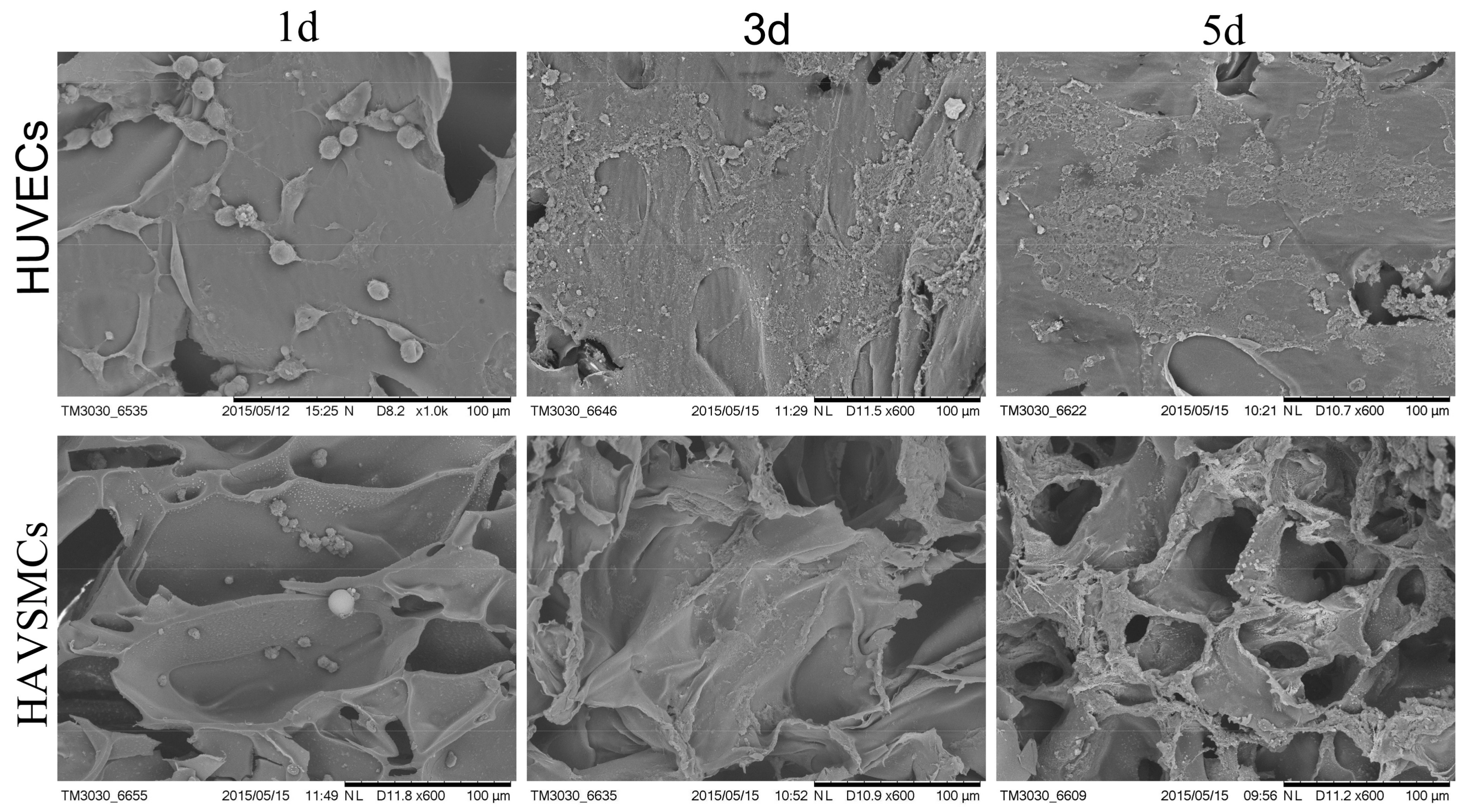
3.1. Cell Morphology and Proliferation of HAVSMC/HUVEC Co-Cultures
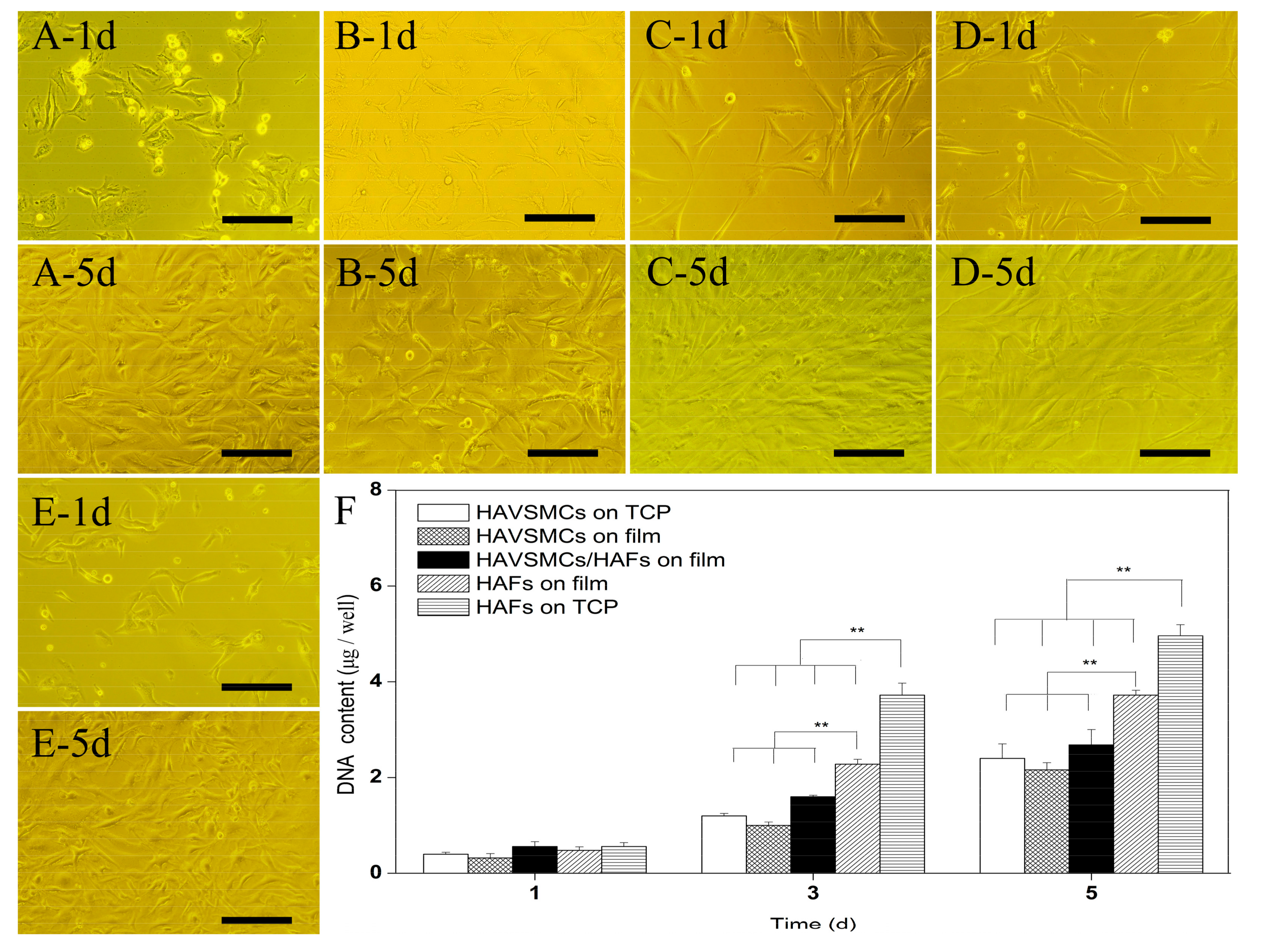
3.2. Cell Morphology and Proliferation of HAVSMC/HAF Co-Cultures
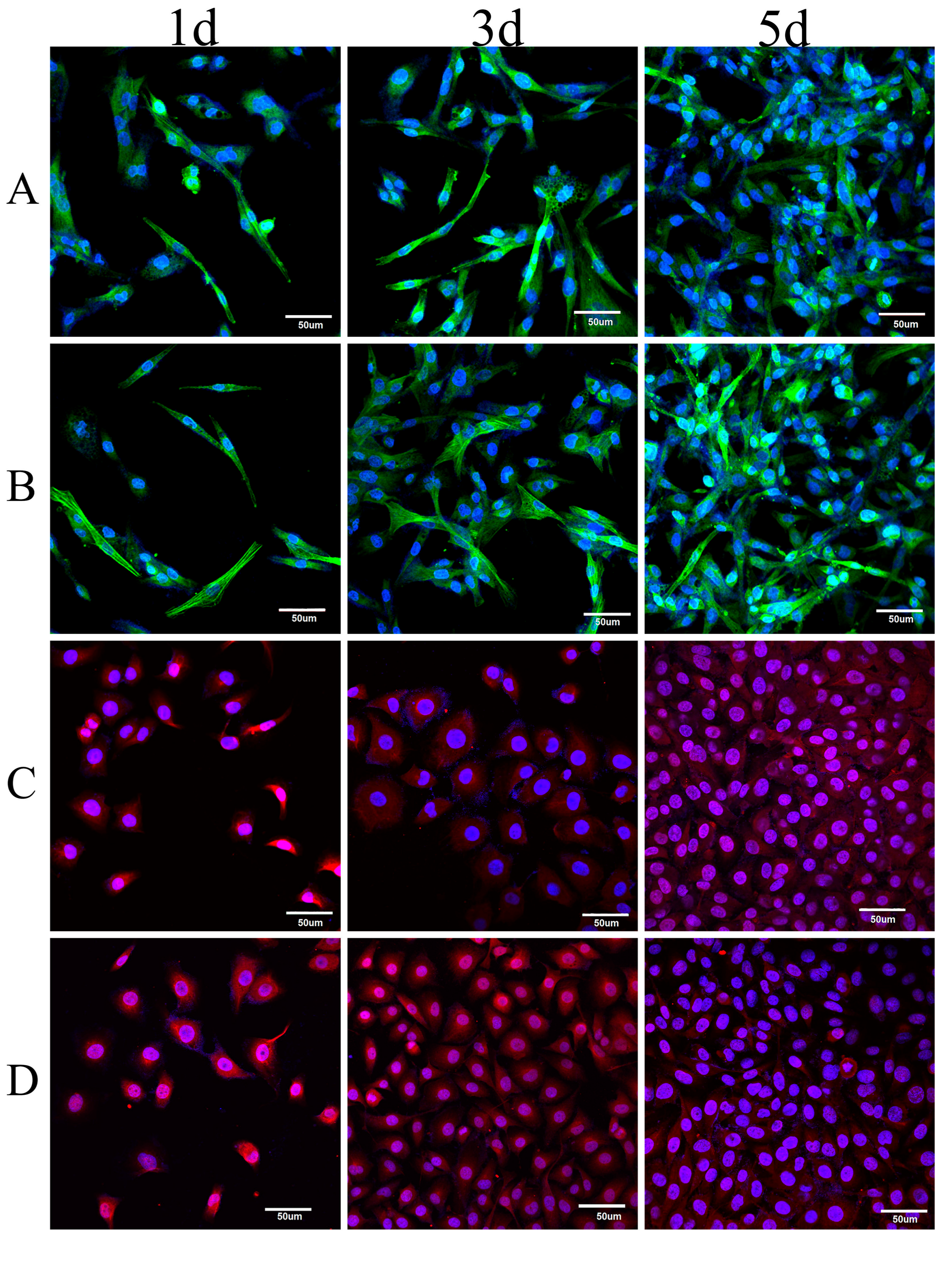
3.3. Immunofluorescence Analysis of Co-Cultured Cells
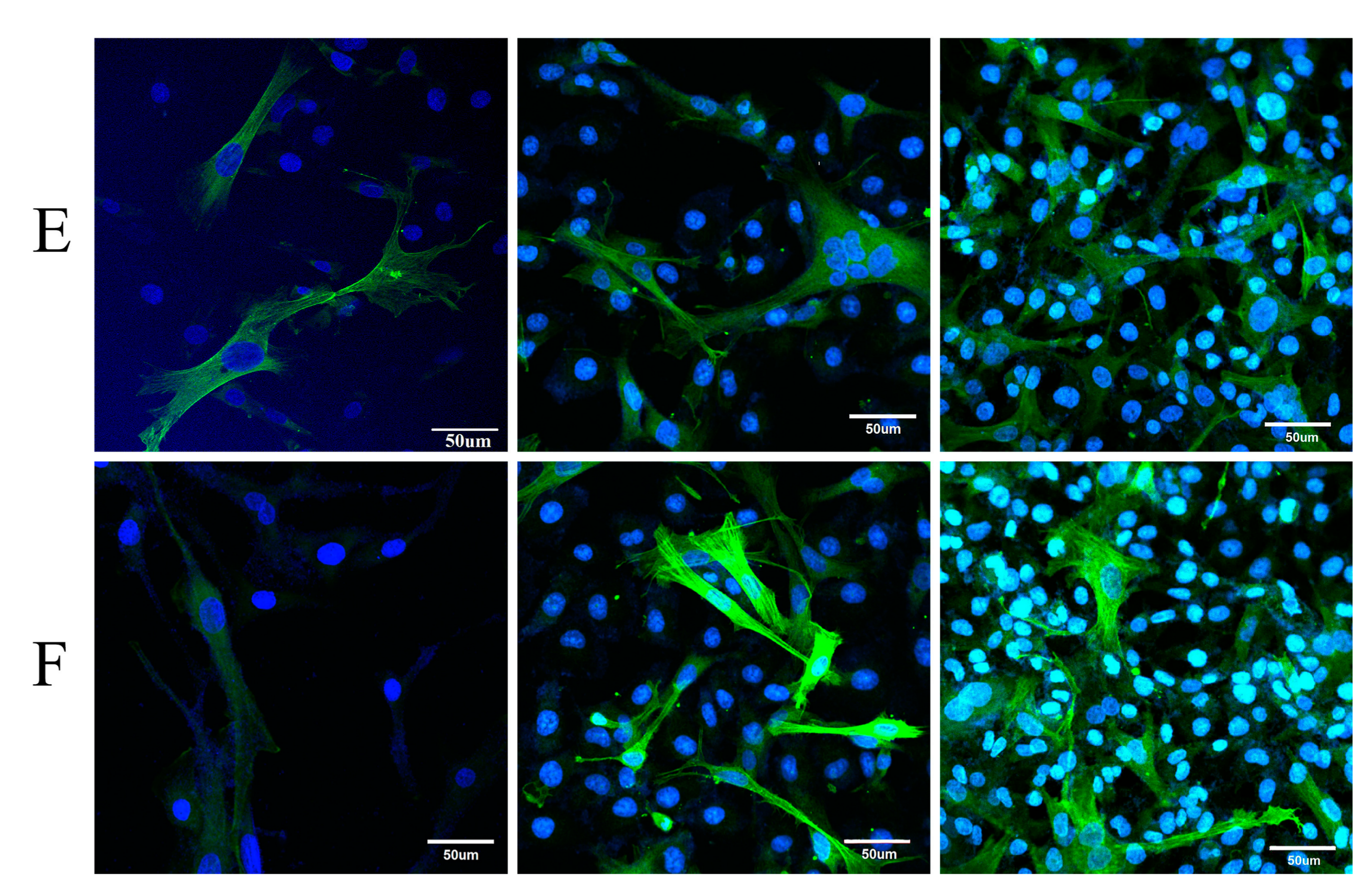
3.4. Cell Morphology on SFTSs
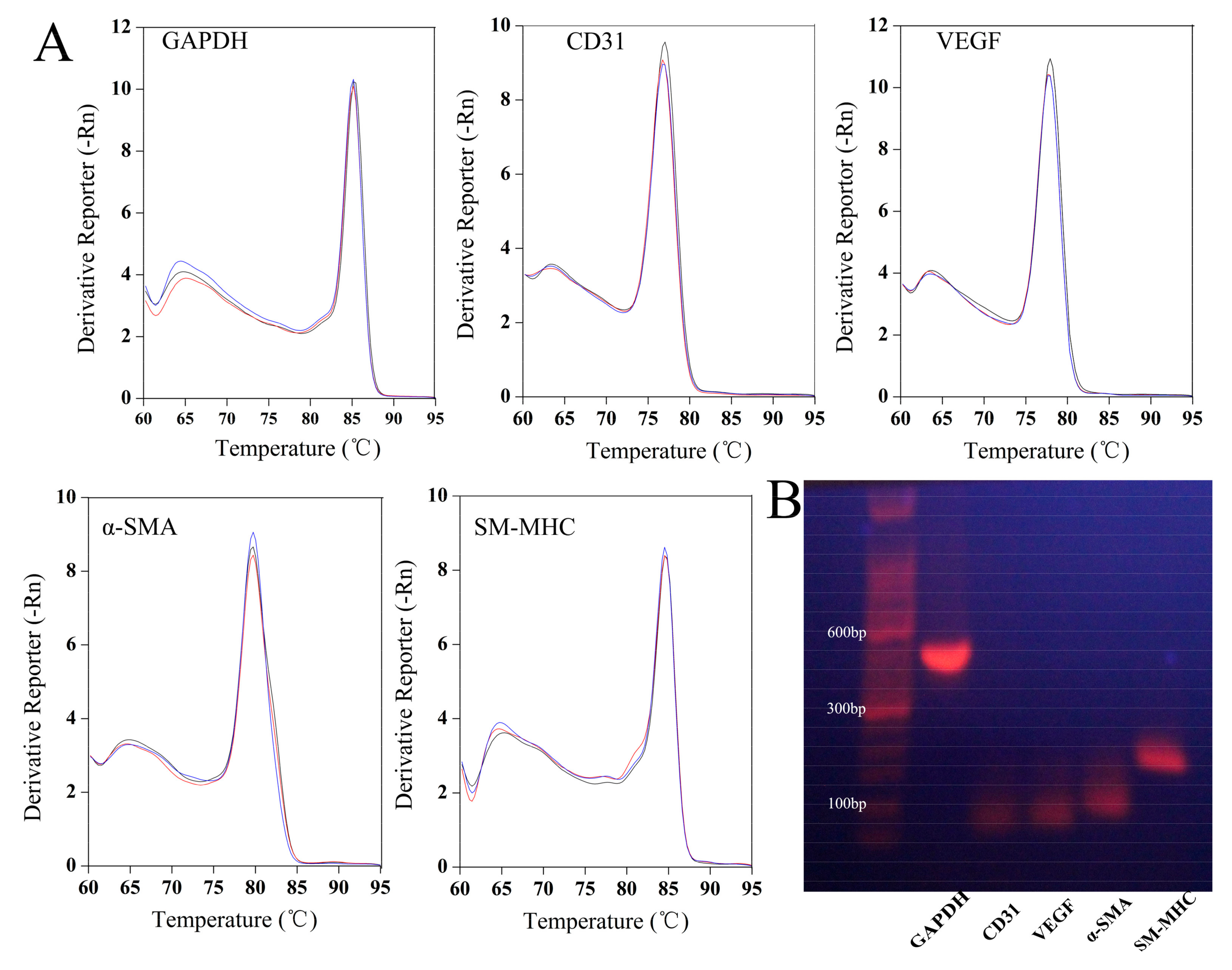
3.5. Appraisal of Primers for PCR
3.6. Cytokine Expression Levels of Co-Culture on SF Films
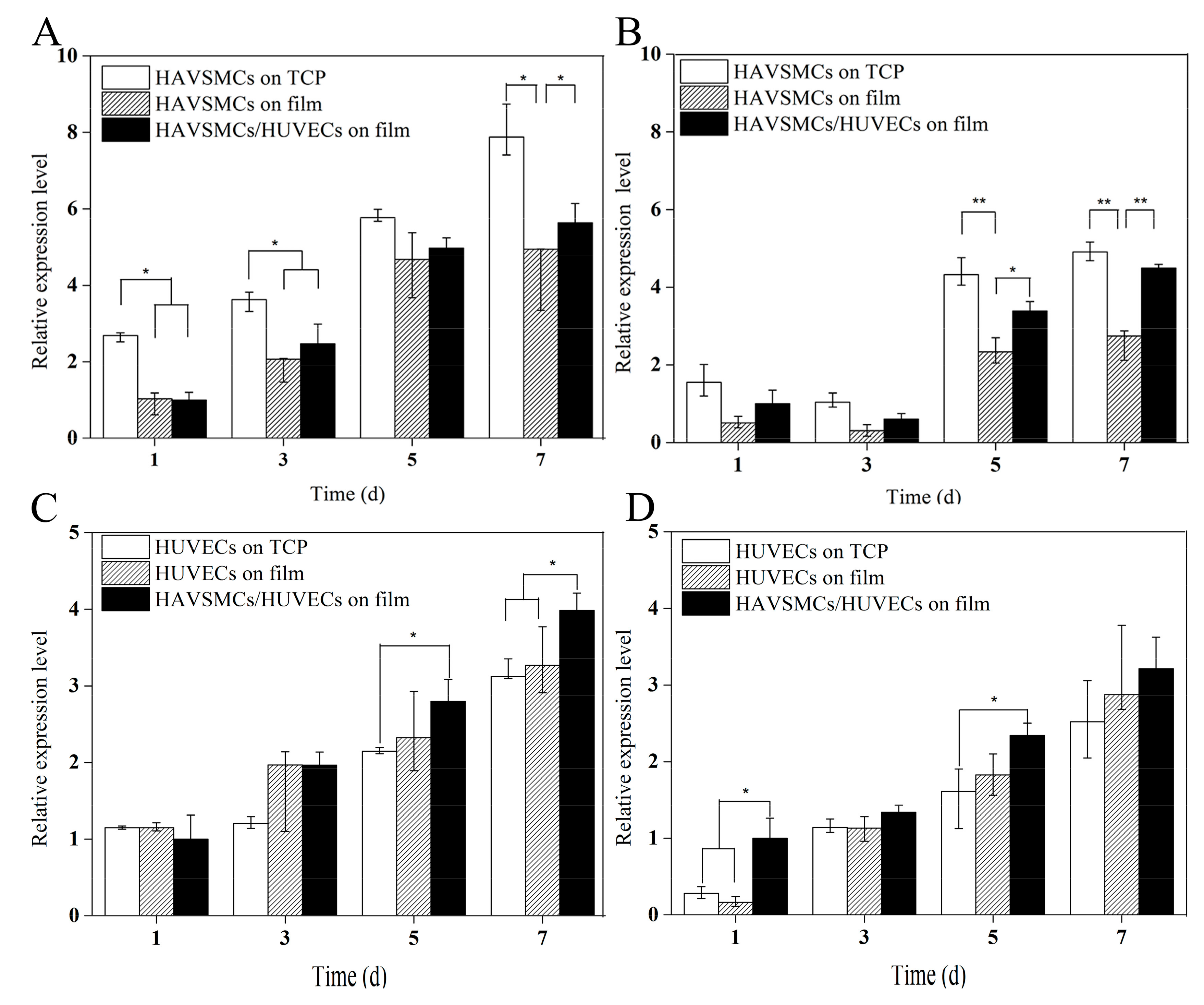
3.6.1. HUVEC/HAVSMC Co-Cultures
3.6.2. HAVSMC/HAF Co-Cultures
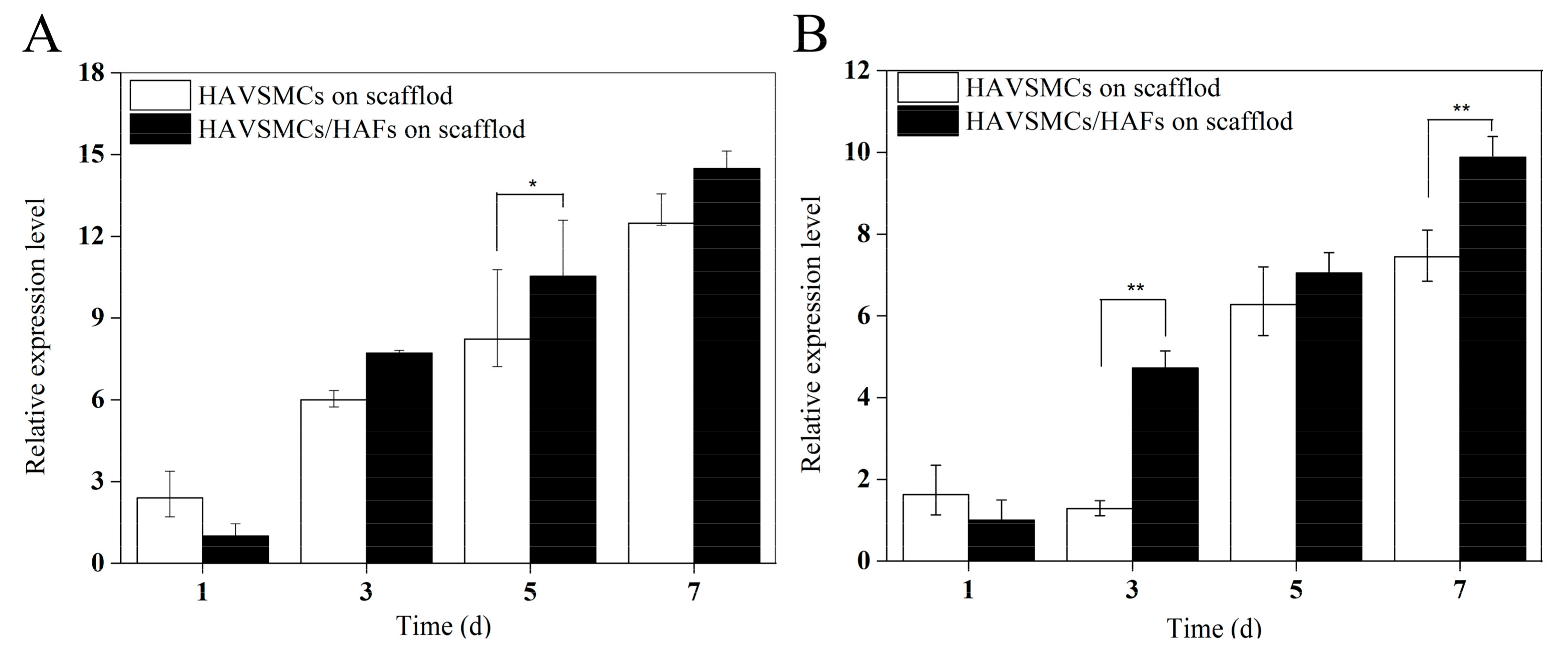
3.7. Cytokine Expression Levels of Co-Culture on SFTSs
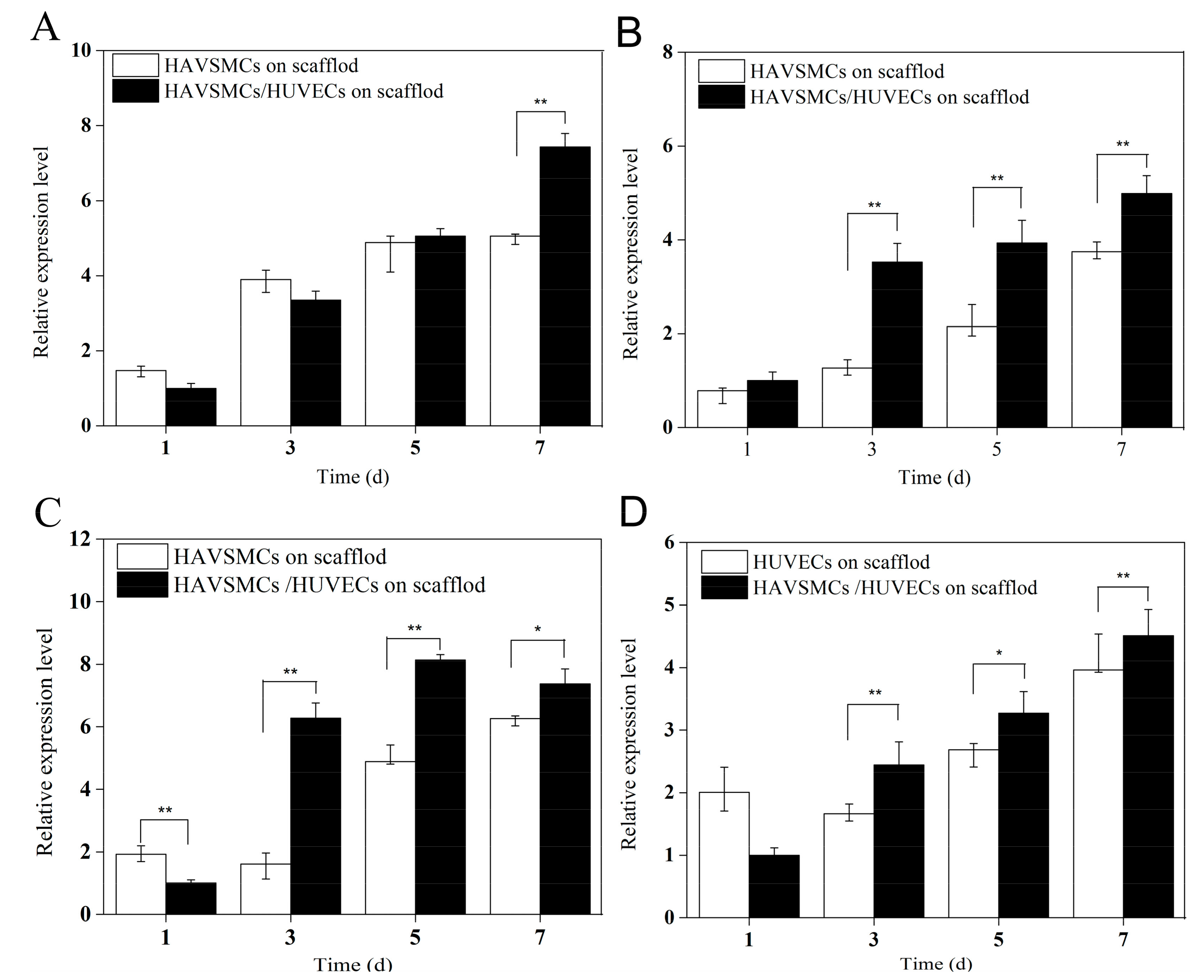
3.7.1. HUVEC/HAVSMC Co-Cultures
3.7.2. HAVSMC/HAF Co-Cultures
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Aboshady, I.; Raad, I.; Shah, A.S.; Vela, D.; Dvorak, T.; SAfi, H.J.; Buja, L.M.; Khalil, K.G. A pilot study of a triple antimicrobial-bonded Dacron graft for the prevention of aortic graft infection. J. Vasc. Surg. 2012, 56, 794–801. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, M.; Meinhart, J.; Zilla, P.; Howanietz, N.; Gorlitzer, M.; Froeschl, A.; Stuempflen, A.; Bezuidenhout, D.; Grabenwoeger, M. Long-term experience in autologous in vitro endothelialization of infrainguinal ePTFE grafts. J. Vasc. Surg. 2009, 49, 352–362. [Google Scholar] [CrossRef] [PubMed]
- Battiston, K.G.; Ouyang, B.; Labow, R.S.; Simmons, C.A.; Santerre, J.P. Monocyte/macrophage cytokine activity regulates vascular smooth muscle cell function within a degradable polyurethane scaffold. Acta Biomater. 2014, 10, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Cummings, I.; George, S.; Kelm, J.; Schmidt, D.; Emmert, M.Y.; Weber, B.; Zünd, G.; Hoerstrup, S.P. Tissue-engineered vascular graft remodeling in a growing lamb model: Expression of matrix metalloproteinases. Eur. J. Cardio-Thorac. Surg. 2012, 41, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Kurobe, H.; Maxfield, M.W.; Tara, S.; Rocco, K.A.; Bagi, P.S.; Yi, T.; Udelsman, B.; Zhuang, Z.W.; Cleary, M.; Iwakiri, Y.; et al. Development of small diameter nanofiber tissue engineered arterial grafts. PLoS ONE 2015, 10, e0120328. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Guo, W.; Chen, M.; Yuan, Z.; Wang, M.; Zhang, Y.; Liu, S.; Xi, T.; Guo, Q. Fabrication and characterization of electrospun nanofibers composed of decellularized meniscus extracellular matrix and polycaprolactone for meniscus tissue engineering. J. Mater. Chem. B 2017, 5, 2273–2285. [Google Scholar] [CrossRef]
- Roh, J.D.; Nelson, G.N.; Brennan, M.P.; Mirensky, T.L.; Yi, T.; Hazlett, T.F.; Tellides, G.; Sinusas, A.J.; Pober, J.S.; Saltzman, W.M.; et al. Small-diameter biodegradable scaffolds for functional vascular tissue engineering in the mouse model. Biomaterials 2008, 29, 1454–1463. [Google Scholar] [CrossRef] [PubMed]
- Dargaville, B.L.; Vaquette, C.; Peng, H.; Rasoul, F.; Chau, Y.Q.; Cooper-White, J.J.; Campbell, J.H.; Whittaker, A.K. Cross-linked poly(trimethylene carbonate-co-l-lactide) as a biodegradable, elastomeric scaffold for vascular engineering applications. Biomacromolecules 2011, 12, 3856–3869. [Google Scholar] [CrossRef] [PubMed]
- Catto, V.; Farè, S.; Freddi, G.; Tanzi, M.C. Vascular tissue engineering: Recent advances in small diameter blood vessel regeneration. ISRN Vasc. Med. 2014, 2014, 1–27. [Google Scholar] [CrossRef]
- De, V.S.; Tille, J.C.; Giliberto, J.P.; Mrowczynski, W.; Gurny, R.; Walpoth, B.H.; Mölle, M. Advantages of bilayered vascular grafts for surgical applicability and tissue regeneration. Acta Biomater. 2012, 8, 3914–3920. [Google Scholar]
- Columbus, S.; Krishnan, L.K.; Kalliyana, K.V. Relating pore size variation of poly (ɛ-caprolactone) scaffolds to molecular weight of porogen and evaluation of scaffold properties after degradation. J. Biomed. Mater. Res. B 2014, 102, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Rossi, L.; Attanasio, C.; Vilardi, E.; De Gregorio, M.; Netti, P.A. Vasculogenic potential evaluation of bottom-up, PCL scaffolds guiding early angiogenesis in tissue regeneration. J. Mater. Sci. Mater. Med. 2016, 27, 107. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, C.E.; Baier, J.M. Acellular vascular tissues: Natural biomaterials for tissue repair and tissue engineering. Biomaterials 2000, 21, 2215–2231. [Google Scholar] [CrossRef]
- Wu, H.C.; Wang, T.W.; Kang, P.L.; Tsuang, Y.H.; Sun, J.S.; Lin, F.H. Coculture of endothelial and smooth muscle cells on a collagen membrane in the development of a small-diameter vascular graft. Biomaterials 2007, 28, 1385–1392. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, S.; Ramamurthi, A. Hyaluronic acid cues for functional endothelialization of vascular constructs. J. Tissue Eng. Regen. Med. 2008, 2, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Sreerekha, P.R.; Divya, P.; Krishnan, L.K. Adult stem cell homing and differentiation in vitro on composite fibrin matrix. Cell Prolif. 2006, 39, 301–312. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Wei, Y.; Yi, H.; Liu, Z.; Sun, D.; Zhao, H. Cytocompatibility of a silk fibroin tubular scaffold. Mater. Sci. Eng. C 2014, 34, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Wheeldon, I.; Farhadi, A.; Bick, A.G.; Jabbari, E.; Khademhosseini, A. Nanoscale tissue engineering: Spatial control over cell-materials interactions. Nanotechnology 2011, 22, 212001. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, G.M.; Rodas, A.C.D.; Leite, C.A.P.; Giles, C.; Higa, O.Z.; Polakiewicz, B.; Beppu, M.M. Preparation and characterization of ethanol-treated silk fibroin dense membranes for biomaterials application using waste silk fibers as raw material. Bioresour. Technol. 2010, 101, 8446–8451. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Chen, J.; Chou, A.H.; Li, G.; Legeros, R.Z. Nonwoven silk fibroin net/nano-hydroxyapatite scaffold: Preparation and characterization. J. Biomed. Mater. Res. A 2009, 91, 1140–1149. [Google Scholar] [CrossRef] [PubMed]
- Vázquez, N.; Rodríguez-Barrientos, C.A.; Aznar-Cervantes, S.D.; Chacón, M.; Cenis, J.L.; Riestra, A.C.; Sánchez-Avila, R.M.; Persinal, M.; Brea-Pastor, A.; Fernández-Vega Cueto, L.; et al. Silk fibroin films for corneal endothelial regeneration: Transplant in a rabbit descemet membrane endothelial keratoplasty. Investig. Ophthalmol. Vis. Sci. 2017, 58, 3357–3365. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Tripathy, N.; Sun, A.C.; Joo, C.K.; Lee, D.; Khang, G. Bioengineered neo-corneal endothelium using collagen type-i coated silk fibroin film. Colloids Surf. B 2015, 136, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Hao, Y.; Yang, G.; Wang, J. Hemocompatibility and cytocompatibility of the hirudin-modified silk fibroin. J. Biomed. Mater. Res. B 2015, 103, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Adalı, T.; Uncu, M. Silk fibroin as a non-thrombogenic biomaterial. Int. J. Biol. Macromol. 2016, 90, 11–19. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.Y.; Tu, F.F.; Liu, Y.F.; Zhang, Y.J.; Li, H.L.; Kang, Z.; Yin, Y.; Wang, J.N. The effect of hirudin modification of silk fibroin on cell growth and antithrombogenicity. Mater. Sci. Eng. C 2017, 75, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, S.; Nandi, S.K.; Mandal, B.B. Stacked silk-cell monolayers as a biomimetic three dimensional construct for cardiac tissue reconstruction. J. Mater. Chem. B 2017, 5, 6325–6338. [Google Scholar] [CrossRef]
- Sun, X.L.; Hao, Y.X.; Wang, Q.Y.; Dong, F.L.; Wang, J.N. Cell growth and proliferation on the interface of a silk fabric tubular scaffold. Text. Res. J. 2016, 86, 2193–2201. [Google Scholar] [CrossRef]
- Yen, K.C.; Chen, C.Y.; Huang, J.Y.; Kuo, W.T.; Lin, F.H. Fabrication of keratin/fibroin membranes by electrospinning for vascular tissue engineering. J. Mater. Chem. B 2015, 4, 237–244. [Google Scholar] [CrossRef]
- Moon, B.M.; Kim, D.K.; Park, H.J.; Ju, H.W.; Lee, O.J.; Kim, J.-H.; Lee, J.M.; Lee, J.S.; Park, C.H. Fabrication and characterization of three-dimensional silk fibroin scaffolds using a mixture of salt/sucrose. Macromol. Res. 2014, 22, 1268–1274. [Google Scholar] [CrossRef]
- Seib, F.P.; Herklotz, M.; Burke, K.A.; Maitz, M.F.; Werner, C.; Kaplan, D.L. Multifunctional silk-heparin biomaterials for vascular tissue engineering applications. Biomaterials 2014, 35, 83–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamada, Y. Sulfation of silk fibroin by sulfuric acid and anticoagulant activity. J. Appl. Polym. Sci. 2003, 87, 2377–2382. [Google Scholar] [CrossRef]
- Zhang, J.; Huang, H.; Ju, R.; Chen, K.; Li, S.; Wang, W.; Yan, Y. In vivo biocompatibility and hemocompatibility of a polytetrafluoroethylene small diameter vascular graft modified with sulfonated silk fibroin. Am. J. Surg. 2017, 213, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.L.; Sun, D.; Yi, H.G.; Wang, J.N. Characterization of a PEG-DE cross-linked tubular silk scaffold. Text. Res. J. 2014, 84, 959–967. [Google Scholar] [CrossRef]
- Singh, R.; Sarker, B.; Silva, R.; Detsch, R.; Dietel, B.; Alexiou, C.; Boccaccini, A.R.; Cicha, I. Evaluation of hydrogel matrices for vessel bioplotting: Vascular cell growth and viability. J. Biomed. Mater. Res. A 2015, 104, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Steucke, K.E.; Tracy, P.V.; Hald, E.S.; Hall, J.L.; Alford, P.W. Vascular smooth muscle cell functional contractility depends on extracellular mechanical properties. J. Biomech. 2015, 48, 3044–3051. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.N.; Yi, H.G.; Wei, Y.Q. Preliminary biocompatibility evaluation of regenerated Antheraea yamamai silk fibroin in vitro. J. Wuhan Univ. Technol. Mater. Sci. Ed. 2011, 26, 1044–1048. [Google Scholar] [CrossRef]
- Liu, Y.X.; Rayatpisheh, S.; Chew, S.Y.; Chanpark, M.B. Impact of endothelial cells on 3d cultured smooth muscle cells in a biomimetic hydrogel. ACS Appl. Mater. Interfaces 2012, 4, 4–1378. [Google Scholar] [CrossRef] [PubMed]
- Hoenig, M.R.; Campbell, G.R.; Campbell, J.H. Vascular grafts and the endothelium. Endothelium 2006, 13, 385–401. [Google Scholar] [CrossRef] [PubMed]

| Gene | Primer Sequence (5′–3′) | Product Length (bp) | Annealing Temperature (°C) | Amplification Efficiency (%) |
|---|---|---|---|---|
| GAPDH | GTCACTGGTGGACCTGACCTAGGGGTCTACATGGCAACTG | 420 | 60 | 105.677 |
| VEGF | GCTCAGAGCGGAGAAAGCATGCAACGCGAGTCTGTGTTTT | 80 | 54 | 108.152 |
| CD31 | GGTGGATGAGGTCCAGATTTCCAGCACAATGTCCTCTCCAG | 67 | 56 | 108.635 |
| α-SMA | CCGACCGAATGCAGAAGGAACAGAGTATTTGCGCTCCGGA | 88 | 56 | 106.284 |
| SM-MHC | GGCCGTCAAGTCCAAGTTCAACCACCTGCAGCAAGATTTCC | 158 | 56 | 90.112 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tu, F.; Liu, Y.; Li, H.; Shi, P.; Hao, Y.; Wu, Y.; Yi, H.; Yin, Y.; Wang, J. Vascular Cell Co-Culture on Silk Fibroin Matrix. Polymers 2018, 10, 39. https://doi.org/10.3390/polym10010039
Tu F, Liu Y, Li H, Shi P, Hao Y, Wu Y, Yi H, Yin Y, Wang J. Vascular Cell Co-Culture on Silk Fibroin Matrix. Polymers. 2018; 10(1):39. https://doi.org/10.3390/polym10010039
Chicago/Turabian StyleTu, Fangfang, Yunfei Liu, Helei Li, Pange Shi, Yunxia Hao, Yue Wu, Honggen Yi, Yin Yin, and Jiannan Wang. 2018. "Vascular Cell Co-Culture on Silk Fibroin Matrix" Polymers 10, no. 1: 39. https://doi.org/10.3390/polym10010039




