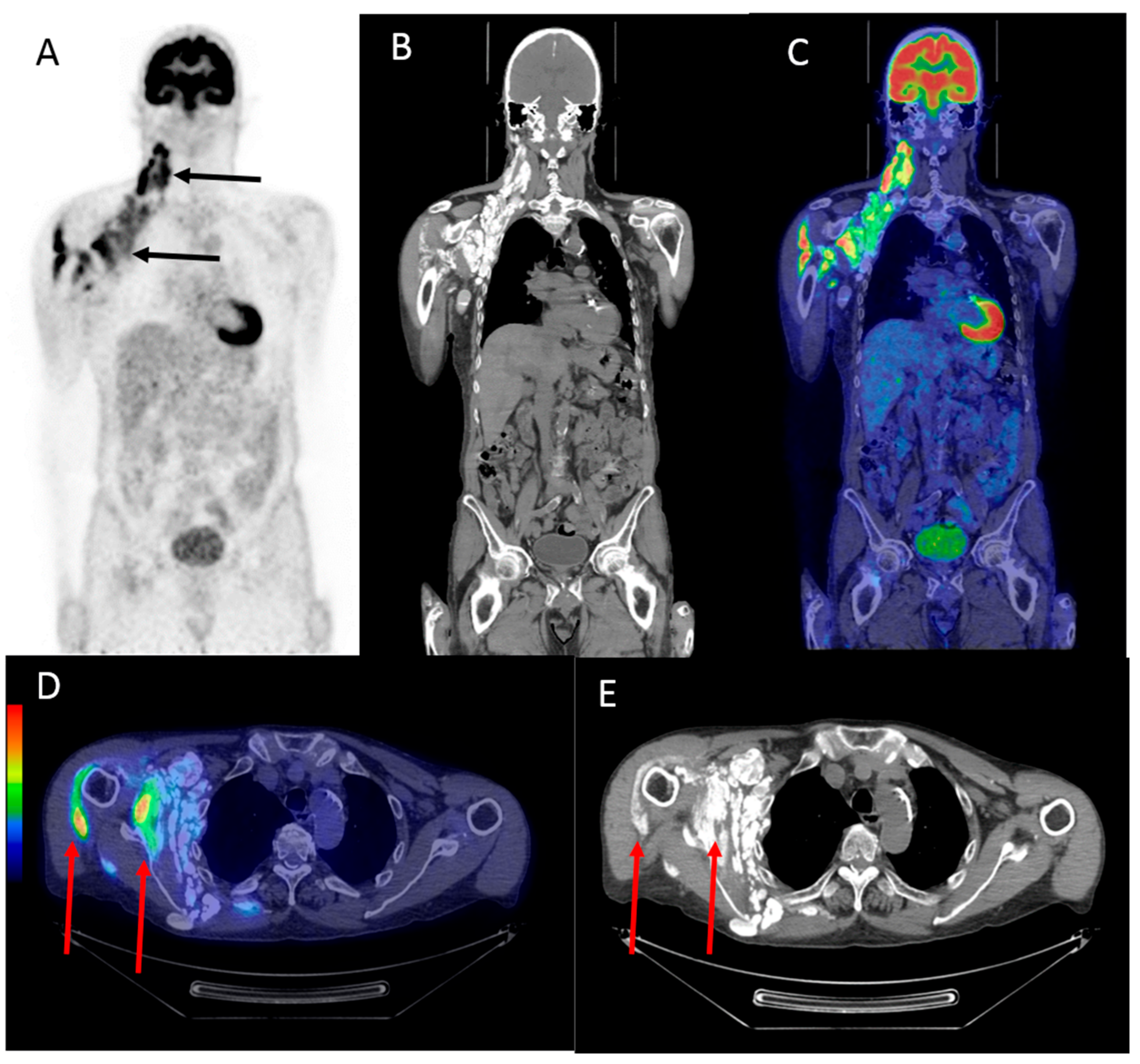
Avid 18F-FDG Uptake in Idiopathic Tumoral Calcinosis Mimicking Lymph Node Metastasis
Abstract
:1. Introduction
2. Case Report
3. Discussion
Acknowledgments
Conflicts of Interest
References
- Tezelamn, S.; Siperstein, A.E.; Duh, Q.Y.; Clark, O.H. Tumoral calcinosis Controversies on the etiology and alternatives in the treatment. Arch. Surg. 1993, 128, 737–744. [Google Scholar] [CrossRef]
- Binnani, P.; Aggarwal, V.; Bahadur, M.M.; Fulara, N. Tumoral calcinosis (Teutschlander disease) in a dialysis patient. Indian J. Nephrol. 2008, 18, 122–124. [Google Scholar] [CrossRef] [PubMed]
- Grellier, J.-F.; Lussato, D.; Queneau, M.; Guernou, M.; Songy, B. Secondary Hyperparathyroidism with “Superscan-Like” Hypermetabolic FDG PET/CT Pattern. Clin. Nucl. Med. 2015, 40, 888–889. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.E. Guyton and Hall Textbook of Medical Physiology; W.B. Saunders: Philadelphia, PA, USA, 2016. [Google Scholar]
- Liu, Y. Scintigraphic Images of Massive Tumoral Calcinosis. Clin. Nucl. Med. 2016, 41, 504–505. [Google Scholar] [CrossRef] [PubMed]
- Olsen, K.M.; Chew, F.S. Tumoral Calcinosis: Pearls polemics and alternative possibilities. Radiographics 2006, 26, 871–885. [Google Scholar] [CrossRef] [PubMed]
- D’souza, M.; Jaimini, A.; Bansal, A.; Tripathi, M.; Sharma, R.; Mondal, A.; Tripathi, R.P. FDG-PET/CT in lymphoma. Indian J. Radiol. Imaging 2013, 23, 354–365. [Google Scholar] [CrossRef] [PubMed]
- Okuyama, C.; Kubota, T.; Matsushima, S.; Ushijima, Y.; Nishimura, T. Intense F-18 FDG accumulation idiopathic tumoral calcinosis. Clin. Nucl. Med. 2009, 34, 230–232. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, K.K.; Karunanithi, S.; Jain, S.; Kumar, R. Ovarian carcinoma producing parathyroid hormone-related protein causing hypercalcemia and metastatic calcification detected on (18)F-FDG PET-CT. Indian J. Nucl. Med. 2013, 28, 237–239. [Google Scholar] [PubMed]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strandberg, J.; Zacho, H.D. Avid 18F-FDG Uptake in Idiopathic Tumoral Calcinosis Mimicking Lymph Node Metastasis. Diagnostics 2017, 7, 60. https://doi.org/10.3390/diagnostics7040060
Strandberg J, Zacho HD. Avid 18F-FDG Uptake in Idiopathic Tumoral Calcinosis Mimicking Lymph Node Metastasis. Diagnostics. 2017; 7(4):60. https://doi.org/10.3390/diagnostics7040060
Chicago/Turabian StyleStrandberg, Jesper, and Helle D. Zacho. 2017. "Avid 18F-FDG Uptake in Idiopathic Tumoral Calcinosis Mimicking Lymph Node Metastasis" Diagnostics 7, no. 4: 60. https://doi.org/10.3390/diagnostics7040060




