Antifungal Activity of Commercial Essential Oils and Biocides against Candida Albicans
Abstract
:1. Introduction
2. Results
2.1. Minimum Inhibitory Concentration (MIC) 80 and Minimal Lethal Concentration
2.2. Minimal Biofilm Eradication Concentration 80
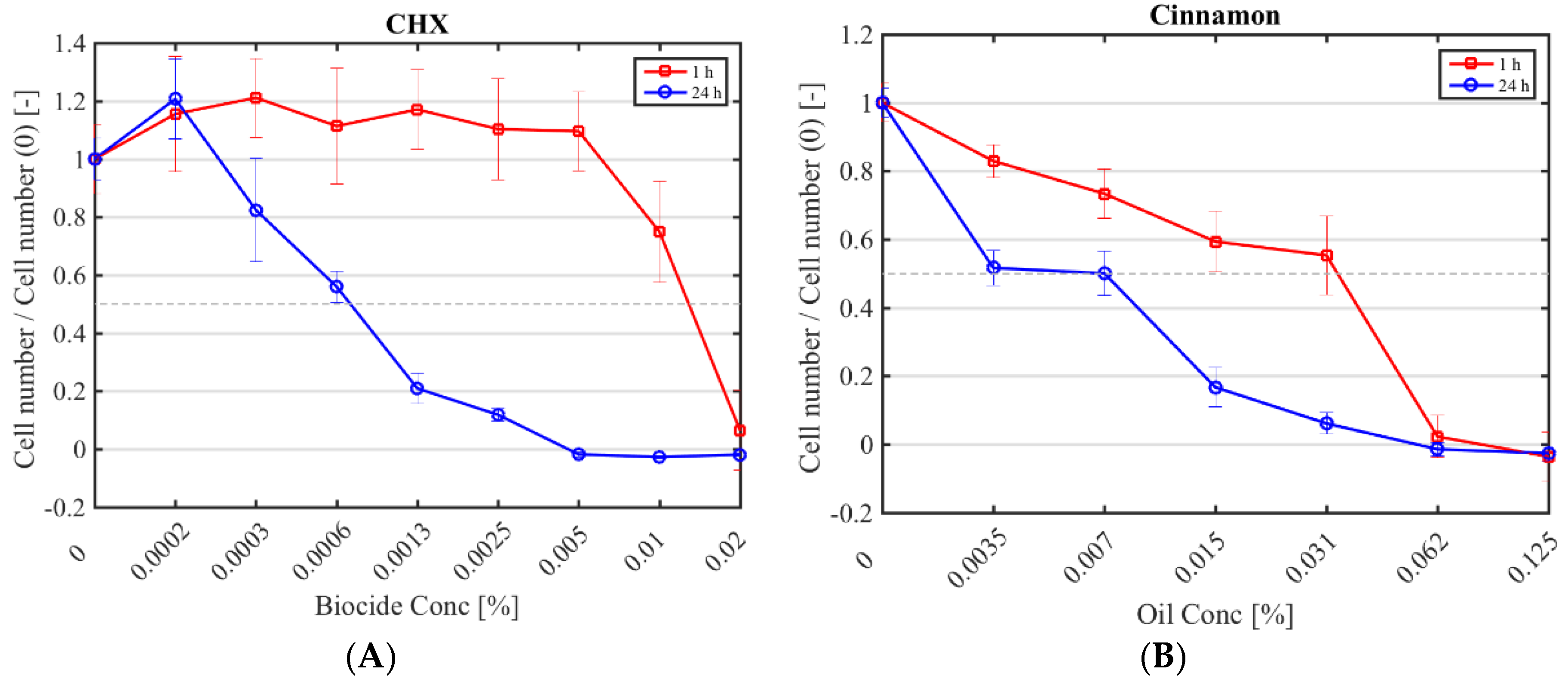
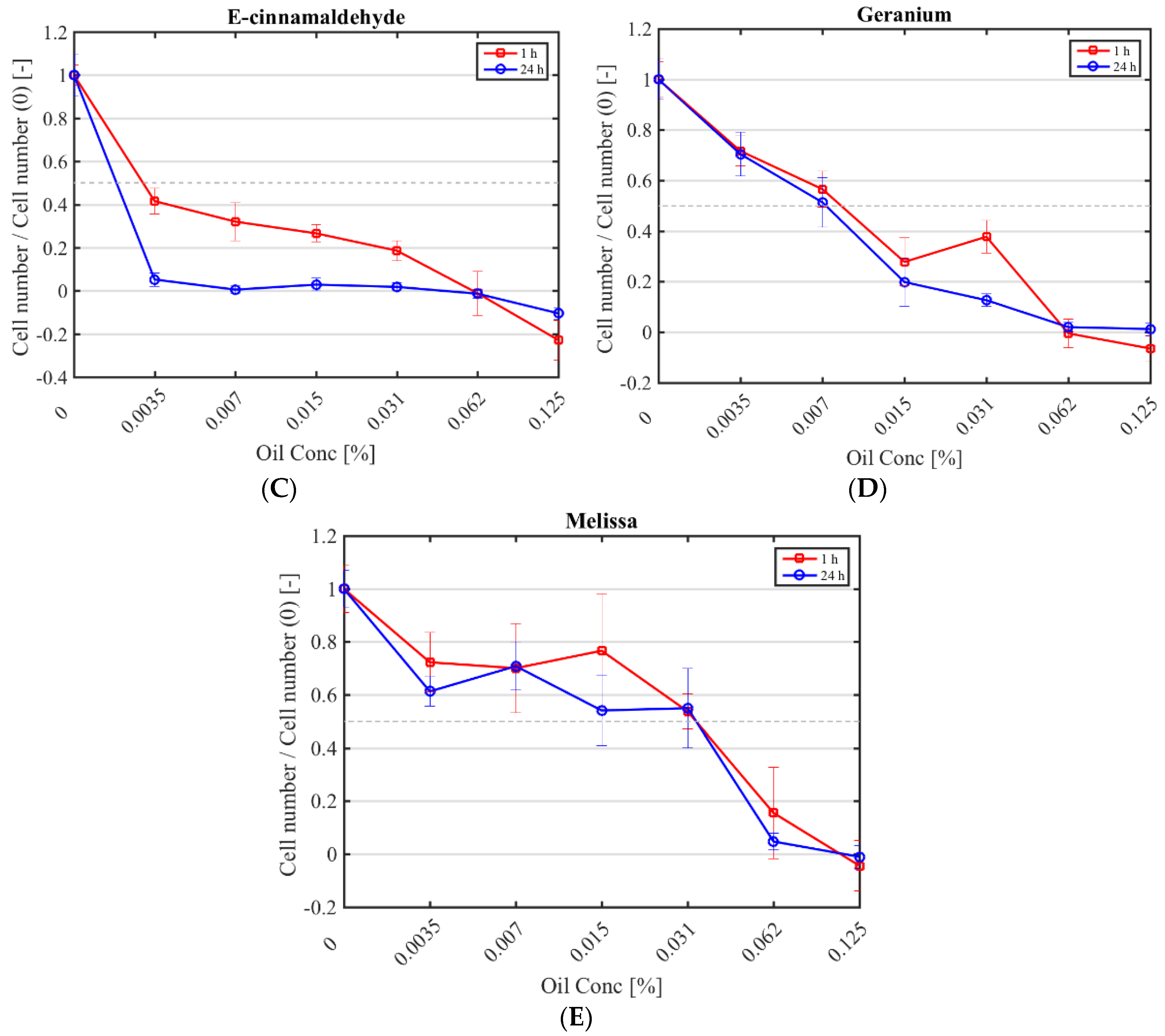
2.3. Half Maximal Inhibitory Concentration (IC50) against Fibroblasts
3. Discussion
4. Materials and Methods
4.1. Essential Oils and Biocides Preparation
4.2. Microorganisms
4.3. Minimum Inhibitory Concentration and Minimal Lethal Concentration
4.4. Minimal Biofilm Eradication Concentration 80
4.5. Half Maximal Inhibitory Concentration
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Muzyka, B.C. Oral fungal infections. Dent. Clin. N. Am. 2005, 49, 49–65. [Google Scholar] [CrossRef] [PubMed]
- Palmer, G.D.; Robinson, P.G.; Challacombe, S.J.; Birnbaum, W.; Croser, D.; Erridge, P.L.; Hodgson, T.; Lewis, D.; McLaren, A.; Zakrzewska, J.M. Aetiological factors for oral manifestations of HIV. Oral Dis. 1996, 2, 193–197. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, G.M.; Mackie, I.D.; Koval, J.; Sandhu, H.S.; Daley, T.D. Factors associated with increased frequency of HIV-related oral candidiasis. J. Oral Pathol. Med. 1991, 20, 332–336. [Google Scholar] [CrossRef] [PubMed]
- Farah, C.S.; Ashman, R.B.; Challacombe, S.J. Oral candidosis. Clin. Dermatol. 2000, 18, 553–562. [Google Scholar] [CrossRef]
- Gleiznys, A.; Zdanavičienė, E.; Žilinskas, J. Candida albicans importance to denture wearers. A literature review. Stomatologija 2015, 17, 54–66. [Google Scholar] [PubMed]
- Yasui, M.; Ryu, M.; Sakurai, K.; Ishihara, K. Colonisation of the oral cavity by periodontopathic bacteria in complete denture wearers. Gerodontology 2012, 29, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Douglass, C.W.; Shih, A.; Ostry, L. Will there be a need for complete dentures in the United States in 2020? J. Prosthet. Dent. 2010, 87, 5–8. [Google Scholar] [CrossRef]
- Sardi, J.C.O.; Scorzoni, L.; Bernardi, T.; Fusco-Almeida, A.M.; Mendes Giannini, M.J. Candida species: Current epidemiology, pathogenicity, biofilm formation, natural antifungal products and new therapeutic options. J. Med. Microbiol. 2016, 62, 10–24. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.; Lewis, M. Pathogenesis and treatment of oral candidosis. J. Oral Microbiol. 2011, 1, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Boros-Majewska, J.; Salewska, N.; Borowski, E.; Milewski, S.; Malic, S.; Wei, X.Q.; Hayes, A.J.; Wilson, M.J.; Williams, D.W. Novel Nystatin A1 derivatives exhibiting low host cell toxicity and antifungal activity in an in vitro model of oral candidosis. Med. Microbiol. Immunol. 2014, 203, 341–355. [Google Scholar] [CrossRef] [PubMed]
- Nazzaro, F.; Fratianni, F.; De Martino, L.; Coppola, R.; De Feo, V. Effect of essential oils on pathogenic bacteria. Pharmaceuticals 2013, 6, 1451–1474. [Google Scholar] [CrossRef] [PubMed]
- Sikkematb, J.; de Bontt, J.A.M. Interactions of cyclic hydrocarbons with biological membranes. J. Biol. Chem. 1994, 269, 8022–8028. [Google Scholar]
- Bakkali, F.; Averbeck, S.; Averbeck, D.; Idaomar, M. Biological effects of essential oils—A review. Food Chem. Toxicol. 2008, 46, 446–475. [Google Scholar] [CrossRef] [PubMed]
- Adil, M.; Singh, K.; Verma, P.K.; Khan, A.U. Eugenol-induced suppression of biofilm-forming genes in Streptococcus mutans: An approach to inhibit biofilms. J. Glob. Antimicrob. Resist. 2014, 2, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, N.N.R.; Alviano, C.S.; Blank, A.F.; Romanos, M.T.V.; Fonseca, B.B.; Rozental, S.; Rodrigues, I.A.; Alviano, D.S. Synergism Effect of the Essential Oil from Ocimum basilicum var. Maria Bonita and Its Major Components with Fluconazole and Its Influence on Ergosterol Biosynthesis. Evid. Based Complement Altern. Med. 2016, 2016, 5647182. [Google Scholar] [CrossRef] [PubMed]
- Rajput, S.B.; Karuppayil, S.M. Small molecules inhibit growth, viability and ergosterol biosynthesis in Candida albicans. Springerplus 2013, 2, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Samber, N.; Khan, A.; Varma, A.; Manzoor, N. Synergistic anti-candidal activity and mode of action of Mentha piperita essential oil and its major components. Pharm. Biol. 2015, 53, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Shreaz, S.; Wani, W.A.; Behbehani, J.M.; Raja, V.; Karched, M.; Ali, I.; Siddiqi, W.A.; Ting, L. Fitoterapia Cinnamaldehyde and its derivatives, a novel class of antifungal agents. Fitoterapia 2016, 112, 116–131. [Google Scholar] [CrossRef] [PubMed]
- de Castro, R.D.; Lima, E.O. Anti-Candida Activity and Chemical Composition of Cinnamomum zeylanicum Blume Essential Oil. Braz. Arch. Biol. Technol. 2013, 56, 749–755. [Google Scholar] [CrossRef]
- Bang, K.; Lee, D.; Park, H.; Rhee, Y. Inhibition of fungal cell wall synthesizing enzymes by trans-cinnamaldehyde. Biosci. Biotechnol. Biochem. 2000, 64, 1061–1063. [Google Scholar] [CrossRef] [PubMed]
- Cox, S.D.; Mann, C.M.; Markham, J.L.; Bell, H.C.; Gustafson, J.E.; Warmington, J.R.; Wyllie, S.G. The mode of antimicrobial action of the essential oil of Melaleuca alternifolia (Tea tree oil). J. Appl. Microbiol. 2000, 88, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Rajkowska, K.; Nowak, A.; Kunicka-styczy, A.; Siadura, A. Biological effects of various chemically characterized essential oils: Investigation of the mode of action against Candida albicans and HeLa cells. RSC Adv. 2016, 6, 97199–97207. [Google Scholar] [CrossRef]
- Singh, S.; Fatima, Z.; Hameed, S. Citronellal-induced disruption of membrane homeostasis in Candida albicans and attenuation of its virulence attributes. Rev. Soc. Bras. Med. Trop. 2016, 49, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Gyawali, R.; Ibrahim, S.A. Natural products as antimicrobial agents. Food Control 2014, 46, 412–429. [Google Scholar] [CrossRef]
- Morais-Braga, M.F.B.; Sales, D.L.; Carneiro, J.N.P.; Machado, J.T.; Thassya, A.; Santos, L.; de Freitas, M.A.; Matos, D.; Tintino, S.R.; Souza, D.S.L.; et al. Psidium guajava L. and Psidium brownianum Mart ex DC.: Chemical composition and anti—Candida effect in association with fluconazole. Microb. Pathog. 2016, 95, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Santos, K.K.; Matias, E.F.; Souza, C.E.; Tintino, S.R.; Braga, M.F.; Guedes, G.M.; Nogueira, L.F.; Morais, E.C.; Costa, J.G.; Menezes, I.R.; et al. Anti-candida activity of Mentha arvensis and Turnera ulmifolia. J. Med. Food 2012, 15, 322–324. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, G.; Berman, C.; Jaffin, R. Chlorhexidine. An adjunct to periodontal therapy. J. Periodontol. 1986, 57, 370–377. [Google Scholar] [PubMed]
- Cullinan, M.P.; Westerman, B.; Hamlet, S.M.; Palmer, J.E.; Faddy, M.J.; Seymour, G.J. The effect of a triclosan-containing dentifrice on the progression of periodontal disease in an adult population. J. Clin. Periodontol. 2003, 30, 414–419. [Google Scholar] [CrossRef] [PubMed]
- Malic, S.; Emanuel, C.; Lewis, M.A.; Williams, D.W. Antimicrobial activity of novel mouthrinses against planktonic cells and biofilms of pathogenic microorganisms. Microbiol. Discov. 2013, 1, 11. [Google Scholar] [CrossRef]
- Hammer, K.A.; Carson, C.F.; Riley, T.V. Antimicrobial activity of essential oils and other plant extracts. J. Appl. Microbiol. 1999, 86, 985–990. [Google Scholar] [CrossRef] [PubMed]
- Janssen, A.M.; Scheffer, J.C.; Svendsen, A.B. Antimicrobial activity of essential oils: A 1976–1986 literature review. Aspects of the test methods. Planta Med. 1986, 53, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Szweda, P.; Gucwa, K.; Kurzyk, E.; Romanowska, E. Essential oils, silver nanoparticles and propolis as alternative agents against fluconazole resistant Candida albicans, Candida glabrata and Candida krusei clinical isolates. Indian J. Microbiol. 2015, 55, 175–183. [Google Scholar] [CrossRef] [PubMed]
- Carvalhinho, S.; Margarida, A.; Sampaio, A. Susceptibilities of Candida albicans mouth isolates to antifungal agents, essentials oils and mouth rinses. Mycopathologia 2012, 174, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Zore, G.B.; Thakre, A.D.; Rathod, V.; Karuppayil, S.M. Evaluation of anti-Candida potential of geranium oil constituents against clinical isolates of Candida albicans differentially sensitive to fluconazole: Inhibition of growth, dimorphism and sensitization. Mycoses 2010, 54, 99–109. [Google Scholar] [CrossRef] [PubMed]
- Mimica-Dukic, N.; Bozin, B.; Sokovic, M.; Simin, N. Antimicrobial and antioxidant activities of Melissa officinalis L. (Lamiaceae) Essential Oil. J. Agric. Food Chem. 2004, 52, 2485–2489. [Google Scholar] [CrossRef] [PubMed]
- Abdellatif, F.; Boudjella, H.; Zitouni, A.; Hassani, A. Chemical composition and antimicrobial activity of the essential oil from leaves of algerian. Exp. Clin. Sci. J. 2014, 13, 772–781. [Google Scholar]
- Marcos-Arias, C.; Eraso, E.; Madariaga, L.; Quindós, G. In vitro activities of natural products against oral Candida isolates from denture wearers. BMC Complement Altern. Med. 2011, 11, 119. [Google Scholar] [CrossRef] [PubMed]
- Hammer, K.A.; Carson, C.F.; Riley, T.V. In vitro activity of essential oils, in particular Melaleuca alternifolia (tea tree) oil and tea tree oil products, against Candida spp. J. Antimicrob. Chemother. 1998, 42, 591–595. [Google Scholar] [CrossRef] [PubMed]
- Sookto, T.; Srithavaj, T.; Thaweboon, S.; Thaweboon, B.; Shrestha, B. In vitro effects of Salvia officinalis L. essential oil on Candida albicans. Asian Pac. J. Trop. Biomed. 2013, 3, 376–380. [Google Scholar] [CrossRef]
- Nacsa-Farkas, E.; Kerekes, E.; Kerekes, E.B.; Krisch, J.; Roxana, P.; Vlad, D.C.; Ivan, P.; Vágvölgyi, C. Antifungal effect of selected European herbs against Candida albicans and emerging pathogenic non-albicans Candida species. Acta Biol. Szeged. 2014, 58, 61–64. [Google Scholar]
- Thosar, N.; Basak, S.; Bahadure, R.N.; Rajurkar, M. Antimicrobial efficacy of five essential oils against oral pathogens: An in vitro study. Eur. J. Dent. 2013, 7. [Google Scholar] [CrossRef] [PubMed]
- Mahboubi, M.; Bidgoli, F.G. Phytomedicine In vitro synergistic efficacy of combination of amphotericin B with Myrtus communis essential oil against clinical isolates of Candida albicans. Phytomedicine 2010, 17, 771–774. [Google Scholar] [CrossRef] [PubMed]
- Brading, M.G.; Cromwell, V.J.; Green, A.K.; Debrabander, S.; Beasley, T. The role of Triclosan in dentifrice formulations, with particular reference to a new 0.3% Triclosan calcium carbonate-based system. Int. Dent. J. 2004, 54, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Hawser, S.P.; Douglas, L.J. Resistance of Candida albicans biofilms to antifungal agents in vitro. Antimicrob. Agents Chemother. 1995, 39, 2128–2131. [Google Scholar] [CrossRef] [PubMed]
- Douglas, L.J. Candida biofilms and their role in infection. Trends Microbiol. 2003, 11, 30–36. [Google Scholar] [CrossRef]
- De Almeida, L.F.D.; Paula, J.F.; Almeida, R.V.; Williams, D.W.; Hebling, J.; Cavalcanti, Y.W. Efficacy of citronella and cinnamon essential oils on Candida albicans biofilms. Acta Odontol. Scand. 2016, 74, 393–398. [Google Scholar] [CrossRef] [PubMed]
- de Campos Rasteiro, V.M.; da Costa, A.C.; Araújo, C.F.; de Barros, P.P.; Rossoni, R.D.; Anbinder, A.L.; Jorge, A.O.; Junqueira, J.C. Essential oil of Melaleuca alternifolia for the treatment of oral candidiasis induced in an immunosuppressed mouse model. BMC Complement. Altern. Med. 2014, 14, 489–499. [Google Scholar] [CrossRef] [PubMed]
- Paul, J.; Adeniran, A.; Augusti, A.; Vargas, C.; Olalekan, O.; Hassan, W.; Ibrahim, M.; Pansera, E.; Francine, D. Antioxidant activity, genotoxicity and cytotoxicity evaluation of lemon balm (Melissa officinalis L.) ethanolic extract: Its potential role in neuroprotection. Ind. Crop. Prod. 2013, 51, 26–34. [Google Scholar]
- Ka, H.; Park, H.; Jung, H.; Choi, J.; Cho, K.; Ha, J.; Lee, K. Cinnamaldehyde induces apoptosis by ROS-mediated mitochondrial permeability transition in human promyelocytic leukemia HL-60 cells. Cancer Lett. 2003, 196, 143–152. [Google Scholar] [CrossRef]
- Barros, F.J.; Costa, R.J.O.; Cesário, F.R.A.S.; Rodrigues, L.B.; de Menezes, I.R.A.; da Costa, J.G.M.; Coutinho, H.D.M.; Galvao, H.B.F. Activity of essential oils of Piper aduncum anf and Cinnamomum zeylanicum by evaluating osmotic and morphologic fragility of erythrocytes. Eur. J. Integr. Med. 2016, 8, 505–512. [Google Scholar] [CrossRef]
- Li, Y.C.; Kuan, Y.H.; Lee, S.S.; Huang, F.M. Cytotoxicity and genotoxicity of chlorhexidine on macrophages in vitro. Environ. Toxicol. 2014, 29, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Cabral, C.T.; Fernandes, M.H. In vitro comparison of chlorhexidine and povidone-iodine on the long-term proliferation and functional activity of human alveolar bone cells. Clin. Oral Investig. 2007, 11, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Mann, C.M.; Markham, J.L. A new method for determining the minimum inhibitory concentration of essential oils. Appl. Microbiol. 1998, 84, 538–544. [Google Scholar] [CrossRef]
- Malic, S.; Hill, K.E.; Ralphs, J.R.; Hayes, A.; Thomas, D.W.; Potts, A.J.; Williams, D.W. Characterization of Candida albicans infection of an in vitro oral epithelial model using confocal laser s canning microscopy. Microbiol. Immunol. 2007, 22, 188–194. [Google Scholar]
| Antimicrobial | Minimum Inhibitory Concentration 80 [% (v/v)] [(g/L)] | |
|---|---|---|
| C. albicans NYCY 1363 | C. albicans 135BM2/94 | |
| Basil | 0.1 (0.9) | 0.1 (0.9) |
| Bergamot | 0.3 (2.6) | 0.3 (2.6) |
| Cinnamon | 0.1 (1.0) | 0.1 (1.0) |
| Citronella | 0.1 (0.9) | 0.1 (0.9) |
| Geranium | 0.07 (0.6) | 0.06 (0.5) |
| Lavender | 0.2 (1.8) | 0.1 (0.9) |
| Melissa | 0.06 (0.5) | 0.06 (0.5) |
| Myrtle | 0.4 (3.5) | 0.3 (2.7) |
| Peppermint | 0.1 (0.9) | 0.1 (0.9) |
| Sage | 0.4 (3.7) | 0.3 (2.7) |
| Spearmint | 0.2 (1.6) | 0.1 (1.1) |
| Tea tree oil | 0.2 (1.8) | 0.2 (1.8) |
| E-cinnamaldehyde | 0.03 (0.3) | 0.01 (0.1) |
| Linalool | 0.1 (0.9) | 0.1 (0.9) |
| CHX | 2 × 10−3 (2.1 × 10−2) | 5 × 10−3 (5.3 × 10−2) |
| Triclosan | 5.66 × 10−4 (8.4 × 10−3) | 5.89 × 10−4 (8.8 × 10−3) |
| Antimicrobial | Minimal Lethal Concentration [% (v/v)] [(g/L)] | |
|---|---|---|
| C. albicans NCYC 1363 | C. albicans 135BM2/94 | |
| Basil | 0.5 (4.5) | 0.5 (4.5) |
| Bergamot | 0.5 (4.4) | 0.5 (4.4) |
| Cinnamon | 0.1 (1.0) | 0.1 (1.0) |
| Citronella | 0.1 (0.9) | 0.1 (2.7) |
| Geranium | 0.1 (0.9) | 0.1 (0.9) |
| Lavender | 0.5 (4.4) | 0.3 (2.6) |
| Melissa | 0.1 (0.9) | 0.1 (0.9) |
| Myrtle | 1 (8.8) | 1 (8.8) |
| Peppermint | 0.3 (2.7) | 0.1 (0.9) |
| Sage | 1 (9.2) | 1 (9.2) |
| Spearmint | 1 (9.2) | 1 (9.2) |
| Tea tree oil | 0.5 (4.5) | 0.3 (2.7) |
| E-cinnamaldehyde | 0.03 (0.3) | 0.03 (0.3) |
| Linalool | 0.3 (2.6) | 0.3 (2.6) |
| CHX | 2.5 × 10−3 (2.7 × 10−2) | 5 × 10−3 (5.3 × 10−2) |
| Triclosan | NA | NA |
| Antimicrobial | Minimal Biofilm Eradication Concentration 80 [% (v/v)] [(g/L)] | |
|---|---|---|
| C. albicans NYCY 1363 | C. albicans 135BM2/94 | |
| Basil | NA | NA |
| Bergamot | NA | NA |
| Cinnamon | NA | NA |
| Citronella | NA | NA |
| Geranium | 2.5 (22.3) | 2 (17.9) |
| Lavender | NA | NA |
| Melissa | 1.5 (13.3) | 1.5 (13.3) |
| Myrtle | NA | NA |
| Peppermint | NA | NA |
| Sage | NA | NA |
| Spearmint | NA | NA |
| Tea tree oil | NA | NA |
| E-cinnamaldehyde | 0.8 (8.4) | 0.8 (8.4) |
| Linalool | 1 (8.7) | 1.5 (13.1) |
| CHX | 0.07 | NA |
| Triclosan | >5 × 10−3 (7.45 × 10−2) | >5 × 10−3 (7.45 × 10−2) |
| Antimicrobial | Half Maximal Inhibitory Concentration [% (v/v)] [(g/L)] | |
|---|---|---|
| 1 h | 24 h | |
| Cinnamon | 0.03 (0.36) | 0.01 (0.11) |
| Geranium | 0.01 (0.08) | 0.01 (0.07) |
| Melissa | 0.03 (0.3) | 0.03 (0.3) |
| E-cinnamaldehyde | 0.003 (0.03) | 0.002 (0.02) |
| CHX | 0.01 (0.15) | 7.32 × 10−4 (0.008) |
| Plant Species | Essential Oil | Origin |
|---|---|---|
| Ocimum basilicum | Basil oil | Leaves |
| Citrus bergamia | Bergamot FCF oil | Peel |
| Cinnamomum zeylanicum | Cinnamon leaf oil | Leaves |
| Cymbopogon winterianus | Citronella oil | Aerial parts |
| Pelargonium graveolens | Geranium oil | Flowering herb |
| Lavandula angustifolia | Lavender oil | Flowering herb |
| Melissa officinalis | Melissa oil | Leaves and tops |
| Myrtus communis | Myrtle oil | Leaves |
| Mentha piperita | Peppermint oil | Whole plant |
| Salvia officinalis | Sage oil | Leaves |
| Mentha spicata | Spearmint oil | Aerial parts |
| Melaleuca alternifolia | Tea tree oil | Leaves and twigs |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Serra, E.; Hidalgo-Bastida, L.A.; Verran, J.; Williams, D.; Malic, S. Antifungal Activity of Commercial Essential Oils and Biocides against Candida Albicans. Pathogens 2018, 7, 15. https://doi.org/10.3390/pathogens7010015
Serra E, Hidalgo-Bastida LA, Verran J, Williams D, Malic S. Antifungal Activity of Commercial Essential Oils and Biocides against Candida Albicans. Pathogens. 2018; 7(1):15. https://doi.org/10.3390/pathogens7010015
Chicago/Turabian StyleSerra, Elisa, Lilia Araida Hidalgo-Bastida, Joanna Verran, David Williams, and Sladjana Malic. 2018. "Antifungal Activity of Commercial Essential Oils and Biocides against Candida Albicans" Pathogens 7, no. 1: 15. https://doi.org/10.3390/pathogens7010015





