The Effect of Anchor Volume on the Mechanical Strengths of Orthodontic Micro-Implants
Abstract
:1. Introduction
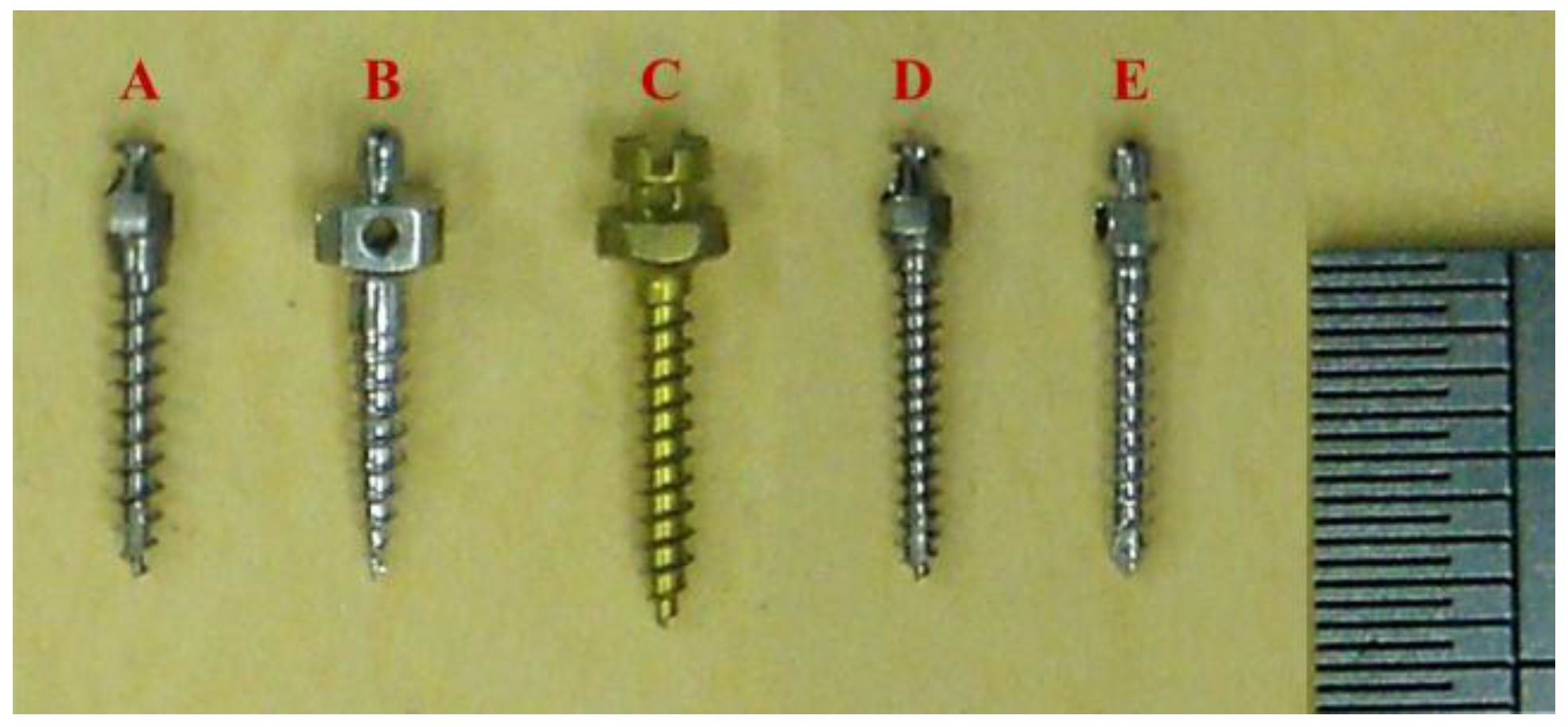
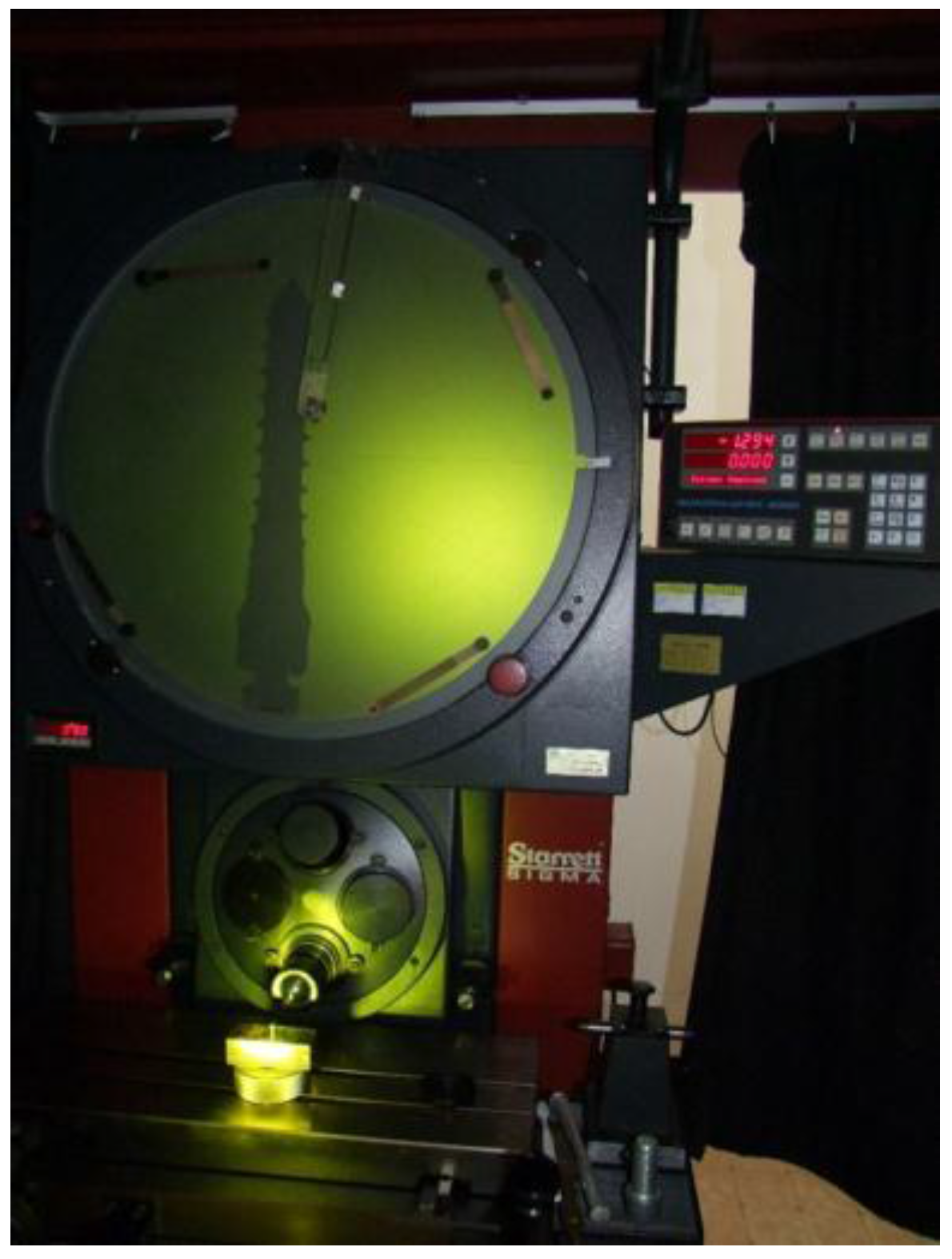
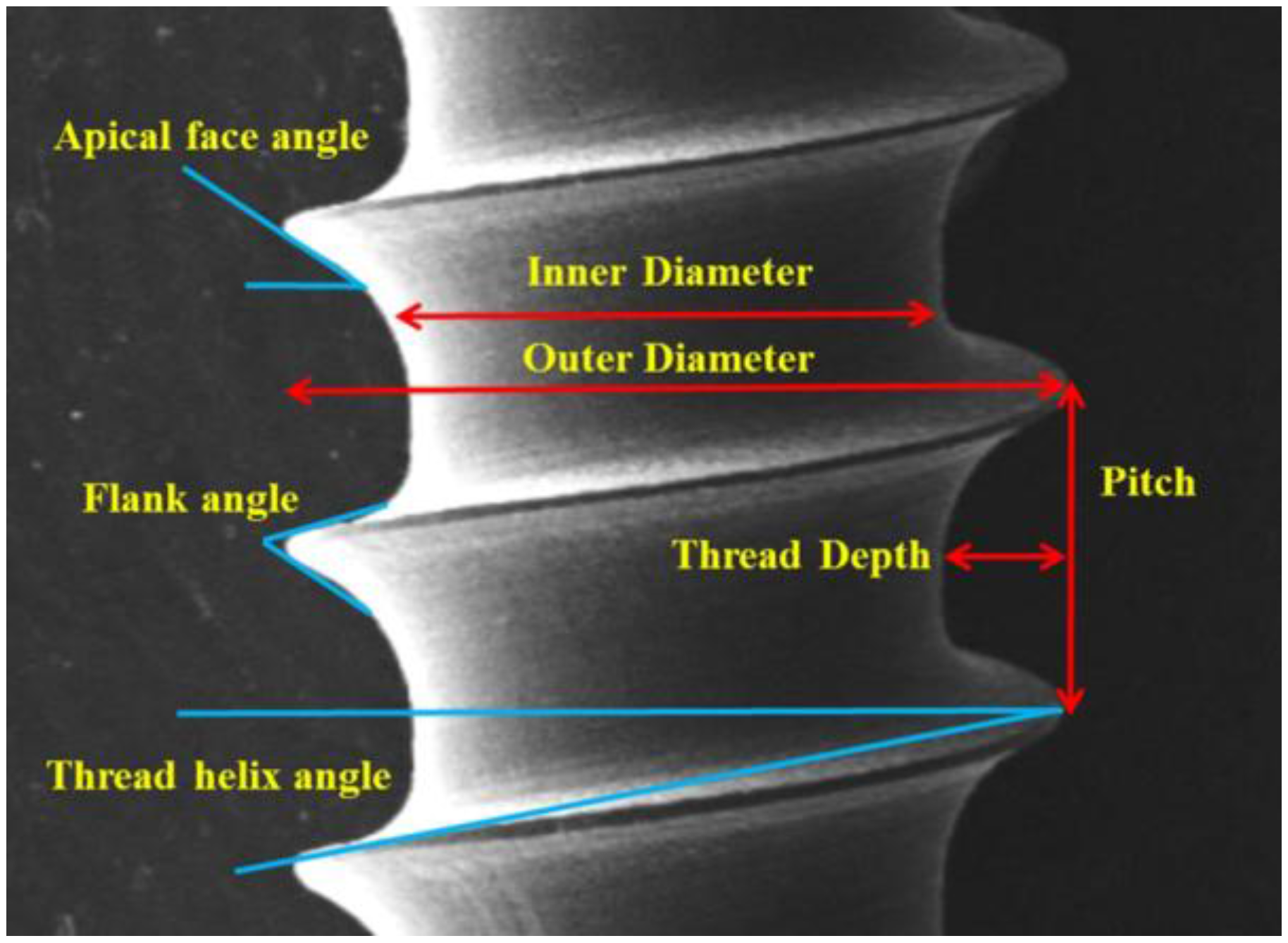
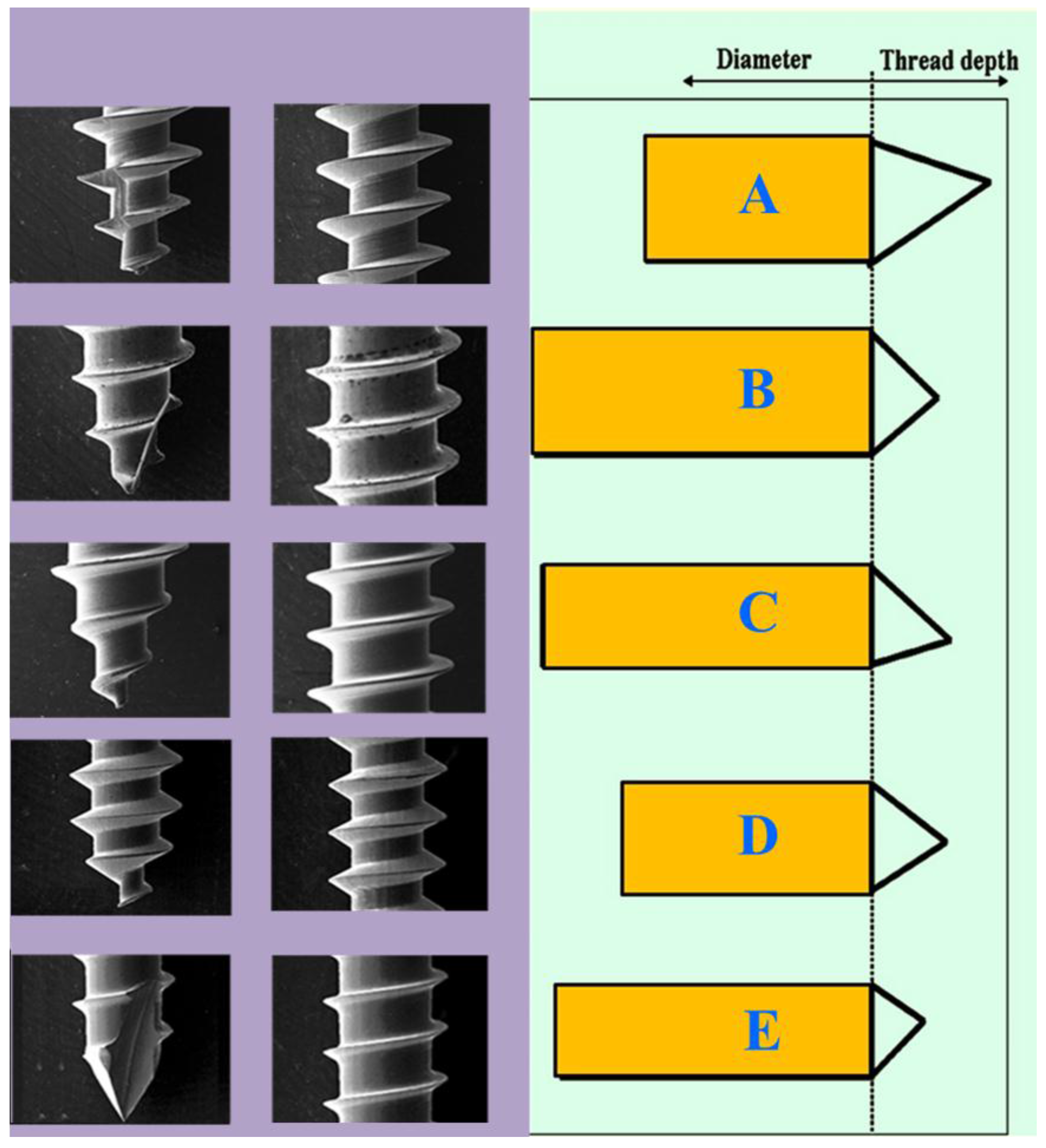
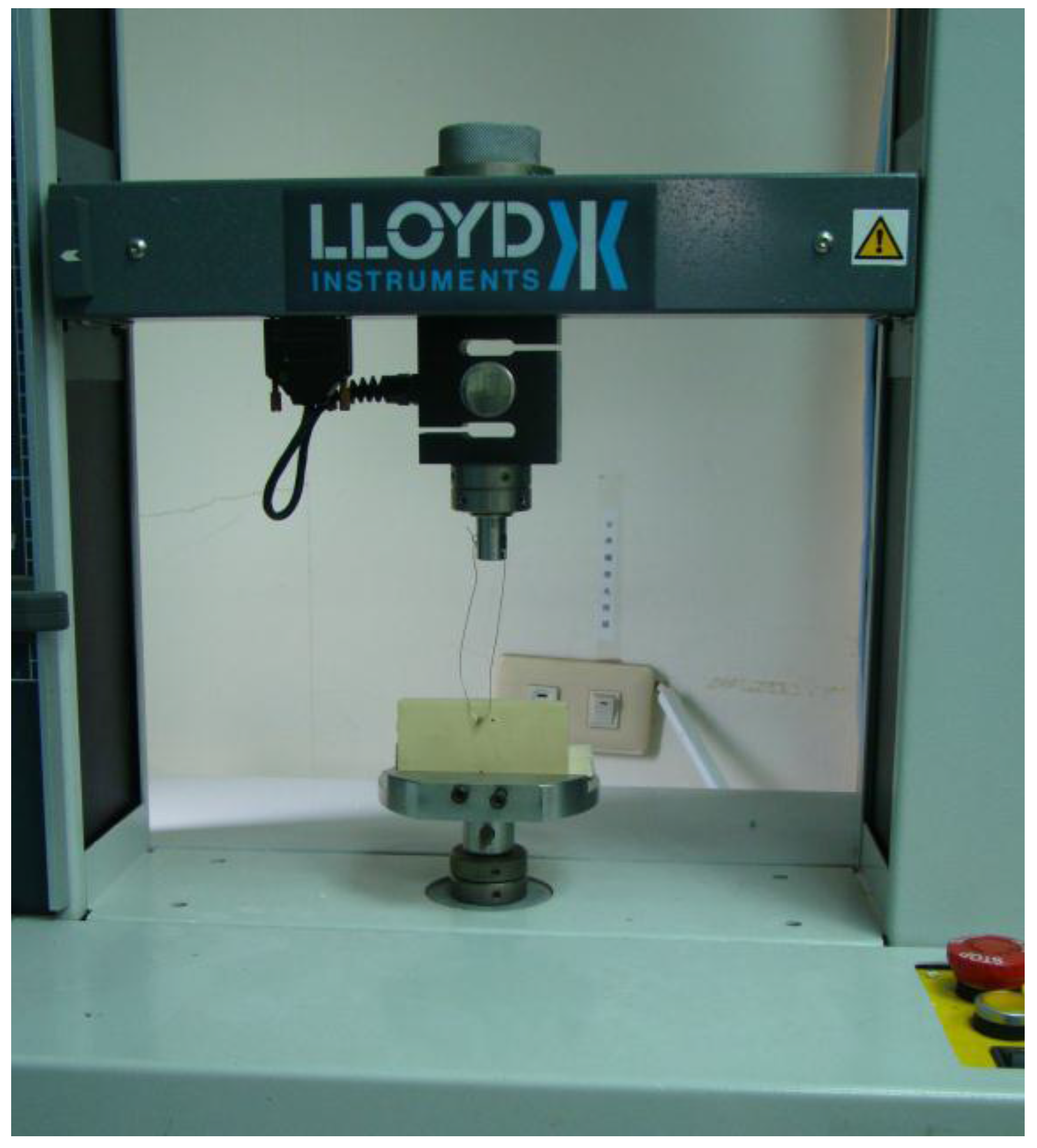
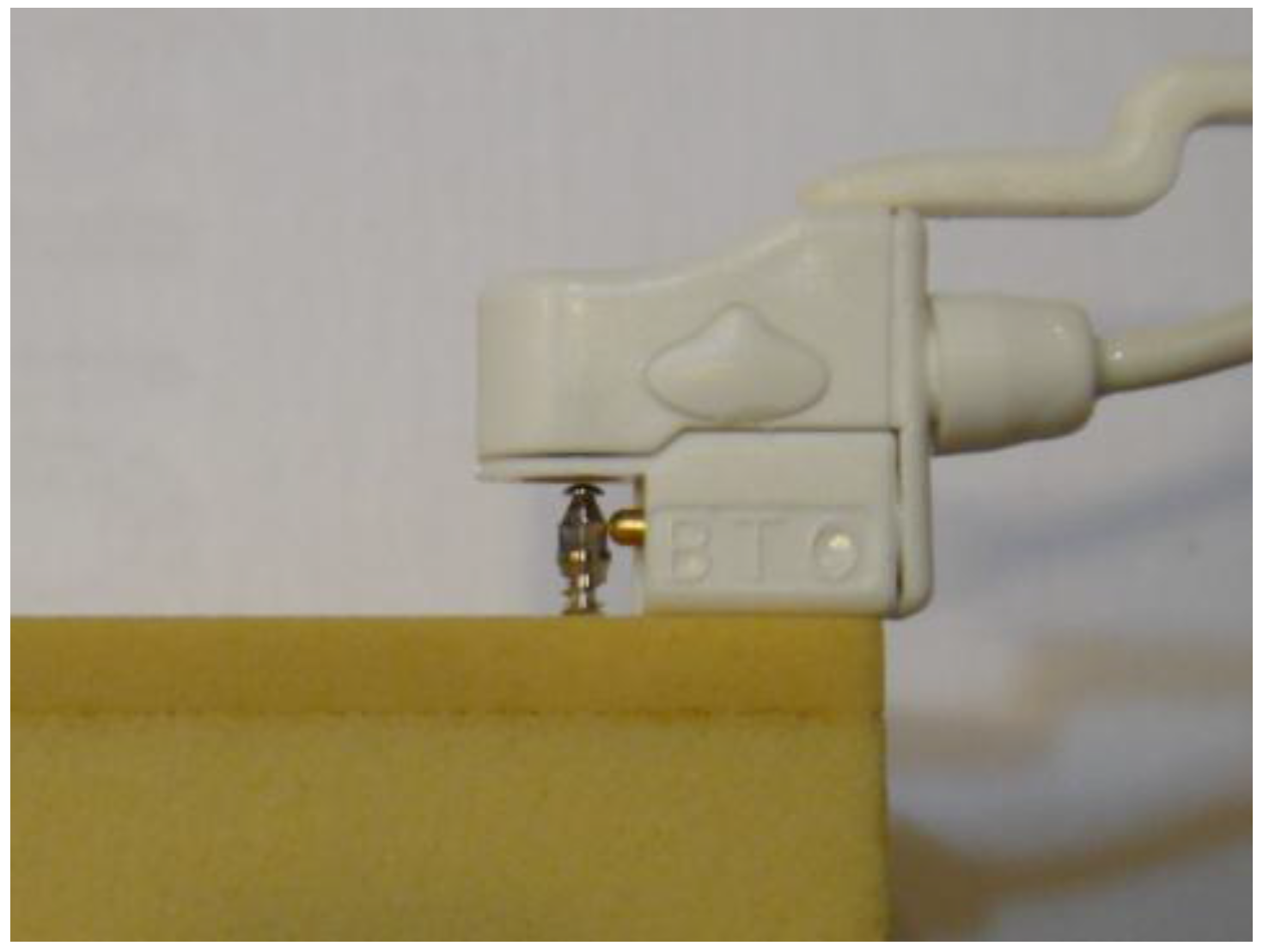
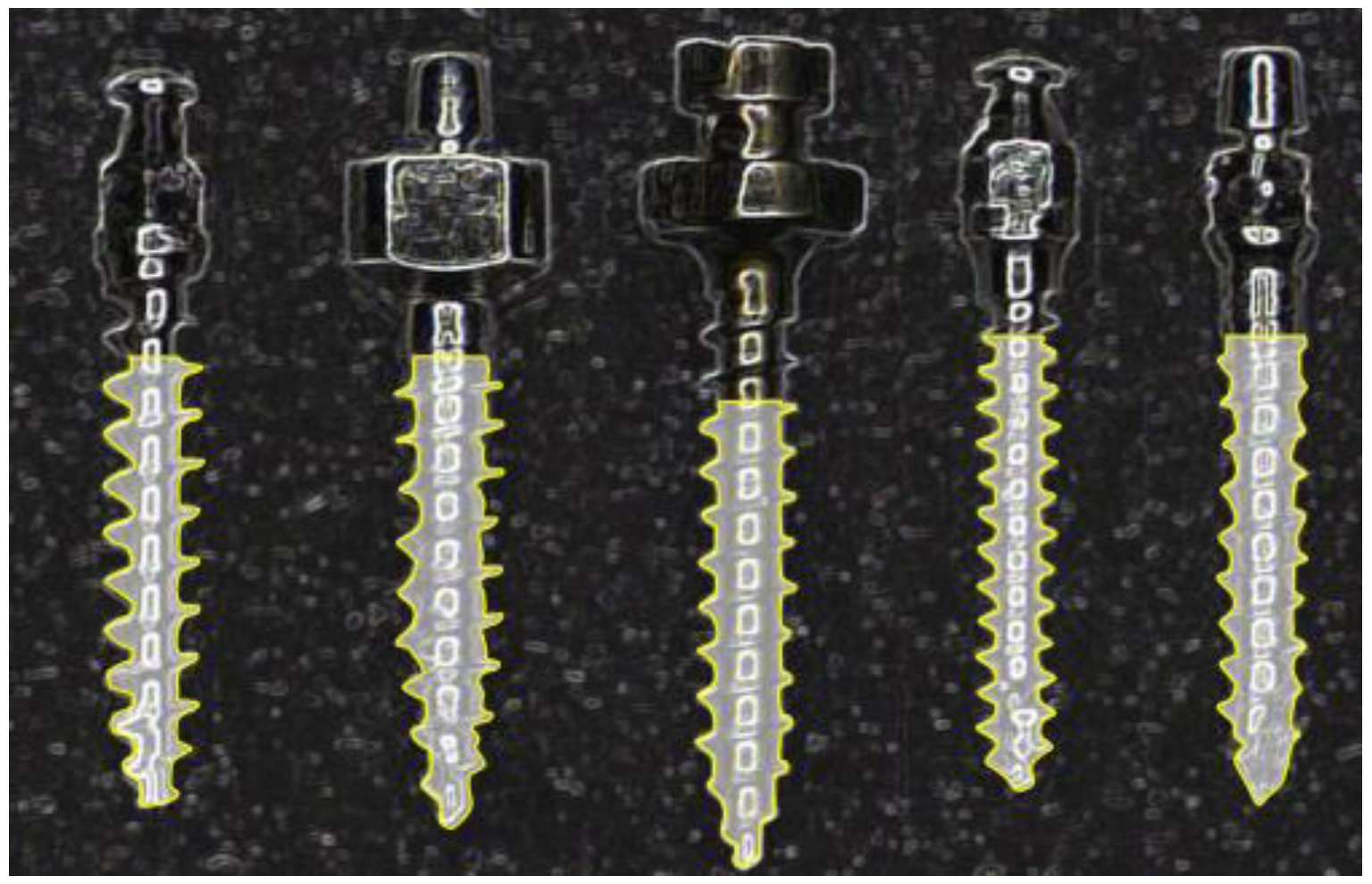
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Kanomi, R. Mini-implant for orthodontic anchorage. J. Clin. Orthod. 1997, 31, 763–767. [Google Scholar] [PubMed]
- Park, H.S. The skeletal cortical anchorage using titanium microscrew implants. Kor. J. Orthod. 1999, 29, 699–706. [Google Scholar]
- Tseng, Y.C.; Hsieh, C.H.; Chen, C.H.; Shen, Y.S.; Huang, I.Y.; Chen, C.M. The application of mini-implants for orthodontic anchorage. Int. J. Oral Maxillofac. Surg. 2006, 35, 704–707. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.Y.; Kuang, S.H.; Wu, C.H. Factors associated with the stability of mini-implants for orthodontic anchorage: A study of 414 samples in Taiwan. J. Oral Maxillofac. Surg. 2009, 67, 1595–1599. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, J.C.; Suarez, F.; Chan, H.L.; Padial-Molina, M.; Wang, H.L. Implants for orthodontic anchorage: Success rates and reasons of failures. Implant Dent. 2014, 23, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.M.; Wu, J.H.; Lu, P.C.; Wang, H.C.; Lee, H.E.; Wang, C.H.; Du, J.K. Horizontal pull-out strength of orthodontic infrazygomatic mini-implant: An in vitro study. Implant Dent. 2011, 20, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Meira, T.M.; Tanaka, O.M.; Ronsani, M.M.; Maruo, I.T.; Guariza-Filho, O.; Camargo, E.S.; Maruo, H. Insertion torque, pull-out strength and cortical bone thickness in contact with orthodontic mini-implants at different insertion angles. Eur. J. Orthod. 2013, 35, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Pithon, M.M.; Figueiredo, D.S.; Oliveira, D.D. Mechanical evaluation of orthodontic mini-implants of different lengths. J. Oral Maxillofac. Surg. 2013, 71, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Z.; Chen, Y.J.; Tung, Y.Y.; Chiang, Y.Y.; Lai, E.H.; Chen, W.P.; Lin, C.P. Effects of thread depth, taper shape, and taper length on the mechanical properties of mini-implants. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Al-Juboori, M.J.; AbdulRahaman, S.B.; Hassan, A. The correlation between crestal bone resorption and implant stability during healing period using resonance frequency analysis. Implant Dent. 2013, 22, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Makary, C.; Rebaudi, A.; Sammartino, G.; Naaman, N. Implant primary stability determined by resonance frequency analysis: Correlation with insertion torque, histologic bone volume, and torsional stability at 6 weeks. Implant Dent. 2012, 21, 474–480. [Google Scholar] [CrossRef] [PubMed]
- Fuster-Torres, M.Á.; Peñarrocha-Diago, M.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Relationships between bone density values from cone beam computed tomography, maximum insertion torque, and resonance frequency analysis at implant placement: A pilot study. Int. J. Oral Maxillofac. Implants 2011, 26, 1051–1056. [Google Scholar] [PubMed]
- Brown, R.N.; Sexton, B.E.; Gabriel Chu, T.M.; Katona, T.R.; Stewart, K.T.; Kyung, H.M.; Liu, S.S. Comparison of stainless steel and titanium alloy orthodontic miniscrew implants: A mechanical and histologic analysis. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 496–504. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.H.; Park, Y.C.; Hwang, C.J.; Kim, J.Y.; Choi, E.H.; Cha, J.Y. A comparison of tapered and cylindrical miniscrew stability. Eur. J. Orthod. 2014, 36, 557–562. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, E.Y.; Suzuki, B.; Aramrattana, A.; Harnsiriwattanakit, K.; Kowanich, N. Assessment of miniscrew implant stability by resonance frequency analysis: A study in human cadavers. J. Oral Maxillofac. Surg. 2010, 68, 2682–2689. [Google Scholar] [CrossRef] [PubMed]
- Nienkemper, M.; Wilmes, B.; Pauls, A.; Drescher, D. Mini-implant stability at the initial healing period: A clinical pilot study. Angle Orthod. 2014, 84, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Hung, E.; Oliver, D.; Kim, K.B.; Kyung, H.M.; Buschang, P.H. Effects of pilot hole size and bone density on miniscrew implants’ stability. Clin. Implant Dent Relat. Res. 2012, 14, 454–460. [Google Scholar] [CrossRef] [PubMed]
- Salmória, K.K.; Tanaka, O.M.; Guariza-Filho, O.; Camargo, E.S.; de Souza, L.T.; Maruo, H. Insertional torque and axial pull-out strength of mini-implants in mandibles of dogs. Am. J. Orthod. Dentofac. Orthop. 2008, 133, e15–e22. [Google Scholar] [CrossRef] [PubMed]

| Micro-implant | A | B | C | D | E |
|---|---|---|---|---|---|
| Inner diameter | 0.84 | 1.11 | 1.02 | 0.87 | 1.20 |
| Outer diameter | 1.50 | 1.57 | 1.50 | 1.33 | 1.33 |
| Inner diameter/ | 0.56 | 0.71 | 0.68 | 0.65 | 0.84 |
| Outer diameter | |||||
| Thread pitch | 0.70 | 0.68 | 0.65 | 0.50 | 0.60 |
| Thread depth | 0.33 | 0.23 | 0.24 | 0.23 | 0.06 |
| Thread angle (degree) | |||||
| Apical face angle | 33.00 | 31.50 | 32.00 | 32.00 | 33.00 |
| Flank angle | 49.00 | 57.00 | 46.00 | 58.50 | 56.50 |
| Thread helix angle | 20.50 | 11.50 | 12.00 | 14.50 | 11.50 |
| Micro-Implant | Resonance Frequency | Insertion Torque | Horizontal Pullout | Anchor Volume | ||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| A | 9.0 | 0.02 | 4.2 | 0.82 | 159.9 | 13.91 | 4.6 | 0.40 |
| B | 8.4 | 0.28 | 7.4 | 2.26 | 190.9 | 14.93 | 7.6 | 0.39 |
| C | 9.9 | 0.21 | 7.1 | 1.86 | 180.0 | 15.53 | 7.3 | 0.22 |
| D | 6.8 | 0.30 | 4.2 | 0.38 | 162.5 | 6.48 | 3.5 | 0.92 |
| E | 7.1 | 0.18 | 6.9 | 0.82 | 183.7 | 11.17 | 6.8 | 0.49 |
| Intergroup | C > A, C > B, C > E | B > A, B > D, C > A | B > A, B > D | B > A, B > D, C > A | ||||
| Comparison * | C > D, A > B, A > E | C > D, E > A, E > D | C > D, E > A, E > D | |||||
| A > D, B > E, B > D | A > D | |||||||
| Variables | Correlation Coefficient | |||
|---|---|---|---|---|
| RF | IT | HPS | AV | |
| RF | 1.000 | 0.026 | 0.069 | 0.436 * |
| IT | 0.026 | 1.000 | 0.550 * | 0.742 * |
| HPS | 0.069 | 0.550 * | 1.000 | 0.653 * |
| AV | 0.436 * | 0.742 * | 0.653 * | 1.000 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tseng, Y.-C.; Wu, J.-H.; Ting, C.-C.; Wang, H.-C.; Chen, H.-S.; Chen, C.-M. The Effect of Anchor Volume on the Mechanical Strengths of Orthodontic Micro-Implants. Metals 2017, 7, 112. https://doi.org/10.3390/met7040112
Tseng Y-C, Wu J-H, Ting C-C, Wang H-C, Chen H-S, Chen C-M. The Effect of Anchor Volume on the Mechanical Strengths of Orthodontic Micro-Implants. Metals. 2017; 7(4):112. https://doi.org/10.3390/met7040112
Chicago/Turabian StyleTseng, Yu-Chuan, Ju-Hui Wu, Chun-Chan Ting, Huang-Chi Wang, Hong-Sen Chen, and Chun-Ming Chen. 2017. "The Effect of Anchor Volume on the Mechanical Strengths of Orthodontic Micro-Implants" Metals 7, no. 4: 112. https://doi.org/10.3390/met7040112





