Depression Risks and Correlates among Different Generations of Chinese Americans: The Effects of Relationships with Friends and Relatives
Abstract
:1. Introduction
1.1. Generational Differences in Depression among Chinese Americans
1.2. Predictors of Depression among Chinese Americans
2. Methods
2.1. Data Source
2.2. Measures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Conflicts of Interest
References
- Almeida, Joanna, S. V. Subramanian, Ichiro Kawachi, and Beth E. Molnar. 2011. Is Blood Thicker Than Water? Social Support, Depression and the Modifying Role of Ethnicity/Nativity Status. Journal of Epidemiology and Community Health 65: 51–56. [Google Scholar] [CrossRef] [PubMed]
- Bartley, Allen, and Paul Spoonley. 2008. Intergenerational Transnationalism: 1.5 Generation Asian Migrants in New Zealand. International Migration 46: 63–84. [Google Scholar] [CrossRef]
- Berry, John W. 1990. Acculturation and Adaptation: A General Framework. In Mental Health of Immigrants and Refugees. Edited by Wayne H. Holtzman and Thomas H. Bornemann. Austin: Hogg Foundation for Mental Health, pp. 90–102. [Google Scholar]
- Berry, John W. 2003. Conceptual Approaches to Acculturation. In Acculturation: Advances in Theory, Measurement, and Applied Research. Edited by K. M. Chun, P. Balls Organista and G. Marín. Washington: American Psychological Association, pp. 17–37. [Google Scholar]
- Canino, Glorisa, William A. Vega, William M. Sribney, Lynn A. Warner, and Margarita Alegría. 2008. Social Relationships, Social Assimilation, and Substance Use Disorders among Adult Latinos in the U.S. Journal of Drug Issues 38: 69–101. [Google Scholar] [CrossRef] [PubMed]
- Chen, Irene G., Robert E. Roberts, and Lu A. Aday. 1998. Ethnicity and Adolescent Depression: The Case of Chinese Americans. Journal of Nervous 186: 623–30. [Google Scholar] [CrossRef]
- Cheung, Chau-Kiu, and Christopher Bagley. 1998. Validating An American Scale in Hong Kong: The Center for Epidemiological Studies Depression Scale (CES-D). Journal of Psychology 132: 169. [Google Scholar] [CrossRef] [PubMed]
- Chou, Kee-Lee, Iris Chi, and Nelson W. S. Chow. 2004. Sources of Income and Depression in Elderly Hong Kong Chinese: Mediating and Moderating Effects of Social Support and Financial Strain. Aging & Mental Health 8: 212–21. [Google Scholar]
- CPES. 2007. Collaborative Psychiatric Epidemiology Surveys (CPES), 2001–2003 User’s Guide. Available online: http://www.icpsr.umich.edu/icpsrweb/ICPSR/studies/20240 (accessed on 31 March 2017).
- CPES. 2008. CPES Weights Charts. Available online: http://www.icpsr.umich.edu/files/CPES/CPES%20Weights%20Chart.pdf (accessed on 31 March 2017).
- Das, Ajit K., and Sharon F. Kemp. 1997. Between Two Worlds: Counseling South Asian Americans. Journal of Multicultural Counseling and Development 25: 23–33. [Google Scholar] [CrossRef]
- Fong, Timothy P. 2007. The Contemporary Asian American Experience: Beyond the Model Minority, 3rd ed. Upper Saddle River: Pearson. [Google Scholar]
- Gao, Ling-ling, Sally Wai-chi Chan, and Qing Mao. 2009. Depression, Perceived Stress, and Social Support among First-Time Chinese Mothers and Fathers in the Postpartum Period. Research in Nursing & Health 32: 50–58. [Google Scholar]
- Gee, Gilbert C., Michael Spencer, Juan Chen, Tiffany Yip, and David T. Takeuchi. 2007. The Association between Self-Reported Racial Discrimination and 12-Month DSM-IV Mental Disorders among Asian Americans Nationwide. Social Science & Medicine 64: 1984–96. [Google Scholar]
- Goebert, Deborah. 2009. Social Support, Mental Health, Minorities, and Acculturative Stress. In Determinants of Minority Mental Health and Wellness. Edited by S. Loue and M. Sajatovic. New York: Springer, pp. 1–24. [Google Scholar]
- Greenberger, Ellen, and Chuansheng Chen. 1996. Perceived Family Relationships and Depressed Mood in Early and Late Adolescence: A Comparison of European and Asian Americans. Developmental Psychology 32: 707–16. [Google Scholar] [CrossRef]
- Heeringa, Steven G., James Wagner, Myriam Torres, Naihua Duan, Terry Adams, and Patricia Berglund. 2004. Sample Designs and Sampling Methods for the Collaborative Psychiatric Epidemiology Studies (CPES). International Journal of Methods in Psychiatric Research 13: 221–40. [Google Scholar] [CrossRef] [PubMed]
- Hoeffel, Elizabth M., Sonya Rastogi, Myoung Ouk Kim, and Hasan Shahid. 2012. The Asian Population: 2010. In 2010 Census Briefs; Suitland: U.S. Census Bureau. [Google Scholar]
- Huang, Frederick Y., Henry Chung, Kurt Kroenke, Kevin L. Delucchi, and Robert L. Spitzer. 2006. "Using the Patient Health Questionnaire-9 to Measure Depression among Racially and Ethnically Diverse Primary Care Patients". Journal of General Internal Medicine 21(6): 547–52. [Google Scholar] [CrossRef] [PubMed]
- Hwang, Wei-Chin, Hector F. Myers, and David T. Takeuchi. 2000. "Psychosocial Predictors of First-Onset Depression in Chinese Americans". Social Psychiatry and Psychiatric Epidemiology 35(3): 133–45. [Google Scholar] [CrossRef]
- Hwu, Hao-Gwo, I-Hao Chang, Eng-Kung Yeh, Ching-Jui Chang, and Ling-Ling Yeh. 1996. Major Depressive Disorder in Taiwan Defined by the Chinese Diagnostic Interview Schedule. The Journal of Nervous and Mental Disease 184(8): 497–502. [Google Scholar] [CrossRef]
- Jackson, James S., Myriam Torres, Cleopatra H. Caldwell, Harold W. Neighbors, Randolph M. Nesse, Robert Joseph Taylor, Steven J. Trierweiler, and David R. Williams. 2004. The National Survey of American Life: A Study of Racial, Ethnic and Cultural Influences on Mental Disorders and Mental Health. International Journal of Methods in Psychiatric Research 13: 196–207. [Google Scholar] [CrossRef] [PubMed]
- Juang, Linda P., and Alvin A. Alvarez. 2010. Discrimination and Adjustment among Chinese American Adolescents: Family Conflict and Family Cohesion as Vulnerability and Protective Factors. American Journal of Public Health 100: 2403–9. [Google Scholar] [CrossRef] [PubMed]
- Juang, Linda P., Moin Syed, and Miyuki Takagi. 2007. Intergenerational Discrepancies of Parental Control among Chinese American Families: Links to Family Conflict and Adolescent Depressive Symptoms. Journal of Adolescence 30: 965–75. [Google Scholar] [CrossRef] [PubMed]
- Kalibatseva, Zornitsa, and Frederick T. Leong. 2011. Depression among Asian Americans: Review and Recommendations. Depression Research and Treatment 2011: 9. [Google Scholar] [CrossRef] [PubMed]
- Kessler, Ronald C., and T. Bedirhan Üstün. 2004. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research 13: 93–121. [Google Scholar] [CrossRef] [PubMed]
- Kessler, Ronald C., Katherine A. McGonagle, Shanyang Zhao, Christopher B. Nelson, Michael Hughes, Suzann Eshleman, Hans-Ulrich Wittchen, and Kenneth Kendler. 1994. Lifetime and 12-Month Prevalence of DSM-III-R Psychiatric Disorders in the United States Results from the National Comorbidity Survey. Archives of General Psychiatry 51: 8–19. [Google Scholar] [CrossRef] [PubMed]
- Kessler, Ronald C., Patricia Berglund, Wai Tat Chiu, Olga Demler, Steven Heeringa, Eva Hiripi, Robert Jin, Beth-Ellen Pennell, Ellen E. Walters, Alan Zaslavsky, and Hui Zheng. 2004. The US National Comorbidity Survey Replication (NCS-R): Design and Field Procedures. International Journal of Methods in Psychiatric Research 13: 69–92. [Google Scholar] [CrossRef]
- Kim, Hyoun K., and Patrick C. McKenry. 2002. The Relationship between Marriage and Psychological Well-being A Longitudinal Analysis. Journal of Family Issues 23: 885–911. [Google Scholar] [CrossRef]
- Kim, Bryan S. K., Bradley R. Brenner, Christopher T. H. Liang, and Penelope A. Asay. 2003. A Qualitative Study of Adaptation Experiences of 1.5-Generation Asian Americans. Cultural Diversity & Ethnic Minority Psychology 9: 156–70. [Google Scholar]
- Kleinman, Arthur M. 1977. Depression, Somatization and the “New Cross-cultural Psychiatry”. Social Science & Medicine 11: 3–9. [Google Scholar]
- Kleinman, Arthur M. 1982. Neurasthenia and Depression: A Study of Somatization and Culture in China. Culture, Medicine and Psychiatry 6: 117–90. [Google Scholar] [CrossRef] [PubMed]
- Kriegsman, Didi M. W., Brenda W. J. H. Penninx, Jacques Th. M. Van Eijk, A. Joan P. Boeke, and Dorly J. H. Deeg. 1996. Self-Reports and General Practitioner Information on the Presence of Chronic Diseases in Community Dwelling Elderly. Journal of Clinical Epidemiology 49: 1407–17. [Google Scholar] [CrossRef]
- Kuo, Wen H. 1984. Prevalence of Depression among Asian-Americans. The Journal of Nervous and Mental Disease 172: 449–57. [Google Scholar] [CrossRef] [PubMed]
- Lai, Daniel W. 2004. Depression among Elderly Chinese-Canadian Immigrants from Mainland China. Chinese Medical Journal 117: 677–83. [Google Scholar] [PubMed]
- Lee, Minsun. 2011. Generational Diversity among Immigrants. The Clinical Psychologist 64: 11–12. [Google Scholar]
- Lee, Sing, S. C. Fung, A. Tsang, Z. R. Liu, Y. Q. Huang, Y. L. He, M. Y. Zhang, Y. C. Shen, M. K. Nock, and Ronald C. Kessler. 2007. Lifetime Prevalence of Suicide Ideation, Plan, and Attempt in Metropolitan China. Acta Psychiatrica Scandinavic 116: 429–37. [Google Scholar] [CrossRef] [PubMed]
- Lee, Sing, A. Tsang, Y. Q. Huang, Y.-L. He, Z. R. Liu, M.-Y. Zhang, Y.-C. Shen, and Ronald C. Kessler. 2009. The Epidemiology of Depression in Metropolitan China. Psychological Medicine 39: 735–47. [Google Scholar] [CrossRef] [PubMed]
- Lee, Minsun, David T. Takeuchi, Zvi Gellis, Philip Kendall, Lin Zhu, Shanyang Zhao, and Grace X. Ma. 2016. The Impact of Perceived Need and Relational Factors on Mental Health Service Use among Generations of Asian Americans. Journal of Community Health, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Leu, Janxin, Irene H. Yen, Stuart A. Gansky, Emily Walton, Nancy E. Adler, and David T. Takeuchi. 2008. The Association between Subjective Social Status and Mental Health among Asian Immigrants: Investigating the Influence of Age at Immigration. Social Science & Medicine 66: 1152–64. [Google Scholar]
- Leung, C. M., K. K. Chan, and K. K. Cheng. 1992. Psychiatric morbidity in a general medical ward. Hong Kong’s experience. General Hospital Psychiatry 14: 196–200. [Google Scholar] [CrossRef]
- Lieber, Eli, Dorothy Chin, Kazuo Nihira, and Iris T. Mink. 2001. Holding on and Letting Go: Identity and Acculturation among Chinese Immigrants. Cultural Diversity and Ethnic Minority Psychology 7: 247–61. [Google Scholar] [CrossRef] [PubMed]
- Lin, Nan. 1989. Measuring Depressive Symptomatology in China. Journal of Nervous and Mental Disease 177: 121–31. [Google Scholar] [CrossRef] [PubMed]
- Marsella, Anthony J. 1978. Thoughts on Cross-Cultural Studies on the Epidemiology of Depression. Culture, Medicine and Psychiatry 2: 343–57. [Google Scholar] [PubMed]
- Mezzich, Juan E., Laurence J. Kirmayer, Arthur M. Kleinman, Horatio Fabrega, Delores L. Parron, Buron J. Good, Keh-Ming Lin, and Spero M. Manson. 1999. The Place of Culture in DSM-IV. The Journal of Nervous and Mental Disease 187: 457–64. [Google Scholar] [CrossRef] [PubMed]
- Mui, Ada C. 1999. Living Alone and Depression among Older Chinese Immigrants. Journal of Gerontological Social Work 30: 147–66. [Google Scholar] [CrossRef]
- Mulvaney-Day, Norah E., Margarita Alegría, and William Sribney. 2007. Social Cohesion, Social Support, and Health among Latinos in the United States. Social Science & Medicin 64: 477–95. [Google Scholar]
- Nguyen, Duy, and Lindsay A. Bornheimer. 2014. Mental Health Service Use Types among Asian Americans with a Psychiatric Disorder: Considerations of Culture and Need. The Journal of Behavioral Health Services & Research 41: 520–28. [Google Scholar]
- Nicdao, Ethel G., Seunghye Hong, and David T. Takeuchi. 2008. Social Support and the Use of Mental Health Services among Asian Americans: Results from the National Latino and Asian American Study. Research in the Sociology of Health Care 26: 167–84. [Google Scholar]
- Obradović, Jelena, Nicole Tirado-Strayer, and Janxin Leu. 2013. The Importance of Family and Friend Relationships for the Mental Health of Asian Immigrant Young Adults and Their Nonimmigrant Peers. Research in Human Development 10: 163–83. [Google Scholar]
- Park, Kyeyoung. 1999. "I Really Do Feel I’m 1.5!": The Construction of Self and Community by Young Korean Americans. Amerasia Journal 25: 139–63. [Google Scholar] [CrossRef]
- Portes, Alejandro, and Rubén G. Rumbaut. 2001. Legacies: The Story of the Immigrant Second Generation. Oakland: University of California Press. [Google Scholar]
- Qin, Desirée Boalian, Niobe Way, and Preetika Mukherjee. 2008. The Other Side of the Model Minority Story the Familial and Peer Challenges Faced by Chinese American Adolescents. Youth & Society 39: 480–506. [Google Scholar]
- Radloff, Lenore S. 1977. The CES-D Scale A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement 1: 385–401. [Google Scholar] [CrossRef]
- Rumbaut, Rubén G. 1994. The Crucible within: Ethnic Identity, Self-Esteem, and Segmented Assimilation among Children of Immigrants. The International Migration Review 28: 748–94. [Google Scholar] [CrossRef]
- Salant, Talya, and Diane S. Lauderdale. 2003. Measuring Culture: A Critical Review of Acculturation and Health in Asian Immigrant Populations. Social Science & Medicine 57: 71–90. [Google Scholar]
- Sangalang, Cindy C., and Gilbert C. Gee. 2012. Depression and Anxiety among Asian Americans: The Effects of Social Support and Strain. Social Work 57: 49–60. [Google Scholar] [CrossRef] [PubMed]
- Schmid, Carol L. 2001. Educational Achievement, Language-Minority Students, and the New Second Generation. Sociology of Education 74: 71–87. [Google Scholar] [CrossRef]
- Shen, Biing-Jiun, and David T. Takeuchi. 2001. A Structural Model of Acculturation and Mental Health Status among Chinese Americans. American Journal of Community Psychology 29: 387–418. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. 2015. Stata Statistical Software: Release 14. College Station: StataCorp LP. [Google Scholar]
- Stice, Eric, Jennifer Ragan, and Patrick Randall. 2004. Prospective Relations between Social Support and Depression: Differential Direction of Effects for Parent and Peer Support? Journal of Abnormal Psychology 113: 155–59. [Google Scholar] [CrossRef] [PubMed]
- Tabora, Betty, and Jacquelyn H. Flaskerud. 1994. Depression among Chinese Americans: A Review of the Literature. Issues in Mental Health Nursing 15: 569–84. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, David T., Rita Chi-Ying Chung, Keh-Ming Lin, Haikang Shen, Karen Kurasaki, Chi-Ah Chun, and Stanley Sue. 1998. Lifetime and Twelve-Month Prevalence Rates of Major Depressive Episodes and Dysthymia among Chinese Americans in Los Angeles. American Journal of Psychiatry 155: 1407–14. [Google Scholar] [CrossRef] [PubMed]
- Takeuchi, David T., Nolan Zane, Seunghye Hong, David H. Chae, Fang Gong, Gilbert C. Gee, Emily Walton, Stanley Sue, and Margarita Alegría. 2007. Immigration-Related Factors and Mental Disorders among Asian Americans. American Journal of Public Health 97: 84–90. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Jeanne L., and Robert W. Levenson. 1997. Cultural Influences on Emotional Responding Chinese American and European American Dating Couples during Interpersonal Conflict. Journal of Cross-Cultural Psychology 28: 600–25. [Google Scholar] [CrossRef]
- Tseng, Wen-Shing, and Jing Hsu. 1970. Chinese Culture, Personality Formation and Mental Illness. International Journal of Social Psychiatry 16: 5–14. [Google Scholar] [CrossRef]
- Uba, Laura. 2003. Asian Americans: Personality Patterns, Identity, and Mental Health. New York: Guilford Press. [Google Scholar]
- Waters, Mary C., and Tomás R. Jiménez. 2005. Assessing Immigrant Assimilation: New Empirical and Theoretical Challenges. Annual Review of Sociology 31: 105–25. [Google Scholar] [CrossRef]
- Wei, Meifen, Tsun-Yao Ku, Daniel W. Russell, Brent Mallinckrodt, and Kelly Yu-Hsin Liao. 2008. Moderating Effects of Three Coping Strategies and Self-Esteem on Perceived Discrimination and Depressive Symptoms: A Minority Stress Model for Asian International Students. Journal of Counseling Psychology 55: 451–62. [Google Scholar] [CrossRef] [PubMed]
- Willgerodt, Mayumi Anne, and Elaine Adams Thompson. 2006. Ethnic and Generational Influences on Emotional Distress and Risk Behaviors among Chinese and Filipino American Adolescents. Research in Nursing & Health 29: 311–24. [Google Scholar]
- Wu, Bei, Thanh V. Tran, and Quartel-Ayne Amjad. 2004. Chronic Illnesses and Depression among Chinese Immigrant Elders. Journal of Gerontological Social Work 43: 79–95. [Google Scholar] [CrossRef]
- Ying, Yu-Wen. 1988. Depressive Symptomatology among Chinese-Americans as Measured by the CES-D. Journal of Clinical Psychology 44: 739–46. [Google Scholar] [CrossRef]
- Ying, Yu-Wen, and Meekyung Han. 2007. The Longitudinal Effect of Intergenerational Gap in Acculturation on Conflict and Mental Health in Southeast Asian American Adolescents. American Journal of Orthopsychiatry 77: 61–66. [Google Scholar] [CrossRef] [PubMed]
- Young, Christina B., Daniel Z. Fang, and Sidney Zisook. Depression in Asian-American and Caucasian Undergraduate Students. Journal of Affective Disorders 125: 379–82. [CrossRef] [PubMed]
- Zhang, Amy Y., Lucy C. Yu, Jianping Yuan, Zhifu Tong, Chaoyuan Yang, and Stephen E. Foreman. 1997. Family and Cultural Correlates of Depression among Chinese Elderly. International Journal of Social Psychiatry 43: 199–212. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Min. 1997. Segmented Assimilation: Issues, Controversies, and Recent Research on the New Second Generation. The International Migration Reviews 31: 975–1008. [Google Scholar] [CrossRef]
| 1 | −(−0.71)/0.70 = 1.01, which is −1 times the coefficient for the main effect of being first generation CA divided by the coefficient for the interaction term “1st G CAs × FS.” |
| 2 | − (−0.71)/ −0.62 = −1.14, which is –1 times the coefficient for the main effect of being first generation CA divided by the coefficient for the interaction term “1st G CAs × FC.” |
| 3 | − (−0.23)/−0.89 = −0.26, which is −1 times the coefficient for the main effect of being second generation CAs divided by the coefficient for the interaction term “2nd G CAs × FC.” |
| 1st G CA% or mean (s.e.) | 2nd G CA% or mean (s.e.) | 3rd-or-higher G CA% or mean (s.e.) | Non-Hispanic White% or mean (s.e.) | |
|---|---|---|---|---|
| n | 475 | 74 | 50 | 3892 |
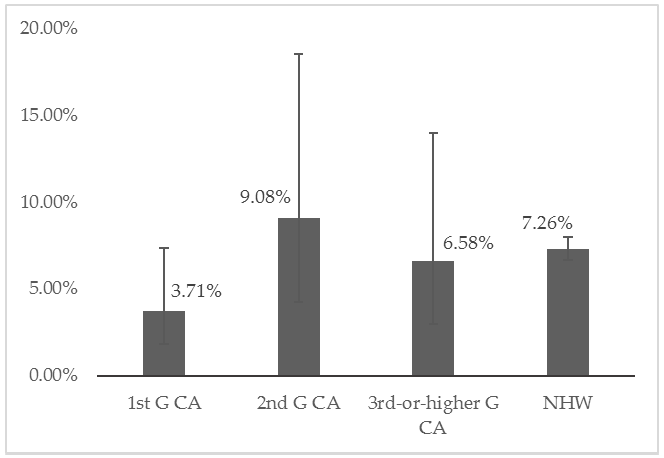
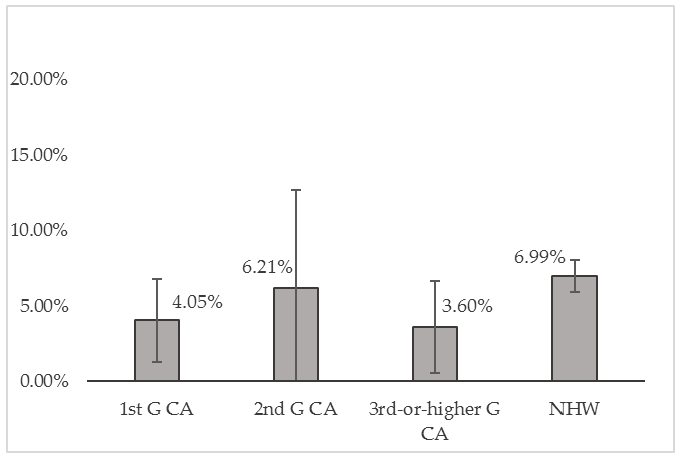
| DSM-IV MDD in 12 months | 3.71% (0.01) | 9.08% (0.03) | 6.58% (0.03) | 7.26% (0.003) |
| female | 54.20% (0.02) | 56.47% (0.07) | 41.84% (0.05) | 51.84% (0.01) |
| age (mean) | 43.67 (1.25) | 39.05 (2.89) | 41.19 (1.61) | 46.70 (0.56) |
| marital status | ||||
| never married | 15.92% (0.02) | 40.64% (0.09) | 28.20% (0.06) | 19.43% (0.01) |
| married/cohabiting | 74.16% (0.02) | 45.19% (0.08) | 50.63% (0.12) | 61.13% (0.01) |
| divorced/separated/widowed | 9.92% (0.02) | 14.17% (0.05) | 21.18% (0.12) | 19.44% (0.01) |
| college degree | 42.58% (0.04) | 55.88% (0.06) | 42.88% (0.06) | 26.84% (0.01) |
| family income level | ||||
| below poverty line | 21.47% (0.03) | 17.52% (0.05) | 16.19% (0.06) | 8.14% (0.01) |
| 1–3 times of poverty line | 16.88% (0.02) | 15.56% (0.06) | 12.29% (0.04) | 25.44% (0.01) |
| 3–6 times of poverty line | 23.18% (0.02) | 23.24% (0.06) | 21.45% (0.13) | 33.04% (0.01) |
| ≥ 6 times of poverty line | 38.47% (0.04) | 43.68% (0.06) | 50.07% (0.17) | 33.38% (0.02) |
| work status | ||||
| employed | 65.08% (0.03) | 57.81% (0.06) | 68.78% (0.12) | 65.95% (0.01) |
| unemployed | 5.28% (0.01) | 4.42% (0.02) | 10.97% (0.09) | 5.07% (0.01) |
| not in labor force | 29.65% (0.03) | 37.77% (0.06) | 20.25% (0.07) | 28.98% (0.01) |
| chronic physical condition | 27.05% (0.03) | 33.40% (0.07) | 47.36% (0.08) | 50.19% (0.01) |
| friend support (z) | –0.40 (0.06) | 0.30 (0.09) | 0.31 (0.14) | 0.29 (0.02) |
| relative support (z) | –0.54 (0.06) | 0.07 (0.15) | 0.02 (0.10) | 0.14 (0.02) |
| friend conflict (z) | –0.02 (0.06) | 0.31 (0.10) | 0.25 (0.10) | –0.03 (0.02) |
| relative conflict (z) | –0.06 (0.05) | 0.17 (0.13) | 0.15 (0.13) | –0.13 (0.02) |
| N = 4491 |
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| NHW (ref) | 1 | 1 | 1 | 1 |
| 1st G CA | –0.81 (0.40)* | –0.83 (0.41) * | –0.86 (0.42) * | –0.71 (0.42) * |
| 2nd G CA | 0.05 (0.44) | 0.04 (0.42) | –1.24 (1.14) | –0.23 (1.14) |
| 3rd-or-higher G CA | –0.39 (0.35) | –0.41 (0.37) | 0.73 (0.68) | –0.77 (0.68) |
| chronic physical condition | 0.96 (0.14) *** | 0.95 (0.15) *** | 0.97 (0.14) *** | |
| 1st G CA * chronic | 0.44 (0.45) | |||
| 2nd G CA * chronic | 0.90 (1.07) | |||
| 3rd-or-higher G CA * chronic | –2.89 (2.34) | |||
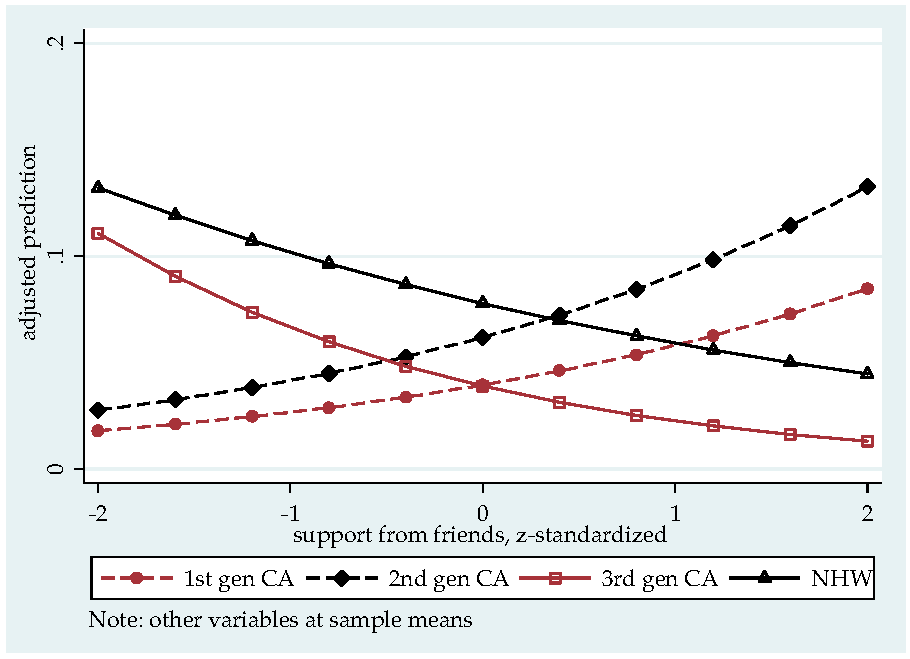
| FS | –0.21 (0.06) *** | –0.20 (0.07) ** | –0.30 (0.09) ** | |
| RS | –0.26 (0.09) ** | –0.30 (0.09) ** | –0.21 (0.06) ** | |
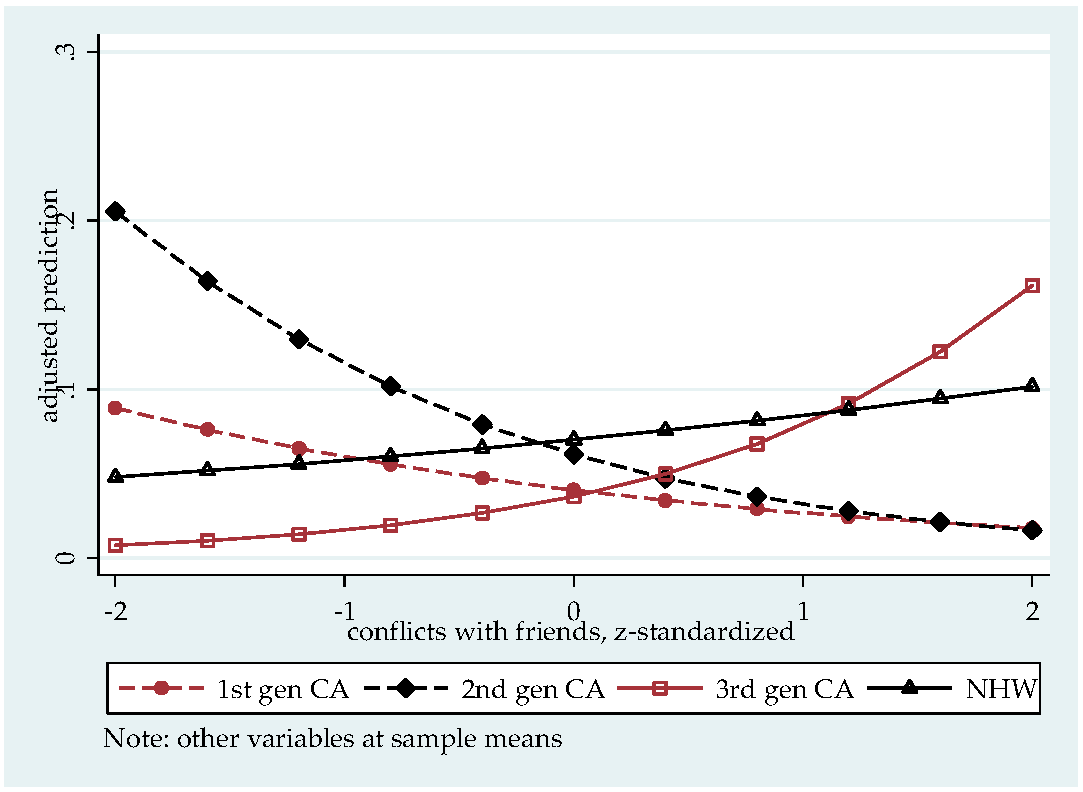
| FC | 0.13 (0.06) * | 0.20 (0.07) ** | 0.20 (0.07) ** | |
| RC | 0.18 (0.07) * | 0.12 (0.07) | 0.12 (0.07) † | |
| 1st G CA * FS | 0.68 (0.40)† | 0.70 (0.39) † | ||
| 2nd G CA * FS | 1.03 (0.58)† | 0.72 (0.42) † | ||
| 3rd-or-higher G CA * FS | –0.62 (1.68) | –0.27 (0.87) | ||
| 1st G CA * RS | 0.07 (0.17) | |||
| 2nd G CA * RS | –0.78 (0.54) | |||
| 3rd-or-higher G CA * RS | –0.33 (0.81) | |||
| 1st G CA * FC | –0.60 (0.30) * | –0.62 (0.30) * | ||
| 2nd G CA * FC | –1.01 (0.38) ** | –0.89 (0.48)† | ||
| 3rd-or-higher G CA * FC | 0.30 (0.55) | 0.61 (0.62) | ||
| 1st G CA * RC | 0.29 (0.33) | 0.28 (0.32) | ||
| 2nd G CA * RC | 1.07 (0.40) ** | 0.65 (0.43) | ||
| 3rd-or-higher G CA * RC | –1.05 (1.45) | –1.23 (0.79) | ||
| female (ref: male) | 0.65 (0.08) *** | 0.72 (0.08) *** | 0.71 (0.08) *** | 0.72 (0.08) *** |
| age | 0.11 (0.03) *** | 0.08 (0.03) *** | 0.08 (0.03) ** | 0.08 (0.03) ** |
| age^2 | –0.001 (0.0003) *** | –0.001 (0.0003) *** | –0.001 (0.0003) *** | –0.001 (.0003) *** |
| never married (ref) | 1 | 1 | 1 | 1 |
| married/cohabitating | –0.68 (0.18) *** | –0.75 (0.18) *** | –0.73 (0.18)*** | –0.73 (0.18)*** |
| div/sep/wid | 0.29 (0.20) | 0.17 (0.20) | 0.19 (0.20) | 0.17 (0.20) |
| employed (ref) | 1 | 1 | 1 | 1 |
| unemployed | 0.49 (0.28) | 0.41 (0.29) | 0.36 (0.30) | 0.36 (0.30) |
| not in labor force | 0.68 (0.17) *** | 0.56 (0.17) *** | 0.54 (0.17)** | 0.53 (0.17)** |
| college | –0.06 (0.13) | 0.12 (0.13) | 0.11 (0.13) | 0.12 (0.13) |
| constant | –4.27 (0.50) | –4.13 (0.53) | –4.11 (0.54) | –4.12 (0.53) |
| N = 4491 | ||||
© 2017 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, L. Depression Risks and Correlates among Different Generations of Chinese Americans: The Effects of Relationships with Friends and Relatives. Soc. Sci. 2017, 6, 56. https://doi.org/10.3390/socsci6020056
Zhu L. Depression Risks and Correlates among Different Generations of Chinese Americans: The Effects of Relationships with Friends and Relatives. Social Sciences. 2017; 6(2):56. https://doi.org/10.3390/socsci6020056
Chicago/Turabian StyleZhu, Lin. 2017. "Depression Risks and Correlates among Different Generations of Chinese Americans: The Effects of Relationships with Friends and Relatives" Social Sciences 6, no. 2: 56. https://doi.org/10.3390/socsci6020056






