Effect of Yang-Style Tai Chi on Gait Parameters and Musculoskeletal Flexibility in Healthy Chinese Older Women
Abstract
:1. Introduction
2. Methods
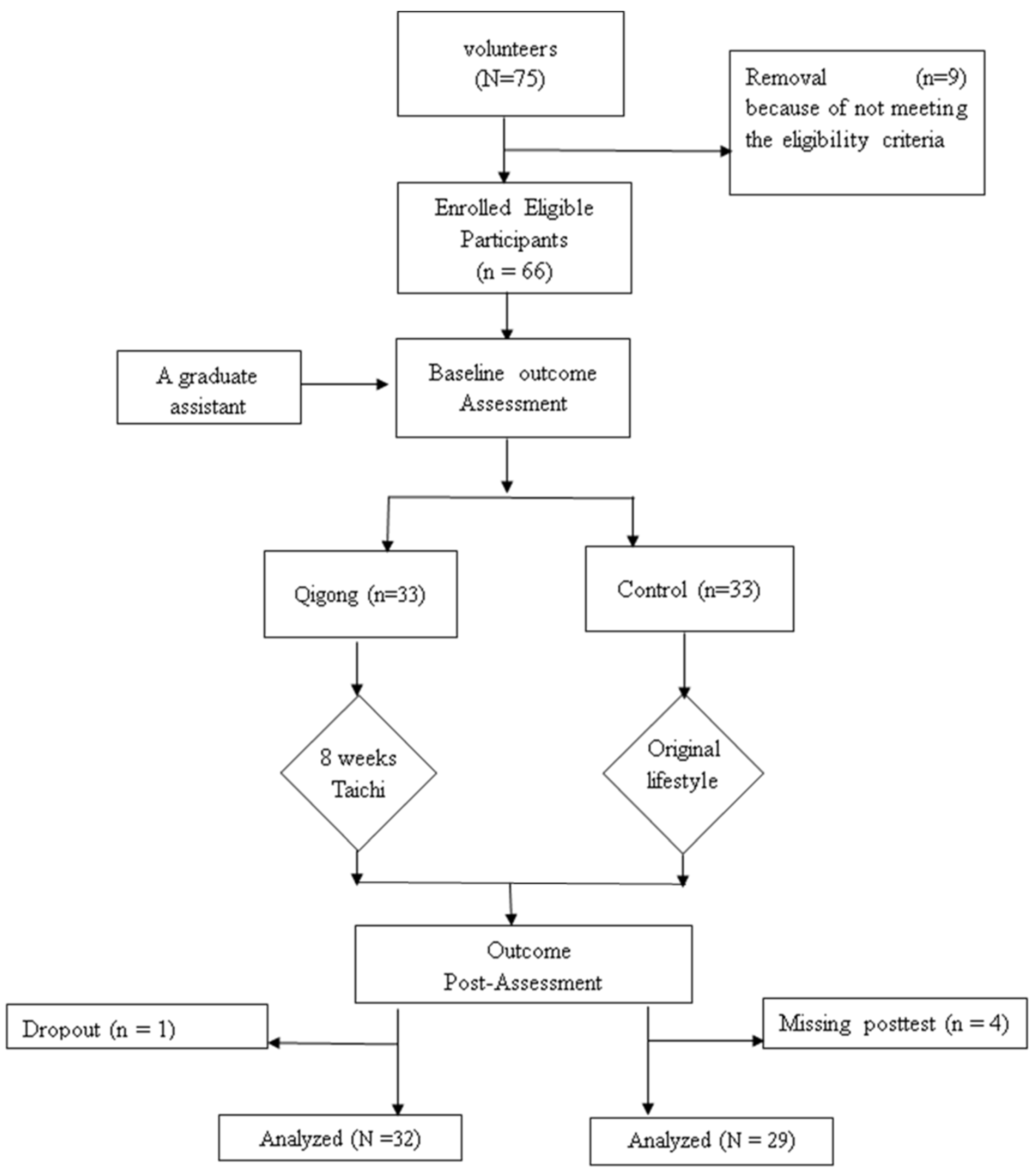
2.1. Study Design
2.1.1. Study Participants
2.1.2. Randomization and Intervention Program
2.1.3. Adverse Event
2.2. Measurement
2.2.1. Physical Activity Level
2.2.2. Primary Outcomes
2.2.3. Secondary Outcome Measures
2.2.4. Statistical Analysis
3. Results
3.1. Study Participants
3.2. Effects of an 8-Week Tai Chi Training Program on Gait Parameters
3.3. Effects of an 8-Week Tai Chi Training Program on Flexibility
3.4. Effects of an 8-Week Tai Chi Training Program on Joint Range of Motion
4. Discussion
Study Limitation
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Zeng, Y.; George, L. Family dynamics of 63 million (in 1990) to more than 330 million (in 2050) elders in China. Demogr. Res. 2000, 2, 1–48. [Google Scholar] [CrossRef]
- Lou, L.; Zou, L.; Fang, Q.; Wang, H.; Liu, Y.; Tian, Z.; Han, Y. Effect of Taichi Softball on Function-Related Outcomes in Older Adults: A Randomized Control Trial. Evid. Based Complement. Altern. Med. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Salzman, B. Gait and balance disorders in older adults. Am. Fam. Phys. 2010, 82, 61–68. [Google Scholar]
- Dong, X.; Chang, E.S.; Simon, M.A. Physical function assessment in a community-dwelling population of US Chinese older adults. J. Gerontol. Ser. A 2014, 69, S31–S38. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Marjorie, W.H. Motor Control Translating Research into Clinical Practice, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007. [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key Indicators of Well-Being; Federal Interagency Forum on Aging-Related Statistics: Washington, DC, USA, 2012. [Google Scholar]
- Hardy, S.E.; Perera, S.; Roumani, Y.F.; Chandler, J.M.; Studenski, K.A. Improvement in usual gait speed predicts better survival in older adults. J. Am. Geriatrics Soc. 2007, 55, 1727–1734. [Google Scholar] [CrossRef] [PubMed]
- Lopopolo, R.B.; Greco, M.; Sullivan, D.; Craik, R.L.; Mangione, K.K. Effect of therapeutic exercise on gait speed community-dwelling elderly people: A meta-analysis. Phys. Ther. 2006, 86, 520–540. [Google Scholar] [PubMed]
- Zou, L.; Wang, H.; Xiao, Z.; Fang, Q.; Zhang, M.; Li, T.; Du, G.; Liu, Y. Tai chi for health benefits in patients with multiple sclerosis: A systematic review. PLoS ONE 2017, 12, e0170212. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Wei, A.; Lu, Y.; Yu, B.; Chen, W.; Lu, Y.; Liu, Y.; Yu, D.; Zou, L. Simplified tai chi program training versus traditional tai chi on the functional movement screening in older adults. Evid. Based Complement. Altern. Med. 2016, 2016, 1–6. [Google Scholar]
- Zou, L.; SasaKi, J.E.; Wang, H.; Xiao, Z.; Fang, Q.; Zhang, M. A Systematic Review and Meta-Analysis Baduanjin Qigong for Health Benefits: Randomized Controlled Trials. Evid. Based Complement. Altern. Med. 2017, 2017, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Chaoyi, W. Traditional Chinese Baduanjin Qigong for Older Adults: A Mini-Review. Open Access J. Gerontol. Geriatr. Med. 2017, 1, 555561. [Google Scholar]
- Li, F.; Harmer, P.; Fisher, K.J.; McAuley, E.; Chaumeton, N.; Eckstrom, E.; Wilson, N.L. Tai Chi and fall reductions in older adults: A randomized controlled trial. J. Gerontol. Ser. A 2005, 60, 187–194. [Google Scholar] [CrossRef]
- Choi, J.H.; Moon, J.S.; Song, R. Effects of Sun-style Tai Chi exercise on physical fitness and fall prevention in fallprone older adults. J. Adv. Nurs. 2005, 51, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Ding, L.; Chen, B.; Zou, L.; Tian, G. An investigation of motivational differences for participants in Chinese martial arts. Asia Pac. J. Sport Soc. Sci. 2015, 4, 53–66. [Google Scholar] [CrossRef]
- Li, F.; Harmer, P.; Fitzgerald, K.; Eckstrom, E.; Stock, R.; Galver, J.; Maddalozzo, G.; Batya, S. Tai chi and postural stability in patients with Parkinson’s disease. N. Engl. J. Med. 2012, 366, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Amano, S.; Nocera, J.R.; Vallabhajosula, S.; Juncos, J.; Gregor, R.; Waddell, D.; Wolf, S.; Hass, C. The effect of Tai Chi exercise on gait initiation and gait performance in persons with Parkinson’s disease. Parkinsonism Relat. Disord. 2013, 19, 955–960. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Li, X.Y.; Gong, L.; Zhu, Y.; Hao, Y. Tai Chi for improvement of motor function, balance and gait in Parkinson’s disease: A systematic review and meta-analysis. PLoS ONE 2014, 9, e102942. [Google Scholar] [CrossRef] [PubMed]
- McGibbon, C.A.; Krebs, D.E.; Parker, S.W.; Scarborough, D.M.; Wayne, P.M.; Wolf, S.L. Tai Chi and vestibular rehabilitation improve vestibulopathic gait via different neuromuscular mechanisms: Preliminary report. BMC Neurol. 2005, 5, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, C.L.; James, C.R.; Chyu, M.C.; Bixby, W.; Brismée, J.M.; Zumwalt, M.A.; Poklikuha, G. Effects of Tai Chi on gait kinematics, physical function, and pain in elderly with knee osteoarthritis—A pilot study. Am. J. Chin. Med. 2008, 36, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Huang, L.; Wu, X.; Wang, L.; Zhang, Y.; Fang, M.; Liu, Y.; Li, J. Effects of Tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis: A randomized controlled trial. J. Sport Health Sci. 2016, 5, 297–303. [Google Scholar] [CrossRef]
- Chao, Y.F.; Chen, S.Y.; Lan, C.; Lai, J. The cardiorespiratory response and energy expenditure of Tai-Chi-Qui-Gong. Am. J. Chin. Med. 2002, 30, 451–461. [Google Scholar] [CrossRef] [PubMed]
- Hui, S.S.; Woo, J.; Kwok, T. Evaluation of energy expenditure and cardiovascular health effects from Tai Chi and walking exercise. Hong Kong Med. J. 2009, 15, 4. [Google Scholar] [PubMed]
- Smith, L.L.; Wherry, S.J.; Larkey, L.K.; Anisworth, B.E.; Swan, P.D. Energy expenditure and cardiovascular responses to Taichi Easy. Complement. Ther. Med. 2015, 23, 802–805. [Google Scholar] [CrossRef] [PubMed]
- Rauh, M.J.; Hovell, M.F.; Hofstetter, C.R.; Sallis, J.F.; Gleghorn, A. Reliability and validity of self-reported physical activity in Latinos. Int. J. Epidemiol. 1992, 21, 966–971. [Google Scholar] [CrossRef]
- Florindo, A.A.; Latorre, M.D. Validation and reliability of the Baecke questionnaire for the evaluation of habitual physical activity in adult men. Revista Brasileira de Medicina do Esporte 2003, 9, 129–135. [Google Scholar] [CrossRef]
- Peeler, J.; Anderson, J.E. Reliability of the Thomas test for assessing range of motion about the hip. Phys. Ther. Sport 2007, 8, 14–21. [Google Scholar] [CrossRef]
- Maki, B.E. Gait changes in older adults: Predictors of falls or indicators of fear? J. Am. Geriatr. Soc. 1997, 45, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.P. Gait as a total pattern of movement: Including a bibliography on gait. Am. J. Phys. Med. Rehabil. 1967, 46, 290–333. [Google Scholar]
- Liang, S.Y.; Wu, W.C. Simplified Tai Chi Chuan; YMAA Publication Center: Wolfeboro, NH, USA, 1996. [Google Scholar]
- Wayne, P.M.; Hausdorff, J.M.; Lough, M.; Gow, B.; Lipsitz, L.; Novak, V.; Macklin, E.; Peng, C.; Manor, B. Tai chi training may reduce dual task gait variability, a potential mediator of fall risk, in healthy older adults: Cross-sectional and randomized trial studies. Front. Hum. Neurosci. 2015, 9, 332. [Google Scholar] [CrossRef] [PubMed]
- Al-Obaidi, S.; Wall, J.C.; Al-Yaqoub, A.; Al-Ghanim, M. Basic gait parameters: A comparison of reference data for normal subjects 20 to 29 years of age from Kuwait and Scandinavia. J. Rehabil. Res. Dev. 2003, 40, 361. [Google Scholar] [CrossRef] [PubMed]
- Oberg, T.; Karsznia, A.; Oberg, K. Basic gait parameters: Reference data for normal subjects, 10–79 years of age. J. Rehabil. Res. Dev. 1993, 30, 210. [Google Scholar] [PubMed]
- Chamberlin, M.E.; Fulwider, B.D.; Sanders, S.L.; Medeiros, J.M. Does fear of falling influence spatial and temporal gait parameters in elderly persons beyond changes associated with normal aging? J. Gerontol. Ser. A 2005, 60, 1163–1167. [Google Scholar] [CrossRef]
- Himann, J.E.; Cunningham, D.A.; Rechnitzer, P.A.; Paterson, D.H. Age-related changes in speed of walking. Med. Sci. Sports Exerc. 1988, 20, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Kirkwood, R.N.; Gomes, H.D.; Sampaio, R.F.; Culham, E.; Costigan, P. Biomechanical analysis of hip and knee joints during gait in elderly subjects. Acta Ortop. Bras. 2007, 15, 267–271. [Google Scholar] [CrossRef]
- Kerrigan, D.C.; Lee, L.W.; Collins, J.J.; Riley, P.O.; Lipsitz, L.A. Reduced hip extension during walking: Healthy elderly and fallers versus young adults. Arch. Phys. Med. Rehabil. 2001, 82, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Lelas, J.L.; Merriman, G.J.; Riley, P.O.; Kerrigan, D.C. Predicting peak kinematic and kinetic parameters from gait speed. Gait Posture 2003, 17, 106–112. [Google Scholar] [CrossRef]
- Cofré, L.E.; Lythgo, N.; Morgan, D.; Galea, M.P. Aging modifies joint power and work when gait speeds are matched. Gait Posture 2011, 33, 484–489. [Google Scholar] [CrossRef] [PubMed]
- Hanlon, M.; Anderson, R. Prediction methods to account for the effect of gait speed on lower limb angular kinematics. Gait Posture 2006, 24, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.W.; Son, S.M.; Lee, N.K. Changes of kinematic parameters of lower extremities with gait speed: A 3D motion analysis study. J. Phys. Ther. Sci. 2015, 27, 477–479. [Google Scholar] [CrossRef] [PubMed]
- Verfaillie, D.F.; Nichols, J.F.; Turkel, E.; Hovell, M.F. Effects of resistance, balance, and gait training on reduction of risk factors leading to falls in elders. J. Aging Phys. Act. 1997, 5, 213–228. [Google Scholar] [CrossRef]
- Lamoureux, E.; Sparrow, W.; Murphy, A.; Newton, R. The effects of improved strength on obstacle negotiation in community-living older adults. Gait Posture 2003, 17, 273–283. [Google Scholar] [CrossRef]
- Kerrigan, D.C.; Xenopoulos-Oddsson, A.; Sullivan, M.J.; Lelas, J.J.; Riley, P.O. Effect of a hip flexor-stretching program on gait in the elderly. Arch. Phys. Med. Rehabil. 2003, 84, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, C.L. The effects of hip and ankle stretching on gait function of older people. Arch. Phys. Med. Rehabil. 2008, 89, 1421–1428. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.; Davids, J.R. Gait analysis: Normal and pathological function. J. Pediatr. Orthop. 1992, 12, 815. [Google Scholar] [CrossRef]
- Chiacchiero, M.; Dresely, B.; Silva, U.; Silva, U.; Delosreyes, R.; Vorik, B. The relationship between range of movement, flexibility, and balance in the elderly. Top. Geriatr. Rehabil. 2010, 26, 148–155. [Google Scholar] [CrossRef]
- Maynard, V.; Bakheit, A.M.; Oldham, J.; Freeman, J. Intra-rater and inter-rater reliability of gait measurements with CODA mpx30 motion analysis system. Gait Posture 2003, 17, 59–67. [Google Scholar] [CrossRef]
| Outcome Measure | Within-Group Effects | Between-Group Effects | |||
|---|---|---|---|---|---|
| Baseline | Week 8 | p | Baseline—Week 8 | p | |
| Mean ± SD | Mean ± SD | Percentage Change | |||
| Stride length (m) | <0.0001 | ||||
| TC (n = 32) | 1.12 ± 0.08 | 1.24 ± 0.09 | <0.05 | +8.6 | |
| CG (n = 29) | 1.12 ± 0.05 | 1.12 ± 0.13 | >0.05 | 0.2 | |
| Gait speed (m/s) | 0.0017 | ||||
| TC (n = 32) | 1.06 ± 0.17 | 1.21 ± 0.23 | <0.05 | +13.9 | |
| CG (n = 29) | 1.06 ± 0.07 | 1.06 ± 0.09 | >0.05 | +0.4 | |
| Cycle time (sec) | 0.6783 | ||||
| TC (n = 32) | 1.09 ± 0.12 | 1.08 ± 0.09 | >0.05 | −1.0 | |
| CG (n = 29) | 1.08 ± 0.05 | 1.08 ± 0.09 | >0.05 | +0.7 | |
| Stance phase (%) | <0.0001 | ||||
| TC (n = 32) | 66.3 ± 4.1 | 61.8 ± 2.6 | <0.05 | −5.5 | |
| CG (n = 29) | 66.9 ± 4.0 | 66.0 ± 3.8 | >0.05 | −1.4 | |
| Swing phase (%) | <0.0001 | ||||
| TC (n = 32) | 33.7 ± 2.3 | 38.4 ± 1.9 | <0.05 | +10.1 | |
| CG (n = 29) | 33.1 ± 2.0 | 33.0 ± 2.8 | >0.05 | −2.8 | |
| Double support time (sec) | <0.0001 | ||||
| TC (n = 32) | 0.33 ± 0.05 | 0.26 ± 0.05 | <0.05 | −21.1 | |
| CG (n = 29) | 0.33 ± 0.02 | 0.33 ± 0.01 | >0.05 | −0.7 | |
| Outcome Measure | Within-Group Effects | Between-Group Effects | |||
|---|---|---|---|---|---|
| Baseline | Week 8 | p | Baseline—Week 8 | p | |
| Mean ± SD | Mean ± SD | Percentage Change | |||
| Hip flexion (degree) | < 0.0001 | ||||
| TC (n = 32) | 70.0 ± 6.8 | 91.9 ± 8.0 | <0.05 | +22.6 * | |
| CG (n = 29) | 69.5 ± 3.7 | 69.9 ± 4.5 | >0.05 | +0.4 | |
| Rectus femoris (degree) | 0.0386 | ||||
| TC (n = 32) | 6.0 ± 2.5 | 2.0 ± 1.3 | <0.05 | −61.5 * | |
| CG (n = 29) | 5.8 ± 1.6 | 3.0 ± 2.3 | >0.05 | −2.0 | |
| Plantar flexion (degree) | <0.0001 | ||||
| TC (n = 32) | 41.6 ± 5.3 | 49.7 ± 3.1 | <0.05 | +17.5 * | |
| CG (n = 29) | 42.0 ± 4.2 | 42.7 ± 7.4 | >0.05 | +0.9 | |
| Outcome Measure | Within-Group Effects | Between-Group Effects | |||
|---|---|---|---|---|---|
| Baseline | Week 8 | p | Baseline—Week 8 | p | |
| Mean ± SD | Mean ± SD | Percentage Change | |||
| APT (degree) | <0.0001 | ||||
| TC (n = 32) | 9.5 ± 0.8 | 6.2 ± 1.8 | <0.05 | −34.7 | |
| CG (n = 29) | 9.6 ± 0.9 | 9.4 ± 2.1 | >0.05 | −2.5 | |
| LPT (degree) | 0.0102 | ||||
| TC (n = 32) | 6.6 ± 0.7 | 8.3 ± 2.1 | <0.05 | +23.8 | |
| CG (n = 29) | 6.7 ± 2.8 | 6.7 ± 2.6 | >0.05 | +0.3 | |
| PRO (degree) | <0.0001 | ||||
| TC (n = 32) | 10.3 ± 2.0 | 14.7 ± 2.9 | <0.05 | +28.2 | |
| CG (n = 29) | 10.8 ± 6.4 | 10.7 ± 3.9 | >0.05 | −1.8 | |
| HROM (degree) | 0.0010 | ||||
| TC (n = 32) | 29.8 ± 4.5 | 32.9 ± 2.5 | <0.05 | +13.5 | |
| CG (n = 29) | 29.9 ± 3.2 | 29.7 ± 4.5 | >0.05 | −0.9 | |
| KROM (degree) | 0.5245 | ||||
| TC (n = 32) | 53.2 ± 4.8 | 54.9 ± 5.7 | >0.05 | +2.9 | |
| CG (n = 29) | 53.7 ± 4.0 | 53.9 ± 6.5 | >0.05 | +0.4 | |
| AROM (degree) | <0.0001 | ||||
| TC (n = 32) | 28.0 ± 4.2 | 32.6 ± 5.1 | <0.05 | +11.1 | |
| CG (n = 29) | 27.9 ± 3.6 | 27.1 ± 2.1 | >0.05 | −0.2 | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zou, L.; Wang, C.; Tian, Z.; Wang, H.; Shu, Y. Effect of Yang-Style Tai Chi on Gait Parameters and Musculoskeletal Flexibility in Healthy Chinese Older Women. Sports 2017, 5, 52. https://doi.org/10.3390/sports5030052
Zou L, Wang C, Tian Z, Wang H, Shu Y. Effect of Yang-Style Tai Chi on Gait Parameters and Musculoskeletal Flexibility in Healthy Chinese Older Women. Sports. 2017; 5(3):52. https://doi.org/10.3390/sports5030052
Chicago/Turabian StyleZou, Liye, Chaoyi Wang, Zuguo Tian, Huiru Wang, and Yankai Shu. 2017. "Effect of Yang-Style Tai Chi on Gait Parameters and Musculoskeletal Flexibility in Healthy Chinese Older Women" Sports 5, no. 3: 52. https://doi.org/10.3390/sports5030052





