3.1. Rate of Legionella Colonization
Table 1 reports the
Legionella contamination rates, expressed as the ratio of contaminated buildings to the total number of buildings comprised in each campus, together with the number of taps per contamination severity level. In this respect, we have classified each sampling point in three levels of contamination: (i) absence of contamination, when
Legionella counts were below the detection limit of 10
2 CFU/L; (ii) low contamination, when counts comprised between 10
2 and 10
4 CFU/L; and (iii) high contamination, when counts were over 10
4 CFU/L (
Table 1). The severity level was determined by the maximum value detected among all the samples taken from each control point (i.e., hot and cold water).
Although only three campuses were completely free of
Legionella, the contamination rates were quite low since these bacteria were detected in only 12 buildings among the 41 monitored (29%). With respect to the control points, the rate of contamination was even lower, with only 23 contaminated taps among the total of 156 analyzed (14.7%). Furthermore, high-level contaminations were found in only 9 of these taps (5.8% of the total) located in 5 buildings on only 2 campuses (Nos. 5 and 6). Importantly, these buildings are used by less than 20% of the total University users and mostly by students, who tend to have sporadic attendance at the premises. This implies a low frequency of exposure and, consequently, a limited risk of infection for users [
19].
A recent meta-analysis indicated the frequent occurrence of legionellosis in occupational settings, with 27.3% of cases in office buildings [
19]. Nevertheless, only a few papers have investigated the presence of
Legionella in this kind of system, and none in university buildings. Our data indicated that the contamination rate recorded in the University of Perugia buildings was lower than that found in offices or schools in other countries, ranging from more than 30% in Germany [
16] to 60% in Japan and Hungary [
14,
15], and even lower than the 30.5% rate recorded in private apartments in Italy [
13]. Moreover, even if many of the buildings at the University of Perugia are very ancient (ranging in age from the 1960s back to the 13th century) and it has been previously shown that the rate of positive samples increases with the age of the building [
15], we found that only 1 of the 12 contaminated buildings was older than one century, while all the others were very recent (i.e., less than 30 years-old). It is important to underline that the age of a building’s water distribution system is often difficult to assess because pipelines may undergo partial or complete reconstruction. In any case, it was reported that new plumbing systems were significantly less likely to be contaminated by
Legionella only when they were less than 9 years old [
15].
It is well established that the type of hot-water production system has a strong influence on the potential threat of microbial contaminations in plumbing [
15,
20]. In this respect, the buildings of the University of Perugia, even within the same campus, were very heterogeneous (
Table 1). Some buildings, namely those located in campuses Nos. 1, 2, 3, 4 and 8, did not have hot-water production and, indeed, no contaminated taps were found therein. On the contrary, all the contaminations were found in buildings where a hot-water production system was in place, either based on single-point electrical boilers with hot-water storage located in individual premises or on a centralized facility with recirculating hot-water network. Buildings that had only a limited number of single-point heaters in a few premises showed either an absence of
Legionella (those in campuses Nos. 1, 2 and 3) or low concentrations (those in campus No. 4). Most of the contaminated taps were found in the buildings of campuses Nos. 3, 5, 6 and 7, which were characterized by either the centralized production of hot water or the presence of single-point heaters in all the premises. Nevertheless, only 9 of these taps, those in campuses Nos. 5 and 6, showed high levels of contamination (above 10
4 CFU/L). While all the control points of campus No. 6, where a centralized hot-water production system was present, were found contaminated, campus No. 5, characterized by hot water produced in each premise by electrical boilers, presented a more heterogeneous situation with only 9 taps, out of the 40 monitored, found to be contaminated by
Legionella. This corresponded to a 22% contamination rate, with 12% and 10% of low and high levels of contamination, respectively. It is well known that
Legionella is more likely to be found in hot-water mains and, furthermore, the production of hot water by centralized systems has been often associated with higher rates of contamination [
13,
14,
15,
21]. Stagnation, low circulation efficiency, and temperature drop within the hot-water network are also considered typical risk factors of large buildings with extensive plumbing systems [
15]. Nevertheless, in the largest buildings of the University, namely those of campus No. 6, no significant decrease of the hot-water temperature at distal sampling points was observed (data not shown).
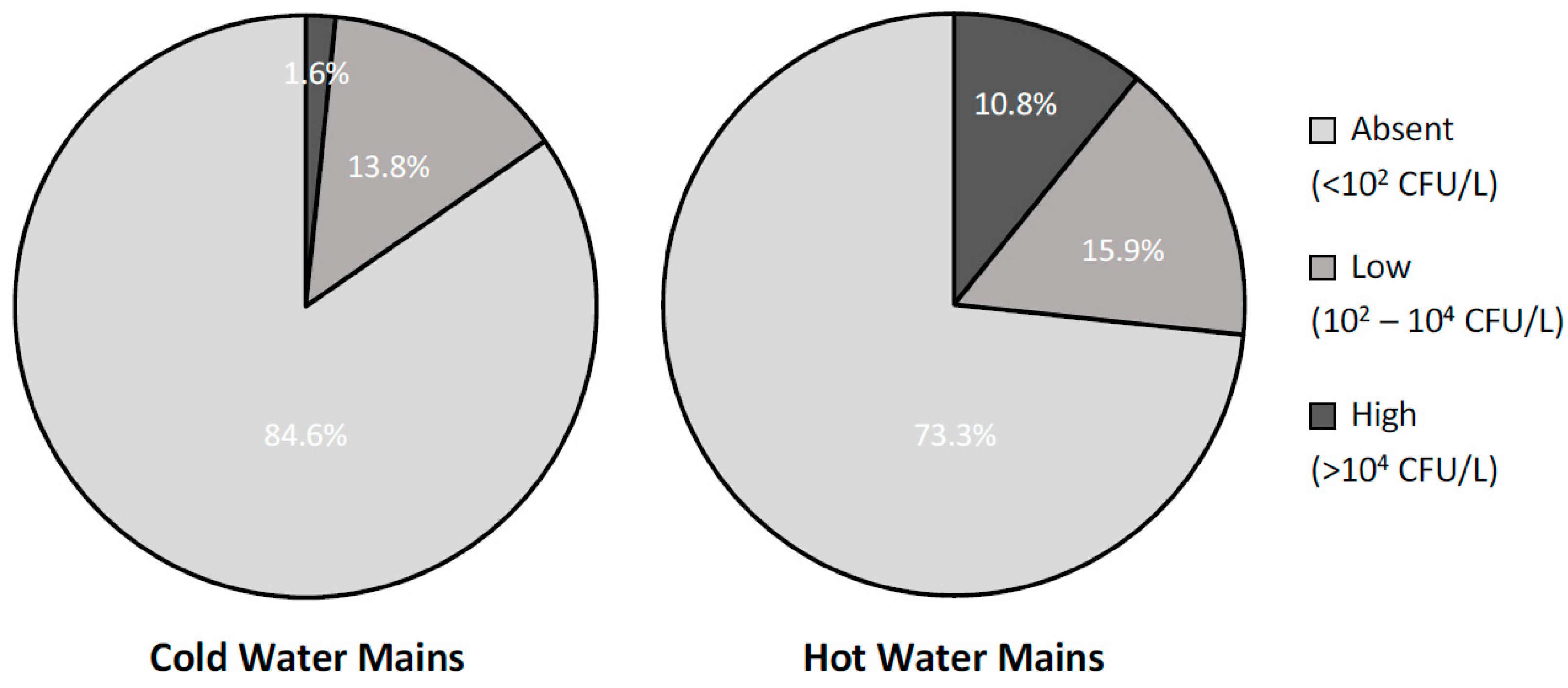
3.2. Effects of Water Heating
To further investigate the effects of water heating on the presence of
Legionella in building plumbing,
Figure 2 reports the contamination rates, divided by severity levels, found in samples collected from the cold- and hot-water distribution networks. As expected, hot-water mains showed a statistically significant higher rate of contamination than the cold-water ones (26.7% and 15.4%, respectively; X
2 = 5,
p = 0.02) and, in particular, a much higher rate of high-severity level contaminations (10.8% and 1.6%, respectively; X
2 = 10,
p = 0.001). Interestingly, all the contaminated samples from cold-water mains were taken in buildings where a hot-water production system was also in place and where water samples from the hot-water mains were contaminated as well. Furthermore, if only post-flush samples, i.e., those representing the status of the entire network rather than a single tap, were considered, the rate of contaminated samples from the cold-water mains dropped to 8.1% with no high-level contaminations present. This evidence suggests that the presence of
Legionella in the cold-water mains might be due, at least in part, to possible cross-contaminations with the hot-water ones occurring in the terminal part of the plumbing.
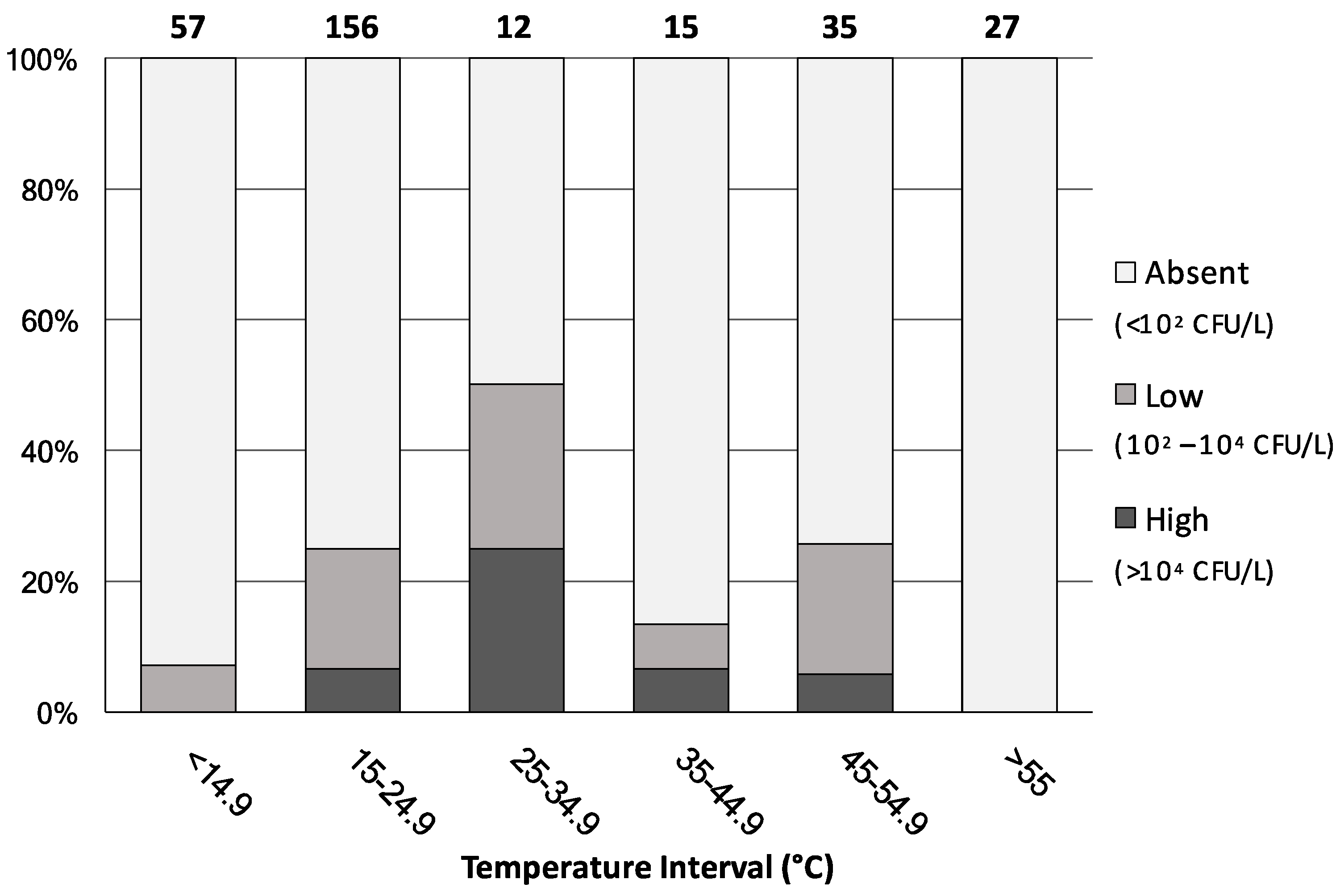
Figure 3 shows the percentage distribution of all 302 water samples, irrespective of their water-network origin, analysed by level of contamination severity and water-temperature interval.
When water temperature was below 14.9 °C or above 55 °C, the rate of
Legionella colonization was either minimal or totally absent, respectively. On the contrary, the highest proportion of the
Legionella positive samples was mainly observed in the 25–55 °C temperature ranges, where almost the totality of the 62 samples came from hot-water mains. Interestingly, among the 156 samples showing a water temperature of between 15 and 24.9 °C, 39 (25% of the total) were found contaminated with
Legionella. These samples originated either from the cold-water mains or from the hot-water network where the hot-water production system was shut-off or not working properly. These data confirm that water temperature represents a key risk factor for
Legionella colonization and further support the international recommended value of 55 °C for hot-water temperature [
9]. Nevertheless, in public buildings it often happens that the temperature of hot water is found below 50 °C, because of energy-saving measures, to prevent the risk of burns, or due to malfunctions in the water-heating and distribution systems [
15,
21]. Our results also indicate the occurrence of this microorganism in cold-water samples. Indeed, although the growth of
Legionella is believed to be restricted to temperatures between 25 and 42 °C, it has been isolated from natural freshwater environments at temperatures below 15 °C [
22] and, recently, detected in public and private cold-water taps across the United States [
23].
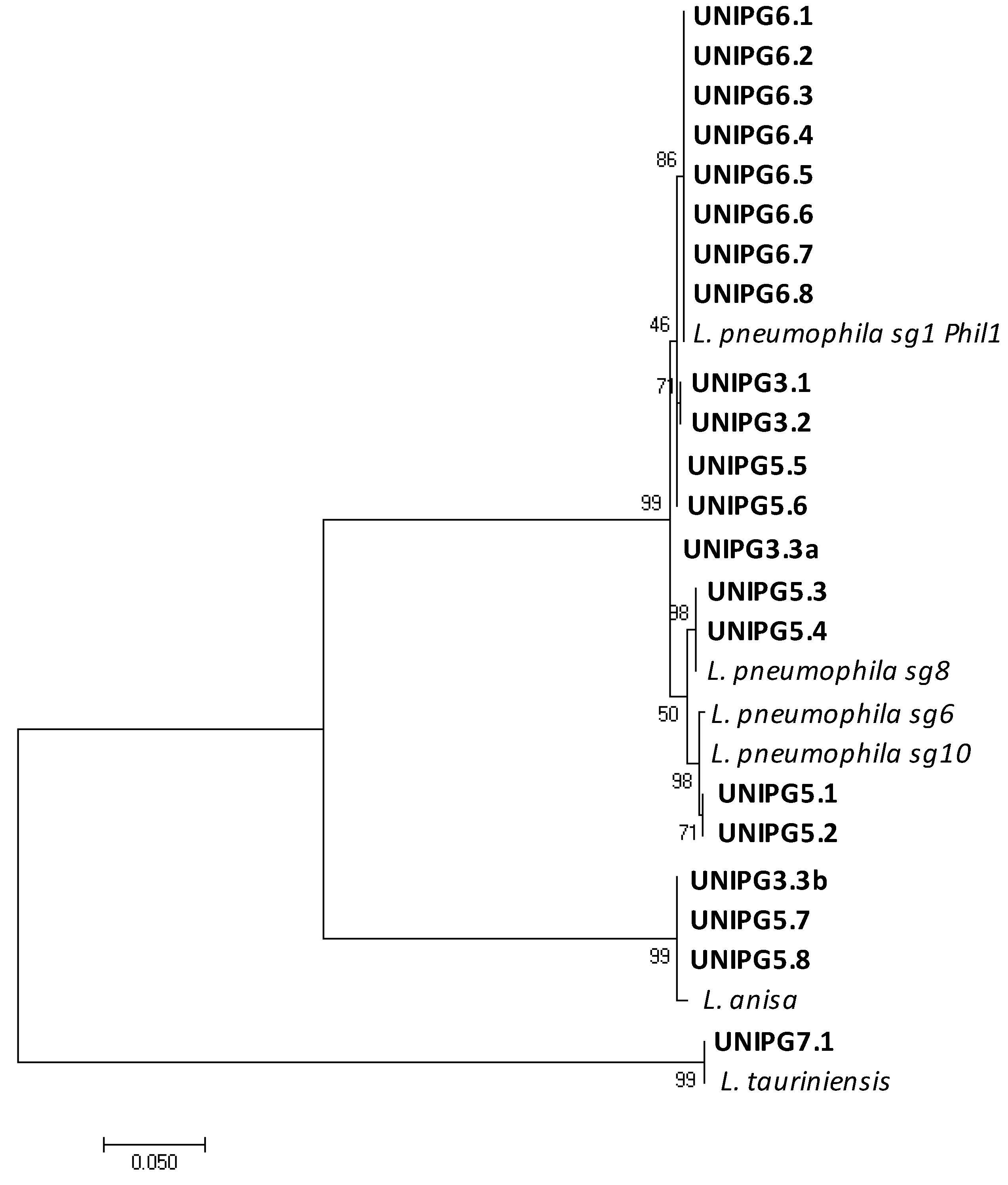
3.3. Phylogenetic Analysis
Considering that several species of
Legionella have been identified but only few of them have been associated with human disease [
1], we used a molecular analysis based on
mip gene sequencing to identify the
Legionella species and to differentiate the serogroups of
L. pneumophila within the strains retrieved from the University buildings’ plumbing (
Table 1 and
Figure 4).
Since several isolates were cultured from each water sample, all the sequences were aligned, and a representative one was chosen from each group of isolates obtained from the same control-point tap and identified as the same
Legionella species. The phylogenetic tree reported in
Figure 4 shows the genetic relationships among the
mip gene sequences of the 21 isolates found in this study and those of closely related reference strains of
Legionella. The presence of
L. pneumophila was shown in 17 taps, with sg 1 being the most represented (13 taps located in campuses Nos. 3, 5 and 6), while sg 8 and sg 6–10 were found only in 4 contaminated taps of campus No. 5. Other distant related
Legionella species were also found, namely
L. anisa (in 1 tap of campus No. 3 and 2 taps of campus No. 5) and
L. tauriniensis in 1 tap of campus No. 7. Interestingly, only a single species of
Legionella was found in each contaminated tap, with the only exception of one tap in a building of campus No. 3 where two different species were recovered, namely
L. pneumophila sg 1, and
L. anisa. As pointed out for the contamination rates, campus No. 5 showed a high heterogeneity also in respect of the
Legionella species found in the hot water from the different electrical boilers (
L. pneumophila sg 1, sg 8, sg 6–10 and
L. anisa). On the contrary, in all the control points of campus No. 6, characterized by a centralized hot-water production system, only
L. pneumophila sg1 was found. This evidence further supports the hypothesis that
Legionella growth and proliferation may likely occur inside the hot-water production system and from there spread to the different taps. Our data are largely in agreement with other works indicating that strains of
L. pneumophila, the species mostly associated to legionellosis, are those mostly often found to contaminate taps of private apartments, hotels and hospitals in Italy [
13] as well as buildings in Hungary, Germany, the USA and Japan [
14,
15,
16,
23]. Nevertheless, we also recovered several isolates of
L. anisa, a species already found in building plumbing [
14] and known to be associated with human infections as one of the pathogens causing Pontiac fever [
1]; as well as one isolate identified as
L. tauriniensis, a species recently isolated from a hospital humidifier in Turin, Italy [
24] but never linked to human disease.
3.4. Remedial Actions in the Contaminated Buildings
Italian and international guidelines suggest the intervention needed for the prevention of
Legionella contamination in the plumbing of premises based both on
Legionella concentration and positive sample rate [
9,
10]. While international guidelines usually define 10
3 CFU/L as the limit of the
Legionella count for public health concerns, the Italian ones consider a system completely under control only when
Legionella is absent in all samples. With counts up to 10
4 CFU/L, carrying out disinfection of the water-distribution system is suggested when 20% or 50% of the collected samples per building are positive, according to Italian and international guidelines respectively. However, immediate action is generally recommended in the case of
Legionella counts over 10
4 CFU/L. In the case study reported here,
Legionella was found in five campuses but in only two cases, namely campuses Nos. 5 and 6, the severity levels of contamination were above the limit at which a remedial action is required (
Table 2). In addition, the building of the laboratory animal facility in campus No. 3 required disinfection because, despite a contamination classified as a low level of severity,
Legionella was present in most of the control points assessed (
Table 2). In the two remaining cases, namely campuses Nos. 4 and 7, no immediate decontamination was necessary because of the low levels of severity and rates recorded. Furthermore, in the case of campus No. 7 the contamination was ascribed to a strain of
L. tauriniensis, a species never associated with clinical cases.
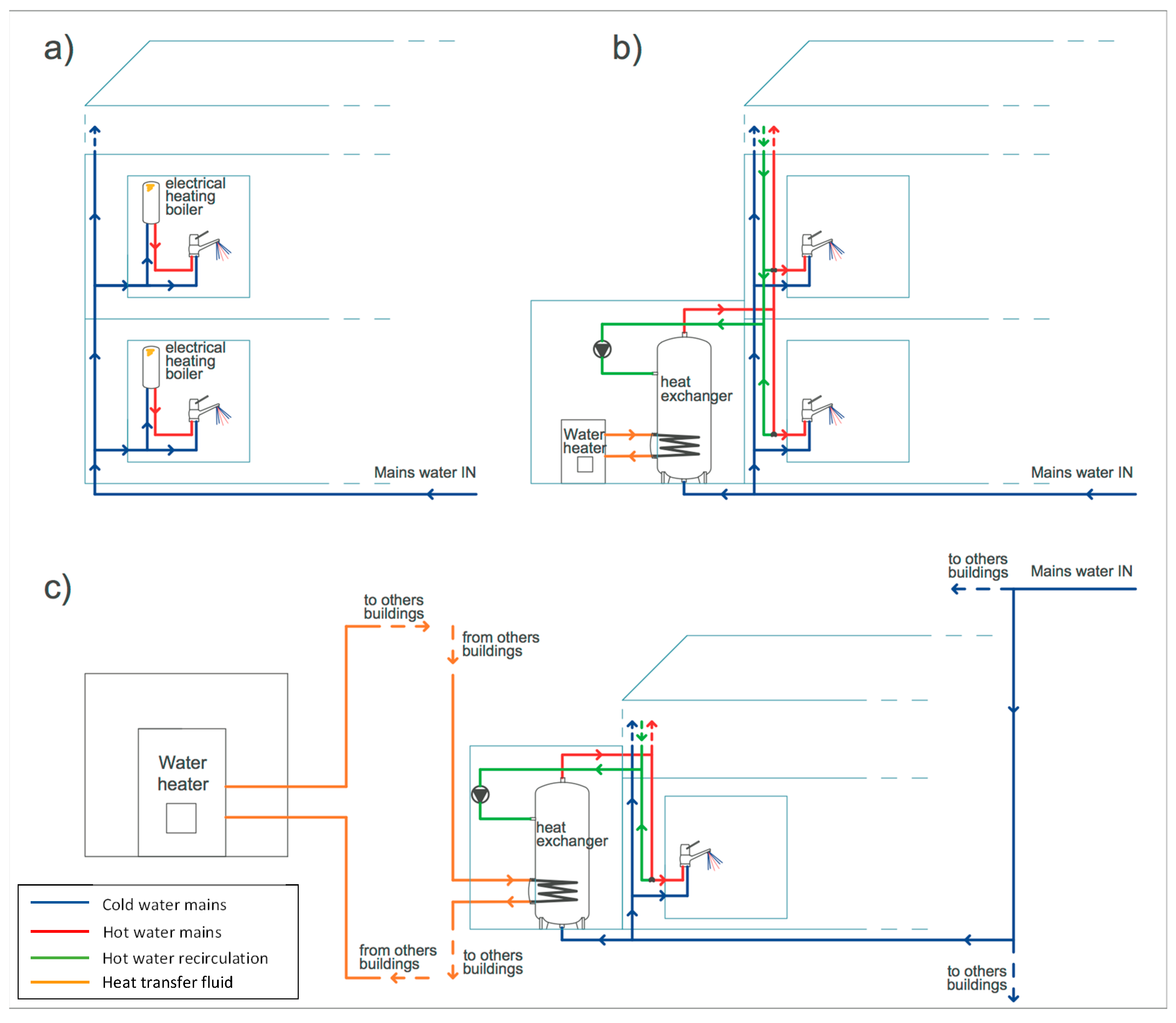
The type of remedial action implemented was based on the characteristics of the hot-water production and distribution systems of each campus (
Figure 5) and on the indications of treatment methods for both emergency and long-term measures provided by Italian and European Guidelines [
9,
10]. To confirm the effectiveness of the decontamination interventions, follow-up monitoring of the presence of
Legionella was carried out according to Italian guidelines by repeating the water sampling of the positive taps 48 h, 1 and 3 months after the intervention [
10] and the results are reported in
Table 2.
Campus No. 5 is composed of six new buildings where each premise has its own single-point electrical boiler with hot-water storage (
Figure 5a). As already underlined, due to the system of hot-water production, these buildings presented the highest heterogeneity of
Legionella contamination, both in terms of severity level and
Legionella species recovered. Indeed, to monitor the
Legionella presence in this campus properly, a considerable sampling effort, based on the analysis of water samples from 40 different control points, was undertaken. All the taps served by electrical boilers set at a temperature higher than 55 °C were free of
Legionella, while contaminations were found only within the boilers that were shut-off or set below 45 °C, with the only exception of one tap where the hot-water temperature was 53 °C. Nevertheless, the electrical boilers allowed higher hot-water temperatures to be achieved and maintained. A thermal disinfection of the contaminated boilers was thus implemented, raising and maintaining the water temperature above the level at which
Legionella cells do not survive (>60 °C) [
2,
9]. This approach proved to be effective as
Legionella was absent in the water samples taken in the following monitoring period (
Table 2). The effectiveness of constant maintenance of the hot-water temperature above 60 °C has been largely demonstrated in hospitals, hotels and households, particularly those with small hot-water production systems, such as single-point electrical boilers [
15,
16]. Indeed, provided there is sufficient heating capacity, this approach is relatively easy to implement and monitor, although increasing energy consumption and risk of scalding for users may be possible disadvantages [
9,
15].
The building hosting the laboratory animal facility was the only one of campus No. 3 showing
Legionella contamination. This building featured a centralized hot-water production system, where water is stored in a tank, heated via a coil (heat exchanger) from a boiler and then distributed to the premises (
Figure 5b). In this case, a combination of hyperchlorination (75 mg/L of sodium hypochlorite for 3 h) and thermal shock (70 °C for 90 min) was implemented [
9,
25]. Furthermore, the thermal treatment was repeated every week. This intervention was proven to be successful in the follow-up monitoring as no recolonization of the plumbing system by
Legionella was observed (
Table 2). Chlorine is often used in the treatment of hot-water systems, although consistent effective levels, especially at distal points, may be difficult to achieve in large plumbing networks and in the presence of hot water or above pH 7 [
9,
25].
Campus No. 6 features the most complicated hot-water network, with centralized systems where hot water is produced and stored by three heat exchangers, one for each of the three buildings, using the room heating system coming from a centralized facility (
Figure 5c). High levels of
L.
pneumophila sg 1 were found in the samples taken from the hot-water taps and in the heat exchangers, despite the hot-water production system being off at the time of sampling. In fact, sampling was performed in the summer period when room heating was not necessary and, consequently, hot water was not produced. In this period, the daily average ambient temperature ranged from 20 to 32 °C, and, in fact, the temperature of the water samples analyzed ranged from 23 to 25 °C, a level that does not limit
Legionella proliferation.
Legionella was not found in cold-water samples taken after flushing, as well as in the common part of the water distribution system (network inlet, reservoir tank, water softener), indicating that the contamination was limited to the hot-water mains and originated inside the heat exchanger, where water stagnation and presence of loose deposits may have favored the growth of
Legionella [
6]. After turning on the hot-water production system, water temperature ranged, during the day, between 22 and 48 °C. This was due to the hot-water production system, based on heat exchange with the heat-transfer fluid, not enabling values high enough for a thermal disinfection to be achieved [
9,
10,
25,
26]. Consequently, a chemical treatment with silver hydrogen peroxide was carried out by adding 6 kg/m
3 of disinfectant directly to the heat exchanger, filling the hot-water mains, and allowing this to remain in contact for 12 h. One week after disinfection,
Legionella was absent in all samples, while after one month hot-water samples were contaminated again, though at low levels of severity (
Table 2). After four months, the contamination overreached the levels of before disinfection (
Table 2), suggesting that the re-growth of
Legionella was favored by the conditions inside the heat exchanger, probably because of the presence of loose deposits and a permissive temperature for cell growth. Since the treatment with silver hydrogen peroxide was shown to be effective in controlling
Legionella growth only in the short-term, it was decided to close down the independent hot-water production and distribution systems (
Figure 5c) to prevent infections. Despite treatment with a stable concentrated solution of hydrogen peroxide and silver being able to exploit the bactericidal action of the two components and their synergy, this approach has been, to date, used in only a limited way for
Legionella decontamination, especially as an emergency measure. It should, therefore, be further validated in real-case scenarios to ensure its effectiveness [
9,
25].