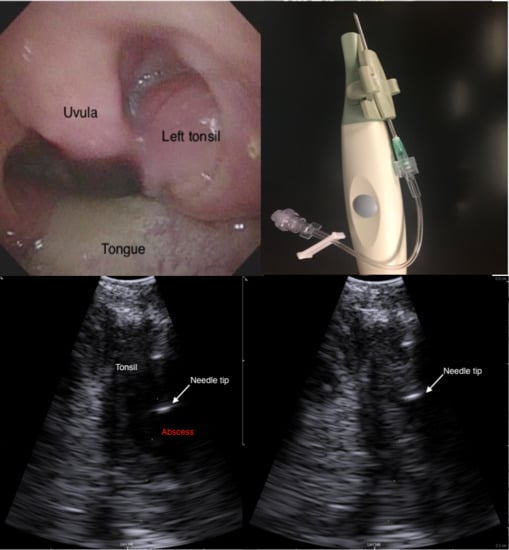
A Novel Technique for Intraoral Ultrasound-Guided Aspiration of Peritonsillar Abscess
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Herzon, F.S.; Harris, P. Peritonsillar abscess: Incidence, current management practices, and a proposal for treatment guidelines. Laryngoscope 1995, 105, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, C.; Biet, A.; Zaatar, R.; Strunski, V. Parapharyngeal abscess: Diagnosis and treatment. Eur. Arch. Oto-Rhino-Laryngol. 2008, 265, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Passy, V. Pathogenesis of peritonsillar abscess. Laryngoscope 1994, 104, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Powell, J.; Wilson, J.A. An evidence-based review of peritonsillar abscess. Clin. Otolaryngol. 2012, 37, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Shaul, C.; Koslowsky, B.; Rodriguez, M.; Schwarz, Y.; Muahnna, N.; Peleg, U.; Sichel, J.Y. Is needle aspiration for peritonsillar abscess still as good as we think? A long-term follow-up. Ann. Otol. Rhinol. Laryngol. 2015, 124, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.R.; Hedges, J.R. Clinical Procedures in Emergency Medicine; Elsevier Health Sciences: Amsterdam, The Netherlands, 2009. [Google Scholar]
- Scott, P.M.J.; Loftus, W.K.; Kew, J.; Ahuja, A.; Yue, V.; Van Hasselt, C.A. Diagnosis of peritonsillar infections: A prospective study of ultrasound, computerized tomography and clinical diagnosis. J. Laryngol. Otol. 1999, 113, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Froehlich, M.H.; Huang, Z.; Reilly, B.K. Utilization of ultrasound for diagnostic evaluation and management of peritonsillar abscesses. Curr. Opin. Otolaryngol. Head Neck Surg. 2017, 25, 163–168. [Google Scholar] [CrossRef] [PubMed]
- Nogan, S.; Jandali, D.; Cipolla, M.; DeSilva, B. The use of ultrasound imaging in evaluation of peritonsillar infections. Laryngoscope 2015, 125, 2604–2607. [Google Scholar] [CrossRef] [PubMed]
- Rehrer, M.; Mantuani, D.; Nagdev, A. Identification of peritonsillar abscess by transcutaneous cervical ultrasound. Am. J. Emerg. Med. 2013, 31, 267.e1–267.e3. [Google Scholar] [CrossRef] [PubMed]
- Filho, B.C.A.; Sakae, F.A.; Sennes, L.U.; Imamura, R.; de Menezes, M.R. Intraoral and transcutaneous cervical ultrasound in the differential diagnosis of peritonsillar cellulitis and abscesses. Braz. J. Otorhinolaryngol. 2006, 72, 377–381. [Google Scholar] [CrossRef]
- Fordham, M.T.; Rock, A.N.; Bandarkar, A.; Preciado, D.; Levy, M.; Cohen, J.; Safdar, N.; Reilly, B.K. Transcervical ultrasonography in the diagnosis of pediatric peritonsillar abscess. Laryngoscope 2015, 125, 2799–2804. [Google Scholar] [CrossRef] [PubMed]
- Salihoglu, M.; Eroglu, M.; Yildirim, A.O.; Cakmak, A.; Hardal, U.; Kara, K. Transoral ultrasonography in the diagnosis and treatment of peritonsillar abscess. Clin. Imaging 2013, 37, 465–467. [Google Scholar] [CrossRef] [PubMed]
- Kew, J.; Ahuja, A.; Loftus, W.K.; Scott, P.M.; Metreweli, C. Peritonsillar abscess appearance on intra-oral ultrasonography. Clin. Radiol. 1998, 53, 143–146. [Google Scholar] [CrossRef]
- Strong, E.B.; Woodward, P.J.; Johnson, L.P. Intraoral ultrasound evaluation of peritonsillar abscess. Laryngoscope 1998, 105, 779–782. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, K.; Jones, A.S.; Shah, K.; Smethurst, A. The role of ultrasound in the management of peritonsillar abscess. J. Laryngol. Otol. 1994, 108, 610–612. [Google Scholar] [CrossRef] [PubMed]
- Costantino, T.G.; Satz, W.A.; Dehnkamp, W.; Goett, H. Randomized Trial Comparing Intraoral Ultrasound to Landmark-based Needle Aspiration in Patients with Suspected Peritonsillar Abscess. Acad. Emerg. Med. 2012, 19, 626–631. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lyon, M.; Blaivas, M. Intraoral ultrasound in the diagnosis and treatment of suspected peritonsillar abscess in the emergency department. Acad. Emerg. Med. 2005, 12, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Blaivas, M.; Theodoro, D.; Duggal, S. Ultrasound-guided drainage of peritonsillar abscess by the emergency physician. Am. J. Emerg. Med. 2003, 21, 155–158. [Google Scholar] [CrossRef] [PubMed]
- Haeggström, D.A.; Gustafsson, D.O.; Engquist, D.S.; Engström, D.C.-F. Intraoral Ultrasonography in the Diagnosis of Peritonsillar Abscess. Otolaryngol. Head Neck Surg. 1993, 108, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Buckley, A.R.; Moss, E.H.; Blokmanis, A. Diagnosis of peritonsillar abscess: Value of intraoral sonography. Am. J. Roentgenol. 1994, 162, 961–964. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Vintzileos, W.; Gordish-Dressman, H.; Bandarkar, A.; Reilly, B.K. Pediatric peritonsillar abscess: Outcomes and cost savings from using transcervical ultrasound. Laryngoscope 2017, 127, 1924–1929. [Google Scholar] [CrossRef] [PubMed]
- Prokofieva, A.; Modayil, V.; Chiricolo, G.; Ash, A.; Raio, C. Ultrasound-guided drainage of peritonsillar abscess: Shoot with your hockey-stick. Int. Emerg. Med. 2016, 11, 883–884. [Google Scholar] [CrossRef] [PubMed]
- Todsen, T. Surgeon-performed ultrasonography. Dan. Med. J. 2017, 64. PMID:29115210. [Google Scholar]
- Tolsgaard, M.G.; Todsen, T.; Sorensen, J.L.; Ringsted, C.; Lorentzen, T.; Ottesen, B.; Tabor, A. International multispecialty consensus on how to evaluate ultrasound competence: A delphi consensus survey. PLoS ONE 2013, 8, e57687. [Google Scholar] [CrossRef] [PubMed]
- Todsen, T.; Melchiors, J.; Charabi, B.; Henriksen, B.; Ringsted, C.; Konge, L.; von Buchwald, C. Competency-based assessment in surgeon-performed head and neck ultrasonography: A validity study. Laryngoscope 2018, 128, 1346–1352. [Google Scholar] [CrossRef] [PubMed]
- Todsen, T.; Tolsgaard, M.G.; Olsen, B.H.; Henriksen, B.M.; Hillingsø, J.G.; Konge, L.; Jensen, M.L.; Ringsted, C. Reliable and valid assessment of point-of-care ultrasonography. Ann. Surg. 2015, 261, 309–315. [Google Scholar] [CrossRef] [PubMed]






© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Todsen, T.; Stage, M.G.; Holst Hahn, C. A Novel Technique for Intraoral Ultrasound-Guided Aspiration of Peritonsillar Abscess. Diagnostics 2018, 8, 50. https://doi.org/10.3390/diagnostics8030050
Todsen T, Stage MG, Holst Hahn C. A Novel Technique for Intraoral Ultrasound-Guided Aspiration of Peritonsillar Abscess. Diagnostics. 2018; 8(3):50. https://doi.org/10.3390/diagnostics8030050
Chicago/Turabian StyleTodsen, Tobias, Mads Georg Stage, and Christoffer Holst Hahn. 2018. "A Novel Technique for Intraoral Ultrasound-Guided Aspiration of Peritonsillar Abscess" Diagnostics 8, no. 3: 50. https://doi.org/10.3390/diagnostics8030050