Microporous Polyurethane Thin Layer as a Promising Scaffold for Tissue Engineering
Abstract
:1. Introduction
2. Experimental
2.1. Polyurethane Synthesis (PUR)
2.2. Microporous Polyurethane Thin Layers (MPTL) Fabrication
2.3. Fourier Transform Infrared Spectroscopy (FTIR)
2.4. Proton Nuclear Magnetic Resonance (1HNMR)
2.5. Water Contact Angle
2.6. Mechanical Properties
2.7. Scanning Electron Microscopy (SEM)
2.8. Biocompatibility Studies of MPTL on NIH3T3 Fibroblast Cell Line
2.8.1. Cell Culture
2.8.2. Indirect MTT Proliferation Assay
2.8.3. Statistical Analysis
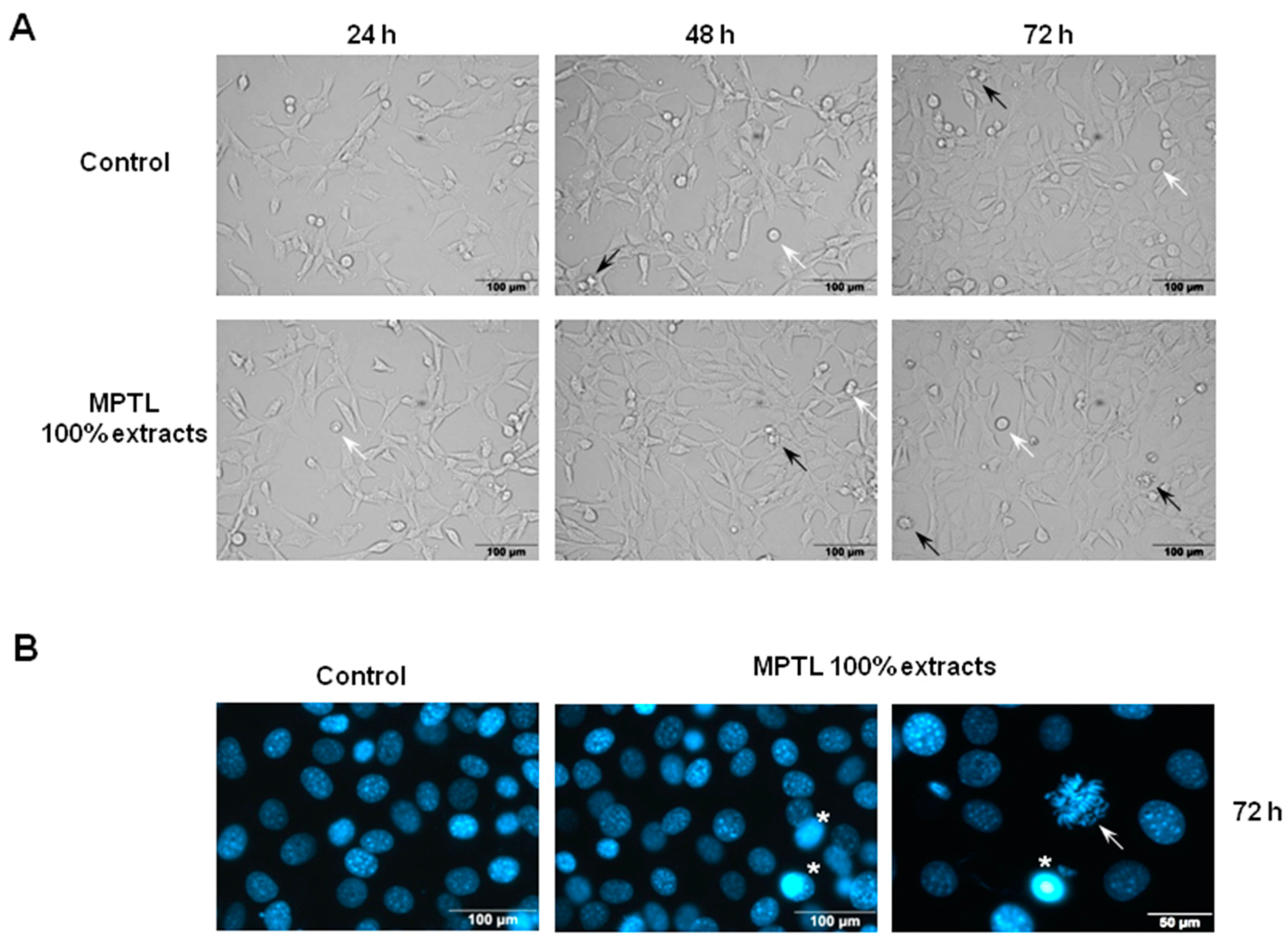
2.8.4. Analysis of Cellular and Nuclear Morphology
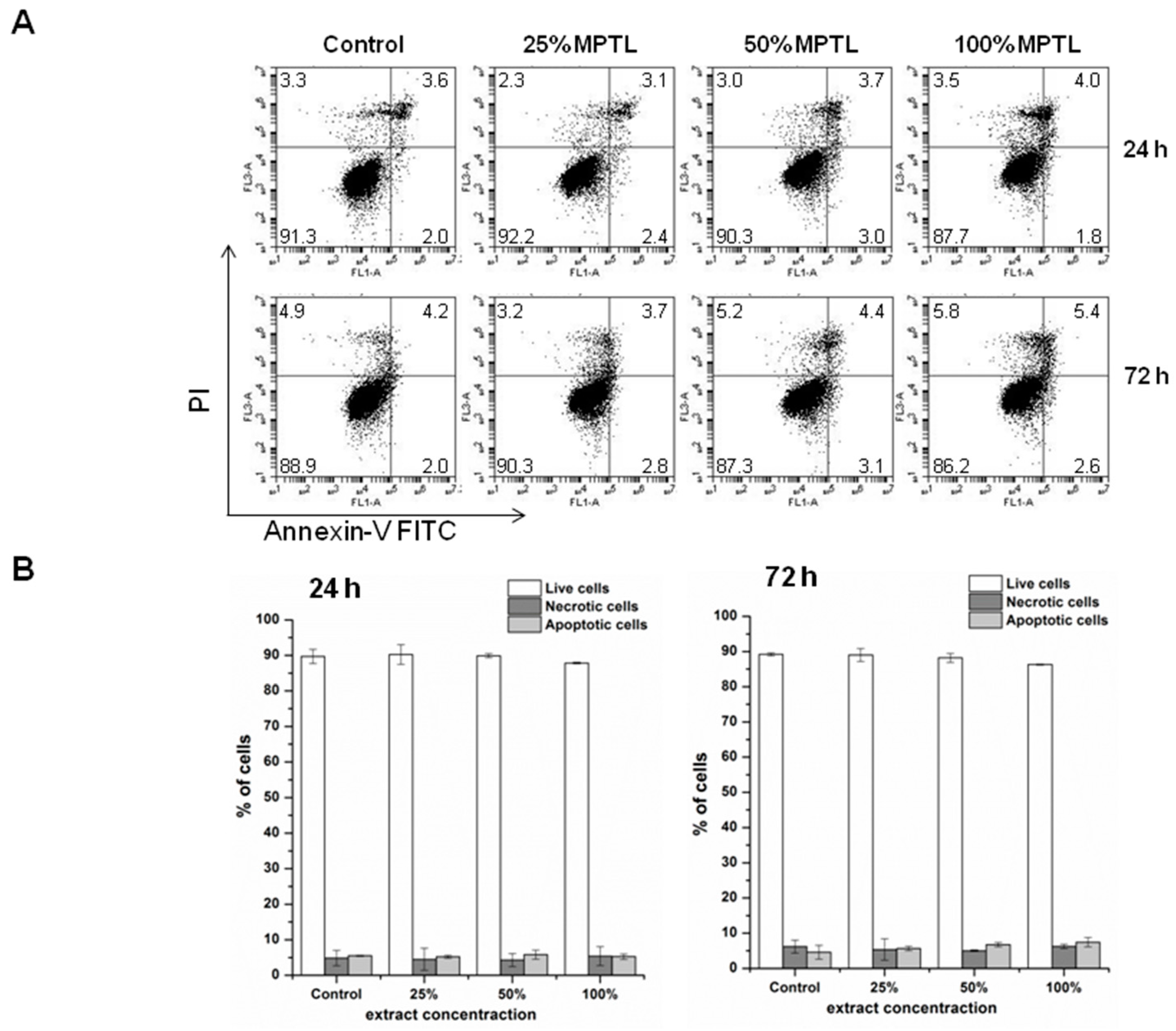
2.8.5. Detection of Apoptotic and Necrotic Cell Death by Flow Cytometry
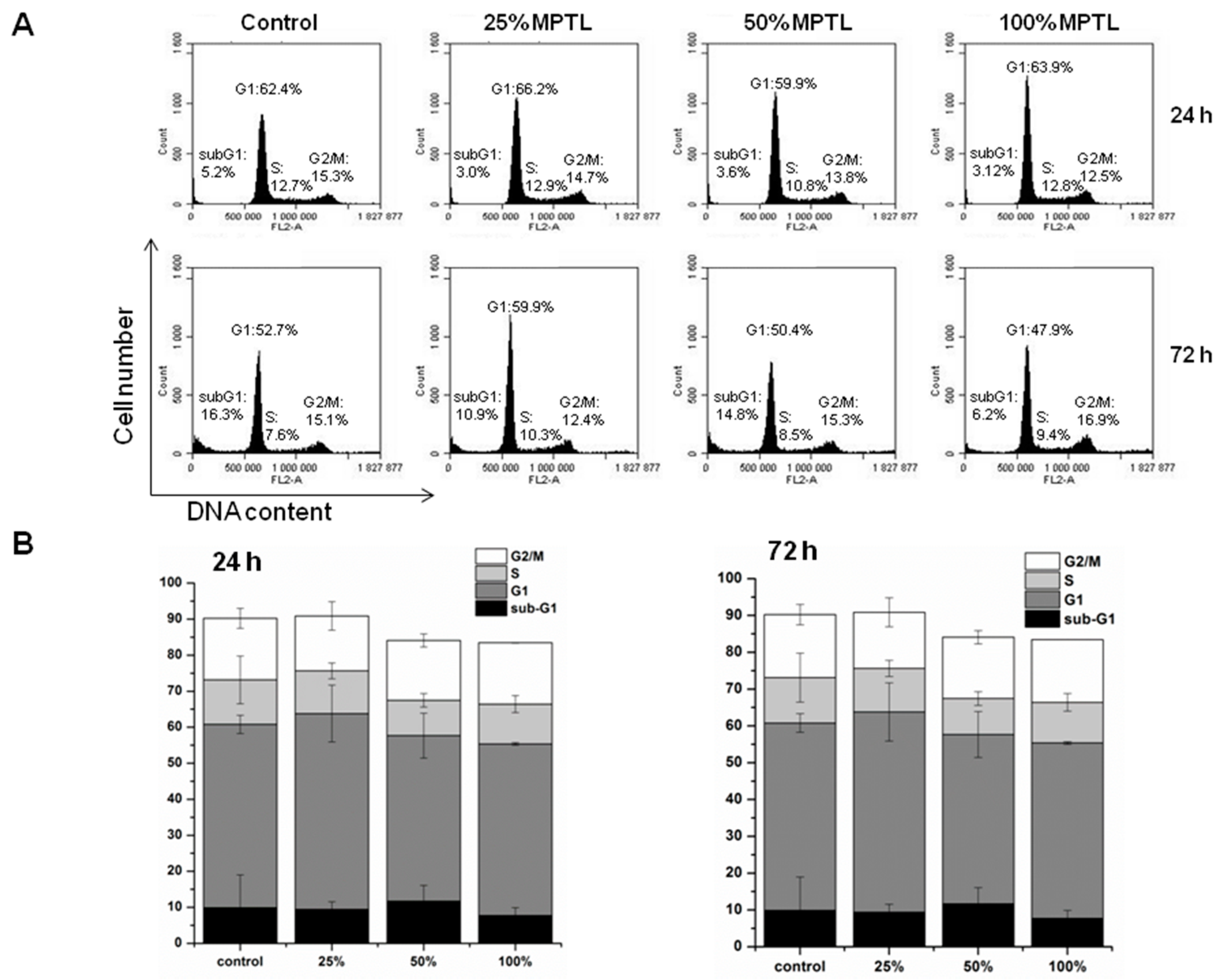
2.8.6. Flow Cytometry Analysis of Cell Cycle
3. Results
3.1. Fourier Transform Infrared Spectroscopy (FTIR)
3.2. Proton Nuclear Magnetic Resonance (1HNMR)
3.3. Water Contact Angle
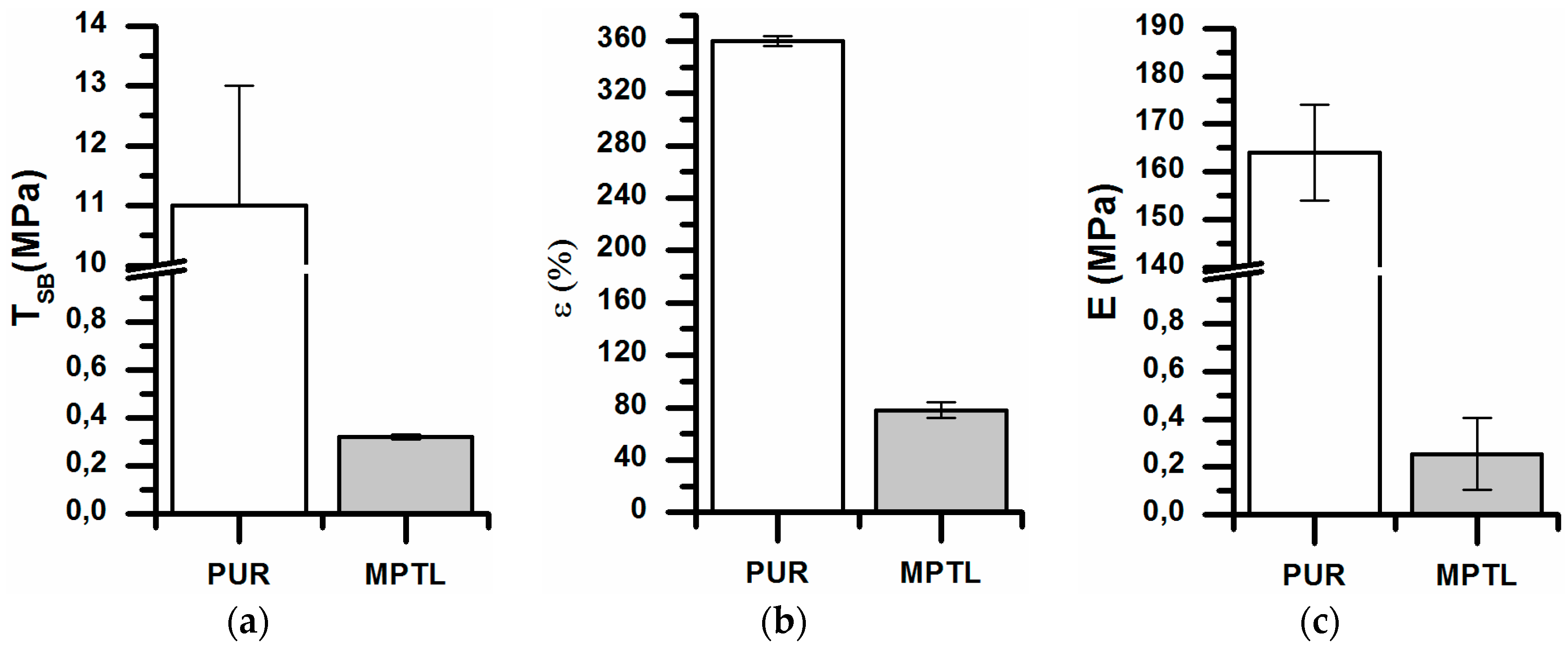
3.4. Mechanical Properties
Tensile Strength (TSb), Elongation at Break (ε) and Young’s Modulus (E)
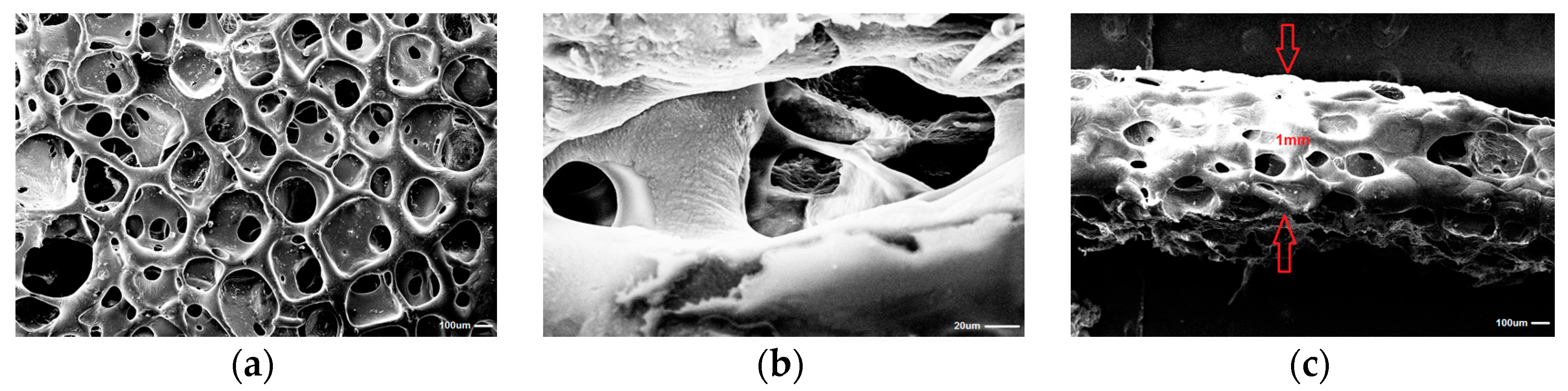
3.5. Scanning Electron Microscopy (SEM)
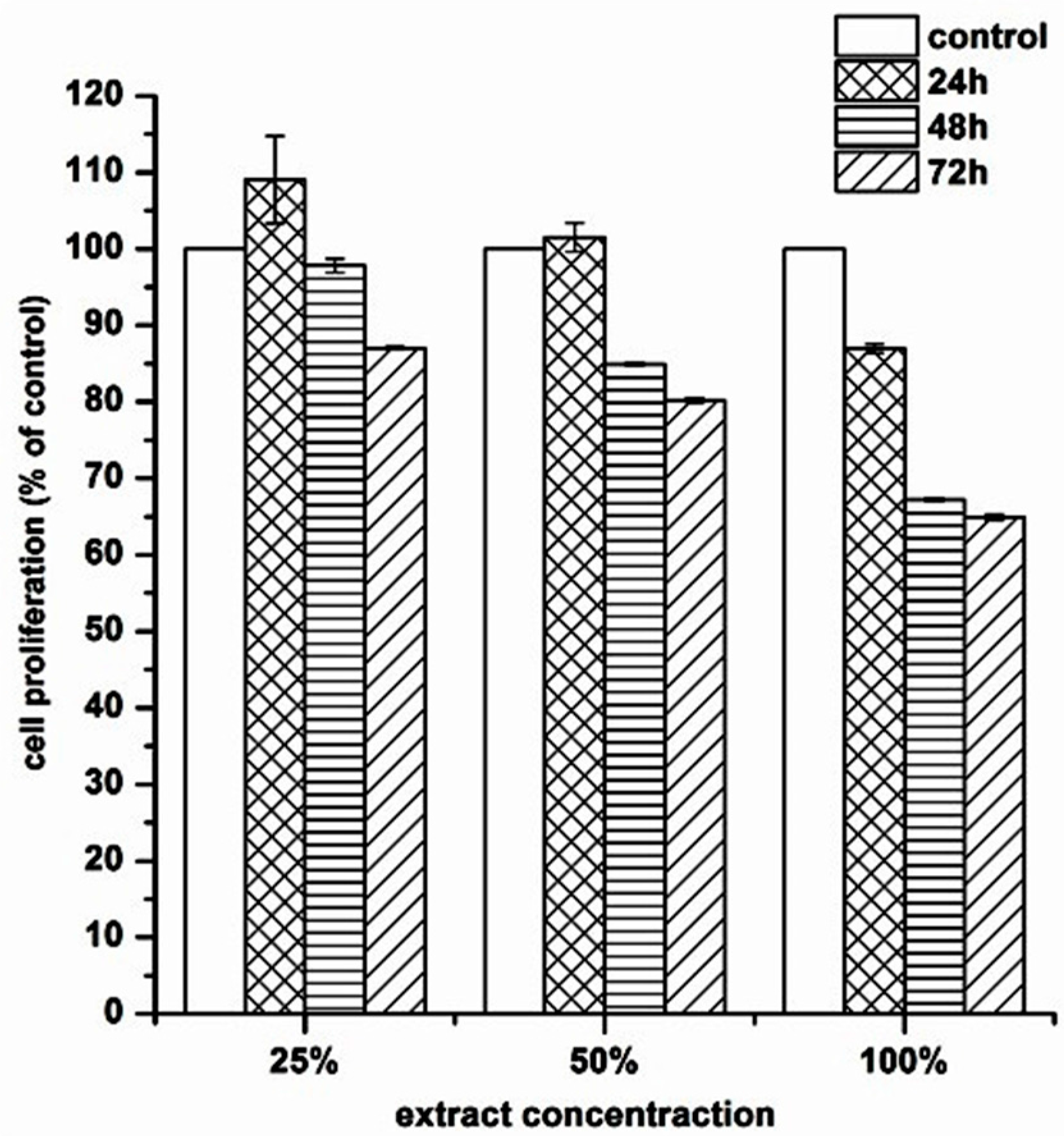
3.6. Biocompatibility of MTPL on Mouse Embryonic NIH 3T3 Fibroblast Cell Line
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Langer, R.; Vacanti, J. Tissue engineering. Science 1993, 260, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Yeong, W.Y.; Chua, C.K.; Leong, K.F.; Chandrasekaran, M. Rapid prototyping in tissue engineering: Challenges and potential. Trends Biotechnol. 2004, 22, 643. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.S.; Mooney, D.J. Development of biocompatible synthetic extracellular matrices for tissue engineering. Trends Biotechnol. 1998, 15, 224–230. [Google Scholar] [CrossRef]
- Kucinska-Lipka, J.; Gubanska, I.; Janik, H.; Sienkiewicz, M. Fabrication of polyurethane and polyurethane based composite fibers by the electrospinning technique for soft tissue engineering of cardiovascular system. Mater. Sci. Eng. C. 2015, 46, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Kucinska-Lipka, J.; Gubanska, I.; Janik, H.; Pokrywczynska, M.; Drewa, T. l-ascorbic acid modified poly(ester urethane)s as a suitable candidates for soft tissue engineering applications. React. Funct. Polym. 2015, 97, 105–115. [Google Scholar] [CrossRef]
- Caracciolo, P.C.; Thomas, V.; Vohra, Y.K.; Buffa, F.; Abraham, G.A. Electrospinning of novel biodegradable poly(ester urethane)s and poly(ester urethane urea)s for soft tissue engineering applications. J. Mater. Sci. Mater. Med. 2009, 20, 2129–2137. [Google Scholar] [CrossRef] [PubMed]
- Abbott, W.M.; Megerman, J.; Hasson, J.E.; L’Italien, G.; Warnock, D.F. Effects of compliance mismatch on vascular graft patency. J. Vasc. Surg. 1987, 5, 376–382. [Google Scholar] [CrossRef]
- Guan, J.; Sacks, M.S.; Beckman, E.; Wagner, W.R. Synthesis, characterization and cytocompatybility of elastomeric, biodegradable poly(ester-urethane)ureas based on poly(caprolactone) and putrescine. J. Biomed. Mater. Res. 2002, 61, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Guan, J.; Sacks, M.S.; Beckman, E.J.; Wagner, W.R. Biodegradable poly(ether ester urethane)urea elastomers based on poly(ether ester) triblock copolymers and putrescine: Synthesis, characterization and cytocompatybility. Biomaterials 2004, 25, 85–96. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Beckamn, E.J.; Piesco, N.J.; Agarwal, S.A. A new-peptide-based urethane polymer: Synthesis, biodegradation and potential to support cell growth in vitro. Biomaterials 2000, 21, 1247–1258. [Google Scholar] [CrossRef]
- Zhang, J.Y.; Beckman, E.J.; Hu, J.; Yuang, G.G.; Agarwal, S.A.; Hollinger, J.O. Synthesis, biodegradability and biocompatybility of lysine diisocyanate-glucose polymers. Tissue Eng. 2002, 8, 771–785. [Google Scholar] [CrossRef] [PubMed]
- Leong, K.F.; Cheah, C.M.; Chua, C.K. Solid freeform fabrication of threedimensional scaffolds for engineering replacement tissues and organs. Biomaterials 2003, 24, 2363–2378. [Google Scholar] [CrossRef]
- Diban, N.; Stamatialis, D.F. Functional polymer scaffolds for blood vessel tisse engineering. Macromol. Symp. 2011, 309/310, 93–99. [Google Scholar] [CrossRef]
- Sachlos, E.; Czernuszka, J.T. Making tissue engineering scaffolds work. Review on the application of solid freeform fabrication technology to the production of tissue engineering scaffolds. Eur. Cells Mater. 2003, 5, 29–40. [Google Scholar] [CrossRef]
- Tran, R.T.; Thevenot, P.; Zhang, Y.; Gyawali, D.; Tang, L.; Yang, J. Scaffold sheet design strategy for soft tissue engineering. Nat. Mater. 2010, 3, 1375–1389. [Google Scholar] [CrossRef] [PubMed]
- Andrews, K.D.; Hunt, J.A.; Black, R.A. Technology of electrostatic spinning for the production of polyurethane tissue engineering scaffolds. Polym. Int. 2008, 57, 203–210. [Google Scholar] [CrossRef]
- Tonda-Turo, C.; Boffito, M.; Cassino, C.; Gentile, P.; Ciardelli, G. Biommimetic polyurethane-based nanofibrous scaffolds. Mater. Lett. 2016, 167, 9–12. [Google Scholar] [CrossRef]
- Sartori, S.; Rechichi, A.; Vozzi, G.; D’Acunto, M.; Heine, E.; Giusti, P. Surface modification of a synthetic polyurethane by plasma glow discharge: Preparation and characterization of bioactive molecules. React. Funct. Polym. 2008, 68, 809–821. [Google Scholar] [CrossRef]
- Draghi, L.; Resta, S.; Pirozzolo, M.G.; Tanzi, M.C. Microspheres leaching for scaffold porosity control. J. Mater. Sci. Mater. Med. 2005, 16, 1093–1097. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Chen, X. Biofabrication of tissue scaffolds. Adv. Biomater. Sci. Biomed. Appl. 2013, 12, 315–328. [Google Scholar]
- Doshi, J.; Renker, D.H. Electrospinning process and application of electrospun fibers. J. Electrost. 1995, 35, 151–160. [Google Scholar] [CrossRef]
- Boffito, M.; Sartori, S.; Ciardelli, G. Polymeric scaffolds for cardiac tissue engineering: Requirements and fabrication technologies. Polym. Int. Forthcom. 2014, 63, 2–11. [Google Scholar] [CrossRef]
- Heijkants, R.G.J.C.; Van Tienen, T.G.; De Groot, J.H.; Pennings, A.J.; Buma, P.P.; Veth, R.P.H. Preparation of a polyurethane scaffold for tissue engineering made by a combination of salt leaching and freeze-drying of dioxane. J. Mater. Sci. 2006, 41, 2423–2428. [Google Scholar] [CrossRef]
- Termonia, Y. Fundamentals of polymer coagulation. J. Polym. Sci. B Polym. Phys. 1995, 33, 279–288. [Google Scholar] [CrossRef]
- Rowlands, A.S.; Lim, S.A.; Martin, D.; Cooper-White, J.J. Polyurethane/poly(lactic-co-glycolic) acid composite scaffolds fabricated by thermally induced phase separation. Biomaterials 2007, 28, 2109–2121. [Google Scholar] [CrossRef] [PubMed]
- Laschke, M.W.; Strohe, A.; Menger, M.D.; Alini, M.; Eglin, D. In vitro and in vivo evaluation of a novel nanosize hydroxyapatite particles/poly(ester-urethane) composite scaffold for bone tissue engineering. Acta Biomater. 2010, 6, 2020–2027. [Google Scholar] [CrossRef] [PubMed]
- Ma, P.X. Scaffolds for tissue fabrication. Mater. Today 2004, 7, 30–40. [Google Scholar] [CrossRef]
- Hubbel, J.A. Biomaterials in tissue engineering. Nat. Biotechnol. 1995, 13, 565–576. [Google Scholar] [CrossRef]
- Kaplan, D.L. (Ed.) Introduction to polymers from renewable resources. In Biopolymers from Renewable Resources; Springer: Berlin, Germany, 1998; pp. 1–29. [Google Scholar]
- Grenier, S.; Sandig, M.; Mequanint, K. Polyurethane biomaterials for fabricating 3D porous scaffolds and supporting vascular cells. J. Biomed. Mater. Res. A 2007, 82A, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Mikos, A.G.; Thorsen, L.A.; Czerwonka, Y.; Bao, Y.; Langer, R.; Winslow, D.N. Prepartion and characterization of poly(l-lactic acid) foams. Polymer 1994, 35, 1068–1077. [Google Scholar] [CrossRef]
- Fromstein, J.D.; Woodhouse, K.A. Elastomeric biodegradable polyurethane blends for soft tissue applications. J. Biomater. Sci. Polym. Ed. 2002, 13, 391–406. [Google Scholar] [CrossRef] [PubMed]
- Rogers, L.; Said, S.S.; Meguanint, K. The effects of fabrication strategies on 3d scaffold morphology, porosity and vascular smooth muscle cell response. J. Biomater. Tissue Eng. 2013, 3, 300–311. [Google Scholar] [CrossRef]
- Janik, H.; Balas, A. Chemical structures and physical properties of cured segmental polyurethanes. Polimery 2009, 54, 195. [Google Scholar]
- Karchin, A.; Simonovsky, F.I.; Ratner, B.D.; Sanders, J.E. Melt electrospinning of biodegradable polyurethane scaffolds. Acta Biomater. 2011, 7, 3277–3284. [Google Scholar] [CrossRef] [PubMed]
- Silvestri, A.; Boffito, M.; Sartori, S.; Ciardelli, G. Biomimetic materials and scaffolds for myocardial tissue regeneration. Macromol. Biosci. 2013, 13, 984–1019. [Google Scholar] [CrossRef] [PubMed]
- Janik, H.; Marzec, M. A review: Fabrication of porous polyurethane scaffolds. Mater. Sci. Eng. C 2015, 48, 586–591. [Google Scholar] [CrossRef] [PubMed]
- Yilgor, I.; Yilgor, E.; Guler, I.G.; Ward, T.C.; Wilkies, G.L. FTIR investigation of the influence of diisocyanate symmetry on the morphology development in model segmented polyurethanes. Polymer 2006, 47, 4105–4114. [Google Scholar] [CrossRef]
- Guelcher, S.A.; Srinivasan, A.; Dumas, J.E.; Didier, J.E.; McBride, S.; Hollinger, J.O. Synthesis, mechanical properties, biocompatybility and degradation of polyurethane networks from lysine polyisocyanates. Biomaterials 2008, 29, 1762–1775. [Google Scholar] [CrossRef] [PubMed]
- Wagenseil, J.E.; Mecham, R.P. Vascular extracellular matrix and arterial mechanics. Physiol. Rev. 2009, 89, 957–989. [Google Scholar] [CrossRef] [PubMed]
- Holzapfel, G.A. Biomechanics of soft Tissue. Comput. Biomech. 2000, 7, 228–253. [Google Scholar]
- Akhtar, R.; Sherratt, M.J.; Cruickshank, J.K.; Derby, B. Characterizing the elastic properties of tissues. Materialstoday 2011, 14, 96–105. [Google Scholar] [CrossRef]
- Wlodkowic, D.; Skommer, J.; Darzynkiewicz, Z. Flow cytoetry-based apoptosis detection. Methods Mol. Biol. 2009, 559, 19–32. [Google Scholar] [PubMed]
- Lalan, S.; Pomerantseva, I.; Vacanti, J.P. Tissue engineering and its potential impact on surgery. World J. Surg. 2001, 25, 1458–1466. [Google Scholar] [CrossRef] [PubMed]

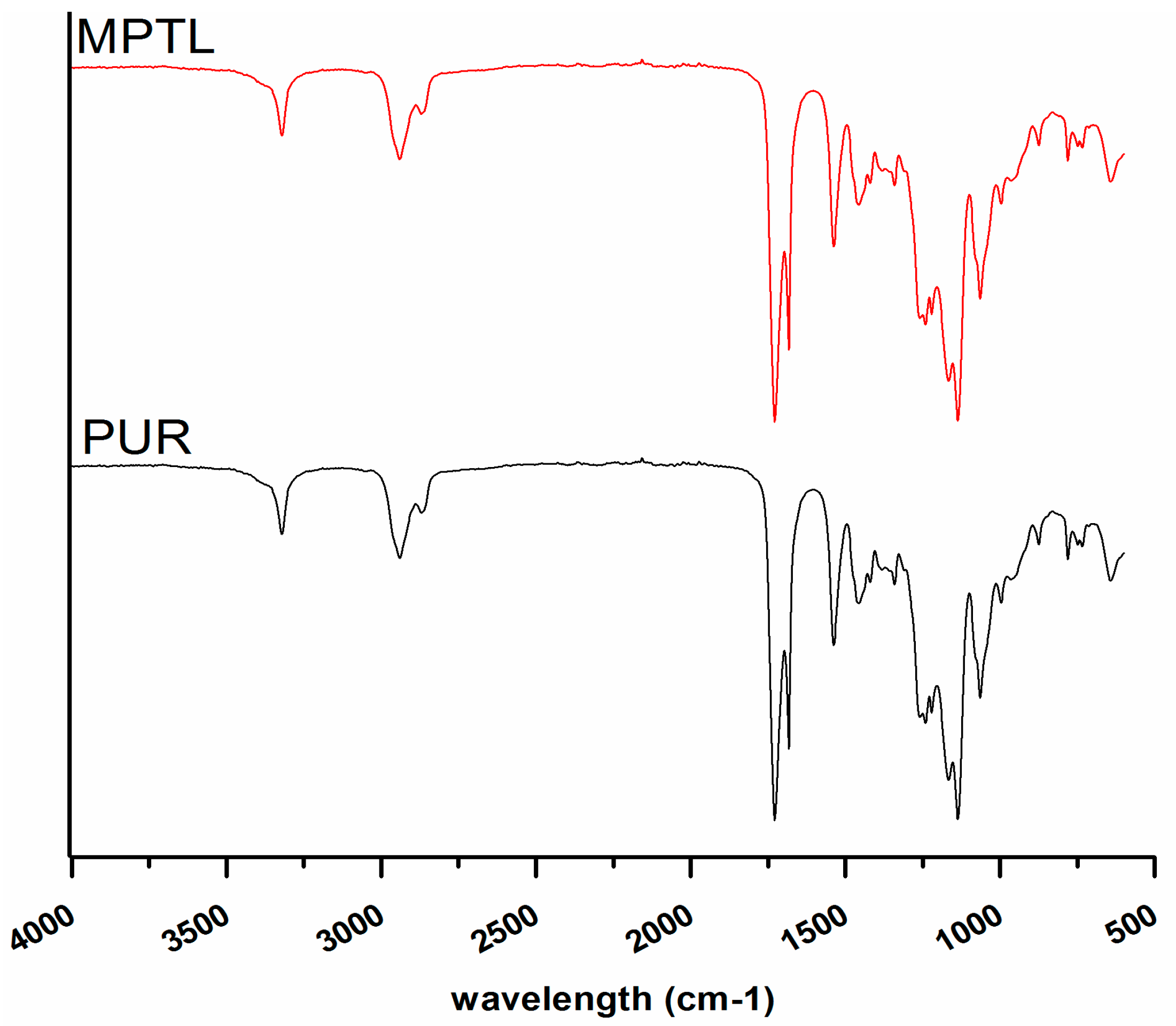

| Native PUR and MPTL Scaffold | |
|---|---|
| Wavelength (cm−1) | Assignments |
| 3319 w | N–H stretching, (urethane bonding) |
| 2930 w, 2859 w | CH3; CH2 (aliphatic) asymmetric and symmetric stretching bonding |
| 1726 vs, 1655 w | C=O stretching of non-hydrogen bonded urethane groups and well ordered and strongly hydrogen bonded urethane groups respectively |
| 1527 m | deformation bond N–H |
| 1451 w, 1420 vw, 1354 vw, 1314 s | planar bonds of symmetric and asymmetric CH2 |
| 1221 s | N–C stretching (urethane bonding) |
| 1168 s, 1138 s | CO–O stretching of ester |
| 1080 m, 1036 m | C–O stretching of urethane groups |
| 969 vw, 943 vw, 871 vw, 779 w | Out of plane bondings of C–H (bending), CH2 scissoring; CH2 wagging; NH and OH scissoring and wagging |
| Native PUR and MPTL Scaffold | |
|---|---|
| Chemical Shift (ppm) | Assignments |
| 1.0–1.25 | protons from –OH groups in BDO chain extender, which ends the PEUs chains; |
| 1.26–1.40 | protons from –NH– groups from urethane bonding: –NH–(C=O)–O– |
| 1.5–1.75 | protons from aliphatic –CH2– groups without neighborhood of functional groups |
| 2.0–2.40 | protons from aliphatic –CH2– groups in macrodiol, connected with carbonyl side of ester group; –(C=O)–O–; aliphatic –CH2– groups connected with BDO chain extender |
| 2.75–3.0 | protons from aliphatic –CH2– connected with urethane bonding from –NH– side; –NH–(C=O)–O– |
| 2.50 | Solvent—DMSO |
| 3.25–3.45 | aliphatic –CH2– groups in macrodiol, connected with ester group from the oxygen side; –O–(C=O)– |
| 3.75–4.45 | aliphatic –CH2– groups connected with urethane group from the oxygen side; –O–(C=O)–NH and protons |
| 6.9–7.15 | Signals of hydrogen bonding present in the PUR and MPTL structure |
| Sample | Water Contact Angle (Average ± SD°) |
|---|---|
| PEU | 78 ± 4 |
| MPTL | 56 ± 6 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kucińska-Lipka, J.; Gubanska, I.; Skwarska, A. Microporous Polyurethane Thin Layer as a Promising Scaffold for Tissue Engineering. Polymers 2017, 9, 277. https://doi.org/10.3390/polym9070277
Kucińska-Lipka J, Gubanska I, Skwarska A. Microporous Polyurethane Thin Layer as a Promising Scaffold for Tissue Engineering. Polymers. 2017; 9(7):277. https://doi.org/10.3390/polym9070277
Chicago/Turabian StyleKucińska-Lipka, Justyna, Iga Gubanska, and Anna Skwarska. 2017. "Microporous Polyurethane Thin Layer as a Promising Scaffold for Tissue Engineering" Polymers 9, no. 7: 277. https://doi.org/10.3390/polym9070277





