Organized Sport Participation and Physical Activity Levels among Adolescents with Functional Limitations
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Materials
“Over the past 7 days, on how many days were you physically active for a total of at least 60 min per day? Please add up all the time you spent in physical activity each day.”(emphasis is the same as in the questionnaire)
2.3. Analyses
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Lee, I.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Sheehan, P.; Sweeny, K.; Rasmussen, B.; Wils, A.; Friedman, H.S.; Mahon, J.; Patton, G.C.; Sawyer, S.M.; Howard, E.; Symons, J.; et al. Building the foundations for sustainable development: A case for global investment in the capabilities of adolescents. Lancet 2017. [Google Scholar] [CrossRef]
- Durstine, J.L.; Painter, P.; Franklin, B.A.; Morgan, D.; Pitetti, K.H.; Roberts, S.O. Physical activity for the chronically ill and disabled. Sports Med. 2000, 30, 207–219. [Google Scholar] [CrossRef] [PubMed]
- Eime, R.M.; Young, J.A.; Harvey, J.T.; Charity, M.J.; Payne, W.R. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: Informing development of a conceptual model of health through sport. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ng, K.W.; Rintala, P.; Saari, A. Functional Difficulties and Physical Activity and Sedentariness [Toimintakyvyn ja-Rajoitteiden Yhteydet Liikunta-Aktiivisuuteen ja Paikallaanoloon]; Kokko, S., Mehtälä, A., Eds.; The Finnish school-aged physical activity monitoring study: Results from 2016; Valtion Liikuntaneuvoston Julkaisuja: Helsinki, Finland, 2016; pp. 73–78. (In Finnish) [Google Scholar]
- Mulligan, H.F.; Hale, L.A.; Whitehead, L.; Baxter, D.G. Barriers to physical activity for people with long-term neurological conditions: A review study. Adapt. Phys. Act. Q. 2012, 29, 243–265. [Google Scholar] [CrossRef]
- Shields, N.; Synnot, A.J.; Barr, M. Perceived barriers and facilitators to physical activity for children with disability: A systematic review. Br. J. Sports Med. 2012, 46, 989–997. [Google Scholar] [CrossRef] [PubMed]
- Bloemen, M.A.T.; Backx, F.J.G.; Takken, T.; Wittink, H.; Benner, J.; Mollema, J.; de Groot, J.F. Factors associated with physical activity in children and adolescents with a physical disability: A systematic review. Dev. Med. Child Neurol. 2015, 57, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Bult, M.K.; Verschuren, O.; Jongmans, M.J.; Lindeman, E.; Ketelaar, M. What influences participation in leisure activities of children and youth with physical disabilities? A systematic review. Res. Dev. Disabil. 2011, 32, 1521–1529. [Google Scholar] [CrossRef] [PubMed]
- Pittet, I.; Berchtold, A.; Akré, C.; Michaud, P.; Suris, J. Sports practice among adolescents with chronic health conditions. Arch. Pediatr. Adolesc. Med. 2009, 163, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Rimmer, J.H.; Rowland, J.L. Physical activity for youth with disabilities: A critical need in an underserved population. Dev. Neurorehabil. 2008, 11, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Shields, N.; Synnot, A. Perceived barriers and facilitators to participation in physical activity for children with disability: A qualitative study. BMC Pediatr. 2016, 16. [Google Scholar] [CrossRef] [PubMed]
- Jaarsma, E.A.; Dijkstra, P.U.; de Blécourt, A.C.E.; Geertzen, J.H.B.; Dekker, R. Barriers and facilitators of sports in children with physical disabilities: A mixed-method study. Disabil. Rehabil. 2015, 37, 1617–1623. [Google Scholar] [CrossRef]
- Geidne, S.; Jerlinder, K. How sports clubs include children and adolescents with disabilities in their activities. A systematic search of peer-reviewed articles. Sport Sci. Rev. 2016, 25, 29–52. [Google Scholar] [CrossRef]
- Antonovsky, A. Health, Stress and Coping; The Jossey-Bass Social and Behavioral Science Series; Jossey-Bass: San Francisco, CA, USA, 1979. [Google Scholar]
- Braun-Lewensohn, O.; Idan, O.; Lindström, B.; Margalit, M. Salutogenesis: Sense of coherence in adolescence. In The Handbook of Salutogenesis; Springer: New York, NY, USA, 2017; pp. 123–136. [Google Scholar] [CrossRef] [Green Version]
- Honkinen, P.K.; Suominen, S.B.; Välimaa, R.S.; Helenius, H.Y.; Rautava, P.T. Factors associated with perceived health among 12-year-old school children. Relevance of physical exercise and sense of coherence. Scand. J. Soc. Med. 2005, 33, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Badura, P.; Sigmund, E.; Madarasova Geckova, A.; Sigmundova, D.; Sirucek, J.; van Dijk, J.P.; Reijneveld, S.A. Is participation in organized leisure-time activities associated with school performance in adolescence? PLoS ONE 2016, 11, e0153276. [Google Scholar] [CrossRef] [PubMed]
- WHO. International Classification of Functioning, Disability and Health (ICF); World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Wilhelmsen, T.; Sørensen, M. Inclusion of Children with Disabilities in Physical Education: A Systematic Review of Literature from 2009 to 2015. Adapt. Phys. Act. Q. 2017, 34, 311–337. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Gorter, J.W. The ‘F-words’ in childhood disability: I swear this is how we should think! Child. Care Health Dev. 2012, 38, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Wichstrøm, L.; von Soest, T.; Kvalem, I.L. Predictors of growth and decline in leisure time physical activity from adolescence to adulthood. Health Psychol. 2013, 32, 775–784. [Google Scholar] [CrossRef] [PubMed]
- Telama, R.; Yang, X.; Hirvensalo, M.; Raitakari, O. Participation in organized youth sport as a predictor of adult physical activity: A 21-year longitudinal study. Pediatr. Exerc. Sci. 2006, 18, 76–88. [Google Scholar] [CrossRef]
- Ng, K.W.; Rintala, P.; Tynjälä, J.A.; Välimaa, R.S.; Villberg, J.; Kokko, S.; Kannas, L.K. Physical activity trends of Finnish adolescents with long-term illnesses or disabilities from 2002 to 2014. J. Phys. Act. Health 2016, 13, 816–821. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Barnes, J.D.; González, S.A.; Katzmarzyk, P.T.; Onywera, V.O.; Reilly, J.J.; Tomkinson, G.R. Global Matrix 2.0: Report Card Grades on the Physical Activity of Children and Youth Comparing 38 Countries. J. Phys. Act. Health 2016, 13, S343–S366. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.W. Physical activity of adolescents with long term illnesses or disabilities in reference to ICF personal factors [Vammaisten ja pitkäaikaissairaiden nuorten liikunta-aktiivisuus ICF-luokituksen yksilötekijöiden näkökulmasta]. In Studies in Sport, Physical Education and Health 245; University of Jyväskylä: Jyväskylä, Finland, 2016. [Google Scholar]
- Ng, K.W.; Rintala, P.; Tynjälä, J.A.; Villberg, J.; Kannas, L.K. Physical activity patterns of adolescents with long term illnesses or disabilities in Finnish general education. Eur. J. Adapt. Phys. Act. 2014, 7, 58–72. [Google Scholar]
- WHO. Global Recommendations on Physical Activity for Health; WHO: Genova, Switzerland, 2010. [Google Scholar]
- Prochaska, J.J.; Sallis, J.F.; Long, B. A physical activity screening measure for use with adolescents in primary care. Arch. Pediatr. Adolesc. Med. 2001, 155, 554–559. [Google Scholar] [CrossRef] [PubMed]
- Vuori, M.T.; Ojala, S.A.K.; Tynjälä, J.A.; Villberg, J.; Välimaa, R.S.; Kannas, L.K. The stability of questions concerning physical activity in the HBSC study. Liikunta Tiede 2005, 42, 39–46. (In Finnish) [Google Scholar]
- Biddle, S.J.H.; Atkin, A.J.; Cavill, N.; Foster, C. Correlates of physical activity in youth: A review of quantitative systematic reviews. Int. Rev. Sport Exerc. Psychol. 2011, 4, 25. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 6th ed.; Pearson Education: Harlow, UK, 2014. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Earlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Tammelin, T.H.; Aira, A.; Hakamäki, M.; Husu, P.; Kallio, J.; Kokko, S.; Laine, K.; Lehtonen, K.; Mononen, K.; Palomäki, S.; et al. Results from Finland’s 2016 Report Card on Physical Activity for Children and Youth. J. Phys. Act. Health 2016, 13, S157–S164. [Google Scholar] [CrossRef] [PubMed]
- Longmuir, P.E.; Bar-Or, O. Factors influencing the physical activity levels of youths with physical and sensory disabilities. Adapt. Phys. Act. Q. 2000, 17, 40–53. [Google Scholar] [CrossRef]
- Aslan, U.B.; Calik, B.B.; Kitiş, A. The effect of gender and level of vision on the physical activity level of children and adolescents with visual impairment. Res. Dev. Disabil. 2012, 33, 1799–1804. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, L.J.; Robinson, B.L.; Rollheiser, H. Youth with Visual Impairments: Experiences in General Physical Education. RE View 2006, 38, 35–48. [Google Scholar] [CrossRef]
- Fleeman, N.; Lindsay, B.; Bradley Peter, M. Care delivery and self-management strategies for children with epilepsy. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef]
- Ramirez, M.; Yang, J.; Bourque, L.; Javien, J.; Kashani, S.; Limbos, M.A.; Peek-Asa, C. Sports Injuries to High School Athletes With Disabilities. Pediatrics 2009, 123, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Shaw, S.M.; Kleiber, D.A.; Caldwell, L.L. Leisure and identity formation in male and female adolescents: A preliminary examination. J. Leis Res. 1995, 27, 245–263. [Google Scholar]
- Carron, A.V.; Widmeyer, W.N.; Brawley, L.R. The development of an instrument to assess cohesion in sport teams: The group environment questionnaire. J. Sport Exerc. Psychol. 1985, 7, 244–266. [Google Scholar] [CrossRef]
- Perrier, M.; Smith, B.; Strachan, S.M.; Latimer-Cheung, A. narratives of athletic identity after acquiring a permanent physical disability. Adapt. Phys. Act. Q. 2014, 31, 106–124. [Google Scholar] [CrossRef] [PubMed]
- Suris, J.; Michaud, P.; Viner, R.M. The adolescent with a chronic condition. Part I: Developmental issues. Arch. Dis. Child. 2004, 89, 938–942. [Google Scholar] [CrossRef] [PubMed]
- Klavina, A.; Block, M.E. The effect of peer tutoring on interaction behaviors in inclusive physical education. Adapt. Phys. Act. Q. 2008, 25, 132–158. [Google Scholar] [CrossRef]
- Badura, P.; Sigmundova, D.; Sigmund, E.; Madarasova Geckova, A.; van Dijk, J.P.; Reijneveld, S.A. Participation in organized leisure-time activities and risk behaviors in Czech adolescents. Int. J. Public Health 2017, 62, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Ng, K.W.; Mäkelä, K.; Parkkari, J.; Kannas, L.; Vasankari, T.; Heinonen, J.O.; Savonen, K.; Alanko, L.; Korpelainen, R.; Selänne, H.; et al. Coaches’ health promotion activity and substance use in youth sports. Societies 2017, 7, 4. [Google Scholar] [CrossRef]
| Not Specified | Breathing | Motor | Communication | Visual | Epilepsy | Motor and Breathing | |
|---|---|---|---|---|---|---|---|
| (n = 548) | (n = 323) | (n = 67) | (n = 29) | (n = 26) | (n = 20) | (n = 28) | |
| Gender | |||||||
| Male | 52.2% | 60.4% | 58.2% | 69.0% | 42.3% | 60.0% | 85.7% |
| Female | 47.8% | 39.6% | 41.8% | 31.0% | 57.7% | 40.0% | 14.3% |
| Age Group | |||||||
| 13 | 49.8% | 45.8% | 50.7% | 55.2% | 42.3% | 75.0% | 57.1% |
| 15 | 50.2% | 54.2% | 49.3% | 44.8% | 57.7% | 25.0% | 42.9% |
| Year of Data Collection | |||||||
| 2002 | 53.8% | 52.3% | 71.6% | 55.2% | 50.0% | 40.0% | 35.7% |
| 2010 | 46.2% | 47.7% | 28.4% | 44.8% | 50.0% | 60.0% | 64.3% |
| Organized Sport | |||||||
| Non-Participant | 58.2% | 60.4% | 65.7% | 79.3% | 69.2% | 60.0% | 60.7% |
| Participant | 41.8% | 39.6% | 34.3% | 20.7% | 30.8% | 40.0% | 39.3% |
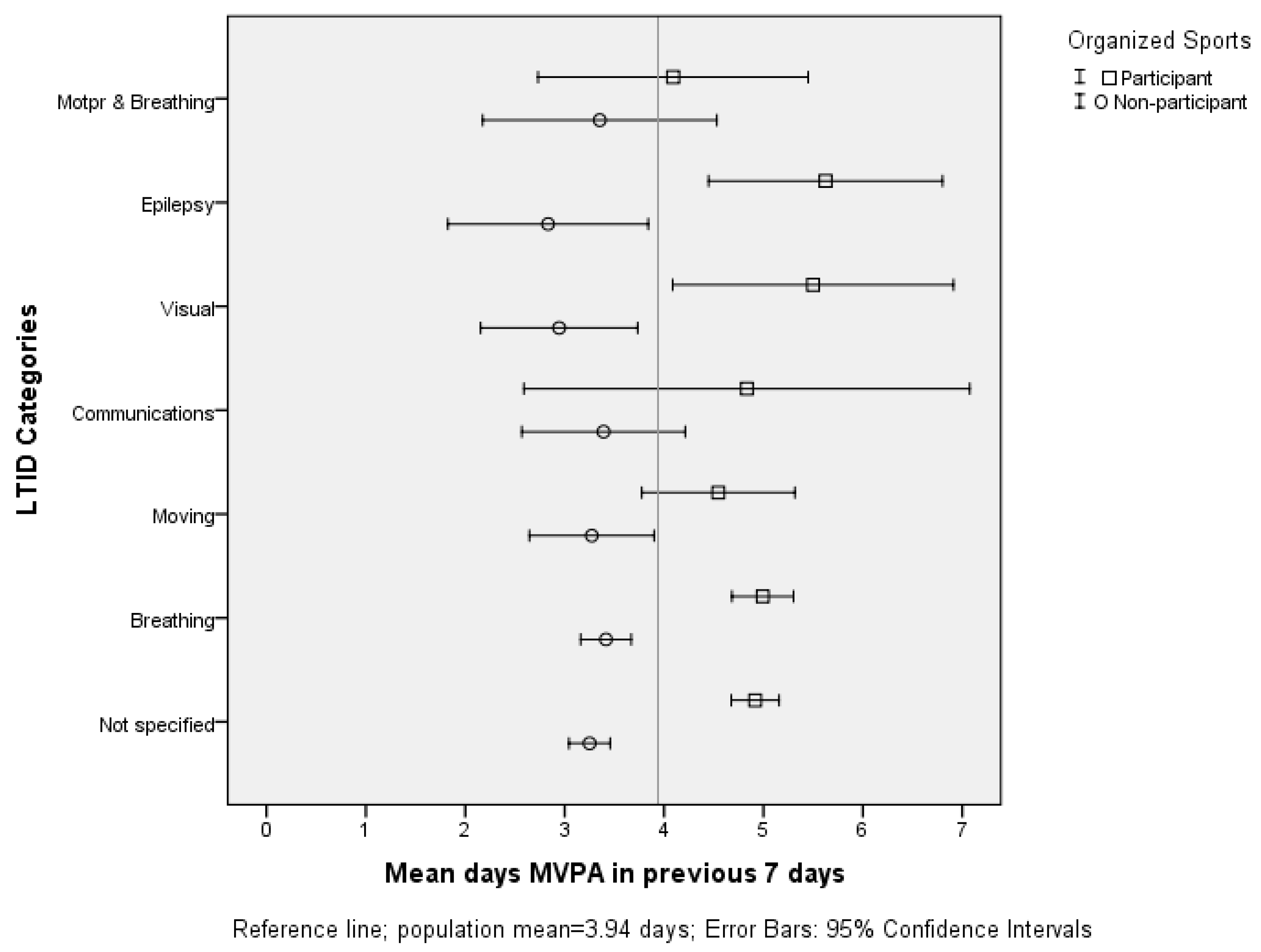
| Non-Participant (n = 628) | Participant (n = 413) | MWtest a | Cohen’s | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | LCI | UCI | Mean | LCI | UCI | p | d | |
| Not Specified | 3.31 | 3.11 | 3.51 | 4.84 | 4.60 | 5.07 | <0.001 | 0.90 |
| Breathing | 3.80 | 3.23 | 3.72 | 4.90 | 4.59 | 5.20 | <0.001 | 0.88 |
| Motor | 3.27 | 2.70 | 3.84 | 4.56 | 3.75 | 5.37 | 0.010 | 0.65 |
| Communication | 3.31 | 2.44 | 4.17 | 5.16 | 3.41 | 6.91 | 0.135 | 0.74 |
| Visual | 2.99 | 2.16 | 3.82 | 5.40 | 4.09 | 6.70 | 0.002 | 1.58 |
| Epilepsy | 2.87 | 1.85 | 3.88 | 5.58 | 4.33 | 6.82 | 0.002 | 1.84 |
| Motor & Breathing | 3.66 | 2.64 | 4.69 | 3.61 | 2.32 | 4.91 | 0.351 | 0.33 |
| Total | 3.34 | 3.20 | 3.48 | 4.85 | 4.67 | 5.02 | <0.001 | 0.89 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, K.; Rintala, P.; Hutzler, Y.; Kokko, S.; Tynjälä, J. Organized Sport Participation and Physical Activity Levels among Adolescents with Functional Limitations. Sports 2017, 5, 81. https://doi.org/10.3390/sports5040081
Ng K, Rintala P, Hutzler Y, Kokko S, Tynjälä J. Organized Sport Participation and Physical Activity Levels among Adolescents with Functional Limitations. Sports. 2017; 5(4):81. https://doi.org/10.3390/sports5040081
Chicago/Turabian StyleNg, Kwok, Pauli Rintala, Yeshayahu Hutzler, Sami Kokko, and Jorma Tynjälä. 2017. "Organized Sport Participation and Physical Activity Levels among Adolescents with Functional Limitations" Sports 5, no. 4: 81. https://doi.org/10.3390/sports5040081





