Nutrition and Supplementation Considerations to Limit Endotoxemia When Exercising in the Heat
Abstract
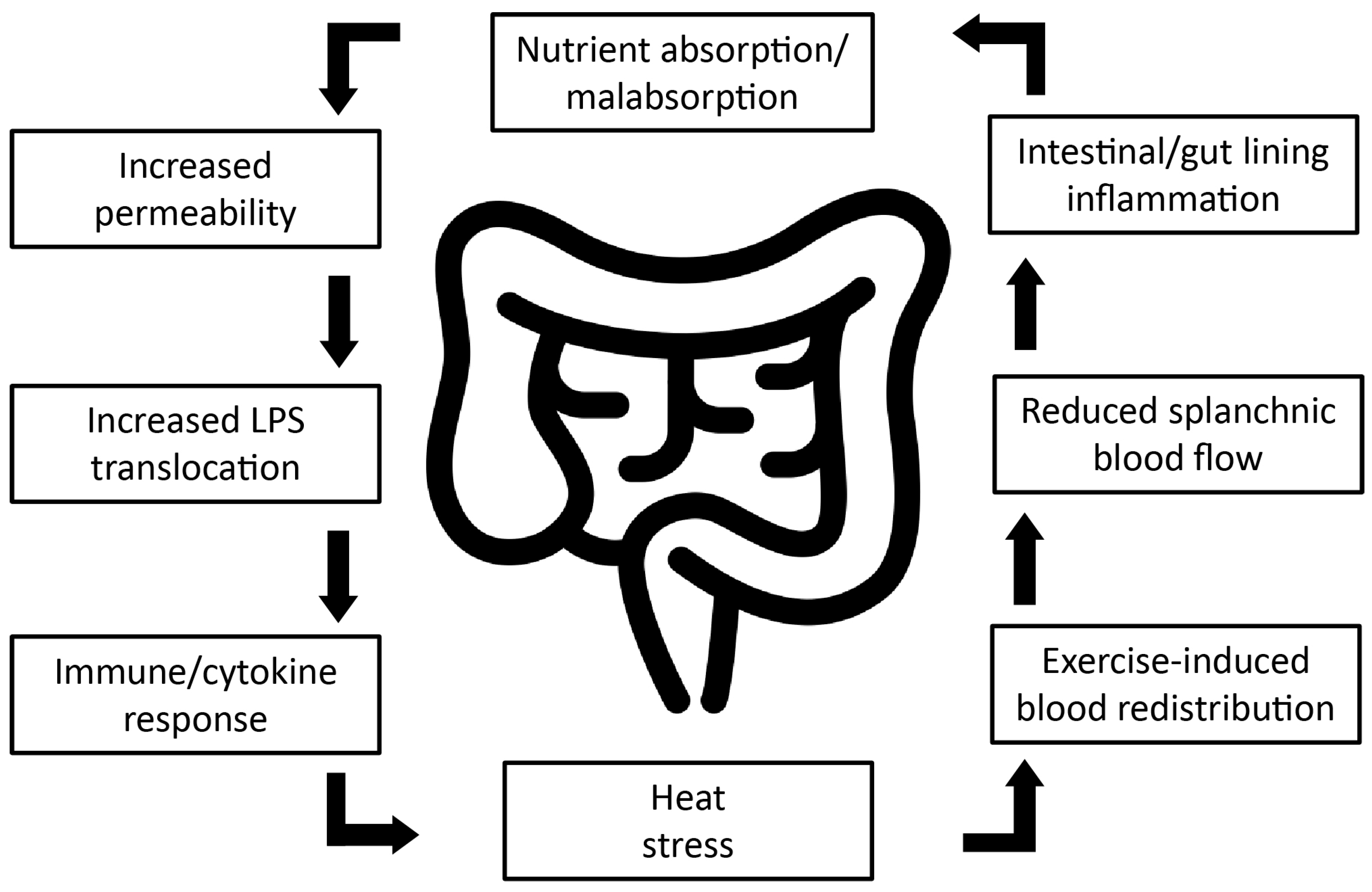
:1. Introduction
2. Lipopolysaccharide and Endotoxemia during Exercise
3. Cytokines
4. Nutrition and Supplementation Strategies for Exercise in the Heat
Other Nutrition and Supplementation Considerations
5. Recommendations and Future Research Directions
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Pyne, D.B.; Guy, J.H.; Edwards, A.M. Managing heat and immune stress in athletes with evidence-based strategies. Int. J. Sports Physiol. Perform. 2014, 9, 744–750. [Google Scholar] [CrossRef] [PubMed]
- Tyler, C.J.; Reeve, T.; Hodges, G.J.; Cheung, S.S. The effects of heat adaptation on physiology, perception and exercise performance in the heat: A meta-analysis. Sports Med. 2016, 46, 1699–1724. [Google Scholar] [CrossRef] [PubMed]
- Aughey, R.J.; Goodman, C.A.; McKenna, M.J. Greater chance of high core temperatures with modified pacing strategy during team sport in the heat. J. Sci. Med. Sport 2014, 17, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Selkirk, G.A.; McLellan, T.M.; Wright, H.E.; Rhind, S.G. Mild endotoxemia, nf-κb translocation, and cytokine increase during exertional heat stress in trained and untrained individuals. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008, 295, R611–R623. [Google Scholar] [CrossRef] [PubMed]
- Sithinamsuwan, P.; Piyavechviratana, K.; Kitthaweesin, T.; Chusri, W.; Orrawanhanothai, P.; Wongsa, A.; Wattanathum, A.; Chinvarun, Y.; Nidhinandana, S.; Satirapoj, L.B. Exertional heatstroke: Early recognition and outcome with aggressive combined cooling—A 12-year experience. Mil. Med. 2009, 174, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Shephard, R.J. Cytokine responses to physical activity, with particular reference to il-6: Sources, actions, and clinical implications. Crit. Rev. Immunol. 2002, 22, 18. [Google Scholar]
- Chalmers, S.; Esterman, A.; Eston, R.; Bowering, K.J.; Norton, K. Short-term heat acclimation training improves physical performance: A systematic review, and exploration of physiological adaptations and application for team sports. Sports Med. 2014, 44, 971–988. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, N.R.; DiMarco, N.M.; Langley, S. Nutrition and athletic performance. Med. Sci. Sports Exerc. 2009, 41, 709–731. [Google Scholar] [PubMed]
- Williams, M.H. Dietary supplements and sports performance: Minerals. J. Int. Soc. Sports Nutr. 2005, 2, 43. [Google Scholar] [CrossRef] [PubMed]
- Lim, C.L.; Pyne, D.; Horn, P.; Kalz, A.; Saunders, P.; Peake, J.; Suzuki, K.; Wilson, G.; Mackinnon, L.T. The effects of increased endurance training load on biomarkers of heat intolerance during intense exercise in the heat. Appl. Physiol. Nutr. Metab. 2009, 34, 616–624. [Google Scholar] [CrossRef] [PubMed]
- Barberio, M.D.; Elmer, D.J.; Laird, R.H.; Lee, K.A.; Gladden, B.; Pascoe, D.D. Systemic LPS and inflammatory response during consecutive days of exercise in heat. Int. J. Sports Med. 2015, 36, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Sakurada, S.; Hales, J.R. A role for gastrointestinal endotoxins in enhancement of heat tolerance by physical fitness. J. Appl. Physiol. 1998, 84, 207–214. [Google Scholar] [CrossRef] [PubMed]
- Van Wijck, K.; Lenaerts, K.; Van Bijnen, A.A.; Boonen, B.; Van Loon, L.; Dejong, C.; Buurman, W.A. Aggravation of exercise-induced intestinal injury by ibuprofen in athletes. Med. Sci. Sports Exerc. 2012, 44, 2257–2262. [Google Scholar] [CrossRef] [PubMed]
- Zuhl, M.; Schneider, S.; Lanphere, K.; Conn, C.; Dokladny, K.; Moseley, P. Exercise regulation of intestinal tight junction proteins. Br. J. Sports Med. 2014, 48, 980–986. [Google Scholar] [CrossRef] [PubMed]
- Bosenberg, A.T.; Brock-Utne, J.G.; Gaffin, S.L.; Wells, M.T.; Blake, G.T. Strenuous exercise causes systemic endotoxemia. J. Appl. Physiol. 1988, 65, 106–108. [Google Scholar] [CrossRef] [PubMed]
- Brock-Utne, J.; Gaffin, S.; Wells, M.; Gathiram, P.; Sohar, E.; James, M.; Morrell, D.; Norman, R. Endotoxaemia in exhausted runners after a long-distance race. S. Afr. Med. J. 1988, 73, 533–536. [Google Scholar] [PubMed]
- Jeukendrup, A.; Vet-Joop, K.; Sturk, A.; Stegen, J.; Senden, J.; Saris, W.; Wagenmakers, A. Relationship between gastro-intestinal complaints and endotoxaemia, cytokine release and the acute-phase reaction during and after a long-distance triathlon in highly trained men. Clin. Sci. 2000, 98, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Gill, S.K.; Teixeira, A.; Rama, L.; Prestes, J.; Rosado, F.; Hankey, J.; Scheer, V.; Hemmings, K.; Ansley-Robson, P.; Costa, R.J. Circulatory endotoxin concentration and cytokine profile in response to exertional-heat stress during a multi-stage ultra-marathon competition. Exerc. Immunol. Rev. 2015, 21, 114–128. [Google Scholar] [PubMed]
- Morrison, S.A.; Cheung, S.S.; Cotter, J.D. Bovine colostrum, training status, and gastrointestinal permeability during exercise in the heat: A placebo-controlled double-blind study. Appl. Physiol. Nutr. Metab. 2014, 39, 1070–1082. [Google Scholar] [CrossRef] [PubMed]
- Snipe, R.M.; Khoo, A.; Kitic, C.M.; Gibson, P.R.; Costa, R.J. Carbohydrate and protein intake during exertional heat stress ameliorates intestinal epithelial injury and small intestine permeability. Appl. Physiol. Nutr. Metab. 2017, 42, 1283–1292. [Google Scholar] [CrossRef] [PubMed]
- Pugh, J.N.; Sage, S.; Hutson, M.; Doran, D.A.; Fleming, S.C.; Highton, J.; Morton, J.P.; Close, G.L. Glutamine supplementation reduces markers of intestinal permeability during running in the heat in a dose-dependent manner. Eur. J. Appl. Physiol. 2017, 117, 2569–2577. [Google Scholar] [CrossRef] [PubMed]
- Shing, C.M.; Peake, J.M.; Lim, C.L.; Briskey, D.; Walsh, N.P.; Fortes, M.B.; Ahuja, K.D.; Vitetta, L. Effects of probiotics supplementation on gastrointestinal permeability, inflammation and exercise performance in the heat. Eur. J. Appl. Physiol. 2014, 114, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Buckley, J.D.; Butler, R.N.; Southcott, E.; Brinkworth, G.D. Bovine colostrum supplementation during running training increases intestinal permeability. Nutrients 2009, 1, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Moncada-Jiménez, J.; Plaisance, E.; Araya-Ramírez, F.; Taylor, J.; Ratcliff, L.; Mestek, M.; Grandjean, P.; AragonVargas, L. Acute hepatic response to diet modification and exercise-induced endotoxemia during a laboratory-based duathlon. Biol. Sport 2010, 27, 111–118. [Google Scholar] [CrossRef]
- Heled, Y.; Fleischmann, C.; Epstein, Y. Cytokines and their role in hyperthermia and heat stroke. J. Basic Clin. Physiol. Pharmacol. 2013, 24, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Fischer, C.P. Interleukin-6 in acute exercise and training: What is the biological relevance. Exerc. Immunol. Rev. 2006, 12, 41. [Google Scholar]
- Mihara, M.; Hashizume, M.; Yoshida, H.; Suzuki, M.; Shiina, M. Il-6/il-6 receptor system and its role in physiological and pathological conditions. Clin. Sci. 2012, 122, 143–159. [Google Scholar] [CrossRef] [PubMed]
- Margeli, A.; Skenderi, K.; Tsironi, M.; Hantzi, E.; Matalas, A.-L.; Vrettou, C.; Kanavakis, E.; Chrousos, G.; Papassotiriou, I. Dramatic elevations of interleukin-6 and acute-phase reactants in athletes participating in the ultradistance foot race spartathlon: Severe systemic inflammation and lipid and lipoprotein changes in protracted exercise. J. Clin. Endocrinol. Metab. 2005, 90, 3914–3918. [Google Scholar] [CrossRef] [PubMed]
- Fortes, M.B.; Di Felice, U.; Dolci, A.; Junglee, N.A.; Crockford, M.J.; West, L.; Hillier-Smith, R.; Macdonald, J.H.; Walsh, N.P. Muscle-damaging exercise increases heat strain during subsequent exercise heat stress. Med. Sci. Sports Exerc. 2013, 45, 1915–1924. [Google Scholar] [CrossRef] [PubMed]
- Cox, A.J.; Pyne, D.B.; Saunders, P.U.; Callister, R.; Gleeson, M. Cytokine responses to treadmill running in healthy and illness-prone athletes. Med. Sci. Sports Exerc. 2007, 39, 1918. [Google Scholar] [CrossRef] [PubMed]
- Ashton, T.; Young, I.S.; Davison, G.W.; Rowlands, C.C.; McEneny, J.; Van Blerk, C.; Jones, E.; Peters, J.R.; Jackson, S.K. Exercise-induced endotoxemia: The effect of ascorbic acid supplementation. Free Radic. Biol. Med. 2003, 35, 284–291. [Google Scholar] [CrossRef]
- Marchbank, T.; Davison, G.; Oakes, J.R.; Ghatei, M.A.; Patterson, M.; Moyer, M.P.; Playford, R.J. The nutriceutical bovine colostrum truncates the increase in gut permeability caused by heavy exercise in athletes. Am. J. Physiol. Gastrointest. Liver Physiol. 2011, 300, G477–G484. [Google Scholar] [CrossRef] [PubMed]
- Walsh, N.P.; Blannin, A.K.; Robson, P.J.; Gleeson, M. Glutamine, exercise and immune function. Sports Med. 1998, 26, 177–191. [Google Scholar] [CrossRef] [PubMed]
- Stellingwerff, T.; Cox, G.R. Systematic review: Carbohydrate supplementation on exercise performance or capacity of varying durations. Appl. Physiol. Nutr. Metab. 2014, 39, 998–1011. [Google Scholar] [CrossRef] [PubMed]
- Steensberg, A.; Febbraio, M.; Osada, T.; Schjerling, P.; van Hall, G.; Saltin, B.; Pedersen, B.K. Low glycogen content increases interleukin-6 in contracting human skeletal muscle. J. Physiol. 2001, 537, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Bishop, N.C.; Walsh, N.P.; Haines, D.L.; Richards, E.E.; Gleeson, M. Pre-exercise carbohydrate status and immune responses to prolonged cycling: II. Effect on plasma cytokine concentration. Int. J. Sport Nutr. Exerc. Metab. 2001, 11, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Cox, A.J.; Pyne, D.; Cox, G.; Callister, R.; Gleeson, M. Influence of chronic dietary carbohydrate supplementation on plasma cytokine responses to exercise. Int. J. Sports Med. 2010, 31, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Taioli, E. Use of permitted drugs in italian professional soccer players. Br. J. Sports Med. 2007, 41, 439–441. [Google Scholar] [CrossRef] [PubMed]
- Alaranta, A.; Alaranta, H.; Heliövaara, M.; Airaksinen, M.; Helenius, I. Ample use of physician-prescribed medications in finnish elite athletes. Int. J. Sports Med. 2006, 27, 919–925. [Google Scholar] [CrossRef] [PubMed]
- Garcin, M.; Mille-Hamard, L.; Billat, V.; Imbenotte, M. Use of acetaminophen in young subelite athletes. J. Sports Med. Phys. Fit. 2005, 45, 604. [Google Scholar]
- Gorski, T.; Cadore, E.L.; Pinto, S.S.; da Silva, E.M.; Correa, C.S.; Beltrami, F.G.; Kruel, L.M. Use of nsaids in triathletes: Prevalence, level of awareness and reasons for use. Br. J. Sports Med. 2011, 45, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Camus, G.; Nys, M.; Poortmans, J.-R.; Venneman, I.; Monfils, T.; Deby-Dupont, G.; Juchmes-Ferir, A.; Deby, C.; Lamy, M.; Duchateau, J. Endotoxaemia, production of tumour necrosis factor α and polymorphonuclear neutrophil activation following strenuous exercise in humans. Eur. J. Appl. Physiol. Occup. Physiol. 1998, 79, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Lopez, R.M.; Casa, D.J. The influence of nutritional ergogenic aids on exercise heat tolerance and hydration status. Curr. Sports Med. Rep. 2009, 8, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Lopez, R.M.; Casa, D.J.; McDermott, B.P.; Ganio, M.S.; Armstrong, L.E.; Maresh, C.M. Does creatine supplementation hinder exercise heat tolerance or hydration status? A systematic review with meta-analyses. J. Athl. Train. 2009, 44, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Kern, M.; Podewils, L.J.; Vukovich, M.; Buono, M.J. Physiological response to exercise in the heat following creatine supplementation. JEP Online 2001, 4, 18–27. [Google Scholar]
- Kilduff, L.P.; Georgiades, E.; James, N.; Minnion, R.; Mitchell, M.; Kingsmore, D.; Hadjicharalambous, M.; Pitsiladis, Y.P. The effects of creatine supplementation on cardiovascular, metabolic, and thermoregulatory responses during exercise in the heat in endurance-trained humans. Int. J. Sport Nutr. Exerc. Metab. 2004, 14, 443–460. [Google Scholar] [CrossRef] [PubMed]
- Mendel, R.W.; Blegen, M.; Cheatham, C.; Antonio, J.; Ziegenfuss, T. Effects of creatine on thermoregulatory responses while exercising in the heat. Nutrition 2005, 21, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Dalbo, V.J.; Roberts, M.D.; Stout, J.R.; Kerksick, C.M. Putting to rest the myth of creatine supplementation leading to muscle cramps and dehydration. Br. J. Sports Med. 2008, 42, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Fiala, K.A.; Casa, D.J.; Roti, M.W. Rehydration with a caffeinated beverage during the nonexercise periods of 3 consecutive days of 2-a-day practices. Int. J. Sport Nutr. Exerc. Metab. 2004, 14, 419–429. [Google Scholar] [CrossRef] [PubMed]
- Roti, M.W.; Casa, D.J.; Pumerantz, A.C.; Watson, G.; Judelson, D.A.; Dias, J.C.; Ruffin, K.; Armstrong, L.E. Thermoregulatory responses to exercise in the heat: Chronic caffeine intake has no effect. Aviat. Space Environ. Med. 2006, 77, 124–129. [Google Scholar] [PubMed]
- Armstrong, L.E.; Pumerantz, A.C.; Roti, M.W.; Judelson, D.A.; Watson, G.; Dias, J.C.; Sökmen, B.; Casa, D.J.; Maresh, C.M.; Lieberman, H. Fluid, electrolyte, and renal indices of hydration during 11 days of controlled caffeine consumption. Int. J. Sport Nutr. Exerc. Metab. 2005, 15, 252–265. [Google Scholar] [CrossRef] [PubMed]
- Robergs, R. Glycerol hyperhydration to beat the heat? Sportsci. Train. Technol. 1998. Available online: http://sportsci.org/traintech/glycerol/rar.htm (accessed on 6 February 2018).
- Kavouras, S.A.; Armstrong, L.E.; Maresh, C.M.; Casa, D.J.; Herrera-Soto, J.A.; Scheett, T.P.; Stoppani, J.; Mack, G.W.; Kraemer, W.J. Rehydration with glycerol: Endocrine, cardiovascular, and thermoregulatory responses during exercise in the heat. J. Appl. Physiol. 2006, 100, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Marino, F.E.; Kay, D.; Cannon, J. Glycerol hyperhydration fails to improve endurance performance and thermoregulation in humans in a warm humid environment. Pflügers Arch. 2003, 446, 455–462. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, E.P.; Burini, R.C. Food-dependent, exercise-induced gastrointestinal distress. J. Int. Soc. Sports Nutr. 2011, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Wittbrodt, E.T. Maintaining fluid and electrolyte balance during exercise. J. Pharm. Pract. 2003, 16, 45–50. [Google Scholar] [CrossRef]
- Jeukendrup, A.E.; Jentjens, R.L.; Moseley, L. Nutritional considerations in triathlon. Sports Med. 2005, 35, 163–181. [Google Scholar] [CrossRef] [PubMed]
- Speedy, D.B.; Rogers, I.R.; Noakes, T.D.; Wright, S.; Thompson, J.M.; Campbell, R.; Hellemans, I.; Kimber, N.E.; Boswell, D.R.; Kuttner, J.A. Exercise-induced hyponatremia in ultradistance triathletes is caused by inappropriate fluid retention. Clin. J. Sport Med. 2000, 10, 272–278. [Google Scholar] [CrossRef] [PubMed]
| Author | Oxygen Uptake (mL·kg−1·min−1) and Sample Size (n) | Experimental Conditions | Exercise and Nutrition/Supplementation Intervention | Biomarker Response |
|---|---|---|---|---|
| Ashton et al., (2003) [31] | 49 ± 3, n = 10 | Laboratory (temperate) | 1000 mg of l-ascorbic acid (vitamin C) 2 h before exercise. Incremental cycle test to exhaustion. | L-ascorbic acid: ↓ LPS |
| Bishop et al., (2001) [36] | 49 ± 3, n = 7 | Laboratory (22 °C, 56% RH) | 3 day Low-CHO or High-CHO diet. 60 min cycle at 60% Wmax and TT | High-CHO: ↓ IL-6 Low-CHO: ↑ IL-6 |
| Buckley et al., (2009) [23] | 53 ± 2, n = 30 | Laboratory (temperate) | 8 week daily supplementation 60 g Bovine Colostrum. Running 3 times per week for 45 min at lactate threshold. | Bovine Colostrum: ↑ L:R |
| Cox et al., (2010) [37] | 65 ± 5, n = 16 | Laboratory (temperate) | 28 day Moderate-CHO or High-CHO diet. 100 min steady state cycling at 70% VO2 max and ~30 min TT. | Moderate-CHO: ↑ IL-6 High-CHO: ↑ IL-6, |
| Moncada-Jiménez et al., (2010) [24] | 57 ± 7, n = 11 | Laboratory (temperate) | 48 h Low-CHO or High-CHO. Duathlon, 5 km run, 30 min stationary cycle, 10 km run. | Low-CHO: ↑ IL-6 and LPS-LPB High-CHO: ↑ IL-6 and LPS-LPB |
| Morrison et al., (2014) [19] | 64 ± 4, n = 7 46 ± 4, n = 8 | 30 °C, 50% RH | 1 week daily supplementation 1.7 g·kg−1 Bovine Colostrum. 30 min cycling at 50% HRR, 30 min running at 80% HRR | Bovine Colostrum: ↑ IL-6 and I-AFBP |
| Shing et al., (2014) [22] | 63 ± 6, n = 10 | 35 °C, 40% RH | 4 weeks daily supplementation probiotics capsule. Running at to exhaustion at 80% of ventilatory threshold | Probiotic: ↓ L:R and LPS Probiotic and Placebo: ↑ IL-6 |
| Pugh et al., (2017) [21] | 52 ± 5, n = 10 | 30 °C, 40–45% RH | 0.25, 0.5 or 0.9 g·kg−1 glutamine 2 h before exercise. 60 min treadmill run at 70% of VO2 max | 0.25, 0.5 and 0.9 g.kg−1 ↓ L:R 0.5 and 0.9 g.kg−1 ↓ I-AFBP |
| Snipe et al., (2017) [20] | 54 ± 6, n = 11 | 35 °C, 27% RH | Water or CHO (15 g) or energy-matched PRO before and every 20 min during 2 h running at 60% VO2 max | CHO and PRO: ↓ I-AFBP and L:R CHO: ↓ IL-6 and LPS |
| Van Wijck et al., (2012) [13] | Well trained, n = 9 | Laboratory (temperate) | 400 mg ibuprofen 1 h before exercise. Cycling at 70% Wmax, ↓ by 25 W until exhaustion. | Ibuprofen: ↑ I-AFBP and L:R |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guy, J.H.; Vincent, G.E. Nutrition and Supplementation Considerations to Limit Endotoxemia When Exercising in the Heat. Sports 2018, 6, 12. https://doi.org/10.3390/sports6010012
Guy JH, Vincent GE. Nutrition and Supplementation Considerations to Limit Endotoxemia When Exercising in the Heat. Sports. 2018; 6(1):12. https://doi.org/10.3390/sports6010012
Chicago/Turabian StyleGuy, Joshua H., and Grace E. Vincent. 2018. "Nutrition and Supplementation Considerations to Limit Endotoxemia When Exercising in the Heat" Sports 6, no. 1: 12. https://doi.org/10.3390/sports6010012





